Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
1
Dyspnea;
Defined as a subjective feeling of an uncomfortable awareness of breathing. It
is a cardinal symptom of cardiopulmonary diseases.
Tachypnea;
Defined as a sign of increased work of breathing (rapid breathing).
Acute dyspnea; (over a period of minutes to days)
Chronic dyspnea; (over months to years)
Mechanisms of dyspnea;
dyspnea results from;
A- Increase work of breathing;
1. Stimulation of intrapulmonary sensory nerves e.g. pneumothorax,
interstitial inflammation.
2. Air flow obstruction e.g. asthma, COPD.
3. Decrease lung compliance e.g. pulmonary odema, pneumonia,
pneumothorax, pulmonary Fibrosis.
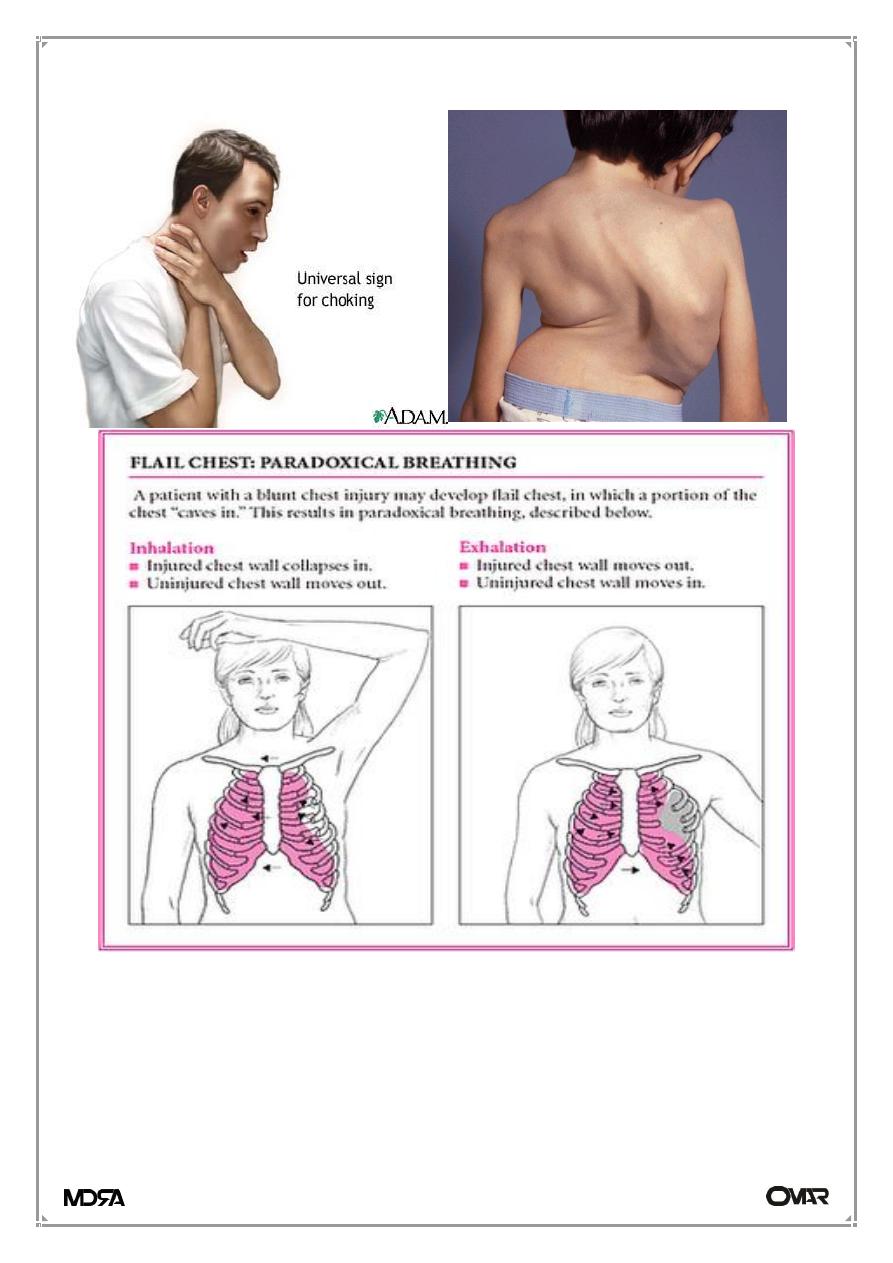
4. Restricted chest expansion e.g. Ankylosing spondylitis, respiratory muscle
paralysis, kyphoscoliosis.
B- Increase ventilatory drive; stimulation of respiratory centers.
1. Increase arterial H+; metabolic Acidosis.
2. Increase arterial PCO2; hypercapnia.
3. Decrease arterial PO2; hypoxia.
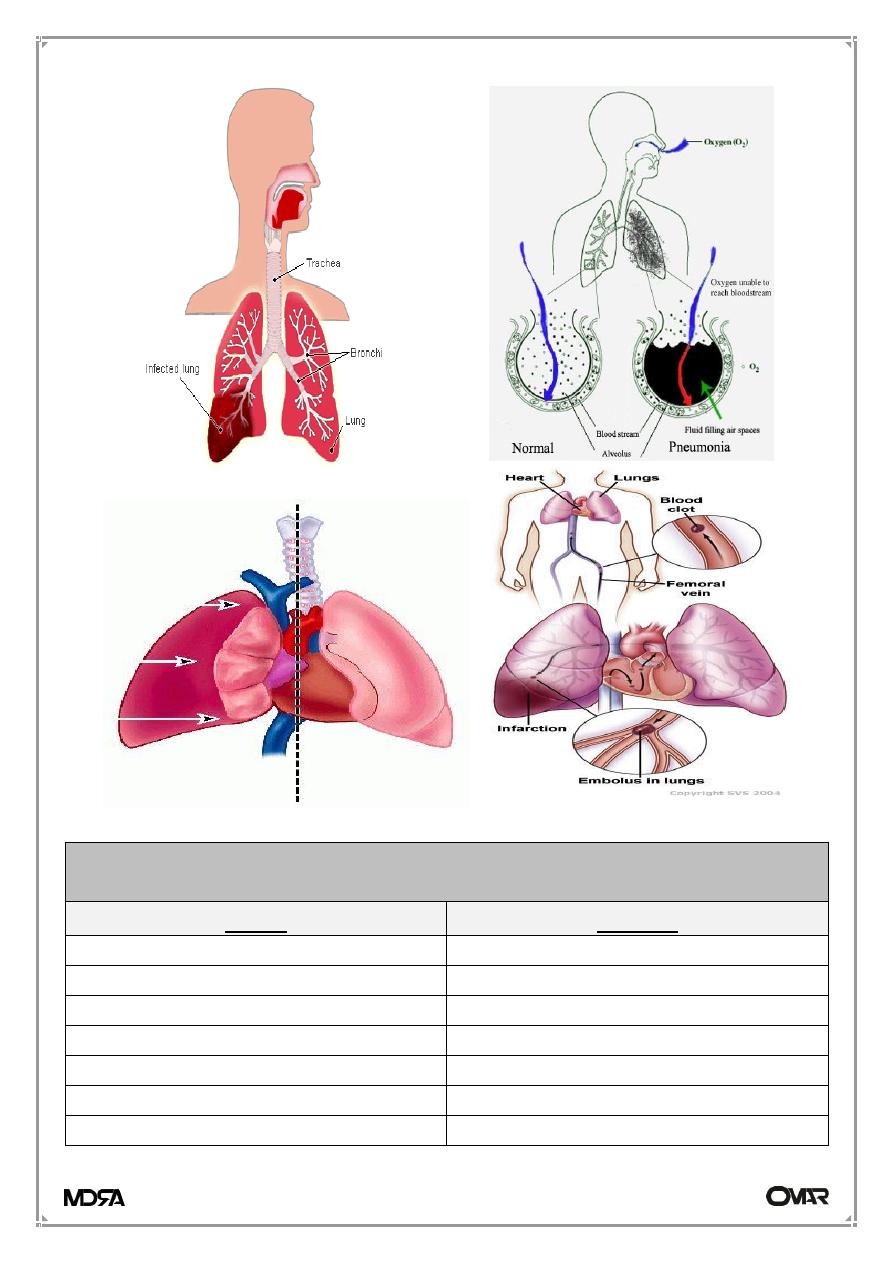
4. Ventilation-perfusion mismaching; pulmonary embolism.
5. Increase central arousal; exercise, anxiety, thyrotoxicosis.
Clinical pattern of dyspnea
1-Exertional dyspnea
2-Orthopnea
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
2
3-Paroxysmal nocturnal dyspnea
4-Dyspnea at rest
5-Chyen-Stokes breathing
6-Hyperventilation(kussmaul breathing)
1-Exertional dyspnea;
It occur at exercise level below that expected for patient age and previous
fitness, occur in both respiratory and cardiac diseases.
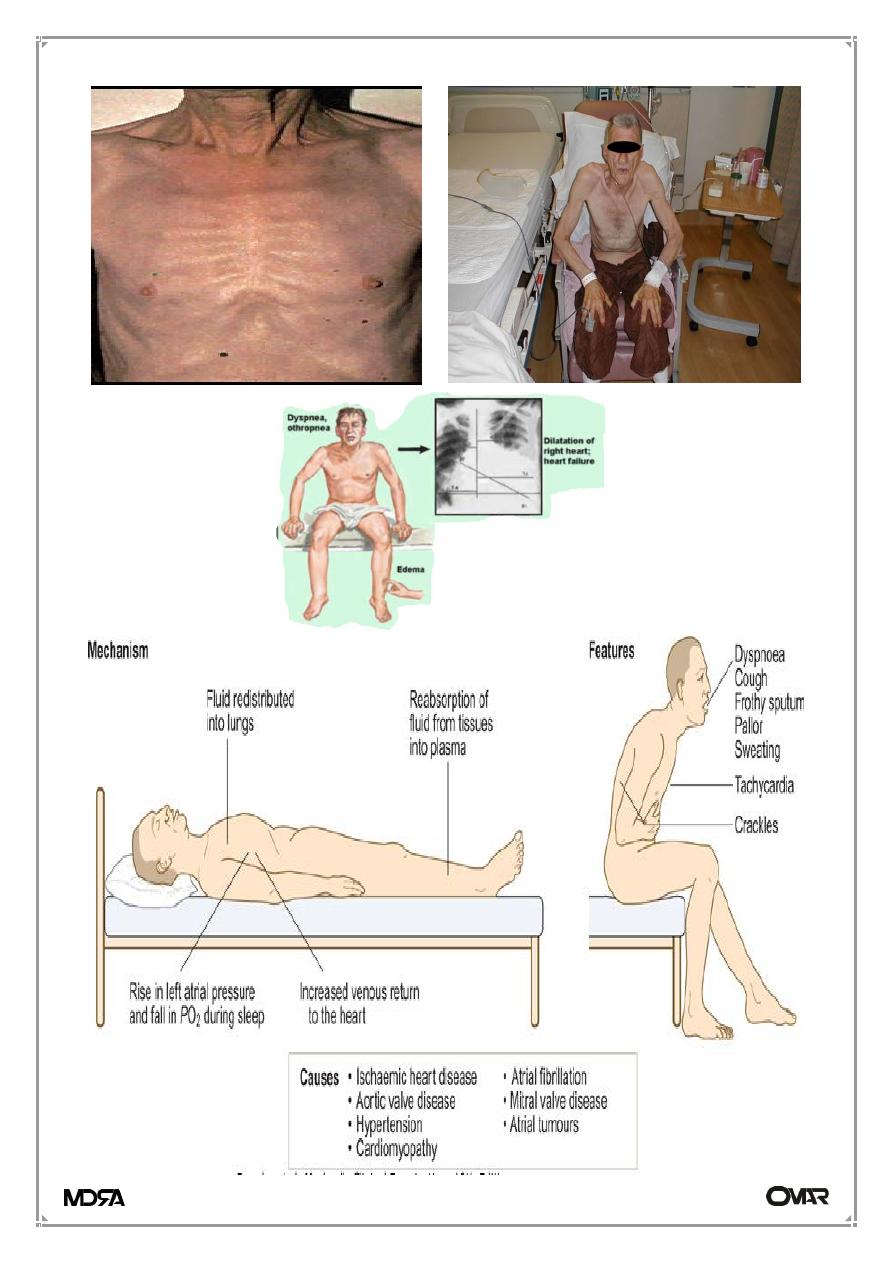
2-Orthopnea;
Dyspnea on lying flat (supine position) due to increase venous return to the
heart, usually occur in patient with heart failure.
3-Paroxysmal nocturnal dyspnea;
Is an acute, sever breathlessness that wake the patient from sleep, to sit
upright position, gasping in bed, he try to open the windows in an attempt to
relieve the distress, associated with cough and frothy sputum, due to fluid shift
from peripheral tissue to the circulation within 1-2 hours of sleep, occur in
heart failure.
4-Dyspnea at rest;
Dyspnea even at sitting position which may indicates sever respiratory or
cardiac diseases.
5-Chyen-Stokes breathing;
Is a cyclical variation in the depth of breathing with overventilation alternating
with period of cessation of breathing (apnea), due to impaired responsiveness
of respiratory centers to CO2, may occur in brain stem stroke or heart failure.
6-Hyperventilation (kussmaul breathing);
It is a rapid, deep breathing at a regular rate, as a response to reduced arterial
PH in metabolic acidosis.
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
3
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
4
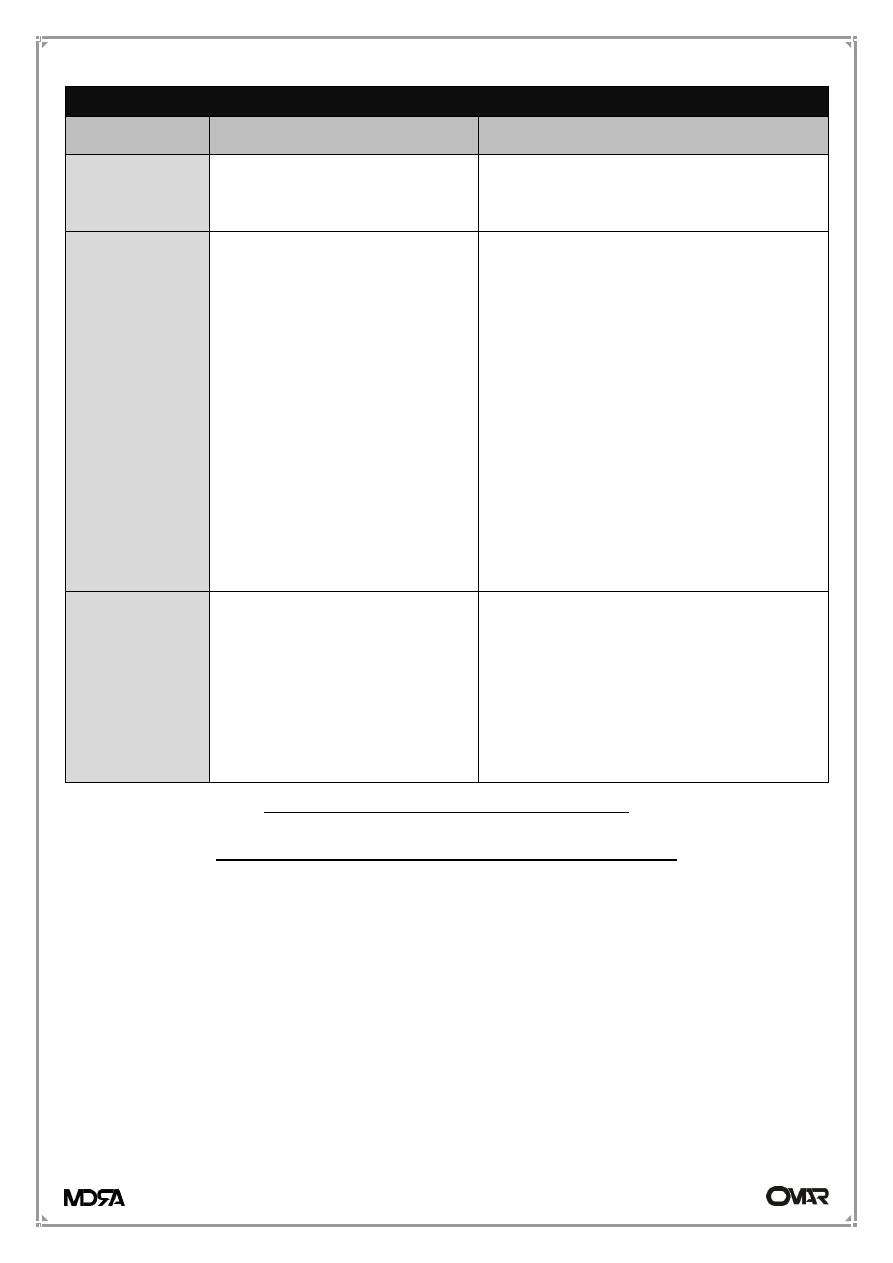
CAUSES OF DYSPNOEA
Acute dyspnoea at rest
Chronic exertional dyspnoea
Cardiovascular
Acute pulmonary oedema
Chronic heart failure, Myocardial
ischaemia (angina equivalent)
Respiratory
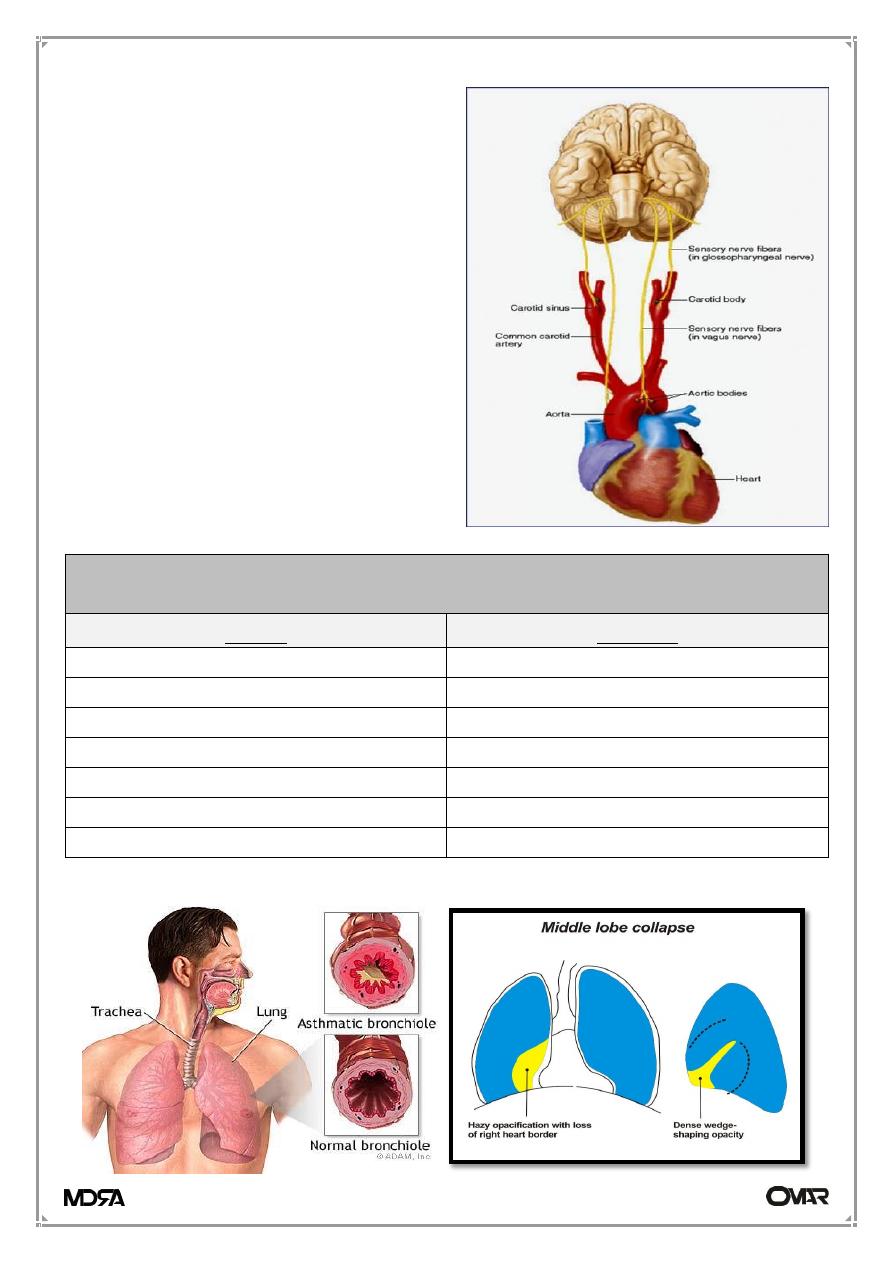
* Acute severe asthma
* Acute exacerbation of
COPD
* Pneumothorax
* Pneumonia
* Pulmonary embolus
Acute respiratory distress
syndrome
Inhaled foreign body
(especially in the child)
Lobar collapse
Laryngeal oedema (e.g.
anaphylaxis)
* COPD
* Chronic asthma
Bronchial carcinoma
Interstitial lung disease (sarcoidosis,
fibrosing alveolitis, extrinsic allergic
alveolitis, pneumoconiosis)
Chronic pulmonary thromboembolism
Lymphatic carcinomatosis (may cause
intolerable dyspnoea)
Large pleural effusion(s)
Others
Metabolic acidosis (e.g.
diabetic ketoacidosis, lactic
acidosis, uraemia, overdose
of salicylates, ethylene glycol
poisoning)
Psychogenic hyperventilation
(anxiety or panic-related)
Severe anaemia
Obesity
Grading the degree of a dyspnea
New York heart association score (NYHA)
There are four functional grades of dyspnea as follows:
Grade I: Dyspnea on running or on doing more than ordinary effort e.g.
climbing stairs, but occur at exercise level below that expected for patient age
and previous fitness.
Grade II: Dyspnea on doing ordinary effort.
Grade III: Dyspnea on doing less than ordinary effort e.g. walking short
distances (20–100 m). Comfortable only at rest.
Grade IV: Dyspnea at rest.
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
5
The important questions to patients with dyspnea includes:
• Mode of onset, duration and progression
• Variability and aggravating/relieving factors
• Severity
• Associated symptoms: e.g. chest pain, cough, wheeze
------------------------------------------------------------------------------------------
RESPIRATORY FAILURE
The term is used when pulmonary gas exchange fails to maintain normal
arterial oxygen and carbon dioxide levels.
Normal arterial blood gases levels =
PaO
2
= 12 - 15 kPa (90 - 113 mmHg)
PaCO
2
= 4.5 - 6 kPa (35 - 45 mmHg)
HCO3 = 22 - 26 mEq/liter
pH = 7.35 - 7.45
Oxygen saturation > 97 %
Classification
Its classified into types I and II relates to the absence or presence of
hypercapnia (raised PaCO
2
).
• Type I (Hypoxemic) respiratory failure;
characterized by Hypoxia PaO
2
< 8.0 kPa (60 mmHg) with normal or low
PaCO
2
< 6.6 kPa (50 mmHg).
• Type II (Hypercapnic) respiratory failure;
characterized by Hypoxia PaO
2
< 8.0 kPa (60 mmHg) and Raised PaCO
2
>
6.6 kPa (50 mmHg).
Acute respiratory failure; develop over minutes or hours.
Chronic respiratory failure; develop over days or longer.
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
6
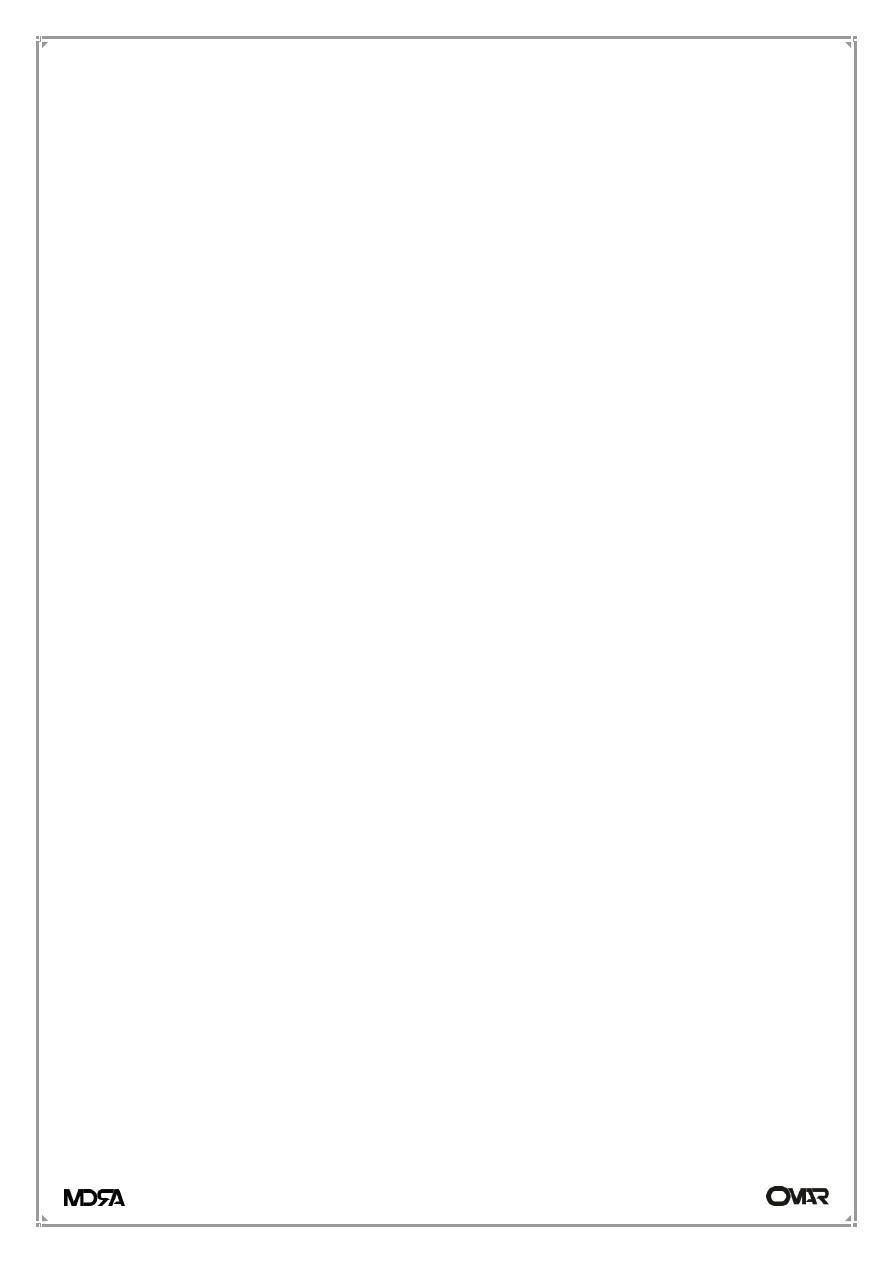
Respiratory chemoreceptors;
1-Peripheral
chemoreceptors;
located in the aorta and carotid
arteries ,respond to change in CO2,
O2 and PH, in blood.
2-Central chemoreceptors; located
in medulla oblongata respond to
change in CO2,and PH but not O2,
in CSF.
Type I
Hypoxia (PaO
2
< 8.0 kPa (60 mmHg)) Normal or low PaCO
2
(< 6.6 kPa (50 mmHg))
acute
chronic
Acute asthma
Emphysema
Pulmonary oedema
Lung fibrosis
Pneumonia
Lymphangitis carcinomatosa
Lobar collapse
Right-to-left shunts
Pneumothorax
Brain-stem lesion
Pulmonary embolus
ARDS
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
7
Type II
Hypoxia (PaO
2
< 8.0 kPa (60 mmHg)) Raised PaCO
2
(> 6.6 kPa (50 mmHg))
acute
chronic
Acute severe asthma
COPD
Acute exacerbation COPD
Sleep apnoea
Upper airway obstruction
Kyphoscoliosis
Acute neuropathies/paralysis
Myopathies/muscular dystrophy
Narcotic drugs
Ankylosing spondylitis
Primary alveolar hypoventilation
Flail chest injury
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
8
Clinical evaluation
1- Initial assessment;
• Assessment of conscious level (response to commands, ability to cough)
• Measurement of respiratory rate, depth and pattern of breathing.
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
9
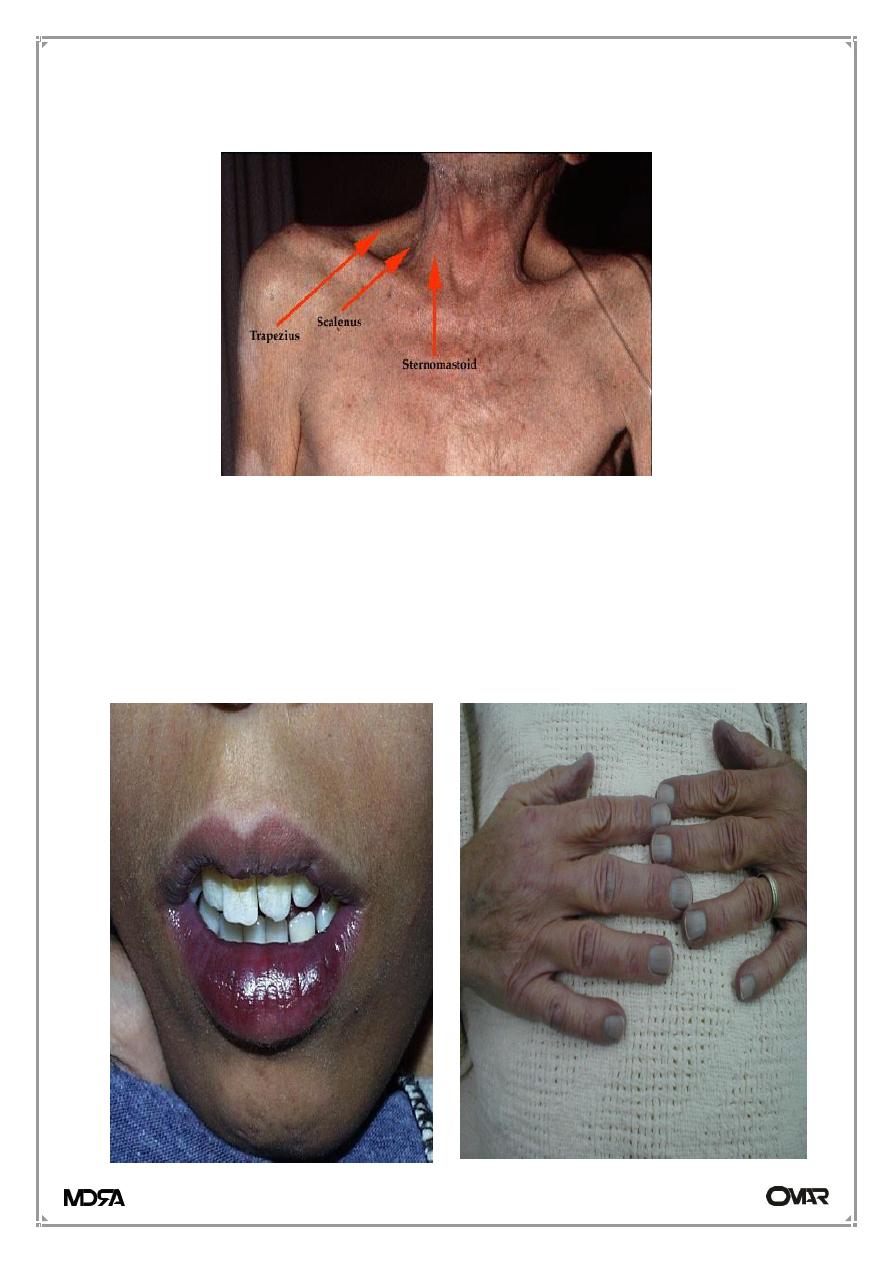
• Signs of respiratory distress; flaring of nostrils, pursed lips breathing, use
accessory muscles of respiration and observed chest wall movement.
• Signs of sever hypoxemia; cyanosis, systemic hypotension, pulmonary
hypertension, polycythemia, tachycardia, and cerebral dysfunction.
• Signs of CO2 retention; warm periphery, bounding pulses, flapping
tremor.
• Signs of cor pulmonale; peripheral oedema, raised JVP, hepatomegaly,
ascites.
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
11
Note; Cor pulmonale; is defined as dilation and hypertrophy of the right
ventricle (RV) in response to diseases of the pulmonary vasculature and/or lung
parenchyma.
• History of chest trauma:
flail chest, ARDS, or pneumothorax.
• Auscultation over chest;
No air entry: pneumothorax
Expiratory ronchi, prolong expiratory phase: airway obstruction.
Bronchial breathing: pneumonia, lung collapse or lung fibrosis.
Crepitation: pneumonia, pulmonary odema, or brochiactaesis.
• Pulse oximetry;
It is a rapid and simple way for detection of blood oxygen content but not CO
2
.
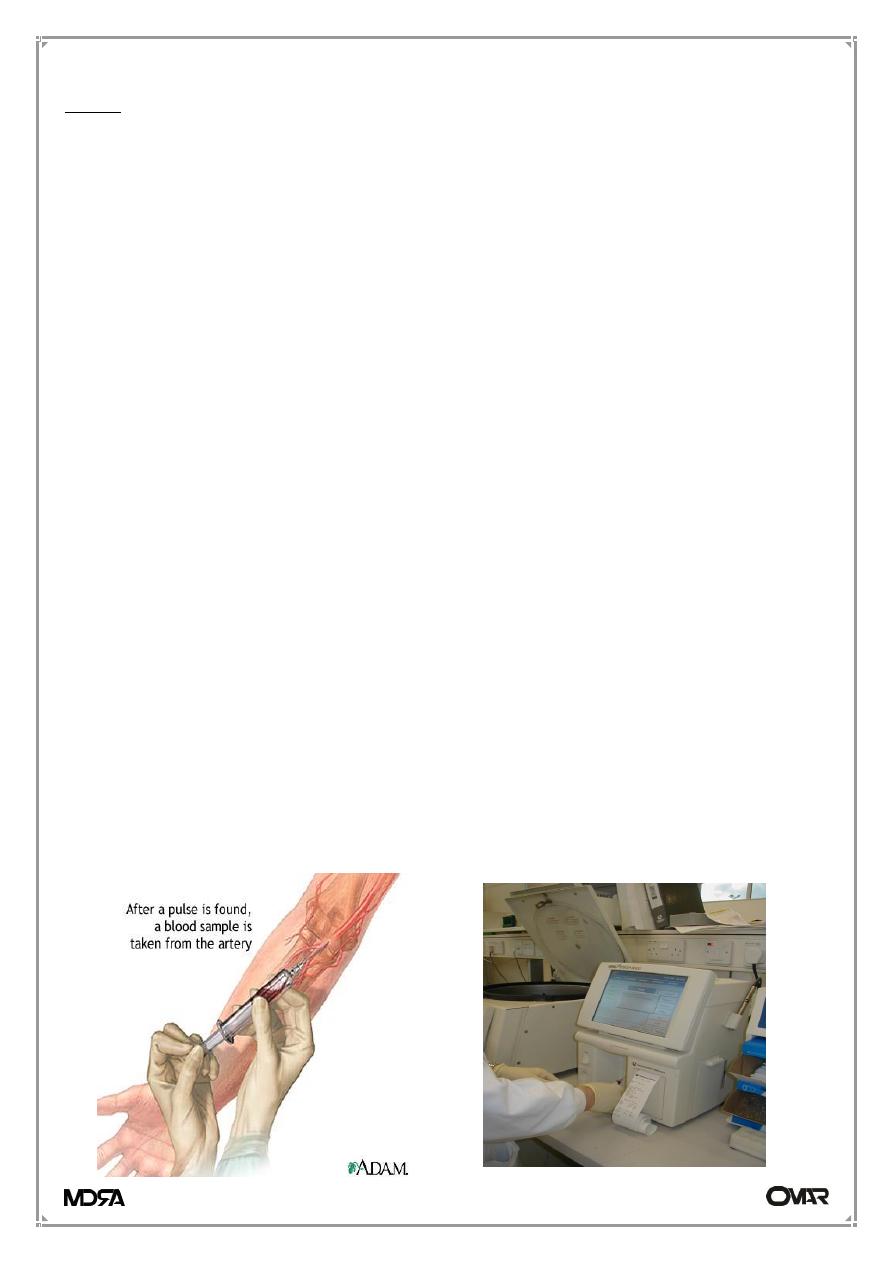
Investigations
1. Arterial blood gases (severity of hypoxaemia, hypercapnia, acidaemia,
bicarbonate)
2. Pulse oximetry
3. Chest X-ray
4. Others; depend on the causes of respiratory failure, e,g. pulmonary function
test.
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
11
Management
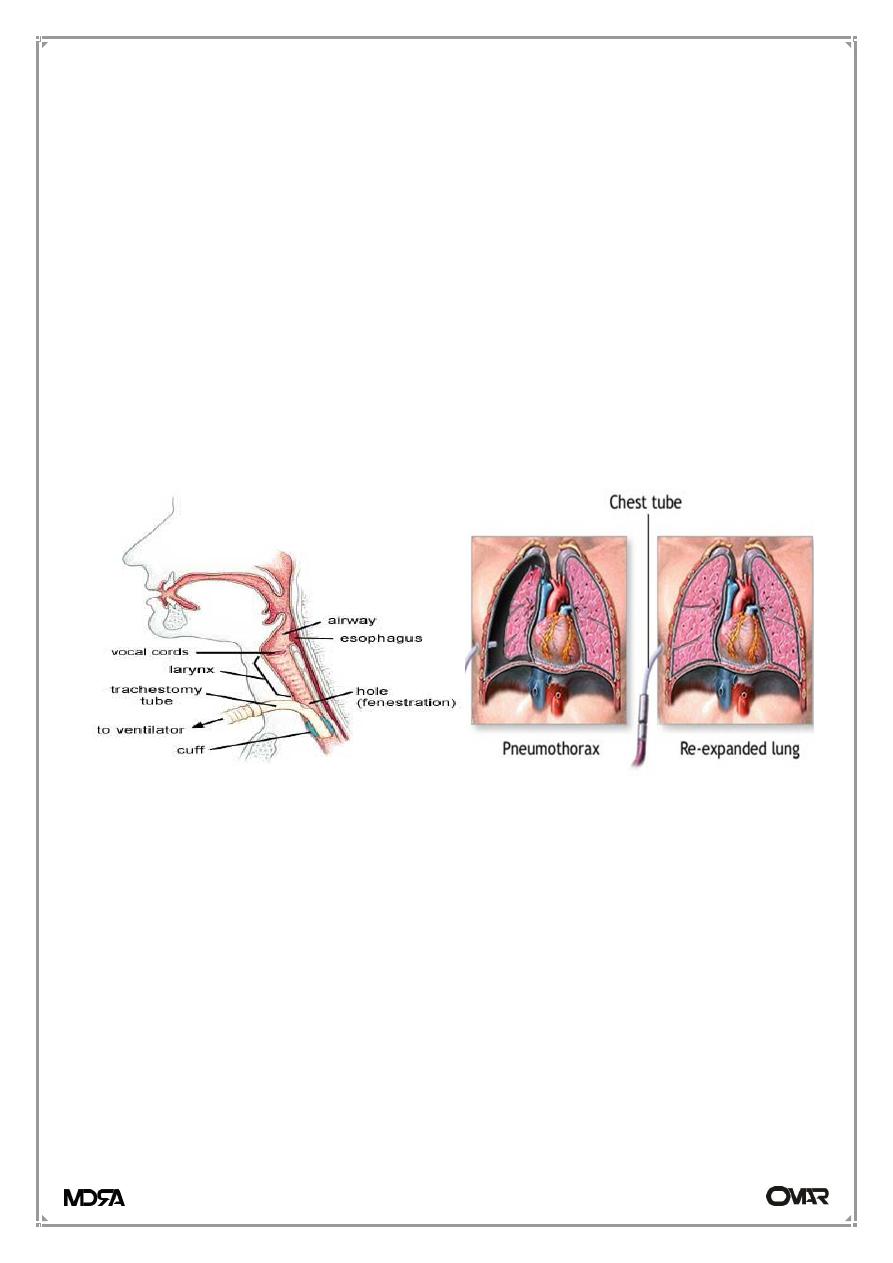
1- Maintenance of airway
2- Treatment of specific precipitating cause;
• Tracheostomy for laryngeal obstruction.
• Fixation of ribs for flail chest injury.
• Reversal of narcotic drugs poisons.
• Nebulised bronchodilators for bronchospasm.
• Chest tube for tension pneumothorax.
• Opiates for sever chest pain.
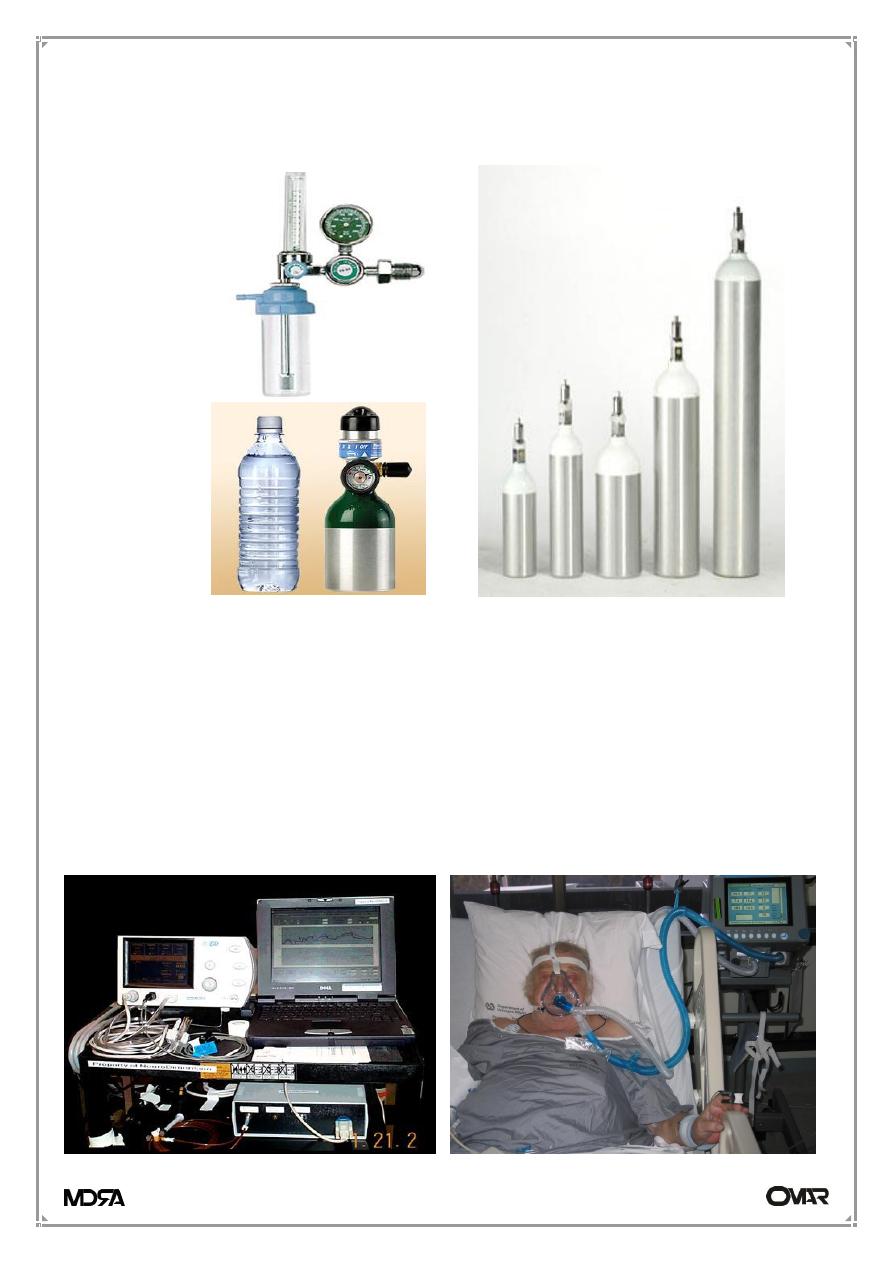
3- Oxygen therapy
For all types of respiratory failure to restore adequate Oxygen level.
Administration of oxygen; Oxygen should always be prescribed in writing with
clearly specified flow rates or concentrations.
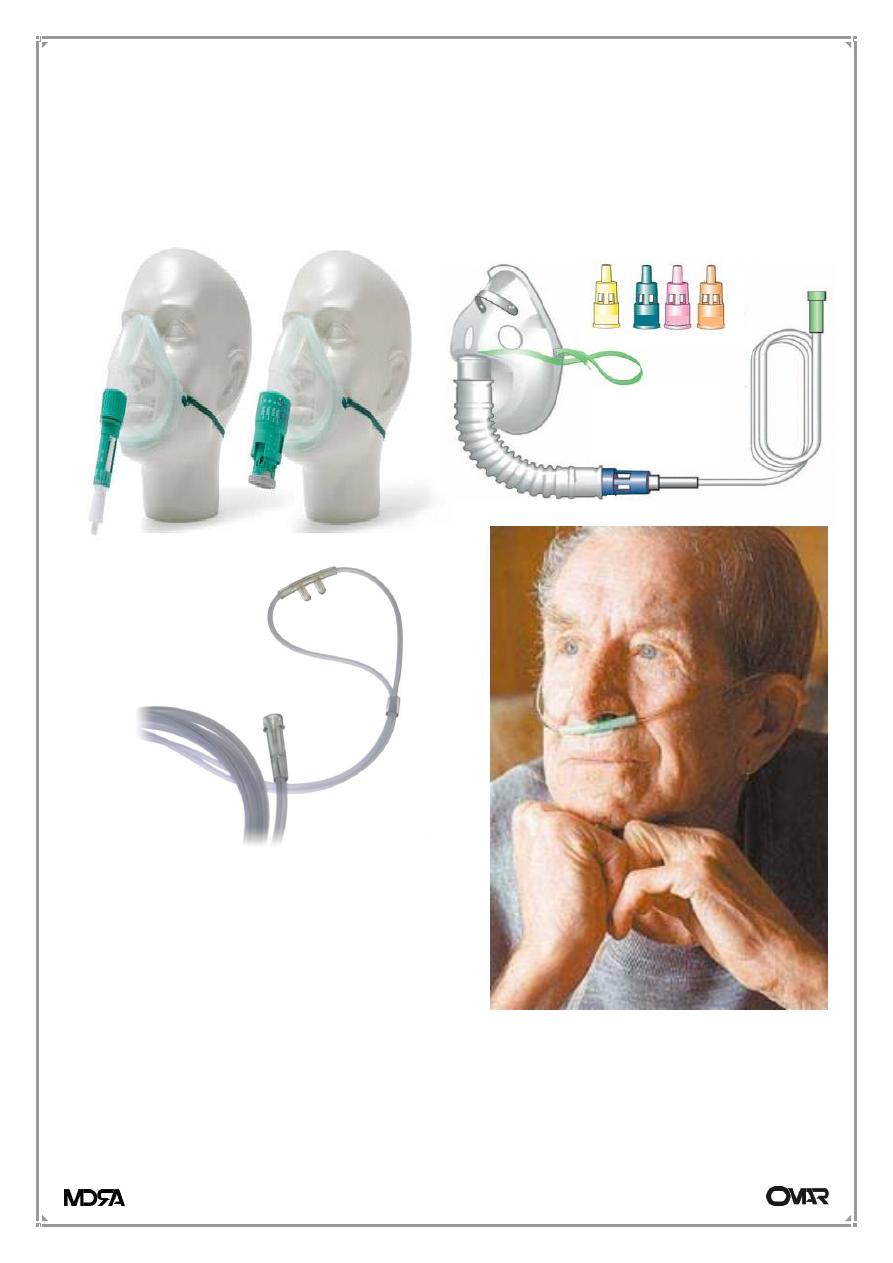
1-High concentrations; Such as 40-60% oxygen via a high-flow mask, are
particularly useful in acute type I respiratory failure such as commonly occurs
in pneumonia, asthma or pulmonary oedema. When high-flow masks are used
for prolonged periods, the oxygen should be humidified by passing it over
warm water.
2-Low concentrations; Venturi masks (24% or 28%) are the most accurate
method of delivering controlled oxygen therapy in type II respiratory failure.
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
12
However, once patients are stable, if a low concentration of oxygen is required
continuously for more than a few hours, 1-2 liters per minute delivered via
nasal cannula allows patients to eat and to undergo physiotherapy etc. while
continuing to receive oxygen.
3-Chronic oxygen delivery
From cylinders delivered to the home, from an oxygen concentrator, is often
given via a low-concentration mask or nasal cannula. Portable oxygen may
increase exercise tolerance in some patients with chronic hypoxic lung disease,
O2 can be administered by nasal
prongs or nasal cannula, which are
generally well tolerated and allow
the patient to cough, speak, eat,
and drink while receiving O2
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
13
and lightweight portable cylinders with oxygen-sparing devices may allow
previously housebound patients to resume outdoor activities.
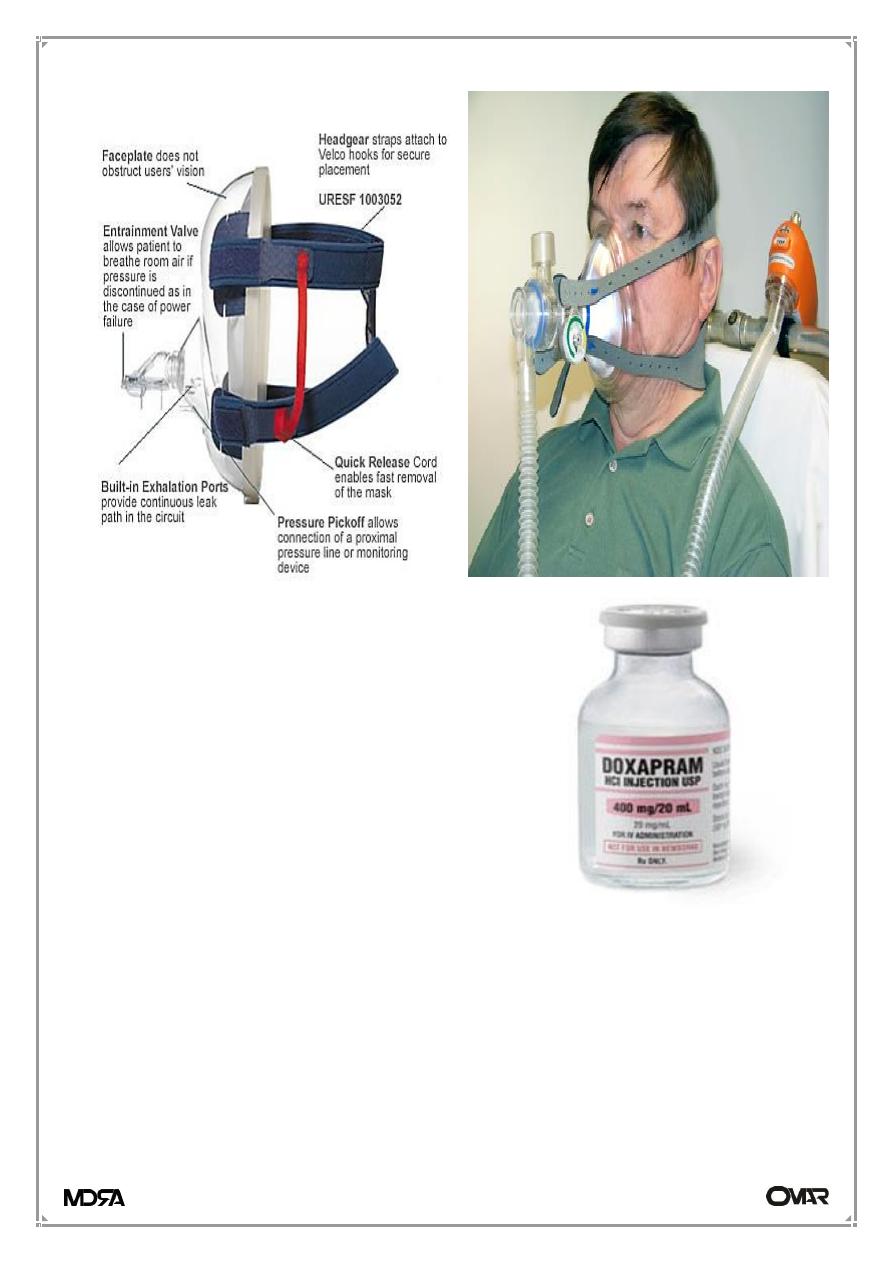
4- Mechanically assisted ventilation
Patients with initially severe respiratory failure (type I or type II) or those who
fail to improve despite optimal medical therapy may require mechanical
ventilation.
The various types of
Non-invasive (via a face or nasal mask) or
Invasive (via an endotracheal tube) ventilation.
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
14
5- Doxapram;
(1.5- 4 mg/min) by slow intravenous infusion
should only be used as a respiratory stimulant
where non-invasive ventilation is not available
or is poorly tolerated, or in those with reduced
respiratory drive. Even in these circumstances
this agent provides only minor and transient
improvements
in
arterial
blood
gas
parameters.
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
15
Cyanosis
Cyanosis refers to a bluish color of the skin and mucous membranes resulting
from an increased quantity of reduced hemoglobin in the small blood vessels
of those areas. It is usually most marked in the lips, nail beds, ears, and malar
eminences.
In general, cyanosis becomes apparent when the concentration of reduced
hemoglobin in capillary blood exceeds 40 g/L (4 g/dL).
therefore, patients with severe anemia may not display cyanosis. Conversely
patients with marked polycythemia tend to be cyanotic at higher levels of Sa
O2
than patients with normal hematocrit values.
Cyanosis may be subdivided into:
1. In the central cyanosis, the Sa
O2
is reduced or an abnormal hemoglobin
derivative is present, and the mucous membranes and skin are both
affected.
2. Peripheral cyanosis is due to a slowing of blood flow and abnormally great
extraction of O
2
from normally saturated arterial blood. It results from
vasoconstriction and diminished peripheral blood flow, such as occurs in
cold exposure, shock, and peripheral vascular disease.
Causes of Cyanosis
Central Cyanosis
1. Decreased arterial oxygen saturation: extensive pneumonia or pulmonary
edema or emphysema. Decreased atmospheric pressure—high altitude.
Alveolar hypoventilation. pulmonary ventilation/perfusion mismatch.
2. Anatomic shunts: Certain types of congenital heart disease like TOF.
Pulmonary arteriovenous fistulas
3. Hemoglobin abnormalities: Methemoglobinemia. Sulfhemoglobinema.
Carboxyhemoglobinemia.
Peripheral Cyanosis
1. Reduced cardiac output
Dr. Hasan
DYSPNOEA - RESPIRATORY FAILURE & CYANOSIS
Internal Medicine
16
2. Cold exposure
3. Arterial obstruction as with an embolus, or cold-induced vasospasm
(Raynaud's phenomenon)
4. Venous obstruction as in thrombophlebitis
The combination of central cyanosis and clubbing is seen in:
• Congenital heart disease and right-to-left shunting like TOF.
• Pulmonary disease such as lung abscess or pulmonary arteriovenous
fistulae.
