Orthognathic Surgery
Orthognathic surgery:Surgery to treat facial disproportion or surgery for correction of dentofacial deformities Orthognathic comes from the Greek orthos (straight) and gnathos (jaw).
Dentofacial deformities could be congenital or acquired. Malocclusion and associated abnormalities of the skeletal components of the face can occur as a result of a variety of factors, including inherited tendencies, prenatal problems, systemic conditions that occur during growth, trauma, and environmental influences
Treatment objectives:
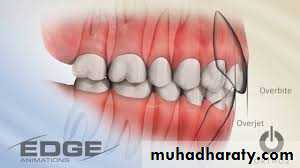
Function: to establish a functional occlusion aiming to achieve normal overbite/overjet and transverse relationships.Aesthetics: to normalize facial balance and proportions in three dimensions, in addition to provide stable results in the long-term.
• Other possible benefits:
Temporo-mandibular joint dysfunction..?Mouth opening
Sleep apnoca
Traumatic occlusions and dental health
The management protocol for facial deformity should comprise the:
HistoryClinical examination
Investigations
Initial diagnose
Treatment plan
Pre-surgical orthodonticsSurgery
Post-surgical orthodontics
When appropriate, restorative dentistry, psychological intervention or support and speech therapy will be required.
Clinical examination
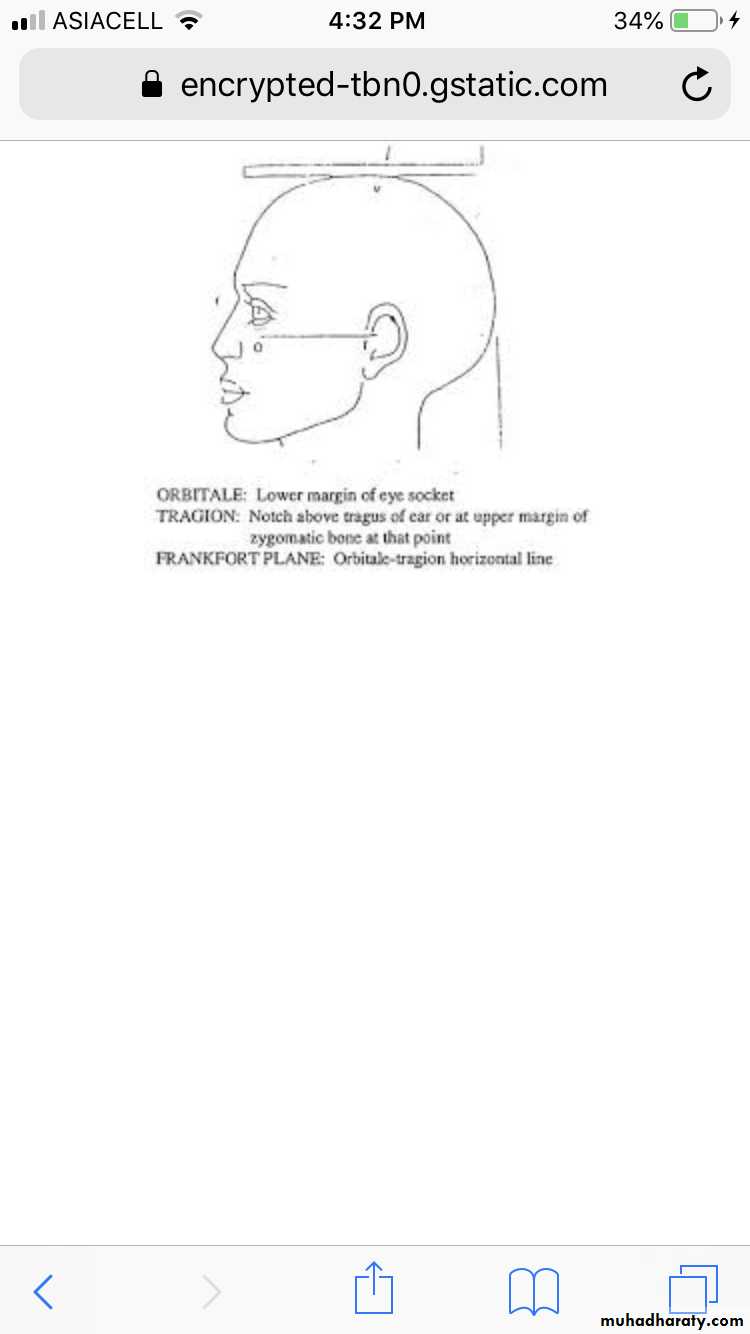
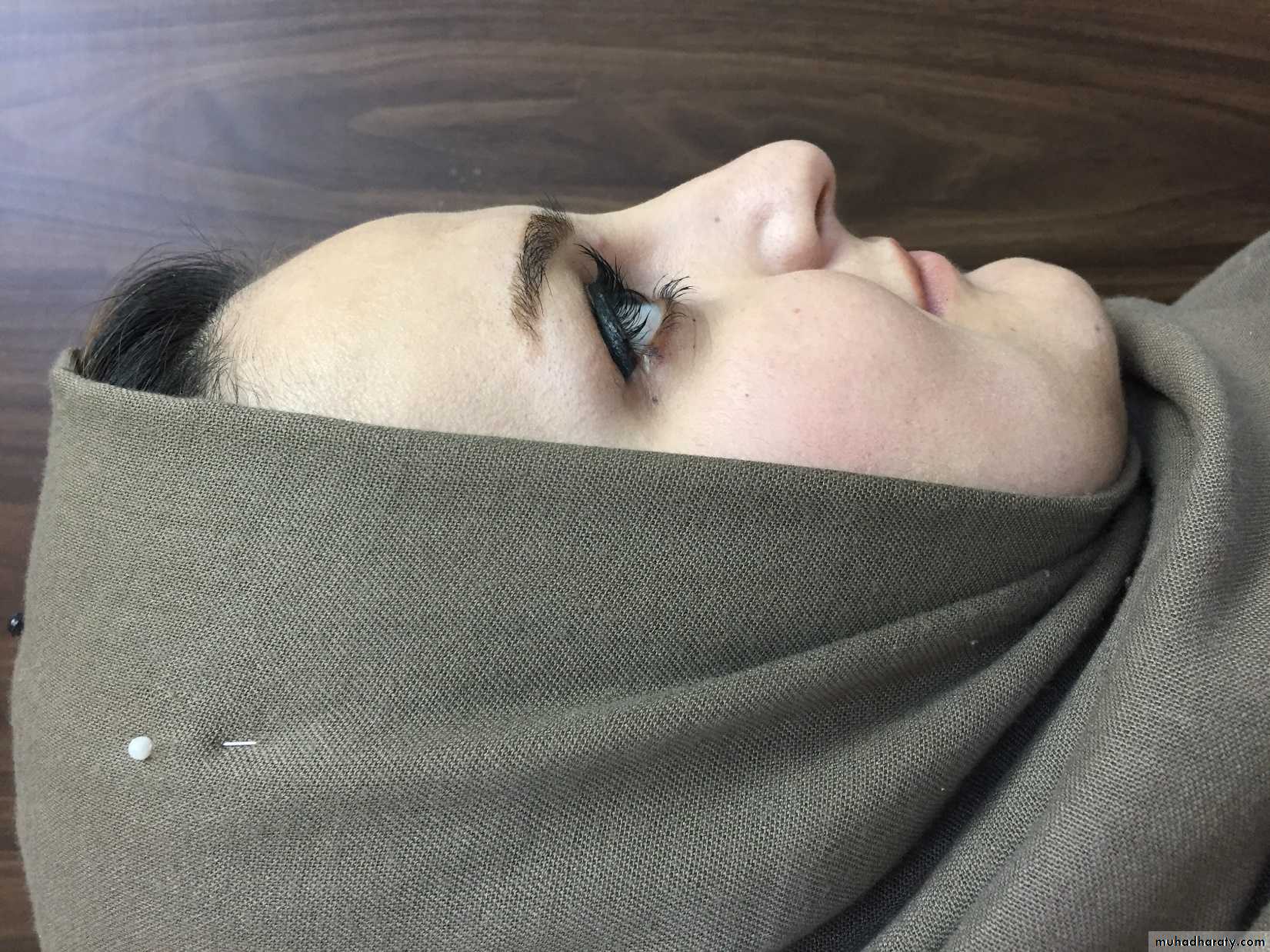
The patient is best assessed sitting upright in good light with head in the natural head position and the Frankfort horizontal parallel to the floor.
Facial evaluation
It is a critical point to remember that facial evaluation is not the search fordeviation from the norm of a single facial unit but the search for proportion
(e.g. a face that is vertically excessive means that, in relation to the transverse
dimension, the face is excessively long and not that it is longer than another
face. By increasing only the vertical dimension facial harmony is lost, but by
increasing both transverse and vertical dimensions harmony is restored.
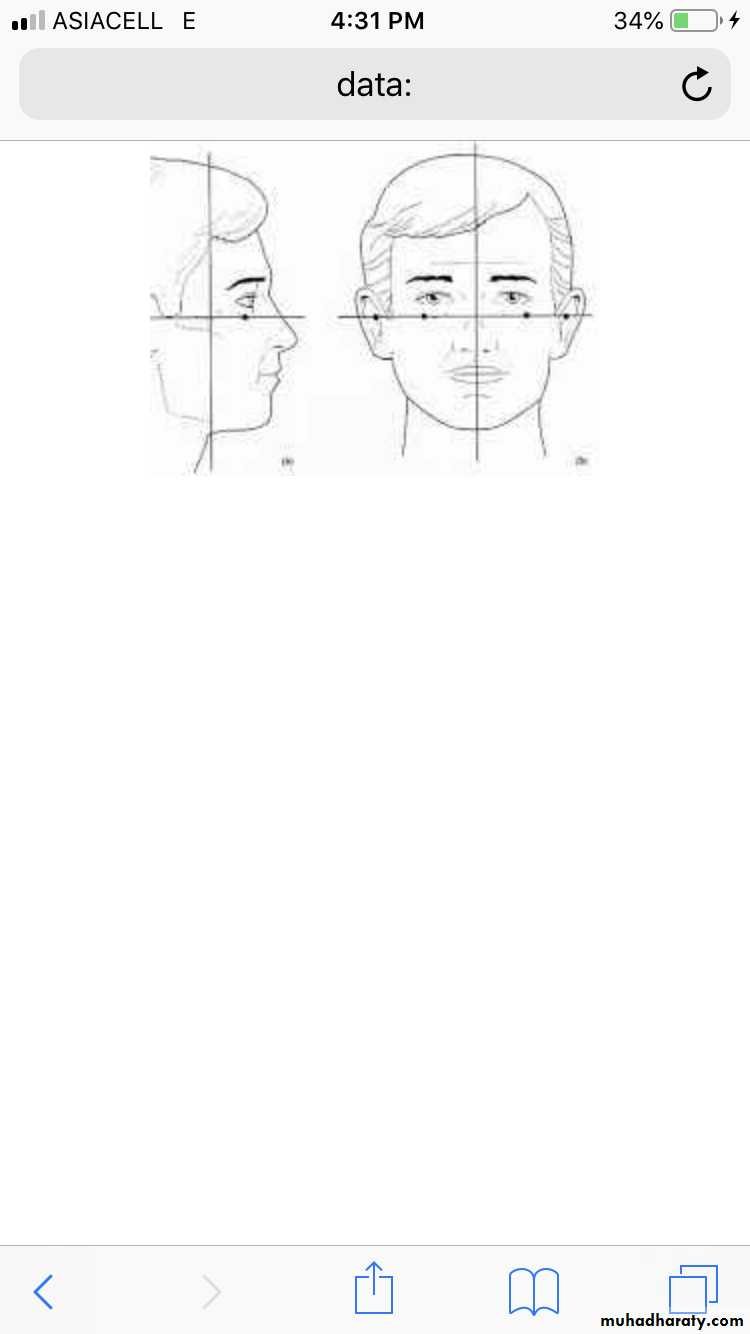
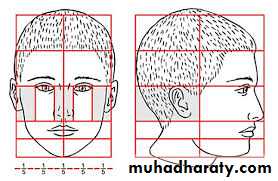
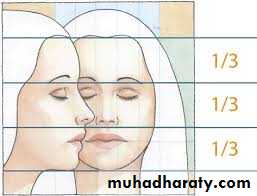
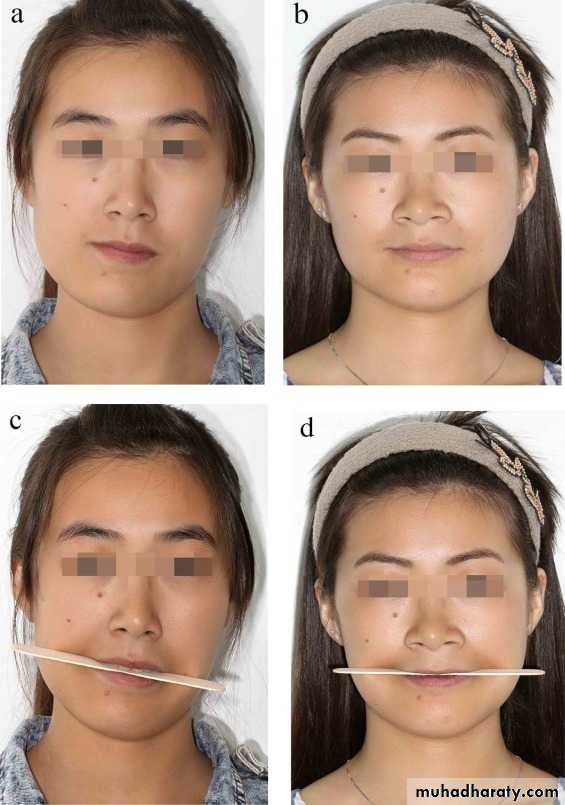
• Frontal view .
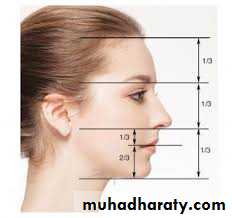
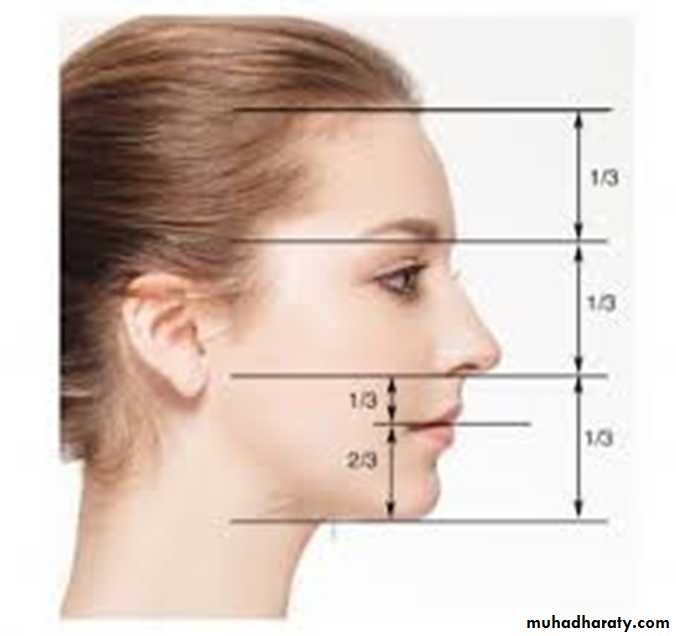
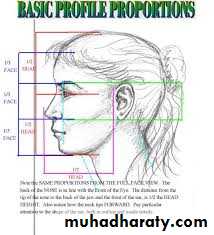
• Facial proportions: The facial height is divided in three main thirds.The :• upper facial third goes from the hairline to the glabella. the middlethird from the glabella to the base of the columella, and the lower thirdfrom the columella to the deepest point of the chin prominence.The lower third is subdivided in to one upper third from the columella base to the lip commissure and two lower thirds from the lower lip to thechin .
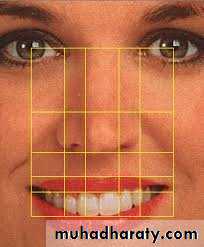
• Special attention should be given to the presence of a gummysmile as well as the symmetry of the smile.
The amount of gingival exposure when smiling and the amount of upper incisor exposure under the upper lip in repose should be correlated. Ideally the upper lip vermillion should fall at the cervico- gingival margin with no more than 2 mm of gingival exposure during smiling.
Facial form:
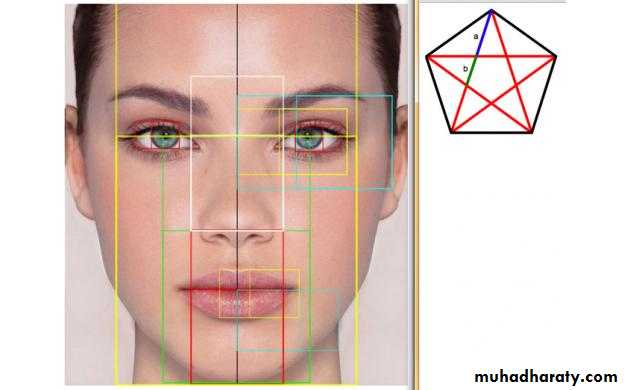
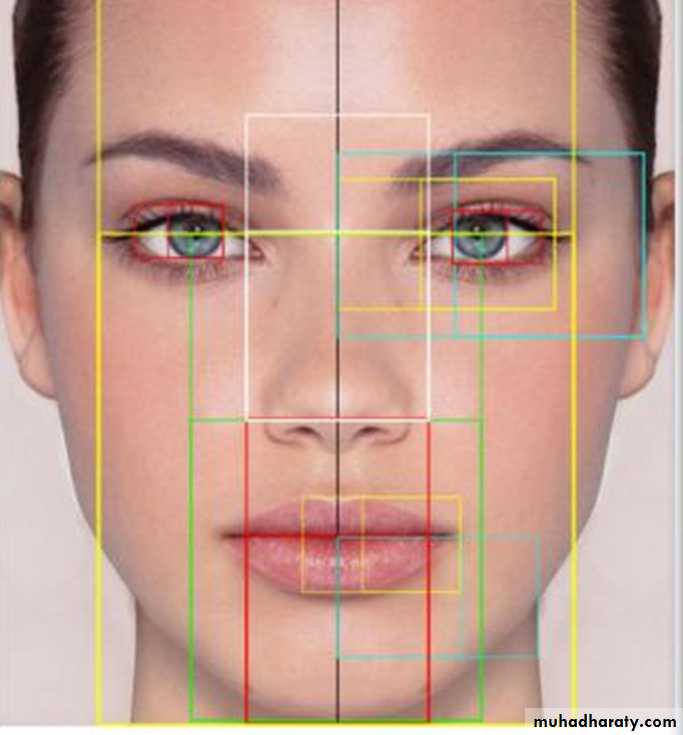
- The relationship between the height and the width of the face has animportant influence on facial form and harmony and should also be correlated with the patient's overall body build. The height-to-width proportions are 1.3:1 for females and 1.35:l for males.
The bigonial width should be approximately 30% less than the bizygomatic dimension and the width and shape of the chin should form a harmonious part of the overall facial contour.
- Transverse dimensions:
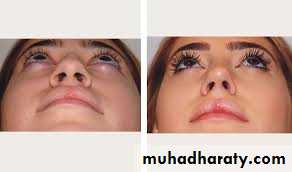
The normal inter-pupillary distance should be 65± 3 mm while the inter-canthal distance should measure 32 ±2 mm.Vertical lines drawn through the medial canthi should coincide with the ala of the nose while vertical lines drawn through the medial margins of the irises of the eyes should coincide with the corners of the mouth.
The measurements will, however, give the clinician an indication of harmony between the nose, mouth, and the eyes. the alar base width will be an important consideration as Le Fort I osteotomy, especially superior repositioning and advancement of the maxilla, may increase the width of the base of the nose. Surgical precautions should be taken to control unwanted nasal changes following Le Fort I osteotomy.
Facial symmetry : the symmetry of the facial midline structures such as the forehead (glabella), nasal tip, upper lip maxillary dental midline, mandibular dental midline, lower lip, and chin should be assessed. The clinician should consider whether orthodontic or surgical Correct of the dental midlines should be planned.
• The left-to- right symmetry must be correlated with the facial midline and the face should be reasonably symmetric vertically and transversely. Keep in mind that no face is perfectly symmetric.
• When evaluating the symmetry of the face it is also very important to assess the presence of any occlusal plane cants. The occlusal plane should be parallel to the inter-pupillary line
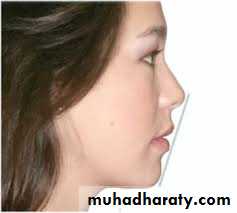
Profile view
Nasolabial angle: is measured between the columella of the nose and the upper lip. The angle should be 90 +_10° and is a guide to the upper lip support by the maxillary incisors. It is, however, also influenced by the decreased vertical dimension due to maxillary vertical deficiency.The lip-chin-throat angle: is formed between the lower border of the chin and a line connecting the lower lip and soft tissue pogonion (110±10º). It is most commonly acute in flat or concave profiles with class III dento-skeletal patterns. An obtuse angle is seen in class II malocclusion, mandibular antero-posterior deficiency, and is often exacerbated by microgenia.
Upper lip length: The upper lip length is measured from subnasale to lower lip and should be 20 ±2 mm for females and 22± 2 mm for males ensure when evaluating the lips that they are in repose. During treatment planning it should be kept in mind that the upper lip length will increase with age.
Ricketts has projected a line from nasal tip to soft tissue pogonion, and suggested the upper lip be 4 mm and the lower 2 mm behind this line. It is very useful in planning.
Labio-mental angle is formed by the intersection of the lower lip and the chin and is measured at soft tissue B-point. The angle should be gently curved (mean 120± 10º)
Documentations of findings
It is recommended to record the clinical findings on standardized documentation sheets. Standard digital photography (profile, frontal view, three quarter view, bird's eye view) are taken and attached to the clinical documentation. Standard especially profile pictures, are necessary to do a profile outcome prediction.Dental examination
A complete dental examination should include assessment of dental arch form, symmetry, tooth alignment, and occlusal abnormalities in the transverse, anteroposterior, and vertical dimensions. The muscles of mastication and TMJ function should also be evaluated. A screening periodontal examination, including probing, should assess the patient's hygiene and current Periodontal health status.Radiographic evaluation:
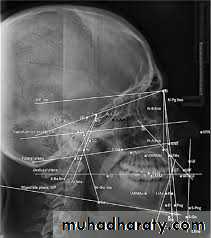
The radiographs mostly used as routine in the diagnosis of dentofacial deformities are lateral and postero- anterior cephalometric radiographs, panoramic radiographs, and periapical radiographs. Other radiographic imaging modalities, such as TMJ tomograms, magnetic resonance imaging (MRI), and computed tomography (CT) scans, may be required as determined by the needs of each individual case. Although clinical evaluation must be the primary diagnostic tool in determining surgical treatment of the orthognathic patient, cephalometric analysis is a helpful diagnostic guide.Lateral cephalometric analysis
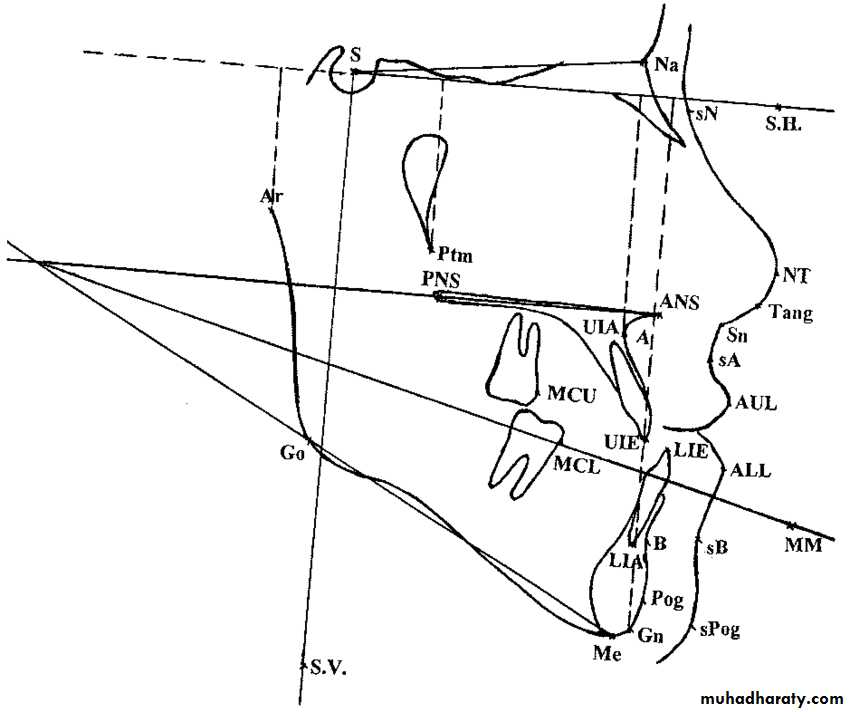
Cephalometric is done to evaluate the proportions of the facial skeleton and to compare an individual patient with norm. Standard skeletal analysis is based on plain X-Rays taken in the sagital and frontal plane. Typically the X-rays are analyzed with the help of computer based programs. Protocols for analysis differ to some extent. All of them are based on reference points, lines, and angles which are marked on the X-ray.Hard tissue landmarks are as follows:
Nasion n (0) the most amteriar point on the fitontal nasal suiure in themidsagittal plane.
Orbitale (OR): the lowest point on the inferior orbital rim.
Sella (S): the center of the sella turcica, as on the lateral cephalogram, which is located by inspection.
Anterior nasal spine (ANS): anterior tip of the nasal spine.
Apoint (A) the most posterior midline point in the concavity where the lower anterior edge of the anterior nasal spine meets the alveolar bone overlying the maxillary incisor teeth.
B-point (B): the most posterior midline point in the concavity of the mandible between the alveolar bone overlying the lower incisor teeth and the pogonion.
Gonion (Go): the point is defined by using two lines, one tangent to the posterior border of the mandibular ramus and the other tangent to the lower border of the mandibular corpus; found by bisecting the angle formed by the two lines and extending the bisector through the curvature of the mandibular angle.
Menton (Me): the most inferior point on the symphysis of the mandible in the midline.
Porion (P): the most superior point of the external auditory meatus (anatomic point); machine porion is the uppermost point on the outline of the rods of the cephalometer.
Condylion (Co): the most postero-superior point on the head of the condyle.
Gnathion (Gn): the lowest, most anterior midpoint on the symphysis of the mandible.
Glabella (G): the most anterior point on the frontal bone.
The following constructed hard tissue facial planes are mostly used:
frankfort horizontal plane (FH): extends from porion to orbitale.
Anterior cranial base (SN): formed by a line drawn from sella to nasion.
Occlusal plane (OP): formed by a line drawn through the mesial cusp contact of the first molar teeth and dividing the incisor overbite.
Mandibular plane (MP): extends from gonion to menton.
Skeletal antero-posterior relationships
• Maxillary antero-posterior position. The analysis gives an indication of the antero-posterior position of the maxilla in relation to the anterior cranial base. The angle between the anterior cranial base (SN) and a line drawn between the nasion (N) and A-point is measured and should be 82º for a normal maxilla• Maxillary depth angle. The angle between the FH and NA alos gives indication of the maxillary antero-posterior position and should be 90º A line perpendicular to FH should therefore fall on A-point.
Mandibular antero-posterior position. The SNB angle is measured between SN and a line drawn between N and B-point and it relates the antero-posterior position of the mandible to SN. This angle should be 80 for a normal mandibular position.
ANB angle. This angle gives the clinician an indication of the inter- relationship between the upper and lower jaw. In class II mandibular deficient cases the angle will be increased while in class III cases the angle will be decreased. An angle of 2 °indicates a normal relationship.
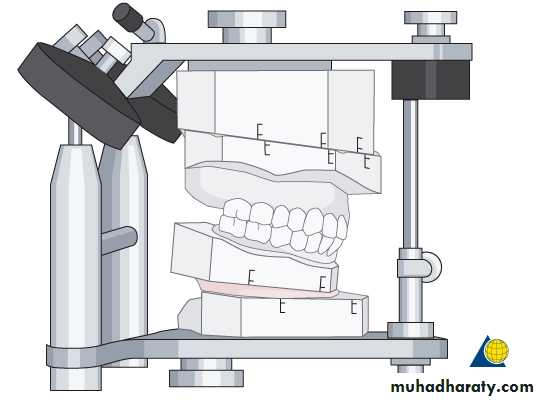
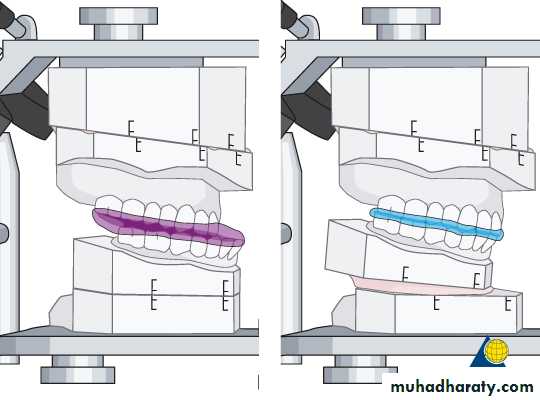
Model analysis
Model analysis (study casts)Plaster of Paris models from the maxilla and mandible are taken and the actual centric occlusion of the patient is recorded. The models are oriented in a semi adjustable articulator after face-bow transfer.
The models allow analyzing the:
occlusionShape of the dental arches
position
Size and shape of the teeth
Position of the jaws in relation to the skull base
Usually two sets of models are used. One is kept to analyze and document the preoperative situation. The second set of models is used to perform mock surgery.
Pre-surgical Orthodontic Considerations
in some cases an adequate occlusal relationship cannot be achieved because of the skeletal discrepancy; some patients may be treated with orthodontic compensation for a skeletal abnormality, resulting in an adequate occlusion but poor facial or dental esthetics or a poor long term prognosis for post treatment retention. These patients should be considered for surgery combined with orthodontic treatment.Treatment Timing
As a general guideline, orthognathic surgery should be delayed until growth is complete in patients who have problems of excess growth, although surgery can be considered earlier for patients with growth deficiencies.
Orthodontic Treatment Objectives
Undesirable angulation of the anterior teeth occurs as a compensatory response to a developing dento-facial deformity. For example, a patient with maxillary deficiency and/or mandibular excess often has dental compensation for the skeletal abnormality with flared upper incisors and retracted or retroclined lower incisors. Dental compensations for the skeletal deformity are corrected before surgery by orthodontically repositioning teeth properly over the underlying skeletal component, without considerations for the bite relationship to the opposing arch.The amount of pre-surgical orthodontics can vary, ranging from appliance placement with minimal tooth movement in some patients to approximately 12 to 18 months of appliance therapy in those with severe crowding and incisor malposition.
The essential steps in orthodontic preparation are to align the arches individually, achieve compatibility of the arches or arch segments, and establish the proper antero-posterior and vertical position of the incisors.
Final Treatment Planning
After the completion of the pre-surgical periodontics, restorative dentistry and orthodontics, the patient returns to the oral and maxillofacial surgeon for final re-surgical planning. The patient's facial structure and the malocclusion are reexamined. re-surgical digital photographs and radiographs are obtained. Pre-surgical models, a centric relation bite registration, and face-bow recording for model mounting are completed. Model surgery on a duplicated set of pre surgical dental casts determines the exact surgical movements necessary to accomplish the desired postoperative occlusion.Mock surgery and fabrication of splints
SURGICAL TREATMENT PHASE
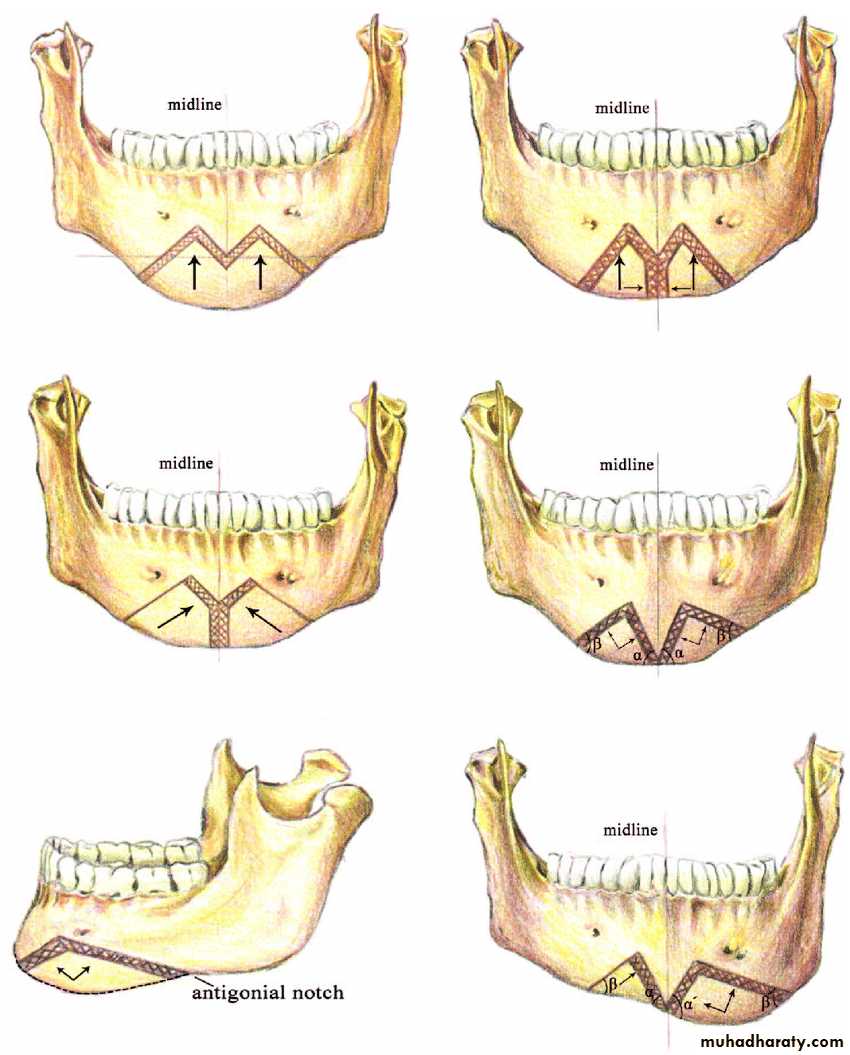
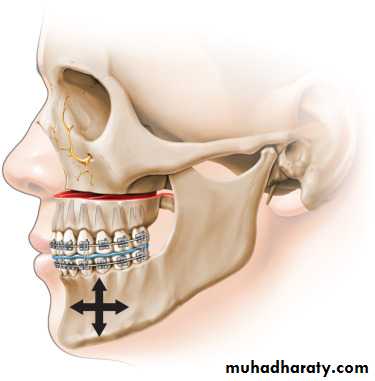
Dento-facial abnormalities frequently can be treated by isolated procedures in the mandible or maxilla and midface area. Because abnormalities can obviously occur in the maxilla and the mandible, surgical correction frequently requires a combination of surgical procedures.Mandibular Excess
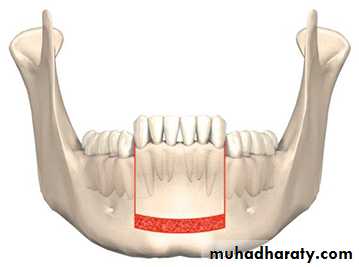
Excess growth of the mandible frequently results in an abnormal occlusion with Class III molar and cusped relationships and a reverse overjet in the incisor area. An obvious facial deformity may also be evident. Facial features associated with mandibular excess include a prominence of the lower third of the face, particularly in the area of the lower lip and chin in the antero-posterior and vertical dimensions.Early treatment of mandibular prognathism dealt with the deformity by removing sections of bone in the body of the mandible, which allowed the anterior segment to be moved posteriorly. As When the reverse overjet relationship is isolated to the anterior dento-alveolar area of the mandible, a subapical osteotomy technique can be used for correction of mandibular dental prognathism.
In this technique, bone is removed in the area of an extraction site of a premolar or molar tooth, and the anterior dento-alveolar segment of the mandible is moved to a more posterior position. Although these procedures are rarely used, they are occasionally performed in cases with unusual arch forms in combination with edentulous spaces.
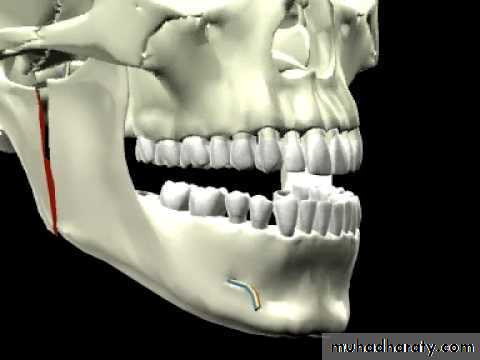
In the early 1950s, Caldwell and Letterman popularized an osteotomy (Sub-sigmoidal osteotomy) performed in the ramus of the mandible for the correction of mandibular excess. In this technique the lateral aspect of the ramus is exposed through a submandibular incision, the ramus is sectioned in a vertical fashion, and the entire body and anterior ramus section of the mandible are moved posteriorly, which places the teeth in proper occlusion. The proximal segment of the ramus(i.e. the portion attached to the condyle) overlaps the anterior segment, and the jaw is stabilized during the healing phase with wiring of the bone segments combined with jaw immobilization using IMF. The external approaches rarely used.
A similar technique is performed with an intraoral incision and an angulated oscillating saw.. The bone segments can be stabilized using IMF, with or without direct wiring of the segments or using rigid fixation with bone plates or screws, eliminating the need for IMF. The advantages of the intraoral technique include elimination of the need for skin incision and decreased risk of damage to the mandibular branch of the facial nerve.
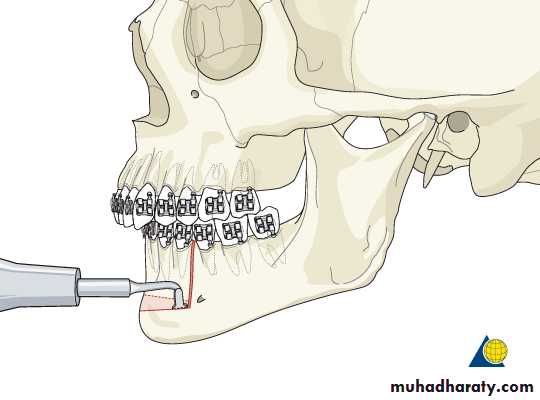
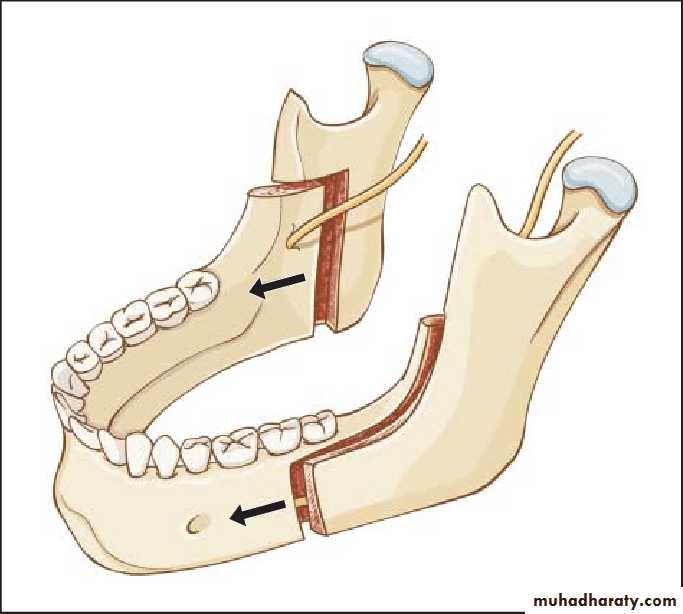
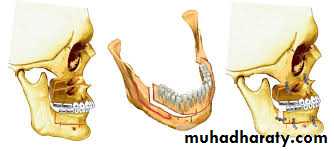
Another popular technique for correction of mandibular prognathism is the bilateral sagittal split osteotomy (BSSO) described Obwegeser .
The BSSO is accomplished through a trans-oral incision similar to that for the intraoral vertical ramus osteotomy. The osteotomy splits the ramus and posterior body of the mandible in a sagittal fashion, which allows setback or advancement of the mandible. The BSSO technique has become one of the most popular methods for treatment of mandibular deficiency and mandibular excess. This is a universal procedure that can be employed for all mandibular movements. Disadvantages include potential trauma of the inferior alveolar nerve, with subsequent decreased sensation in the area of the lower lip and chin during the immediate postoperative period. This may be permanent.
Vertical ramus osteotomy
Sagittal split osteotomyMandibular Deficiency
The most obvious clinical feature of mandibular deficiency is the retruded position of the chin as viewed from the profile aspect. Other facial features often associated with mandibular deficiency may include an excess labio-mental fold with a procumbent appearance of the lower lip, abnormal posture of the upper lip, and poor throat form. Intraorally, mandibular deficiency is associated with Class II molar and canine relationships and an increased overjet in the incisor area.Currently, the BSSO is the most popular technique for mandibular advancement. The osteotomy is frequently stabilized with rigid fixation plates or screws, eliminating the need for IMF If the anteroposterior position of the chin is adequate but if a Class II malocclusion exists. a total subapical osteotomy may be the technique of choice for mandibular advancement.
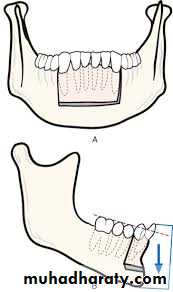
Total subapical osteotomy:
Dento-alveolar segment of mandible is moved anteriorly, allowing correction of Class II malocclusion without increasing chin prominence. When a proper occlusal relationship exists or when anterior positioning of the mandible would not be sufficient to produce adequate projection of the chin, an inferior border osteotomy (genioplasty) with advancement may also be performed.
This technique is usually performed through an intraoral incision. The inferior portion of mandible is osteotomized, moved forward, and stabilized. In addition to anterior or posterior repositioning of the chin, vertical reduction or augmentation and correction of asymmetries can also be accomplished with inferior border osteotomies. Alloplastic materials can occasionally be used to augment chin projection; the material is onlayed in areas of bone deficiencies.
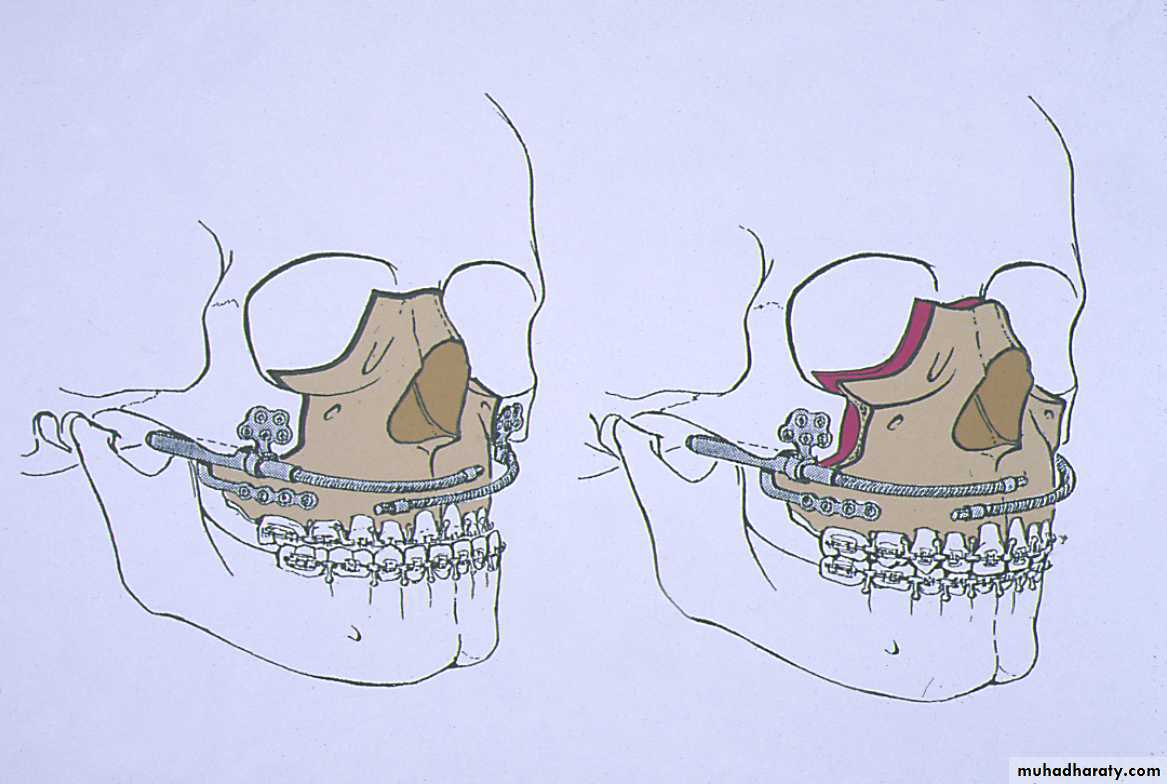
Maxillary Excess
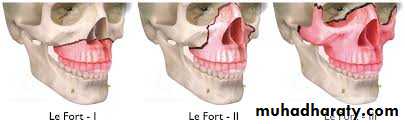
Excessive growth of the maxilla may occur in the anteroposterior, vertical, or transverse dimensions. Surgical correction of dento-facial deformities with total maxillary surgery (Lefort I) has only become popular since the early 1970s. Before that time, maxillary surgery was performed on a limited basis, and most techniques repositioned only portions of the maxilla with segmental surgery. In the early 1970s, research by Bell et al. demonstrated that total maxillary surgery could be performed without jeopardizing the vascular supply to the maxilla.Vertical maxillary excess may result in associated facial characteristics, including:
• Elongation of the lower third of the face• Narrow nose, particularly in the area of the alar base;
• Excessive incisal and gingival exposure.
• lip incompetence.
These patients may exhibit Class l, Class II, or Class III dental malocclusions.
A transverse maxillary deficiency with a posterior cross-bite relationship, constricted palate, and narrow arch form is often seen with this deformity.
Vertical maxillary excess is frequently associated with an anterior open-bite relationship (apertognathia). This results from excessive downward growth of the maxilla, causing downward rotation of the mandible as a result of premature contact of posterior teeth.
To correct this problem, the maxilla is repositioned superiorly (impacted), particularly in the posterior area. This allows the mandible to rotate upward and forward, establishing contact in all areas of the dentition. In some cases the occlusal plane of the maxilla is level after orthodontic preparation, and the open bite can be corrected by repositioning the maxilla in one piece. In other cases, a step in the occlusal plane must be leveled to achieve the desired occlusion. This requires repositioning of the maxilla in segments.
Anteroposterior maxillary excess :
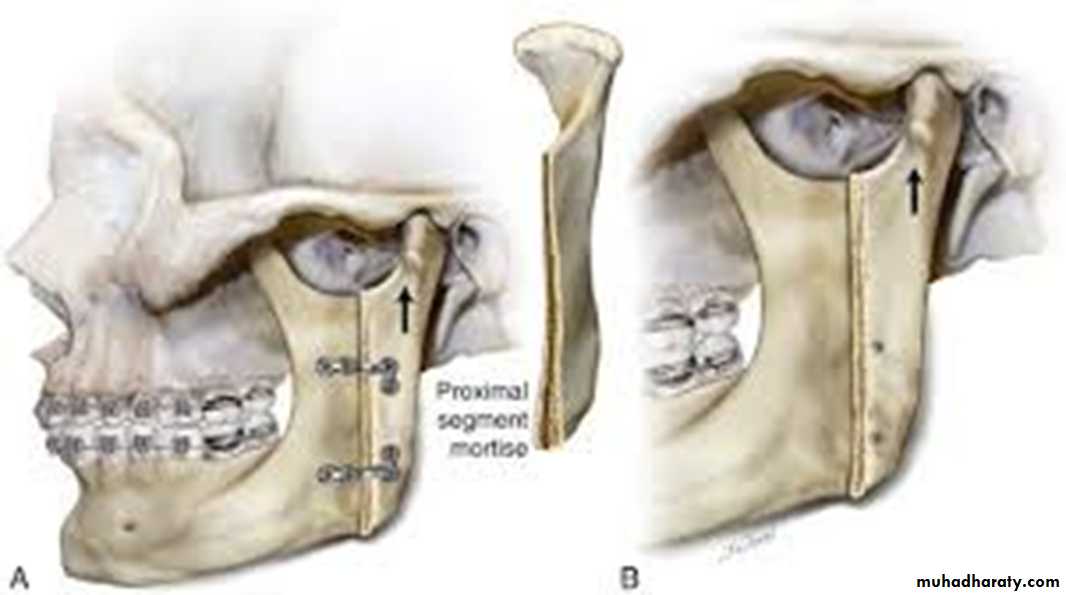
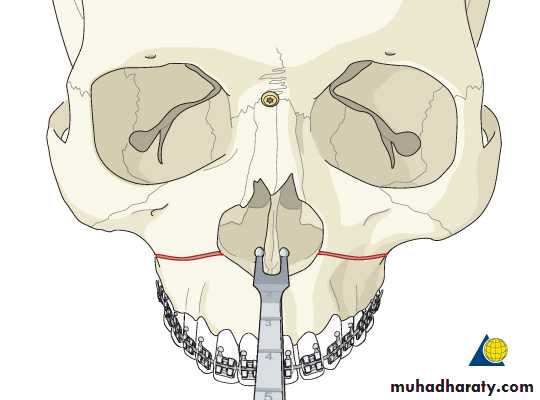
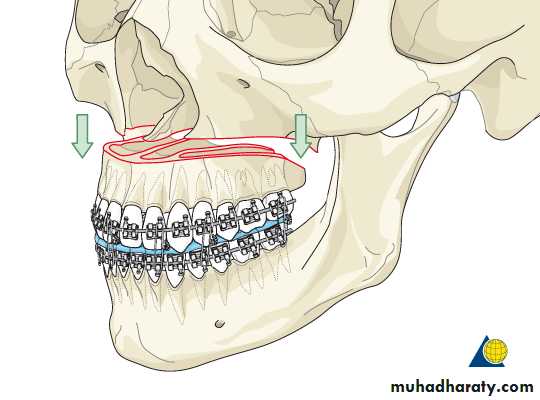
results in a convex facial profile usually associated with incisor protrusion and a Class II occlusal relationship. Total maxillary surgery ( lefort I ) can be completed to correct this problem In some cases the entire maxilla can be moved in one piece in a posterior direction. In addition to procedures in which the maxilla is moved in one piece, the bone can be sectioned into dento-alveolar segments to allow repositioning 1n anteroposterior, superior, or inferior directions or to allow expanding in the transverse directionMaxillary and Midface Deficiency
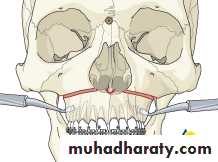
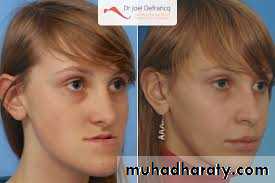
Patients with maxillary deficiency commonly appear to have a retruded upper lip, deficiency of the paranasal and infraorbital rim areas, inadequate tooth exposure during smile, and a prominent chin relative to the middle third of the face.The primary technique for correction of maxillary deficiency is the Le Fort I osteotomy. This technique can be used for advancement of the maxilla to correct a Class III malocclusion and associated facial abnormalities. Depending on the magnitude of advancement, bone grafting may be required to improve bone healing and postoperative stability. In the case of vertical maxillary deficiency, elongation of the lower third of the face can be accomplished by bone grafting the maxilla in an inferior position with the Le Fort I osteotomy technique.
In severe midface deformities with infraorbital rim and malar eminence deficiency, a Le Fort III or modified Le Fort Ill type of osteotomy is necessary. These procedures advance the maxilla and the malar bones and, in some cases. The anterior portion of the nasal bones. This type of treatment is commonly required in patients with craniofacial deformities such as Apert’s or Crouzon's syndrome.
Cruzen Apert
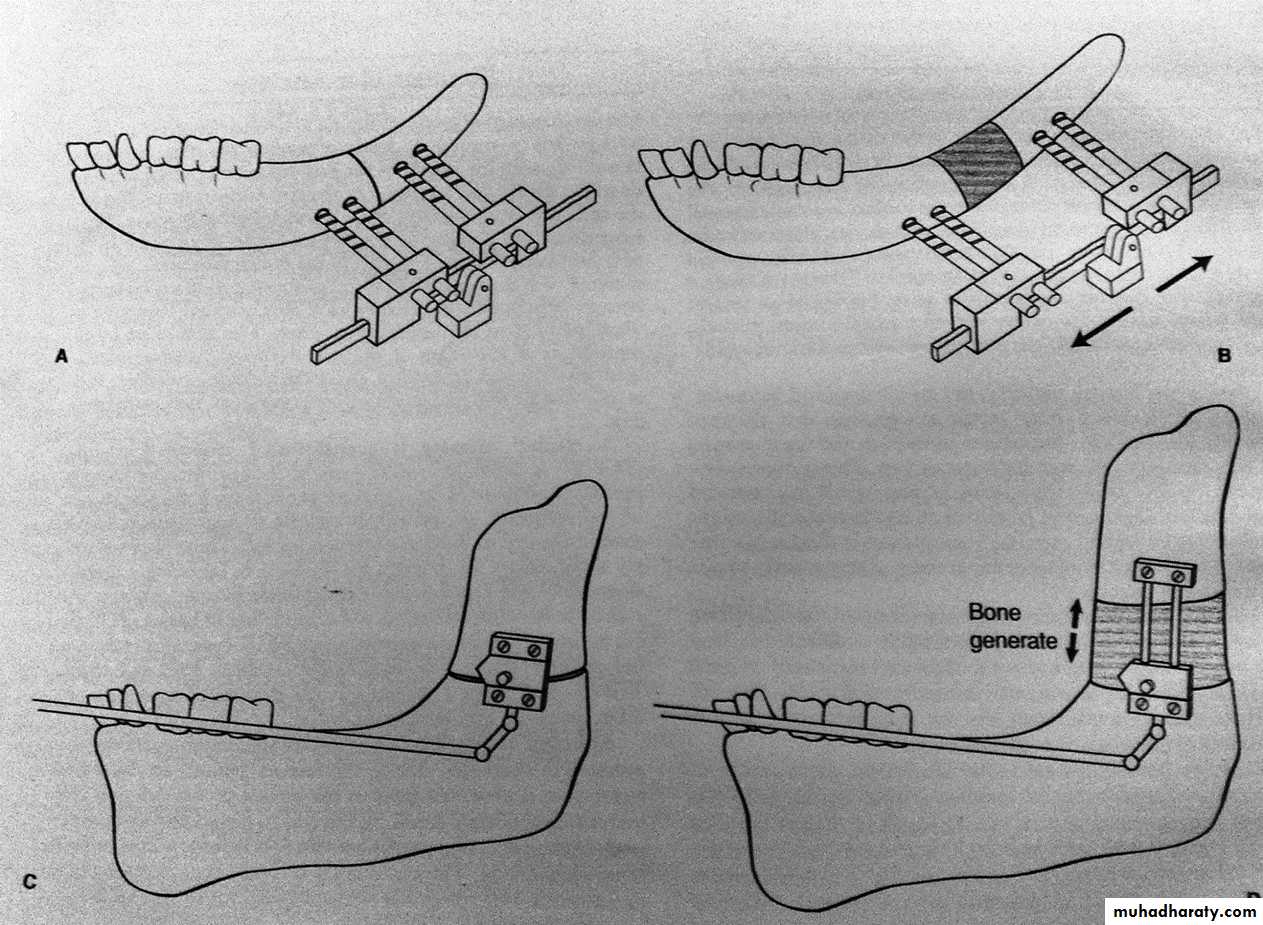
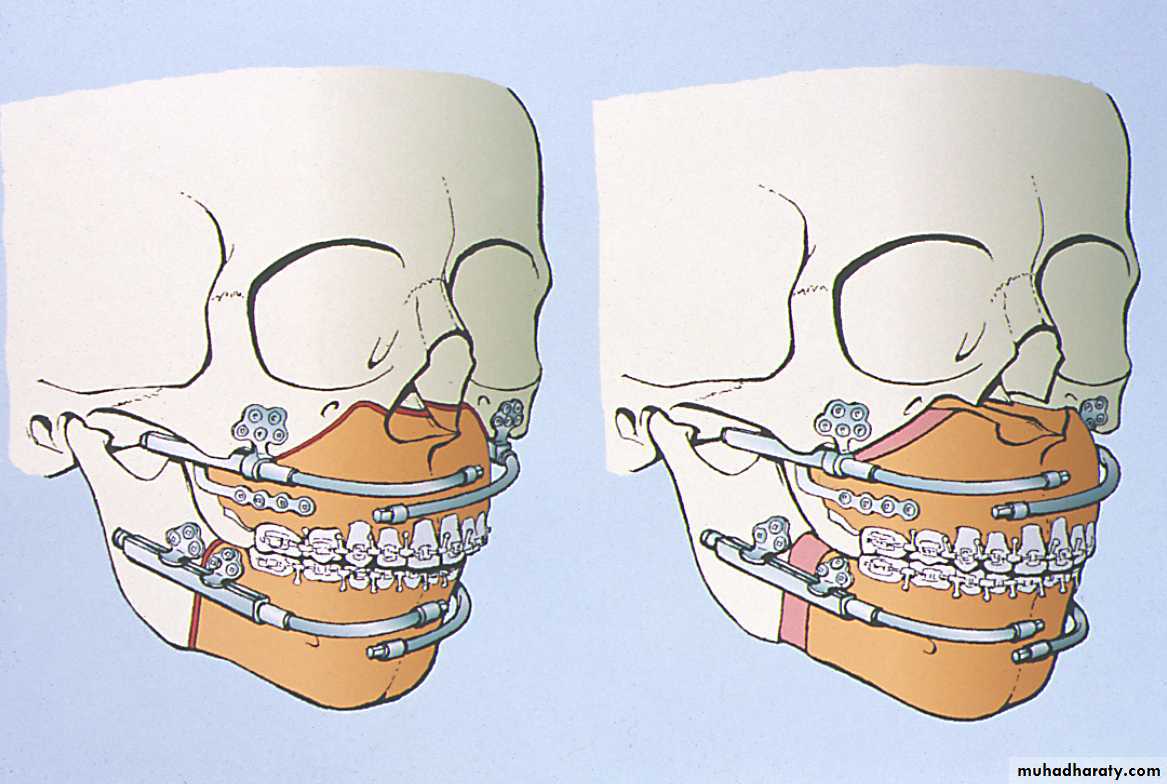
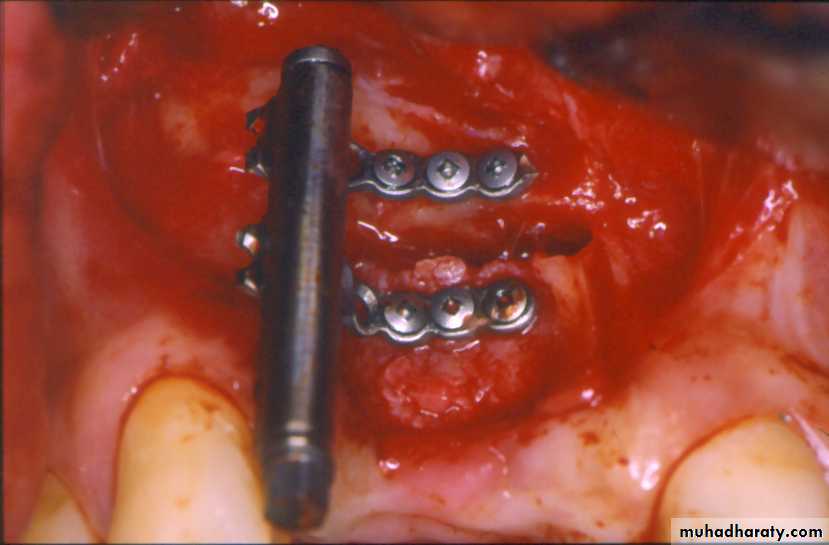
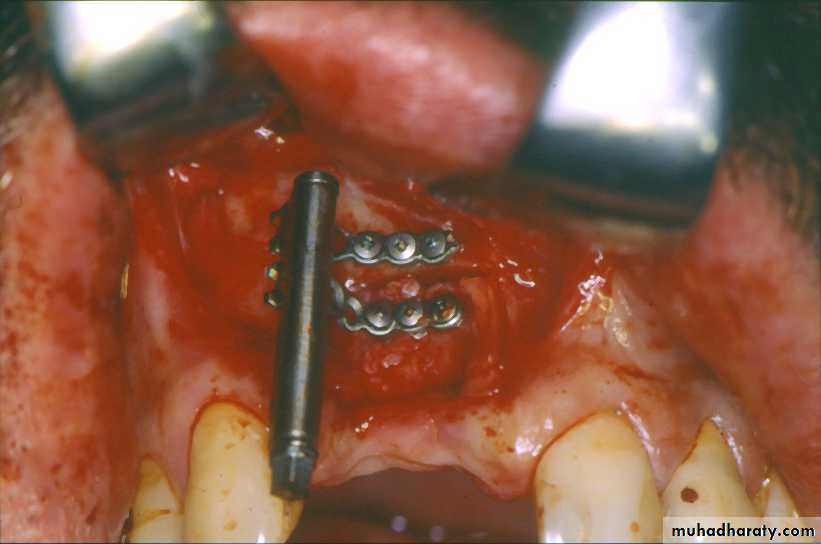
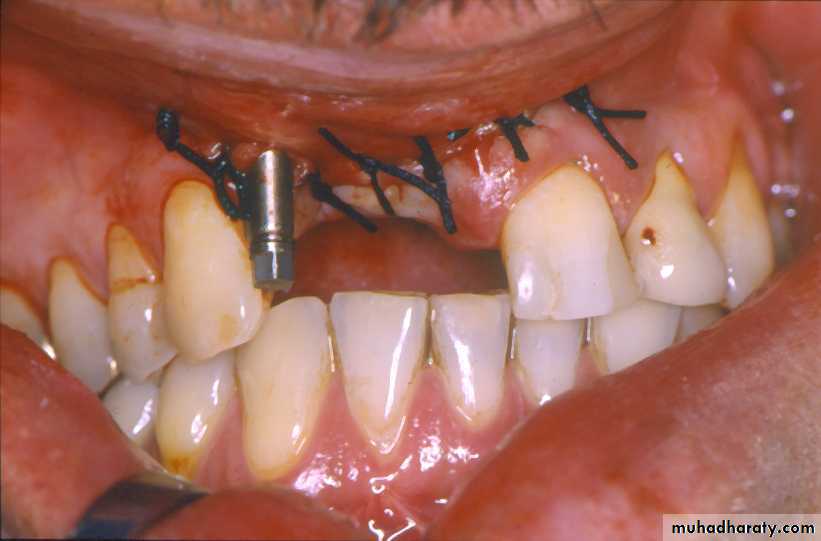
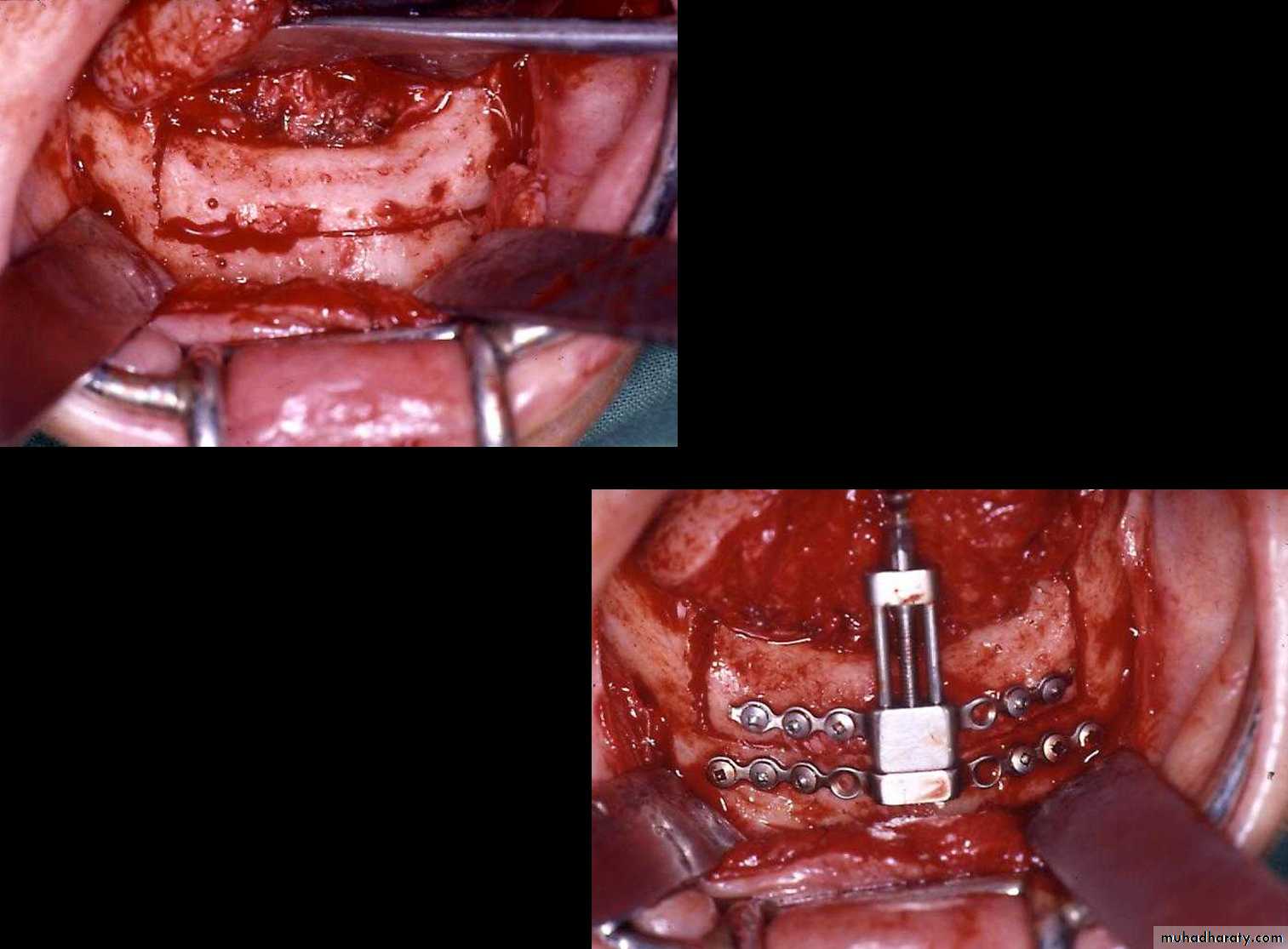
DISTRACTION OSTEOGENESISOne new approach for correction of deficiencies in the mandible and the maxilla involves the use of distraction osteogenesis (DO). When correcting deformities associated with these deficiencies, the conventional osteotomy techniques have several potential limitations. When large skeletal movements are required, the associated soft tissue often cannot adapt to the acute changes and stretching that result from the surgical repositioning of bony segments. This failure of tissue adaptation results in several problems, including surgical relapse, potential excessive loading of the TMJ structures, and increased severity of neurosensory loss as a result of stretching of nerves. In some cases the amount of movement is so large that the gaps created require bone grafts harvested from secondary surgical sites such as the iliac crest.
The bone is separated into segments by either a full thickness osteotomy or by a low-energy corticotomy. The location of the bony separation is termed ( the distraction zone).
time is allowed (5 to 7 days) for reparative callus formation in the distraction zone (the latency period).
Gradual distraction forces are applied to separate the edges and elongate the inter-segmentary callus under tension (the activation period).
a. Rigidity of the distraction device is critical to maintain the inte-rsegmentary gap tissue in a direction or vector parallel to the orientation of the device (the vector of distraction ).
b. A rhythm of 0.25mm four times a day is preferable (0.5mm twice a day is generally acceptable).
4. At the end of activation, the external fixation must be maintain in position to allow consolidation of the newly formed bone (consolidation period).
Consolidatation period usually lasts approximately 8 week.
Advantage of distruction osteogenisis:
• Length of hospitalization time has been redused.
• Distraction even can be performed on an outpatient.
• The technique, which can be applied at a younger age has obviated the need of IMF.
• Obviate the need of blood transfusion.
• No need for autogenous bone graft ( as often required in traditional orthognathic surgery).
• 6. Technique also allows the augmentation of hypo plastic mandible.
• 7. There is gradual distraction not only of the bony skeleton but also of the associated soft tissues, such as muscle of mastication, subcut. Tissue and skin.• 8. Relapse in distraction osteogenisis is minimal in contrast to traditional orthognathic advancement surgery.
• 9. There is no discomfort when the device is in place and the child is able to eat a regular (soft) diet during the period of treatment.
Disadvantages of DO:
• Residual cutaneous scarring.• Injury of inferior alveolar nerve.
• In one patient undergoing unilateral distraction, there was nocturnal TMJ pain on the affected side.
• Changes in the TMJ following unilateral mandibular distraction showed that there was a transient posterior condylar flattening of the ipsilateral condyle and posterosuperior flattening of the contralateral condyle.
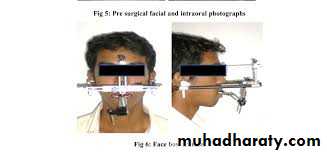
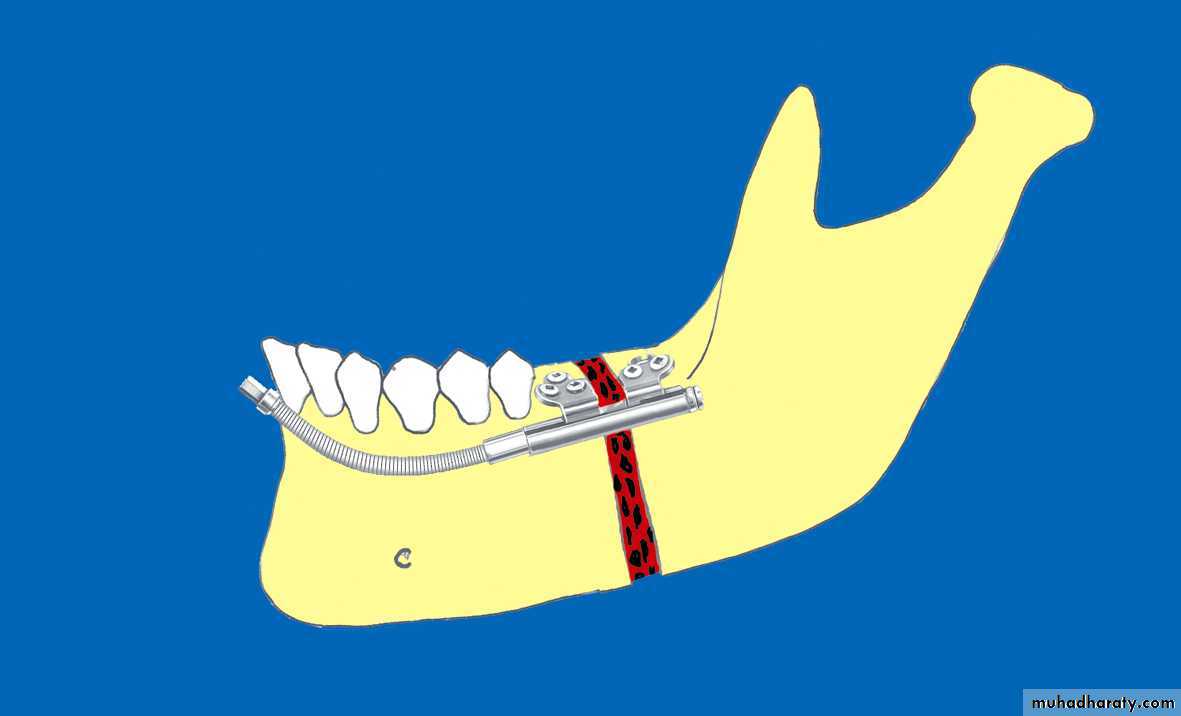
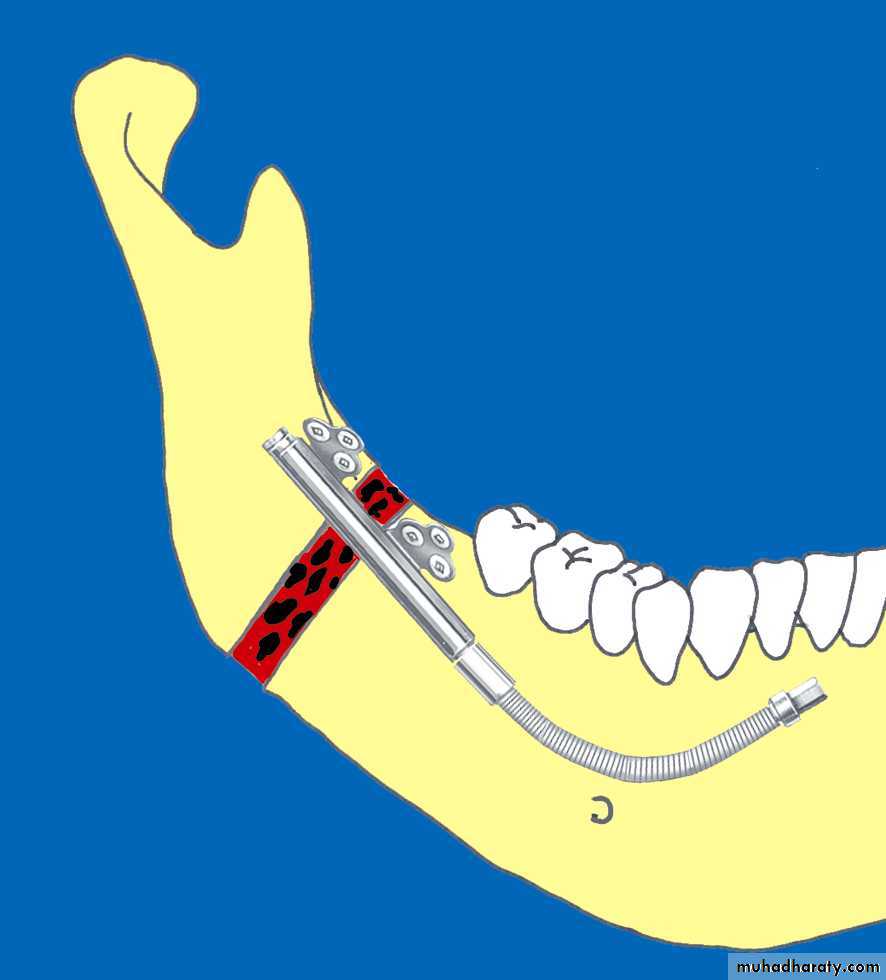
• Mandibular DO:
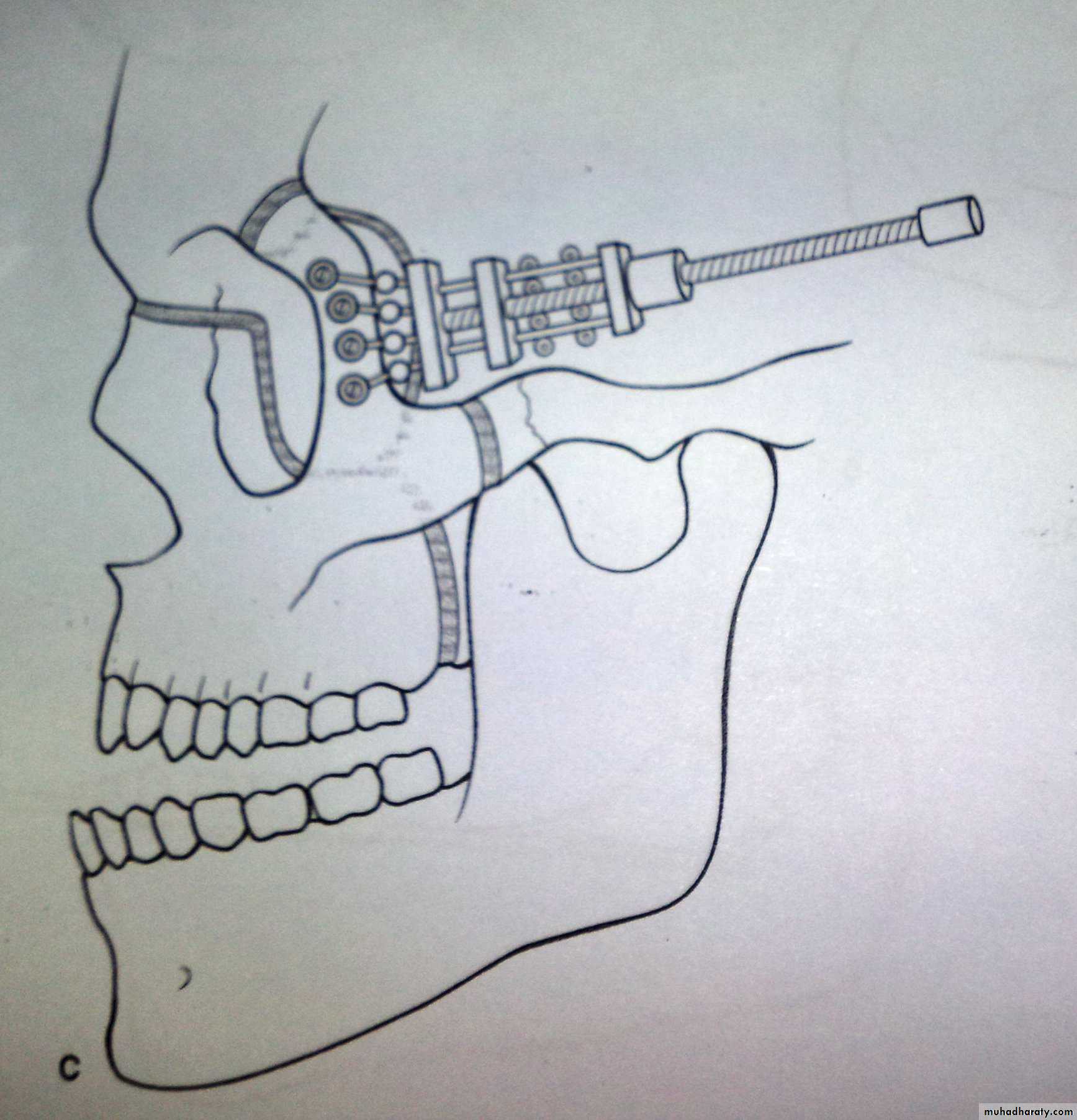
• There are two type of distracters:• External (extra oral) device:
• Indicated when the skeletal site for the osteotomy and pin insertion is diminutive in area and volume.
• Disadvantage is that it leaves an external scar, which can be obvious and hypertrophic in a few patients.
• Internal (intra oral) – buried device:
• Its associated with better scar. the actual progress of the activation cannot be observed externally.
• Disadvantage is that its much more difficult to remove.
• Technique
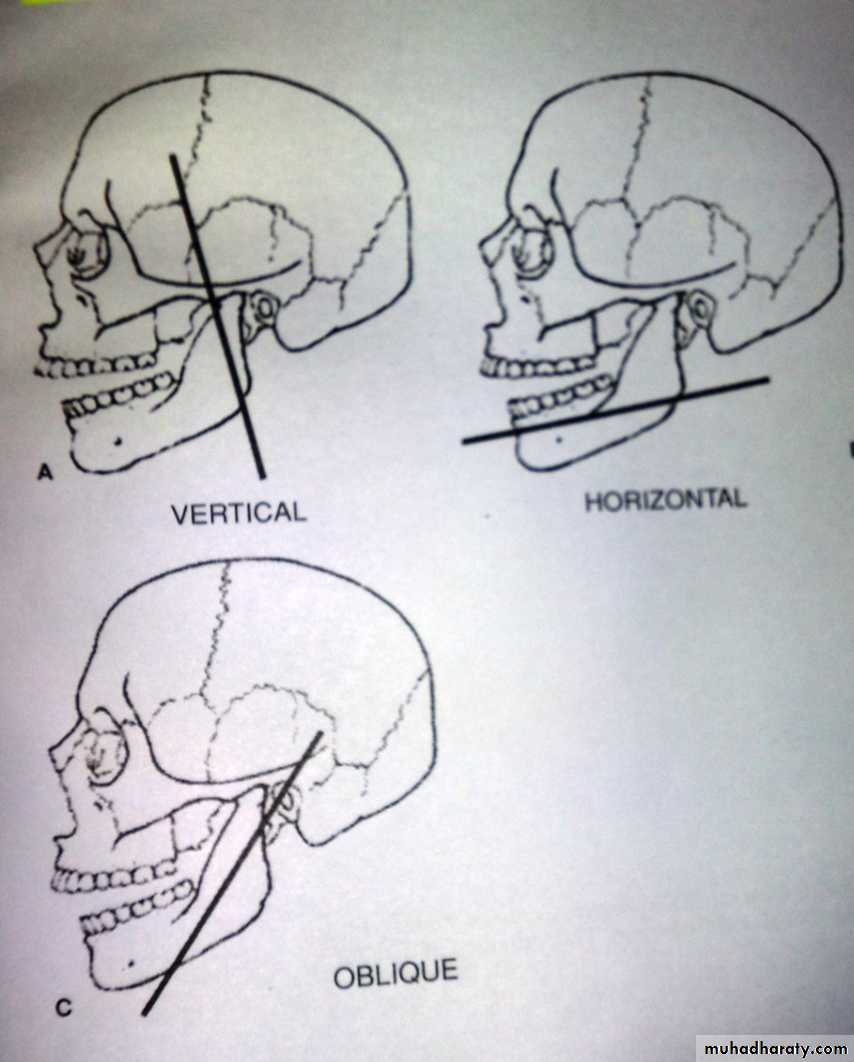
• The first decision is the choice of a vector:• Vertical vector:
• 90 degrees to the maxillary occlusal plane and is indicated when there is a vertical deficiency of the ramus.
• Horizontal vector:
• parallel to the maxillary occlusal plane and is indicated in patients with severe micognathia associated with deficiency of the mandibular body.
• Oblique victor :
• A line bisect the two planes above and its indicated when there is deficiency in both the vertical ramus and the horizontal body of mandible.
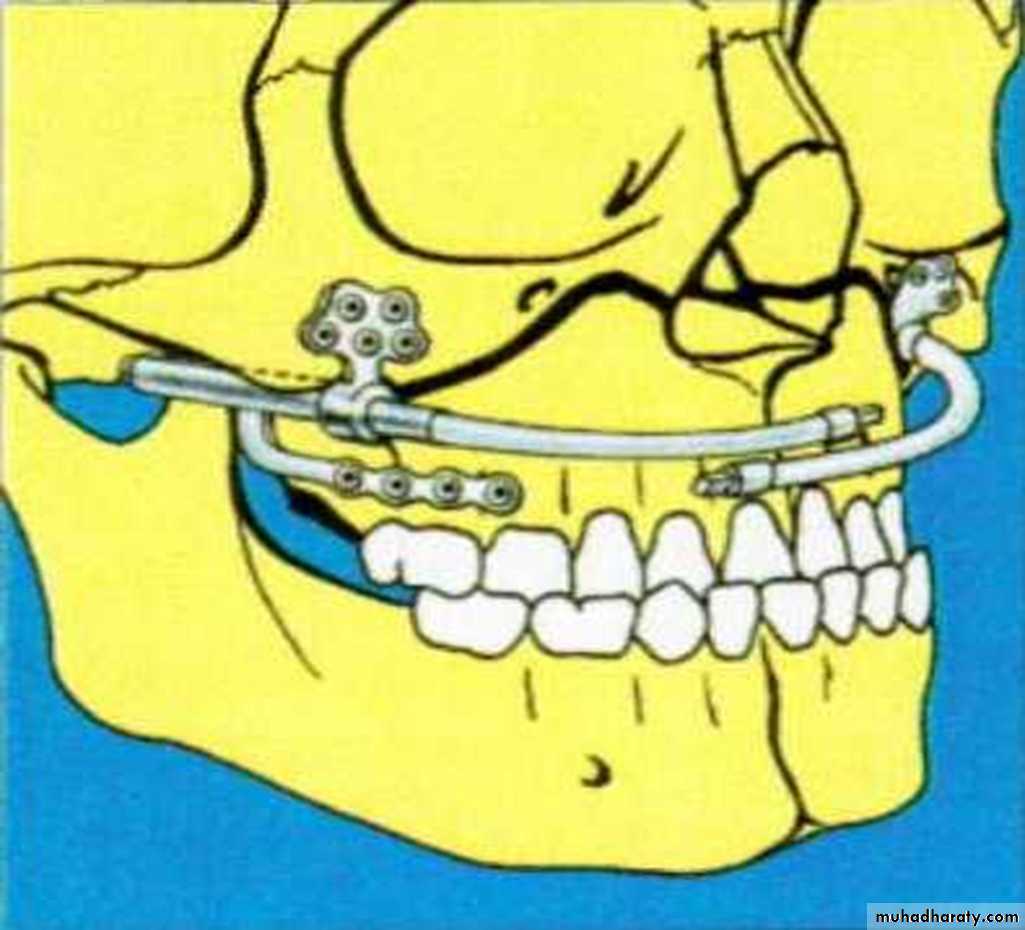
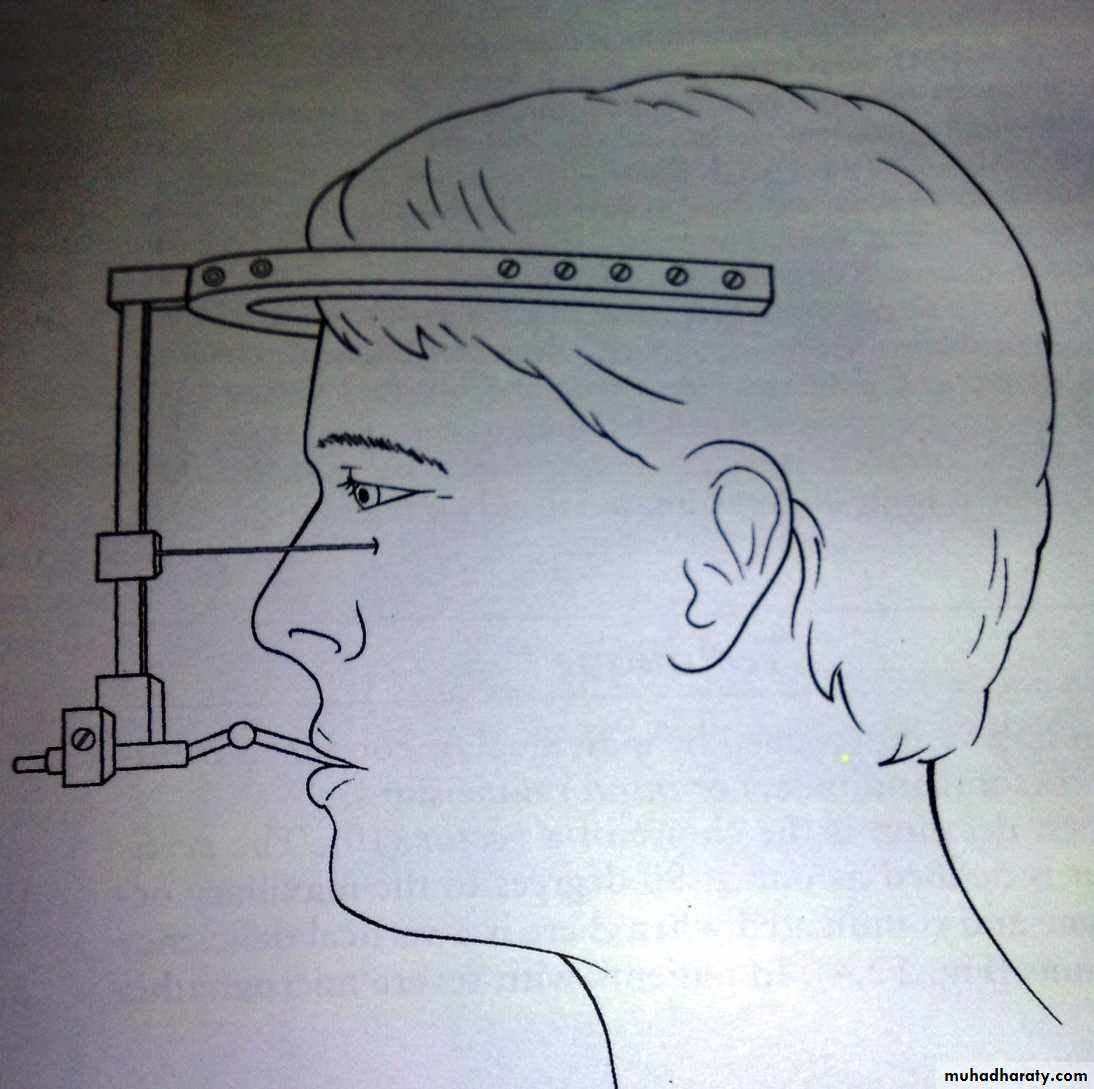
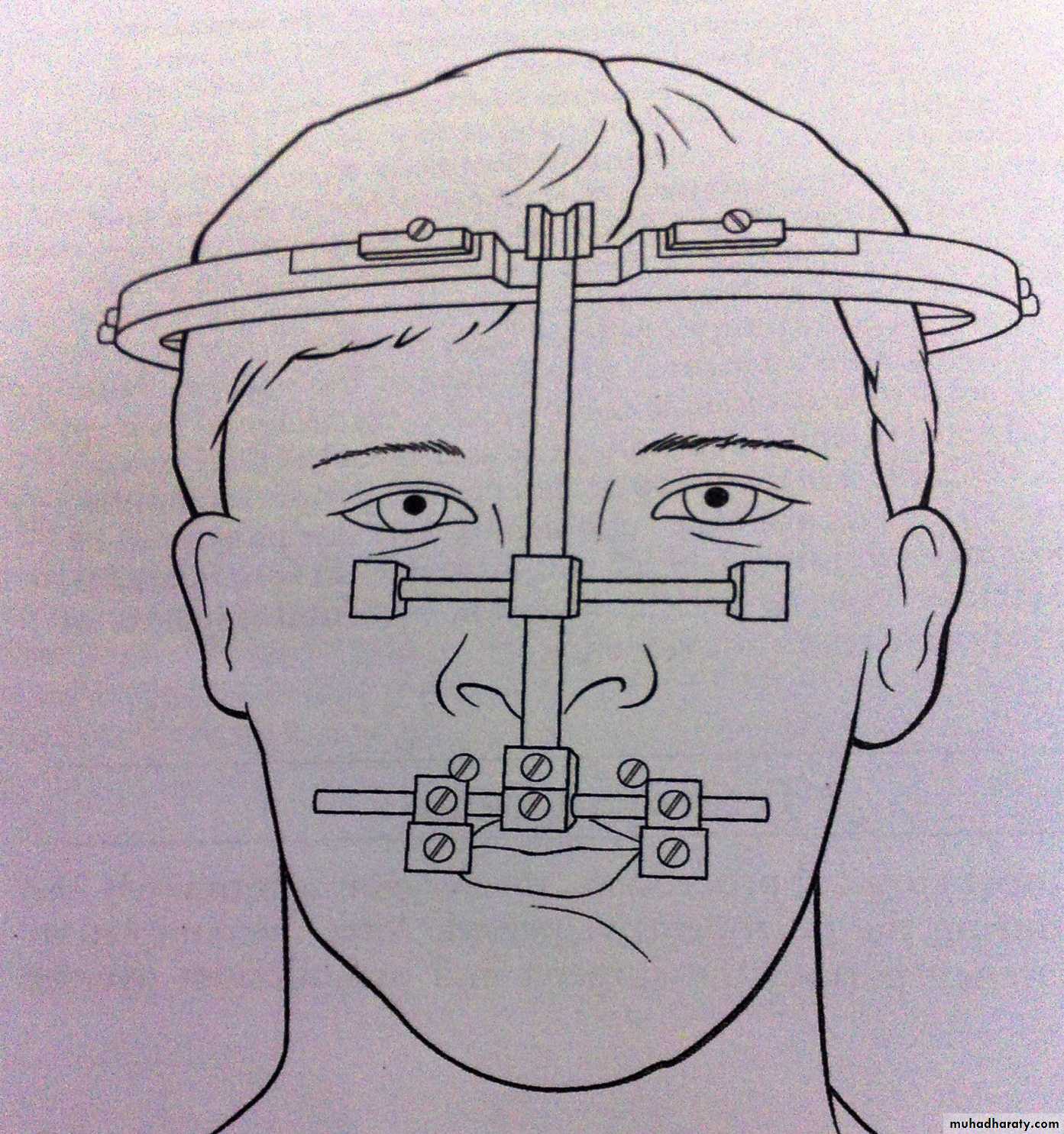
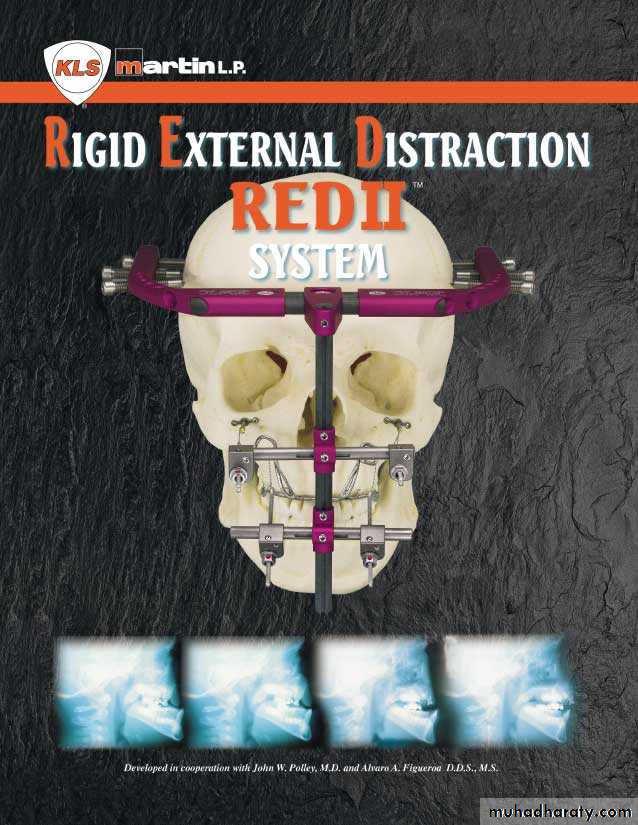
Maxillary distraction
• 1. External head frame rigid external distracter (RED):• Provides relative stability and the ability to change the vector during activation .
• 2. Internal or buried device.
• A vector is usually chosen in a forward and downward direction.
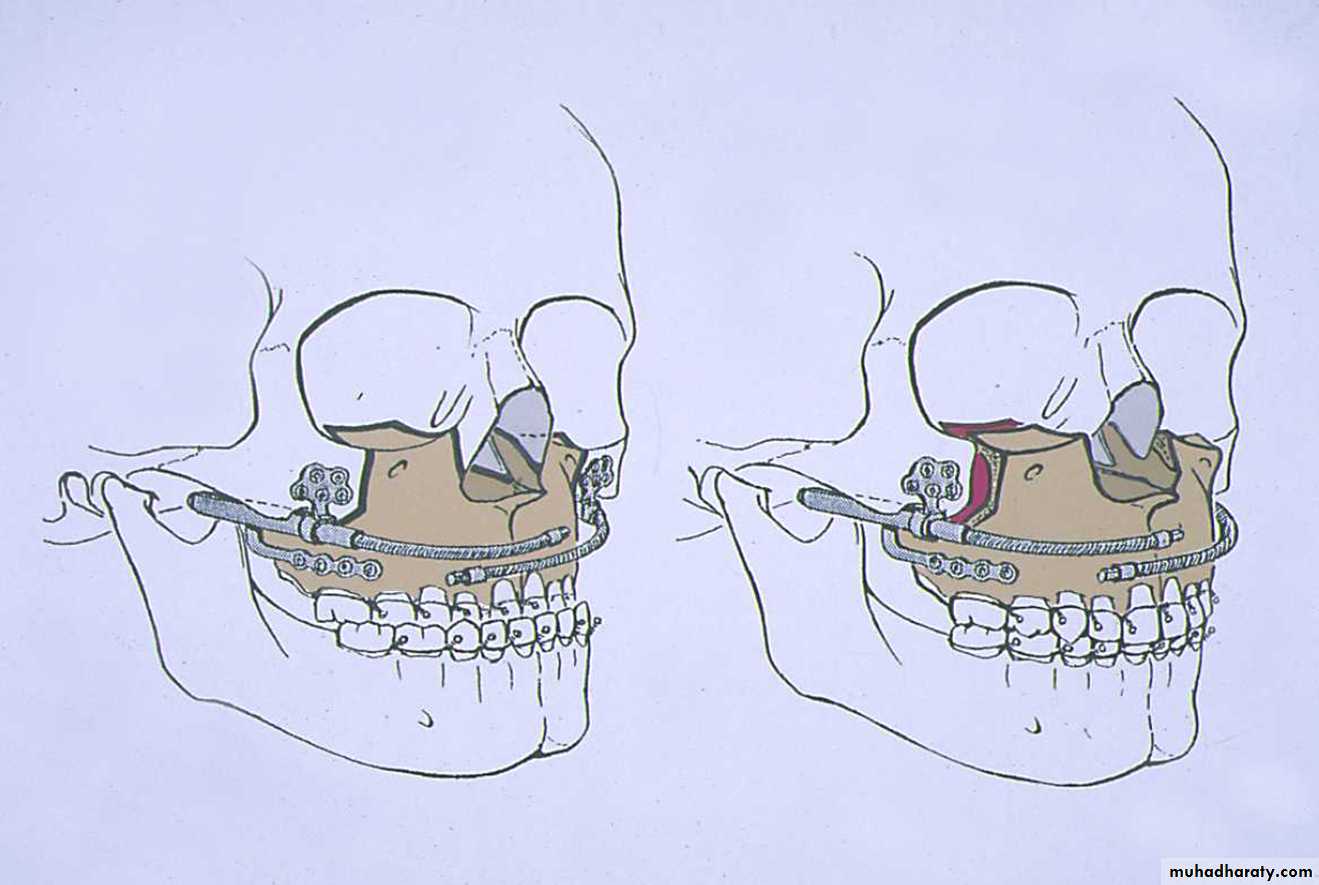
Midface distraction
• It is indicated in the syndromic cranial synostosis patient with exorbitism, malocclusion, sleep apnea, midface retrusion, and severe dismorphism. Patient with orbito facial clefts are also candedates.• Also when performed in a growing child , it must be emphasized to the family that a second midface procedure will be required when the child completes craniofacial skeletal growth in late adolescence.
There are tow types of midface distracters:
• 1. Head frames.
• 2. Buried devices.
AND
THANK YOU