1
Fifth Stage – ENT – Dr.Mushtaq – Lecture 8
Tonsillitis
Acute tonsillitis
• Infection of the tonsil
• May effect any age group but most frequently found in children.
Aetiology
• Viral infection : 50%
influenza ,parainfluenza,adenovirus, & rhinovirus
• Bacterial infection:
- B-haemolytic streptococcus
- Strept.pneumonia,
- H influenzae
- Staph. Aureus
- Moraxella catarrahlis
- Anaerobic organisms
Pathology:
1. Acute paranchymatous type:
whole ts. is infected causing generalized swelling , reddened & edematous
surface.
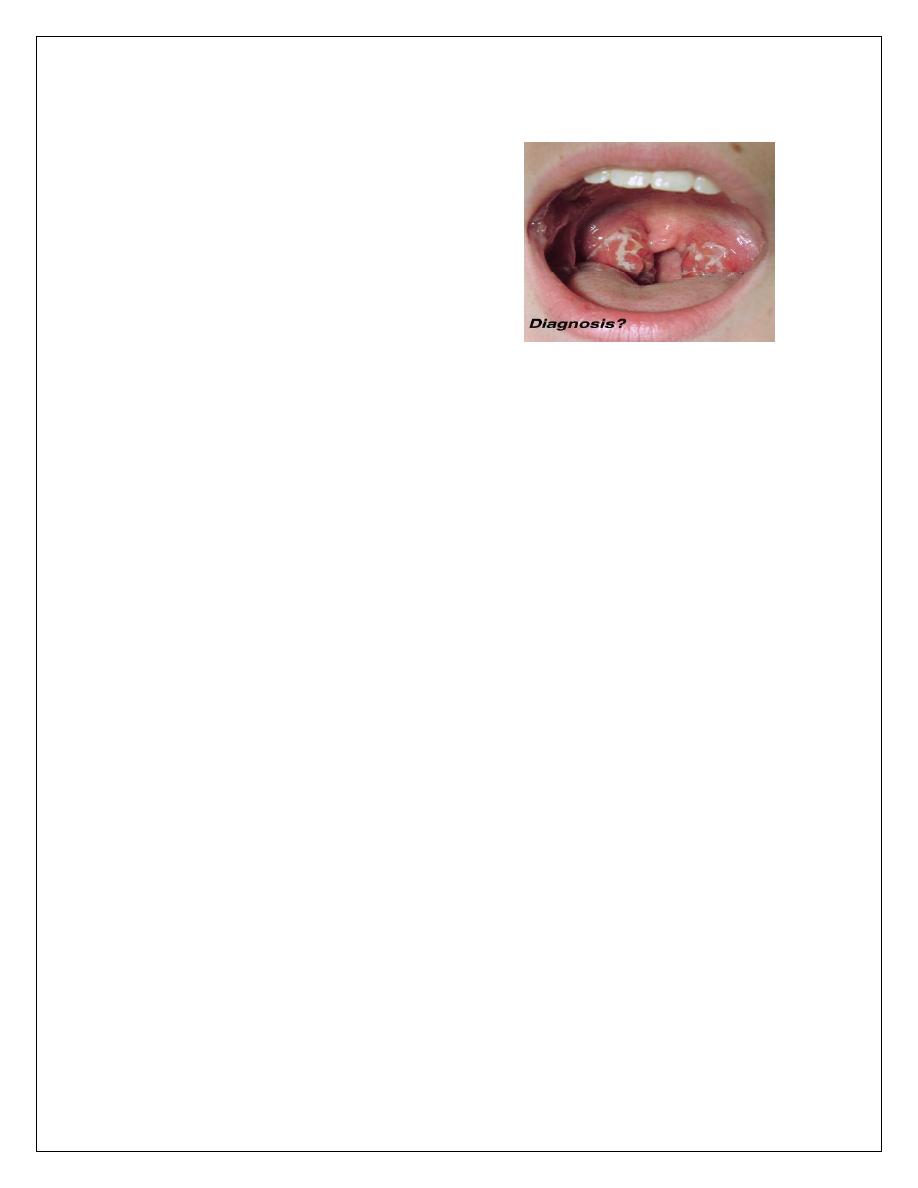
2. Acute follicular ts. :
crypts of ts. Filled with pus giving spotted appearance
Clinical features:
1. Sorethroat
2. Pyrexia
3. Odynophagia
4. Malaise
5. Earache
6. Thickened speech
2
7. In severe cases rigor & signs of toxaemia
8. Appendicitis
may simulated/ mesenteric adenitis.
Examination:
• Congested & enlarged ts.
• Congested pillars.
• Spots of pus or fibrin fill the crypts
• Furred tongue & halitosis
• Enlarged tender cx Ln.
Investigation:
1. Throat swab for c/s
2. Throat swab for K.L.B.
3. Blood film / mono spot test (I.m.n.)
DDX:
1. Scarlet fever
2. Diphtheria
3. Vincent`s infection
4. Agranulocytosis
5. I.M.N. ( glandular fever)
Treatment:
• Bed rest , soft diet ,fluid intake
• Analgesic drug
• Systemic AB.
Complications:
1. Peritonsillar abscess
2. Parapharyngeal abscess
3. Retropharyngeal abscess
4. Edema of the larynx
5. Acute rheumatism
3
6. Acute nephritis
7. Septicemia
8. Acute OM.
Recurrent acute tonsillitis
Clinical features:
1. persistent or recurrent sore throat
2. marked ts. enlargment.
3. injected ant. pillars
4. halitosis
5. persistent cx. adenitis.
Treatment:
tonsillectomy
Tonsillectomy:
Indications:
1- recurrent ts. : 6//1 year
or 3//2 years
2-
recurrent episodes of peritonsillar abscess
3- suspected neoplasm ( unilat enlargement,or ulceration)
Contraindications:
1. Recent ts. infection or URTI
2. Bleeding disorders
3. Using of contraceptives
4. Cleft palate
5. Epidemics of poilo
Complications of tonsillectomy:
A. Peroperative:
1- anaesthetic reaction
4
2- haemorrhage
3- damage to teeth, uvula, or to post. Pharyngeal wall
4- dislocation of the temporomandibular joint
B. Post operative:
Reactionary hemorrhage / 1
st
,24hs
Anaesthetic complications
Secondary haemorrhage / 5
th
– 10
th
day
Infection of the ts. bed
Earache
Pneumonia
Tonsillar remanant
Post ts, haemorrhage:
Reactionary (primary)
secondary
Reactionary haemorrhage:
~2%
Within 24hs
Signs of the bleeding :
- obvious bleeding
- gurgling sound in throat on breathing
- repeated swallowing
- vomiting
- rising pulse rate & lowering of the Bp.
Management:
Blood sample for cross matching
IV, infusion
Identifying the bleeding site
Application of 1:1000 adrenaline soaked gauze or using hydrogen peroxide gurgle
5
If failed >>> 2
nd
anaesthesia >>stop the bleeding
Secondary haemorrhage
5
th
- 10
th
day
Infection
R/: admission & observation
Blood for cross match
AB.
Removal of the clot , H2O2 gargle>>20minutes .if failed>> adrenaline socked
gauze>>20minutes
If failed 2
nd
anaesthesia suturing the pillars .
Peritonsillar abscess(quinsy)
Def; pus collects between ts. & sup. Cons.m.
Aetiology;
- follows tonsillitis
- mostly unilateral
Clinical features:
1) -severe pain
2) -pyrexia up to 40 C°
3) -headache & malaise
4) -trismus
5) -earache
6) -intense salivation
7) Thickened speech
8) Fetor oris

6
Examination
Marked hyperaemic edematous tonsil and palatal region
Oedematous uvula & pushed towards other side
Complications
Parapharyngeal abscess
Oedema of the larynx
septicemia
Treatment
1. Conservative in early stage( cellulitis)
- rest , AB. , analgesia
2. Surgery :
- incision of the abscess
- abscess-tonsillectomy
Thank you,,,
