
_
In health
Visceral lubrication Fluid and particulate absorption
_
In disease
Pain perception (mainly parietal) Inflammatory and immune responses
Fibrinolytic activity
PERITONITIS
Peritonitis is simply defined as inflammation of the peritoneum and may be
localized or generalised. Most cases of peritonitis are caused by an invasion
of the peritoneal cavity by bacteria, , acute bacterial peritonitis. In this
instance, free fluid spills into the peritoneal cavity and circulates largely
directed by the normal peritoneal attachments and gravity.
For example, spillage from a perforated peptic ulcer may run down the right
paracolic gutter leading to presentation with pain in the right iliac fossa
(Valentino’s syndrome) .
Even in patients with non-bacterial peritonitis (e.g. acute pancreatitis,
intraperitoneal rupture of the bladder or haemoperitoneum), the peritoneum
often becomes infected by transmural spread of organisms from the bowel.
Such translocation is a feature of the systemic inflammatory response on the
bowel .Most duodenal and gastric perforations are initially sterile for up to
several hours before becoming secondarily infected
Paths to peritoneal infection
_
Gastrointestinal perforation, e.g. perforated ulcer, appendix, diverticulum
_
Transmural translocation (no perforation), e.g. pancreatitis, ischaemic bowel
_
Exogenous contamination, e.g. drains, open surgery, trauma
_
Female genital tract infection, e.g. pelvic inflammatory disease
_
Haematogenous spread (rare), e.g. septicaemia
Microbiology
Bacteria from the gastrointestinal tract
The number of bacteria within the lumen of the gastrointestinal tract is normally
low until the distal small bowel is reached. However, disease leading to stasis and
overgrowth (e.g. obstruction, chronic and acute motility disturbances) may
increase proximal colonisation. The biliary and pancreatic tracts are also
normally free from bacteria, although they may be infected in disease, e.g.
gallstones. Peritoneal infection is usually caused by two or more bacterial strains.
Gram-negative bacteria contain
endotoxins (lipopolysaccharides) in their cell walls that have multiple toxic effects
on the host, primarily by causing the release of tumour necrosis factor (TNF) from
host leukocytes.
Systemic absorption of endotoxin may produce endotoxic shock with hypotension
and impaired tissue perfusion. Other bacteria such as Clostridium welchii produce
harmful exotoxins.
Bacteroides are commonly found in peritonitis. These Gram negative, non-
sporing organisms.

These organisms are resistant to penicillin and streptomycin but sensitive to
metronidazole, clindamycin
-
Microorganisms in peritonitis
Gastrointestinal source
_
Escherichia coli
Streptococci
Bacteroides
Clostridium Klebsiella pneumoniae
Other sources
_
Chlamydia trachomatis
_
Neisseria gonorrhoeae
_
Haemolytic streptococci
_
Staphylococcu
_
Streptococcus pneumonia
_
Mycobacterium tuberculosis and other
spp.
_
Fungal infections
Localised peritonitis
Anatomical and pathological factors may favour the
localization of peritonitis.
Anatomical
The greater sac of the peritoneum is divided into (1) the subphrenicspaces, (2) the
pelvis and (3) the peritoneal cavity proper. The last is divided into a supracolic
and an infracolic compartment by the transverse colon and transverse mesocolon,
which deters the spread of infection from one to the other.
When the supracolic compartment overflows, as is often the case when a peptic
ulcer perforates, it does so over the colon into the infracolic compartment or by
way of the right paracolic gutter to the right iliac fossa and hence to the pelvis.
Pathological
The clinical course is determined in part by the manner in
which
adhesions form around the affected organ. Inflamed peritoneum
loses its
glistening appearance and becomes reddened
and velvety. Flakes of fibrin appear and cause loops of intestine to become
adherent to one another and to the parietes. There is an outpouring of serous
inflammatory exudate rich in leukocytes
and plasma proteins that soon becomes turbid; if localization occurs, the turbid
fluid becomes frank pus. Peristalsis is retarded
.
The greater omentum, by enveloping and becoming adherent to inflamed
structures, often forms a substantial barrier to the spread of infection .
Diffuse (generalised) peritonitis
A number of factors may favour the development of diffuse peritonitis:
•
Speed of peritoneal contamination is a prime factor. If an inflamed appendix or
other hollow viscus perforates before localisation has taken place, there will be an
efflux of contents into the peritoneal cavity, which may spread over a large area
almost instantaneously -Perforation proximal to an obstruction or from sudden
anastomotic separation is associated with severe generalised peritonitis and a high
mortality rate.
•
Stimulation of peristalsis by the ingestion of food or even water hinders
localisation. Violent peristalsis occasioned by the administration of a purgative or
an enema may cause the widespread distribution of an infection that would
otherwise have remained localised.
•
The virulence of the infecting organism may be so great as to render the
localisation of infection difficult or impossible.
•
Young children have a small omentum, which is less effective in localising
infection.

•
Disruption of localised collections may occur with injudicious handling, e.g.
appendix mass or pericolic abscess.
•
Deficient natural resistance (‘immune deficiency’) may result from use of drugs
(e.g. steroids), disease (e.g. acquired immune deficiency syndrome (AIDS)) or old
age.
With appropriate treatment, localised peritonitis usually resolves; in about 20 per
cent of cases, an abscess follows. Infrequently, localised peritonitis becomes
diffuse. Conversely, in favourable circumstances, diffuse peritonitis can become
localised, most frequently in the pelvis or at multiple sites within the abdominal
cavity.
Clinical features
Localised peritonitis
The initial symptoms and signs of localised peritonitis
are
those of the underlying condition – usually visceral inflammation (hence
abdominal pain, specific GI symptoms + malaise, anorexia and nausea).
When the peritoneum becomes inflamed, abdominal pain will worsen and,
in general, temperature and pulse rate will rise. The pathognomonic signs
are localized guarding (involuntary abdominal wall contraction to protect
the viscus from the examining hand), a positive ‘release’ sign (rebound
tenderness) and, sometimes, rigidity (involuntary constant contraction of the
abdominal wall over the inflamed parietes).
If inflammation arises under the diaphragm, shoulder tip (‘phrenic’) pain
may be felt as the pain is referred to the C5 dermatome.
In cases of pelvic peritonitis arising from an inflamed appendix in the pelvic
position or from salpingitis, the abdominal signs are often slight; there may
be deep tenderness of one or both lower quadrants alone, but a rectal or
vaginal examination reveals marked tenderness of the pelvic peritoneum.
Diffuse (generalised) peritonitis
Early
Abdominal pain is severe and made worse by moving or breathing. It is first
experienced at the site of the original lesion and spreads outwards from this point.
The patient usually lies still. Tenderness and generalised guarding are found on
palpation when the peritonitis affects the anterior abdominal wall.
Infrequent bowel sounds may still be heard for a few hours but they cease with the
onset of paralytic ileus. Pulse and temperature rise in accord with degree of
inflammation and infection.
Late
If resolution or localisation of generalised peritonitis does not occur, the abdomen
will become rigid (generalised rigidity). Distension is common and bowel sounds
are absent. Circulatory failure ensues, with cold, clammy extremities, sunken eyes,
dry tongue, thready (irregular) pulse and drawn and anxious face
(Hippocratic facies). The patient finally lapses into unconsciousness.
Diagnostic aids
Investigations may elucidate a doubtful diagnosis, but the importance of a
careful history and repeated examination must not be forgotten
.
Bedside

•
Urine dipstix for urinary tract infection
•
ECG if diagnostic doubt (as a cause of
abdominal pain) or cardiac history
.
Bloods
•
Baseline U&E for treatment
•
Full blood count for white cell count
(WCC)
•
Serum amylase estimation may establish the diagnosis of acute
pancreatitis provided that it is remembered that moderately raised
values are frequently found following other abdominal catastrophes
and operations, e.g. perforated duodenal ulcer
.
Imaging
•
Erect chest radiograph to demonstrate free subdiaphramatic gas
•
A supine radiograph of the abdomen may confirm the presence of
dilated gas-filled loops of bowel (consistent with a paralytic ileus),
occasionally show other gas-filled structures that may aid diagnosis,
e.g. biliary tree; the faecal pattern may act as a guide to colonic disease
(absent in sites of
significant inflammation, e.g. diverticulitis). In the patient who is too
ill for an ‘erect’ film, a lateral decubitus film can show gas beneath the
abdominal wall (if CT unavailable).
•
Multiplanar computed tomography (CT) is to identify the cause of peritonitis and
may also influence management decisions, e.g. surgical strategy.
•
Ultrasound scanning has undoubted value in certain situations such as pelvic
peritonitis in females and localized right upper quadrant peritonism.
Invasive
•
peritoneal diagnostic aspiration has little residual value.
Management : General care of the patient
., patients will require some or all of the following
Correction of fluid loss and circulating volume
Patients are frequently hypovolaemic with electrolyte disturbances. The
plasma volume must be restored and electrolyte concentrations corrected.
pre-existent and ongoing fluid losses corrected. Special measures may be
needed for cardiac, pulmonary and renal support, especially if septic shock
is present, including central venous pressure monitoring in patients with
concurrent disease.
Urinary catheterisation ± gastrointestinal decompression
A urinary catheter will give a guide to central perfusion and will be required if
abdominal surgery is to proceed. A nasogastric tube is commonly passed to allow
drainage ± aspiration until paralytic ileus has resolved
.
Antibiotic therapy
Administration of parenteral broad-spectrum (aerobic and anaerobic) antibiotics
prevents the multiplication of bacteria and the release of endotoxins
Analgesia
The patient should be nursed in the sitting-up position and must be relieved of pain
before and after operation.
. Freedom from pain allows early mobilization and adequate physiotherapy in the
postoperative period, which helps to prevent basal pulmonary collapse, deep-vein
thrombosis and pulmonary embolism.
Specific treatment of the cause
While difficult to generalise, in patients where specific treatment has not been
guided by CT scanning, early surgical intervention is to be preferred to a ‘wait
and see’ policy assuming that the patient is fit for anaesthesia and that
resuscitation has resulted in a satisfactory restitution of normal body physiology.
This rule is particularly true for previously healthy patients and those with
postoperative peritonitis. More caution is, of course, required in patients at high
operative risk because of comorbidity or advanced age.
_
Complications of peritonitis
_
Systemic complications
Bacteraemic/endotoxic shock
Systemic inflammatory response syndrome
Multiorgan dysfunction syndrome
Death
_
Abdominal complications
Paralytic ileus
Residual or recurrent abscess/inflammatory mass
Portal pyaemia/liver abscess
Adhesional small bowel obstruction
This rule is particularly true for previously healthy patients and those with
postoperative peritonitis. More caution is, of course, required in patients at high
operative risk because of comorbidity or advanced age.
Primary peritonitis
Primary pneumococcal peritonitis may complicate nephrotic syndrome or
cirrhosis in children. Otherwise healthy children, particularly girls between
three and nine years of age, may also be affected, and it is likely that the
route of infection is sometimes via the vagina and Fallopian tubes. At other
times, and
always in males, the infection is blood-borne and secondary to
respiratory tract or middle ear disease.
.
Clinical features
The onset is sudden and the earliest symptom is pain localized to the lower
half of the abdomen. The temperature is raised to 39°C or more and there is
usually frequent vomiting. After 24–48 hours, profuse diarrhoea is
characteristic. There is usually increased frequency of micturition. The last
two symptoms are caused by severe pelvic peritonitis. On examination,

peritonism is usually diffuse but less prominent than in most cases of a
perforated viscus leading to peritonitis.
Investigation and treatment
A leukocytosis _30 000 μL with approximately 90 per cent polymorphs
suggests pneumococcal peritonitis rather than another cause, e.g.
appendicitis. After starting antibiotic therapy and correcting dehydration and
electrolyte imbalance, early surgery is required unless spontaneous infection
of pre-existing ascites is strongly suspected, in which case a diagnostic
peritoneal tap is useful. Laparotomy or laparoscopy may be used. Should the
exudate be odourless and sticky, the diagnosis of pneumococcal
peritonitis is practically certain, but it is essential to perform a
careful exploration to exclude other pathology. Assuming that
no other cause for the peritonitis is discovered, some of the exudate
is aspirated and sent to the laboratory for microscopy, culture
and sensitivity tests. Thorough peritoneal lavage is carried
out and the incision closed. Antibiotic and fluid replacement
therapy are continued and recovery is usual.
Other organisms are now known to cause some cases of primary
peritonitis in children, including Haemophilus, other streptococci
and a few Gram-negative bacteria. Underlying pathology
(including an intravaginal foreign body in girls) must always be
excluded before primary peritonitis can be diagnosed with certainty.
Idiopathic streptococcal and staphylococcal peritonitis
can also occur in adults.
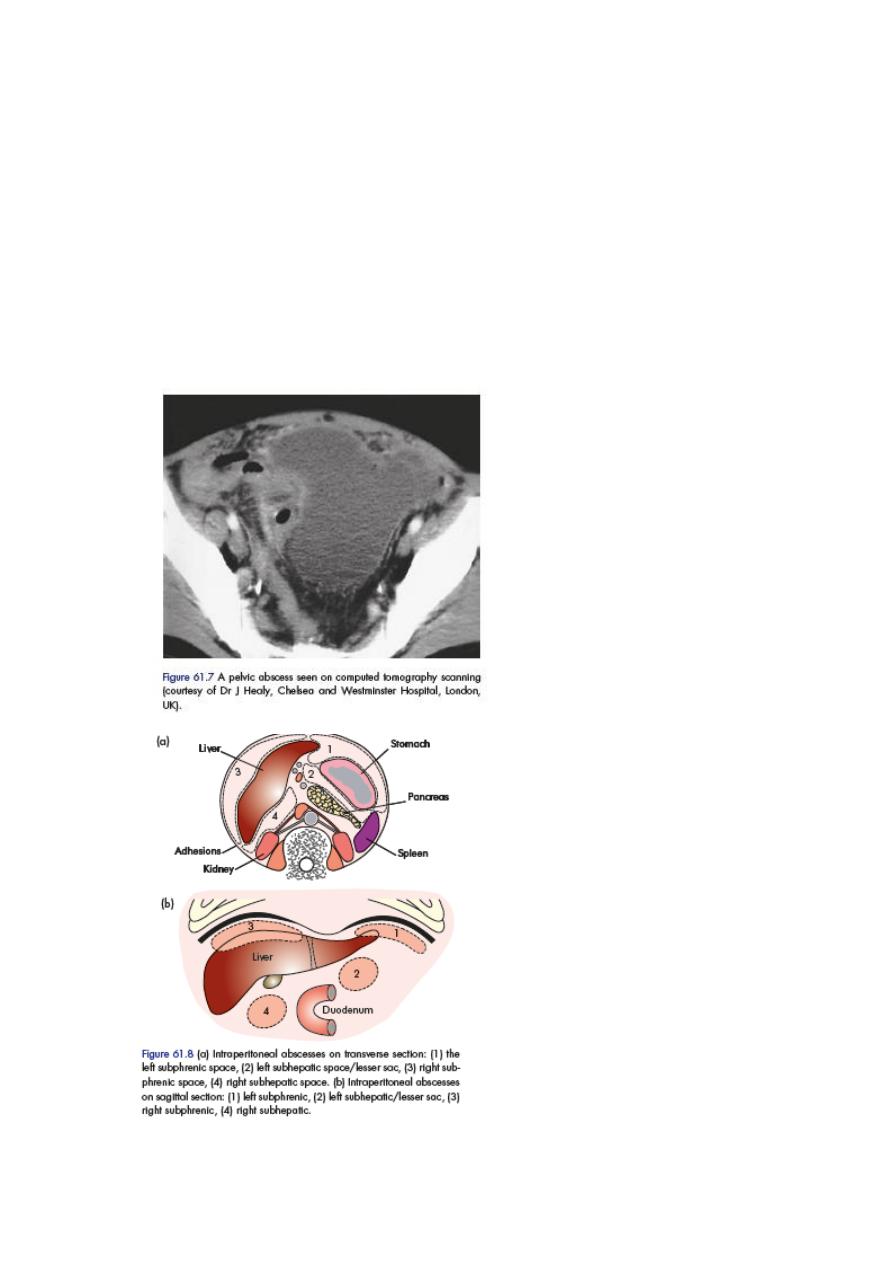
INTRAPERITONEAL ABSCESS
Following intraperitoneal sepsis (usually manifest first as local or diffuse
peritonitis), the anatomy of the peritoneal cavity is such that with the
influence of gravity (depending on patient position – sitting or supine),
abscess development usually occupies one of a number of specific
abdominal or pelvic sites (Figure).
In general, the symptoms and signs of a purulent collection may be vague
and consist of nothing more than lassitude, anorexia and malaise; pyrexia
(often low-grade), mild tachycardia and localised tenderness. Certain sites
have more specific clinical features. Larger abscesses will give rise
to the picture of swinging pyrexia and pulse and a palpable mass.
Blood tests will reveal elevated inflammatory markers
Summary box 61.7
S
Clinical features of an abdominal/pelvic abscess
Symptoms
_
Malaise, lethargy
– failure to recover from surgery as expected
_
Anorexia and weight loss
_
Sweats ± rigors
_
Abdominal/pelvic pain
_
Symptoms from local irritation, e.g. shoulder
tip/hiccoughs
(subphrenic), diarrhoea and mucus (pelvic), nausea and vomiting (any upper
abdominal)
Signs
_
Increased temperature and pulse ± swinging pyrexia
_
Localised abdominal tenderness ± mass (including on pelvic exam
ummary
box 61.9
I
Tuberculous peritonitis
_
Acute (may be clinically indistinguishable from acute
bacterial peritonitis) and chronic forms
_
Abdominal pain, sweats, malaise and weight loss are
frequent
_
Ascites common, may be loculated
_
Caseating peritoneal nodules are common
– distinguish
from metastatic carcinoma and fat necrosis of pancreatitis
_
Intestinal obstruction may respond to antituberculous
treatment without surgery
TUMOURS OF THE PERITONEUM
Primary tumours
Primary tumours of the peritoneum are rare . Mesothelioma of the peritoneum is
less frequent than in the pleural cavity but equally lethal. Asbestos is a recognised
cause. It has a predilection for the pelvic peritoneum.
Chemocytotoxic agents are the mainstay of treatment.
Secondary tumours
Carcinomatosis peritonei
This is a common terminal event in many cases of carcinoma of the stomach,
colon, ovary or other abdominal organs and also of the breast and bronchus. The
peritoneum, both parietal and
visceral, is studded with secondary growths and the peritoneal cavity becomes
filled with clear, straw-coloured or blood-stained ascitic fluid.
The main forms of peritoneal metastases are:
•
discrete nodules – by far the most common variety;
•
plaques varying in size
and colour;
•
diffuse adhesions – this form occurs at a late stage of the disease
and gives rise, sometimes, to a ‘frozen pelvis’.
The main differential diagnosis is from tuberculous peritonitis (tubercles are
greyish and translucent and closely resemble the discrete nodules of peritoneal
carcinomatosis).
Investigation and treatment are as for underlying malignancy.
Pseudomyxoma peritonei
This rare condition occurs more frequently in women. The abdomen is filled with
a yellow jelly, large quantities of which are often encysted. The condition is
associated with mucinous
cystic tumours of the ovary and appendix. Recent studies suggest
that most cases arise from a primary appendiceal tumour with
secondary implantation on to one or both ovaries. It is often
painless and there is frequently no impairment of general
health
, the diagnosis is more often suggested by ultrasound
and CT scanning or made at operation. At laparotomy, masses
of jelly are scooped out. The appendix, if present, should be
excised together with any ovarian tumour.
