Fifth Stage
Medicine
Dr. Fadhil – Lecture 3
1
Rheumatoid arthritis
It ‘s a chronic systemic autoimmune inflammatory disease affecting all joints covered
by synovium leading to destructive polyarthritis
RA is the most common inflammatory arthritis
•
causes severe joint destruction
•
is a systemic disease with systemic damage
•
leads to disability
•
Is associated with significant costs
•
Is an immune mediated disease driven by inflammatory cytokines
•
It can be disabling and painful condition , that can lead to substantial loss of function
and mobility if not adequately treated.
•
The process involves an inflammatory response of the capsule around the
joints(synovium) secondary to swelling of synovial cells, excess synovial fluid, and the
development of fibrous tissue(pannus) in the synovium.
2
•
The pathology of the disease process often lead to destruction of articular cartilage&
ankylosis(fusion) of the joints .
•
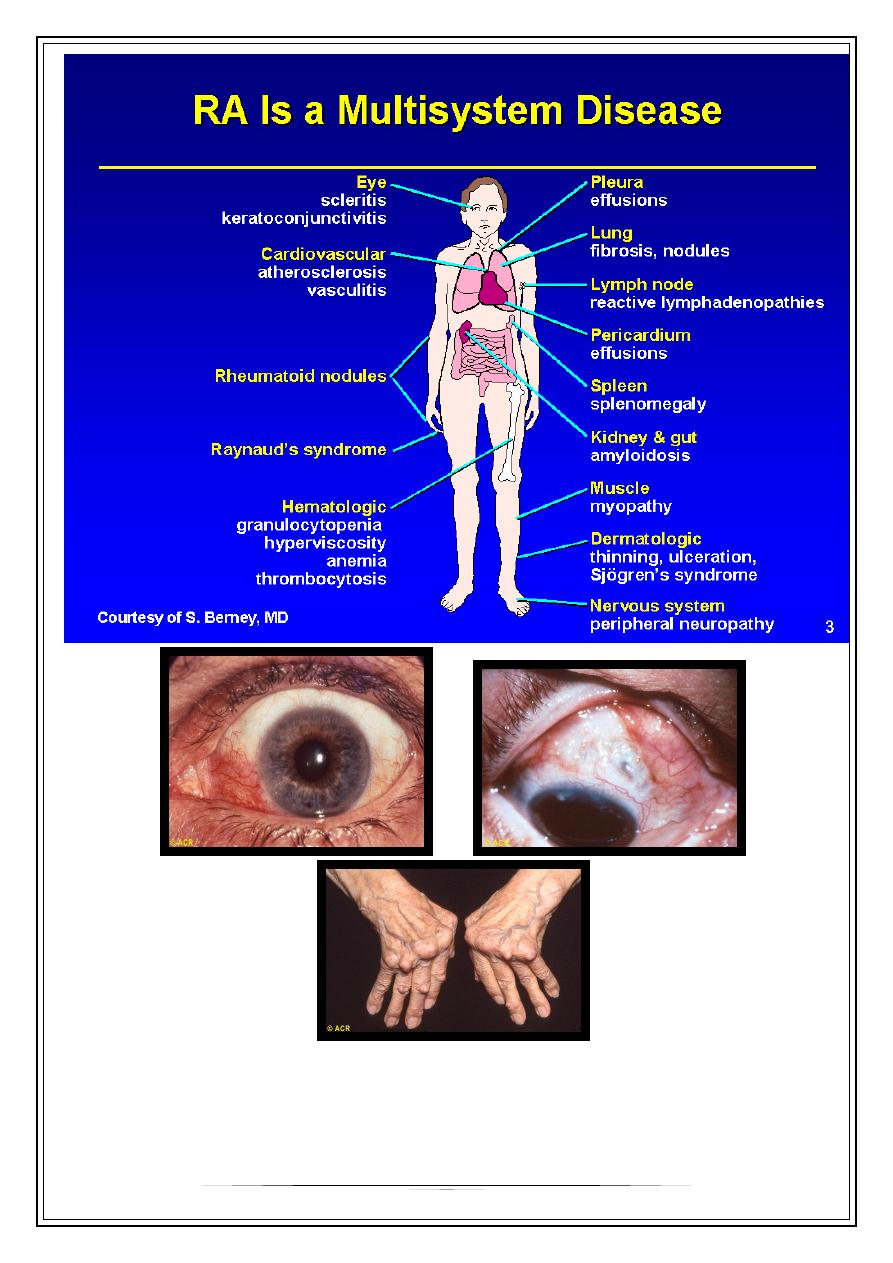
RA can also produce diffuse inflammation in the lungs , the membrane around the
heart(pericardium),the membrane around the lungs(pleura),and the sclera, in
addition to nodular lesions in the subcutaneous tissues.
•
Autoimmunity plays a role in the pathology of RA, and RA is a systemic autoimmune
disease.
Etiology
•
It is an autoimmune disease , higher in monozygotic twins &first degree relatives
with HLA association , for example 50-75% of Caucasians have HLA-DR4, DR1 in
Indians & DW15 in Japanese. DR4 is associated with more erosive disease.
•
Female gender & cigarette smoking are risk factors. There is an increased risk in
breast feeding female.
Pathology
•
The inflammation and thickening of the synovial membranes cause irreversible
damage to the joint capsule and articular cartilage as these structures replaced by
scar like tissue called Pannus.
•
It is much more common than osteoarthritis which is associated with aging. It
primarily affects young& middle age groups. Children are affected by a similar
disorder called juvenile RA.
Presentation
•
70% insidious onset (weeks to mnths)
•
10% acute (fulminant onset)
•
20% sub acute onset
Clinical Features& Diagnosis
•
Tendon and bursa involvement are frequent and often clinically dominant in the early
disease. RA can affect any joint, but has a predilection for metacarpophalangeal,
proximal interphalangeal and metatarsophalangeal joints, as well as the wrists and
knees.
•
Articular and periarticular manifestations include joint swelling and tenderness to
palpation ,with morning stiffness and sever motion impairment in the involved joints.
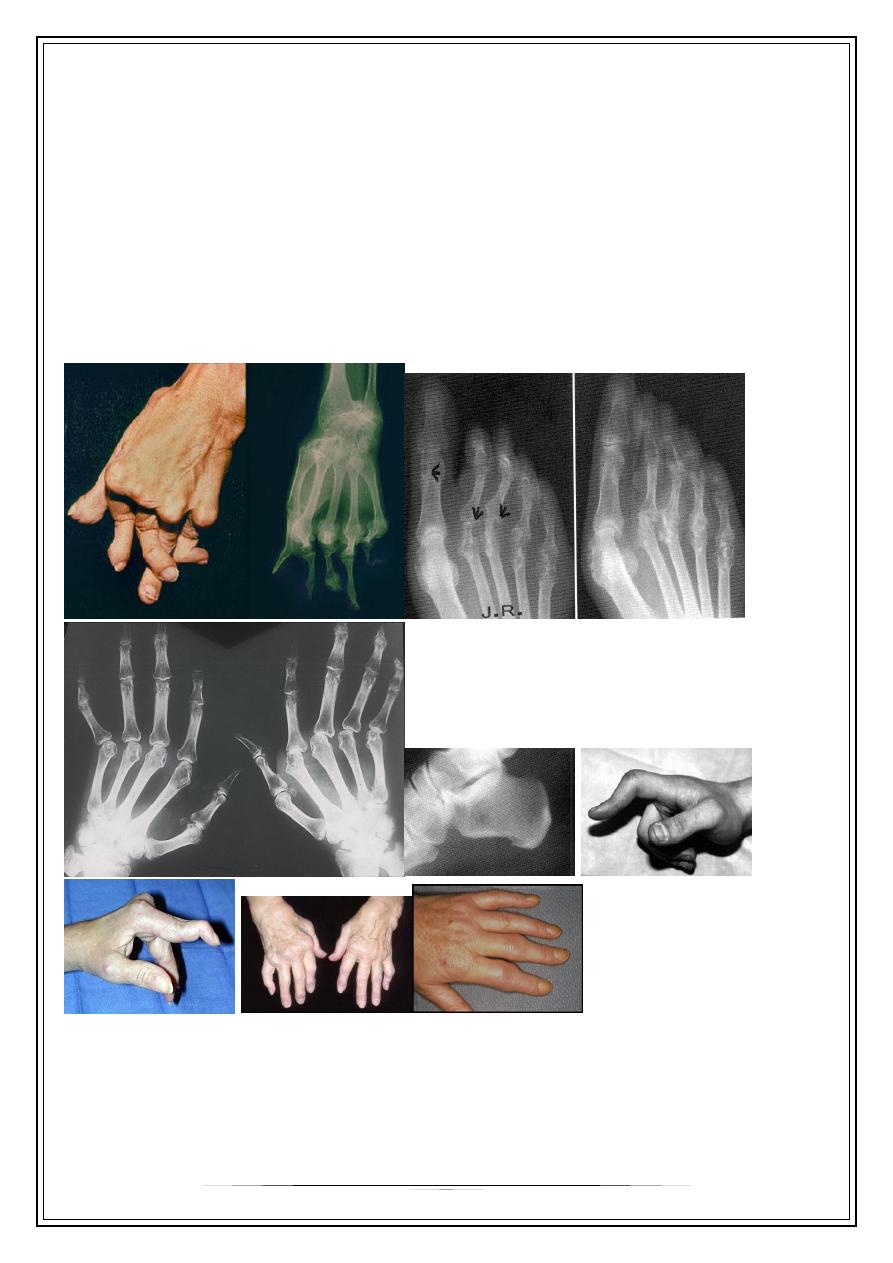
HAND JOINTS
•
Provide a good reflection of disease activity. The typical features are symmetrical
swelling of MCP& PIP joints. They are hot, tender & have stress pain on passive
movement.
3
•
Specific hand abnormalities include swan neck deformity, button hole
(boutonnière) deformity& Z- deformity of thumb. Other abnormalities include :
•
dorsal subluxation of ulnar styloid of the wrist , trigger finger, cock up deformity of
the toe, flatfoot, Baker's(popliteal) cyst which can be mistaken for DVT, but past
history of joint disease & Doppler U/S can establish the diagnosis of DVT.
Extra-articular features
•
Are more common in longstanding RA, but may occur at presentation specially in
men.
•
Most features are due to serositis, granuloma, nodule formation or vasculitis:
1-systemic = fever, weight loss, fatigue, susceptibility to infection
2-MSK =muscle wasting, tenosynovitis, bursitis, osteoporosis
3- hematological= anemia, thrombocytosis, eosinophilia.
Causes of anemia in RA:
*anemia of chronic disease.
*megaloblastic anemia due to folate deficiency or associated pernicious
anemia.
*Felty's syndrome.
*drugs: NSAIDs causing iron deficiency anemia; bone marrow suppression
caused by gold& cytotoxic drugs.
4-lymphatic= splenomegaly, Felty's syndrome
5-nodules= sinuses, fistula
6-ocular= episcleritis, scleritis, scleromalacia, keratoconjunctivitis sicca
7-vasculitis= digital arteritis, ulcers, pyoderma gangerenosum, mononeuritis
multiplex, visceral arteritis
8-cardiac= pericarditis, myocarditis, endocarditis, conduction defect, coronary
vasculitis, granulomatous arteritis
9-pulmonary= nodules, pleural effusion, fibrosing alveolitis, bronchiolitis, Caplan's
syndrome(RA with multiple pulmonary nodules & pneumoconiosis)
10-neurological= cervical cord compression, compression neuropathies, peripheral
neuropathy, mononeuritis multiplex
11-amyloidosis= nephrotic syndrome
Felty's syndrome
The association of splenomegaly, leucopenia, neutropenia(hypersplenism)& leg
ulcers with RA. Splenectomy ameliorates hypersplenism.
It occurs in 1% of RA patients over the age of 50 , more common in female than
male with long standing RA & in deforming but inactive disease..
Such patients have normochromic normocytic anemia, thrombocytopenia& abnormal
liver function tests. It is very common in African Americans& such patients are
susceptible to infections because of neutropenia
4
Diagnostic Tools in Rheumatoid Arthritis
•
Rheumatoid factor
•
Anti-CCP antibodies
5
•
Plain X-ray
•
MRI
•
Ultrasound
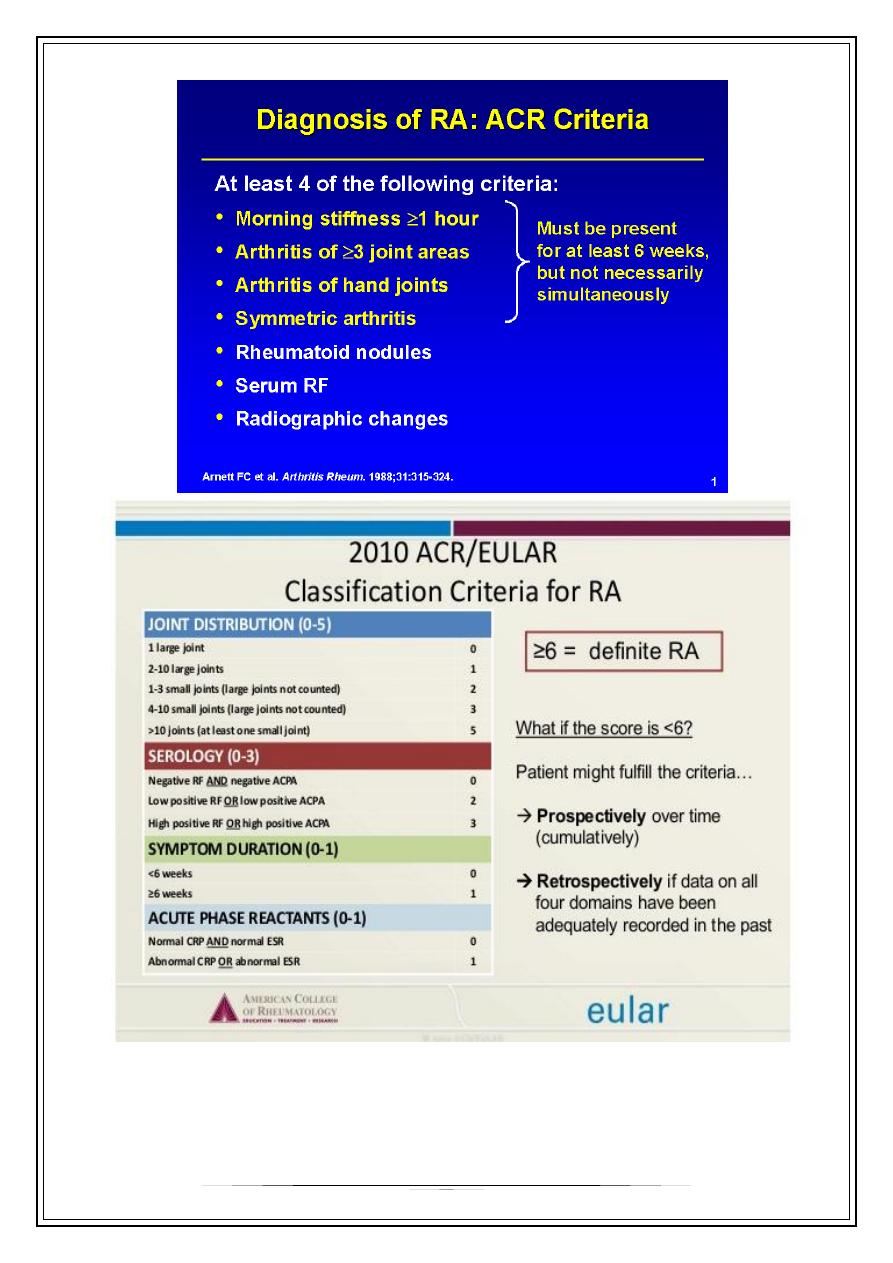
INVESTIGATIONS
1- clinical criteria.
2- acute phase response high ESR& CRP
3- X-ray: the typical radiographic changes of RA are periarticular osteopenia&
marginal non proliferative erosions.
4-serological tests : rheumatoid factor(RF) is usually positive in patients with
seropositive RA. RF has low specificity & sensitivity. It is an IgM antibody directed
against Fc fragment of human IgG. It occurs in a wide variety of diseases & also in
some normal adults.
•
It has prognostic marker, a high titer at presentation is associated with
poorer prognosis. Therefore, it has no rule in diagnosis, since it may appear
years after presentation.
•
10-20% of patients with RA are seronegative
5- What Is Anti-CCP?
•
Anti-CCP, which stands for anti-cyclic citrullinated peptide antibody, is
•
When Is It Appropriate to Have the Anti-CCP Test?
•
to order during the
person who may have rheumatoid arthritis. If present in such a patient at a
moderate to high level, it not only confirms the diagnosis but also may
indicate that the patient is at increased risk for joints damage. Low levels of
this antibody are less significant. In the past, doctors relied on another
antibody, the
6-- examination of synovial fluid: is the most helpful laboratory procedure; the
fluid is inflammatory with >10.000 WBC (PMN cells).
*Antinuclear Abs are common but not diagnostic.
Differential diagnosis
1-SLE
2- Lyme disease-
3-Viral arthritis
4-polymyalgia rheumatica
5- hypothyroidism
6-paraneoplastic syndromes
6
Thank you,,,
