Fifth Stage
Medicine
Dr. Fadhil – Lecture 2
1
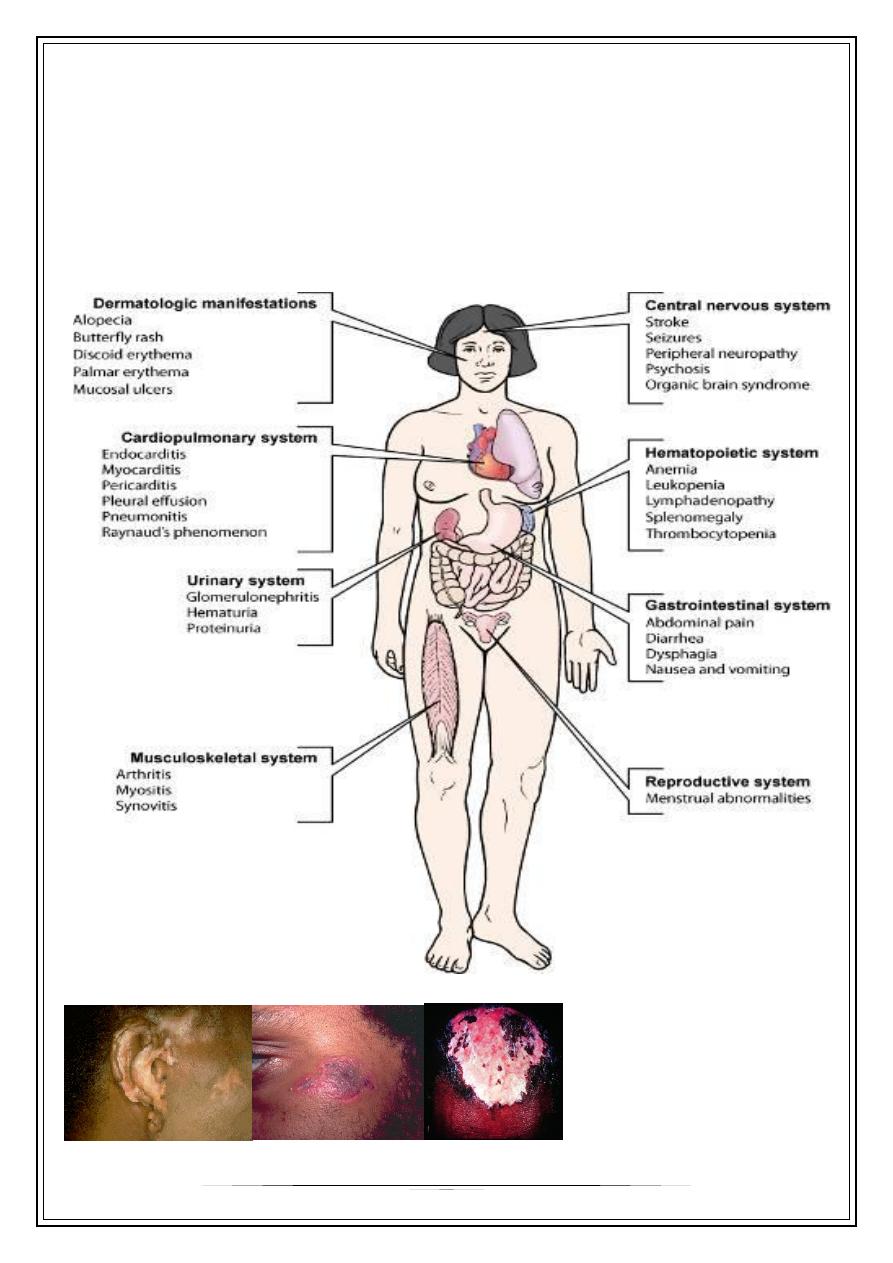
Systemic Lupus erythematosus
The classic presentation of a triad of fever, joint pain, and rash in a woman of
childbearing age should prompt investigation into the diagnosis of SLE
SLE is an autoimmune disease of unknown etiology, characterized by acute&
chronic inflammation of various tissues of the body.
Autoimmune diseases are illnesses that occur when the body’s tissues are
attacked by its own immune system.
Discoid Lesions:
s
2
MALAR RASH:
Jaccoud’s arthropathy:
SLE Around the World
˜
5 million people with SLE
o
40-80 of every 100,000
o
1.5 million Americans
o
16,000 new US cases annually
o
90% of cases occur in women
o
10X more susceptible
˜
Contributions from ethnicity
o
Incidence compared to Caucasians
•
3X higher for Asians
•
4X higher for African Americans (women)
o
Mortality compared to Caucasians
•
2X higher for Asians
•
3X higher for African Americans (women)
˜
Survival Rates
o
~90-95% in Western world
3
In such disease, the type of reaction is one of type 111 hypersensitivity reactions.
The age of presentation is usually in the second & third decades of life. About 10% of
cases may first occur in patients over 60 years of age& such patients may less often
present with malar rash, arthritis & nephritis.
Etiology
—
Etiology is unknown
Most probable causes:
Genetic influence
—
At least 35 genes are known to increase the risk of SLE.
—
A genetic predisposition is supported by 40% concordance in monozygotic twins; if
a mother has SLE, her daughter's risk of developing the disease has been
estimated to be 1:40, and her son's risk, 1:250.
Immunological factors Many immune disturbances, both innate and acquired,
occur in SLE
—
Studies of human leukocyte antigens (HLAs) reveal that HLA-A1, HLA-B8, and HLA-
DR3 are more common in persons with SLE than in the general population. The
presence of the null complement alleles and congenital deficiencies of
complement (especially C4, C2, and other early components) are also associated
with an increased risk of SLE
Environmental and exposure-related causes of SLE are
—
Silica dust and cigarette smoking
—
Administration of estrogen to postmenopausal women
—
Photosensitivity is clearly a precipitant of skin disease Ultraviolet light stimulates
keratinocytes, which leads not only to overexpression of nuclear
ribonucleoproteins
—
Vitamin D deficiency
—
Drugs
—
Numerous studies have investigated the role of infectious etiologies that may also
perpetuate autoimmunity. Patients with SLE have higher titers of antibodies to
Epstein-Barr virus (EBV), have increased circulating EBV viral loads, and make
antibodies to retroviruses
When the body cells die by apoptosis, the cellular remnants appear on the cell
surface as small blebs which carry self-antigens. These antigens include nuclear
constituents(eg. DNA and histones) which are normally hidden from the immune
system.in patients with SLE, removal of these blebs by phagocytes in inefficient so that
they are transferred to lymphoid tissues where they can be taken up by antigen-
presenting cells.
The self antigens from these blebs can then be presented to T-cells which in turn
stimulate B- cells to produce auto-antibodies directed against these antigens.
4
Diagnosis
—
Dx depends on the recognition of specific symptoms & identification of auto
antibodies. Antinuclear antibodies(ANA) are the best screening test. A positive
ANA test is not specific for SLE ,since it can occur in normal individuals & some
patients with other connective tissue diseases & viral infections.
—
A negative ANA makes SLE very unlikely but not impossible. Antibodies to double
stranded DNA (dsDNA) & to Sm are relatively specific for SLE. Anti-dsDNA occurs
in only 30-50 % of patients.
Revised American Rheumatism Association Criteria for SLE:
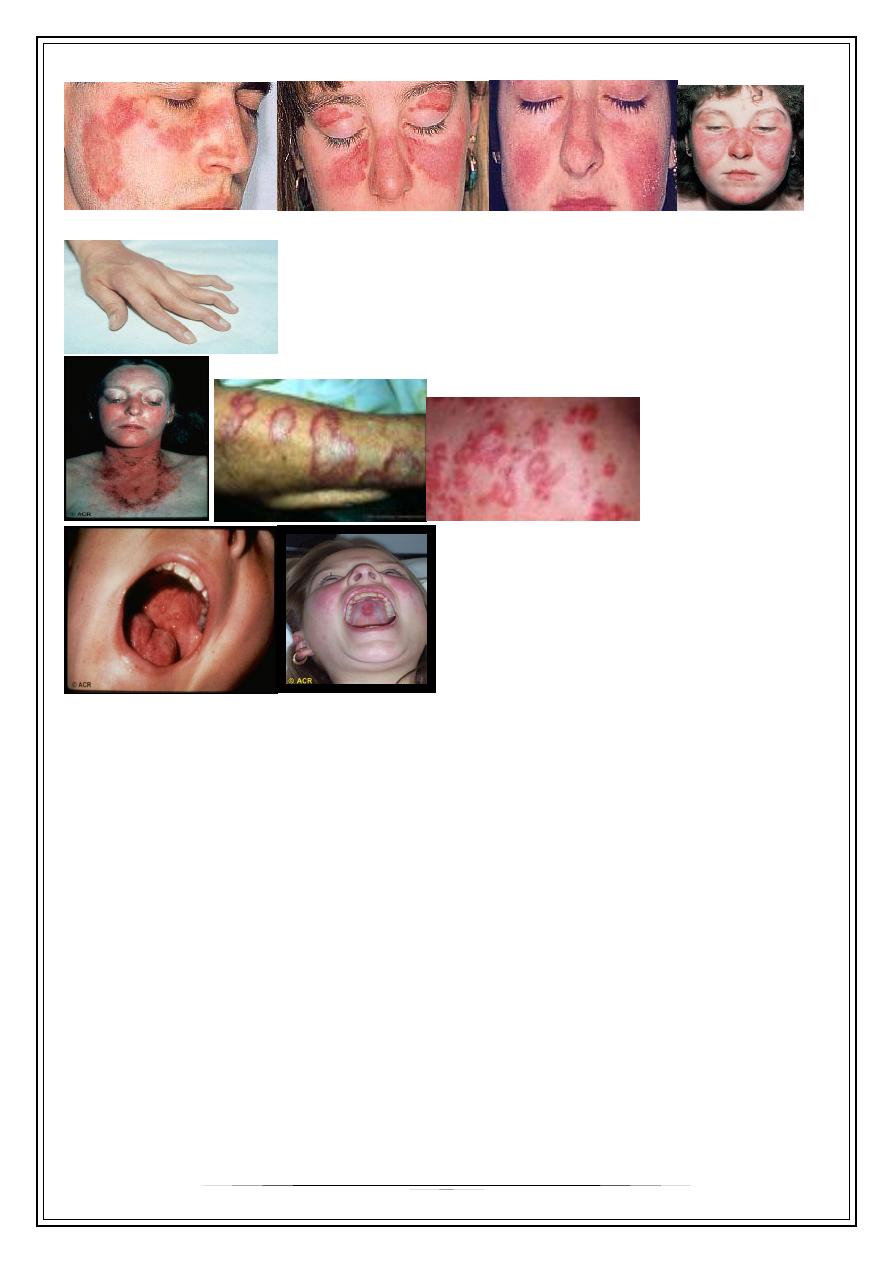
1-MALAR RASH: fixed erythema sparing the nasolabial folds, flat or raised over the malar
eminence.
2-DISCOID RASH: erythematous raised patches with adherent keratotic
scaling & follicular plugging, atrophic scarring may occur.
3-PHOTOSENSITIVITY: rash as a result of unusual reaction to sun light
4-ORAL ULCERS: include oral & nasopharyngeal, observed by physician. It may be
painless.
5-ARTHRITIS: nonerosive arthritis involving two or more peripheral joints, characterized
by tenderness, swelling, or effusion.
6-SEROSITIS: pleuritis or pericarditis documented by ECG or rub or evidence of
pericardial effusion.
7-RENAL DISORDERS: proteinuria greater than 0.5 g\d or greater than 3+ albumin, or
cellular casts(RBC, granular or tubular).
8-NEUROLOGIC DISORDERS: seizures without other cause or psychosis without other
cause.
9-HEMATOLOGIC DISORDERS: hemolytic anemia or leucopenia (less than 4000cell/ ml)
or lymphopenia (less than 1000cell/ml) or thrombocytopenia(less than 100000 ) on two
separate occasions in the absence of offending drugs.
10- Immunologic disorders: anti-dsDNA in abnormal titer, or anti-Sm antibodies or
positive anti-phospholipid antibodies or false positive VDRL.
11- ANTINUCLEAR ANTIBODIES: an abnormal titer of ANA s by immunofluorescence in
the absence of any offending drug.
If four of these criteria are present at any time during the course of the disease serially
or simultaneously, a diagnosis of SLE can be made with 98% specificity &97% sensitivity
2015 ACR/SLICC revised criteria for diagnosis of SLE:
Acute/subacute cutaneous lupus rash - Up to 2 points:
• Malar rash 2.p
• Subacute cutaneous Lupus erythematosus (SCLE) rash - 1.p
• Palpable purpura or urticarial vasculitis 1.p
5
• Photosensitivity 1.p
• Discoid lupus erythematosus (DLE) rash or hypertrophic Lupus rash 1.p
• Non-scarring frank alopecia 1.p
• Oral/nasal ulcers 1.p
• Joint disease 1.p
• Pleurisy and/or pericarditis 1.p
• Psychosis and/or seizure and/or acute confusion 1.p
Kidney involvement Up to 2 points:
• proteinuria≥ 3+ or ≥ 500 mg/day or urinary casts 1.p
• Biopsy-proven nephritis compatible with SLE 2.p
Hematologic Up to 3 points:
• WBC count < 4000/mm3 or lymphocyte count < 1500/mm3 on ≥ 2 occasions
or WBC count < 4000/mm3 along with lymphocyte count < 1500/mm3 in
one occasion 1.p
• Thrombocytopenia < 100,000/mm3 1.p
• Hemolytic Anemia 1.p
• Positive anti-Sm 2.p
• Anti-phospholipid antibodies (aPLs) 1.p
• Low serum complement (C3 and/or C4 and/or CH50) 1 p.
Serologic tests Up to 3 points:
• Low titer positive ANA 1.p
• High titer positive ANA with homogenous or rim pattern 2.p
• Positive anti-ds DNA 2.p
The patients with 4 points out of 16, have definite diagnosis of SLE. With 3 points
highly suggestive SLE, with 2 points probable SLE and with one point possible SLE are
the diagnosis
—
ACR/SLICC=American College of Rheumatology/ Systemic Lupus International Collaborating
Clinics
Clinical Features:
—
Raynaud's phenomenon: common in SLE ,more than other arthropathies.
—
MSK features: joint deformities are rare. Deformity that occur result from tendon
inflammation & damage rather than from bone erosion(jaccoud's arthropathy).
—
Mucocutaneous features: painful oral ulcers are common in SLE. Diffuse non-
scarring alopecia is common, & indicate active disease.
6
3 main types of rash in SLE:
1- classic butterfly facial rash( 20-30% of patients)
2- sub acute cutaneous lupus erythematosus rash (SCLE):
Migratory, nonscarring papulosquamous(psoriaform) or annular
3-discoid lupus:
hyperkeratosis& follicular plugging& may cause scarring alopecia if
present on the scalp.
Other lesions include vacsulitis & livedoreticularis.
—
Renal features : one of the determinants of prognosis.
*SLE accounts for 5-10% of patients with nephrotic syndrome & could be the
presenting feature without other systemic manifestations. It should be suspected
in young female with protein urea & hematuria with low complement.
*Virtually all SLE patients have renal injury on renal biopsy .
*Nephrotic syndrome with nephritic sediments is the most common& 10-15% of
patients have azotemia, with numerous crescents seen on renal biopsy
*WHO had classified lupus nephritis into 5 categories(classes) according to
histopathology & clinical presentation:
•
Class 1- normal
o
accounts for < 5% of SLE patients.
•
Class2- mesangial
o
10% azotemia
•
Class3- focal proliferative
o
20% azotemia, 15% nephrotic syndrome
•
Class4- diffuse proliferative
o
50% frequency , 75% azotemia, 90% nephrotic syndrome
•
Class 5- membranous
o
100% protein urea, 20% azotemia, 90% nephrotic syndrome
*Patients with renal SLE tolerate DIALYSIS & for reasons that are not yet
understood patients placed on chronic dialysis often note dramatic amelioration of
other manifestations of SLE.
*Renal transplantation is also well tolerated with recurrence after transplantation
being relatively rare.
Cardiopulmonary features:
*The main feature is chest pain from pleurisy or pericarditis, myocarditis, &
libman-sacks endocarditis may also occur. The latter is due to non-infectious
vegetations, usually seen in patients with positive antiphospholipid antibodies.
Such patients may also have increased risk of venous thrombosis .
7
*Alveolitis & lung fibrosis occur especially in patients with overlap syndrome.
CNS features:
*Specific features of cerebral lupus include visual hallucinations, chorea, also
associated with antiphospholipid syndrome, organic psychosis, transverse
myelitis& lymphocytic meningitis.
Hematological features:
*Antibody- mediated destruction of peripheral blood cells may cause neutropenia,
lymphopenia, thrombocytopenia or hemolytic anemia. The degree of leucopenia
often with lymphopenia is a good guide to disease activity. ESR is increased but
CRP is normal unless there is serositis or infection. .
*Other manifestations of SLE like fever, Wt loss & lymphadenopathy commonly
accompany active disease. GIT involvement is rare. Chronic fatigue &other
features of fibromayalgia affect up to 80% of patients. These features are
unresponsive to steroids but can be managed with low dose amitriptyline& graded
exercise therapy.
*Note: drug- induced lupus erythematosus is encountered in clinical practice,&
procainamide, isoniazid& hydralazine are responsible for the majority of the cases.
Although multiple organs are affected, nephritis& central nervous system are not
ordinarily present. Antihistone antibodies are characteristic for drug induced lupus
but are not specific for this syndrome.
*Clinical manifestations & many laboratory features return to normal after the
offending drug is with drown.
Management
1- all patients should be educated to avoid sun light & ultraviolet light & use of high
factor sun blocks(sun protection factors) .
2- patients with mild disease need NSAISs & analgesia.
3- patients with more troublesome cutaneous& joint symptoms require
hydroxychloroquine 200-400 mg/ day
4- short courses of oral steroid for mild-moderate disease activity( rash, synovitis,
pleuropericarditis)
5- acute or life threatening disease ( renal , cerebral) require high dose steroids e.g.
oral prednisolone 40-60 mg daily or IV methylprednisolone 500mg-1 gm in
combination with IV cyclophosphamide.
—
In SLE nephritis, pulse IV cyclophosphamide is more effective than pulse IV
methylprednisolone alone, & combination therapy is more effective.
—
Continuous quarterly IV treatment for one year after renal remission decrease the
risk of renal flares.
8
—
Other immunosuppressive drugs like azathioprine, methotrexate, cyclosporine,
tacrolimus& mycophenolate mofetil are useful either alone or in combination with
steroids for sever but non life threatening manifestations or as step down therapy
after cyclophosphamide.
—
Patients with SLE& anti-phospholipid syndrome who have previous thrombosis
require life long warfarin.
—
If the thrombosis occurs in spite of warfarin treatment, the INR ratio should be
increased to 2.5-3.5
—
Fertility rates are normal in patients with SLE, but spontaneous abortions are
frequent.
—
Treatment of pregnant ladies with history of fetal loss & or antiphospholipid
syndrome includes daily low dose aspirin until the last month , daily low dose
aspirin plus daily high dose steroids, or twice daily SC heparin in full
anticoagulating dose. Disease flares in small proportion during pregnancy.
Lupus and pregnancy
—
Infertility can result from SLE treatment regimen.
—
SLE is associated with complications of pregnancy.
—
Pregnancy & post partum can cause exacerbations of SLE.
—
Women with serious SLE should be counseled against pregnancy….
Differential diagnosis
—
Rheumatoid arthritis,
—
Dermatitis,
—
Neurological disorders such as multiple sclerosis & psychiatric disorders&
—
ITP.
Mortality in Lupus - Bimodal Peaks
Early:
—
Increased disease activity
—
Infections due to immunosuppression
Late:
—
Deaths the result of permanent damage: treatment side effects, atherosclerosis
with CAD and heart attacks, strokes, pulmonary, end-stage renal disease (ESRD),
etc
9
Prognosis
5years survival is more than 90% , 10 years survival is 80%,& 70% survival at 20
years. The fallowing factors are associated with poor prognosis:
—
High serum creatinine
—
Hypertension
—
Nephrotic syndrome
—
Anemia
—
Hypoalbuminemia& hypocmplementemia at the time of diagnosis
—
Thrombocytopenia
—
Low socioeconomic status
—
CNS involvement
Thank you,,,
