DR. HADAF ALJUNAIYEH

– A common inflammatory disease of skin
– Chronic relapsing condition
– Unpredictable course
– Has a great impact on patient’s life
Emotional impact
1-Depression
2-Unattractiveness
3-Fear about future
& prognosis
Wrongly assumed to be contagious
Embarrassment in public places & hair
dressers

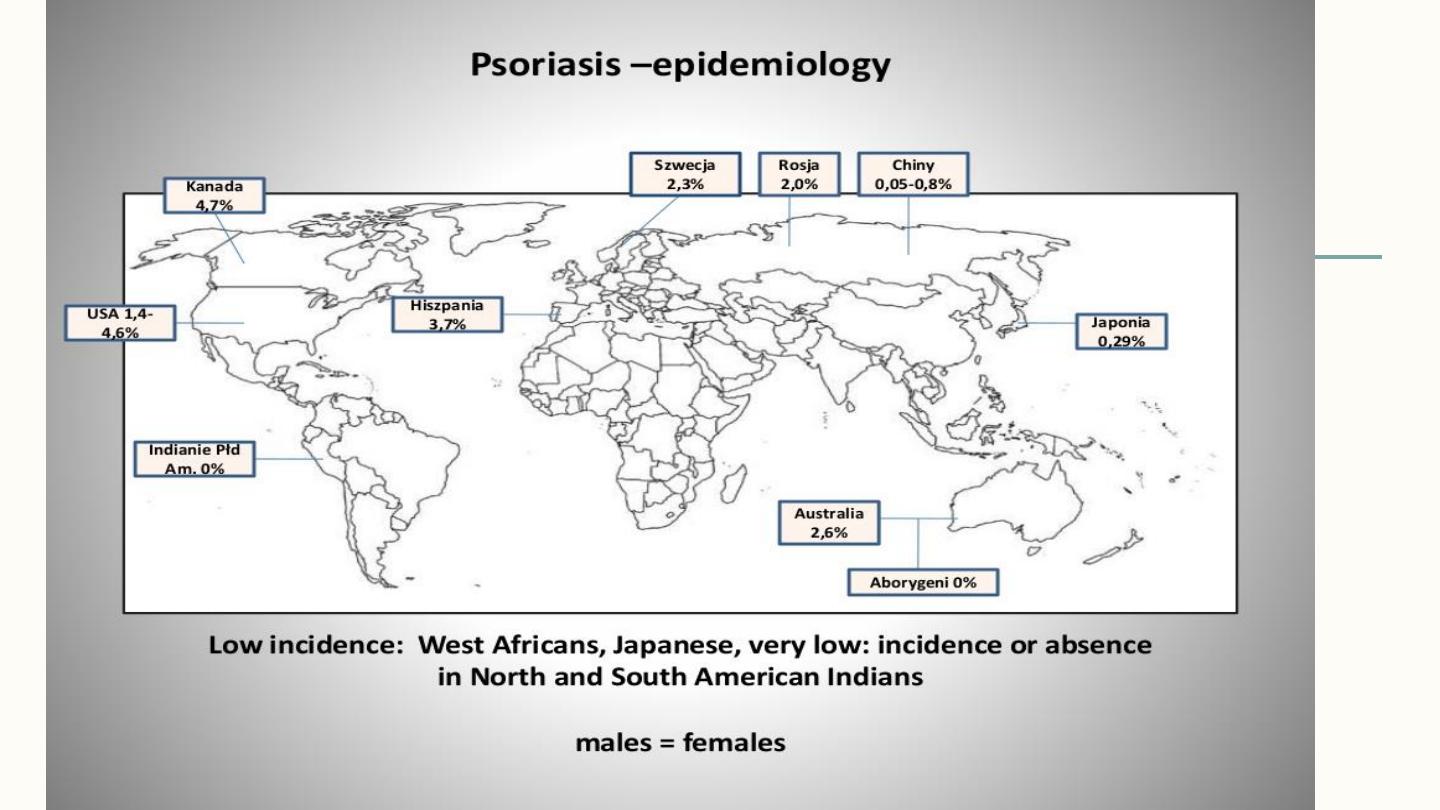
epidemiology
– Prevalence 0.3-25%
– Equal male & female ratio
– Estimated incidence 60 per 100000 per year

Age of onset
Mean age of onset 23-37
2 peaks with possible genetic associations
1-
early onset 16-22 with more severe & aggressive
presentation & possible first degree relative affection
2
_
late onset 57-60 which is milder & absent first degree
relative involvement

pathogenesis
2 key pathophysiological aspects:
1)Increased rate of keratincytes proliferation+ parakeratosis.
2) large inflammatory cell infiltrate as polymorphs, T cells, &
others.
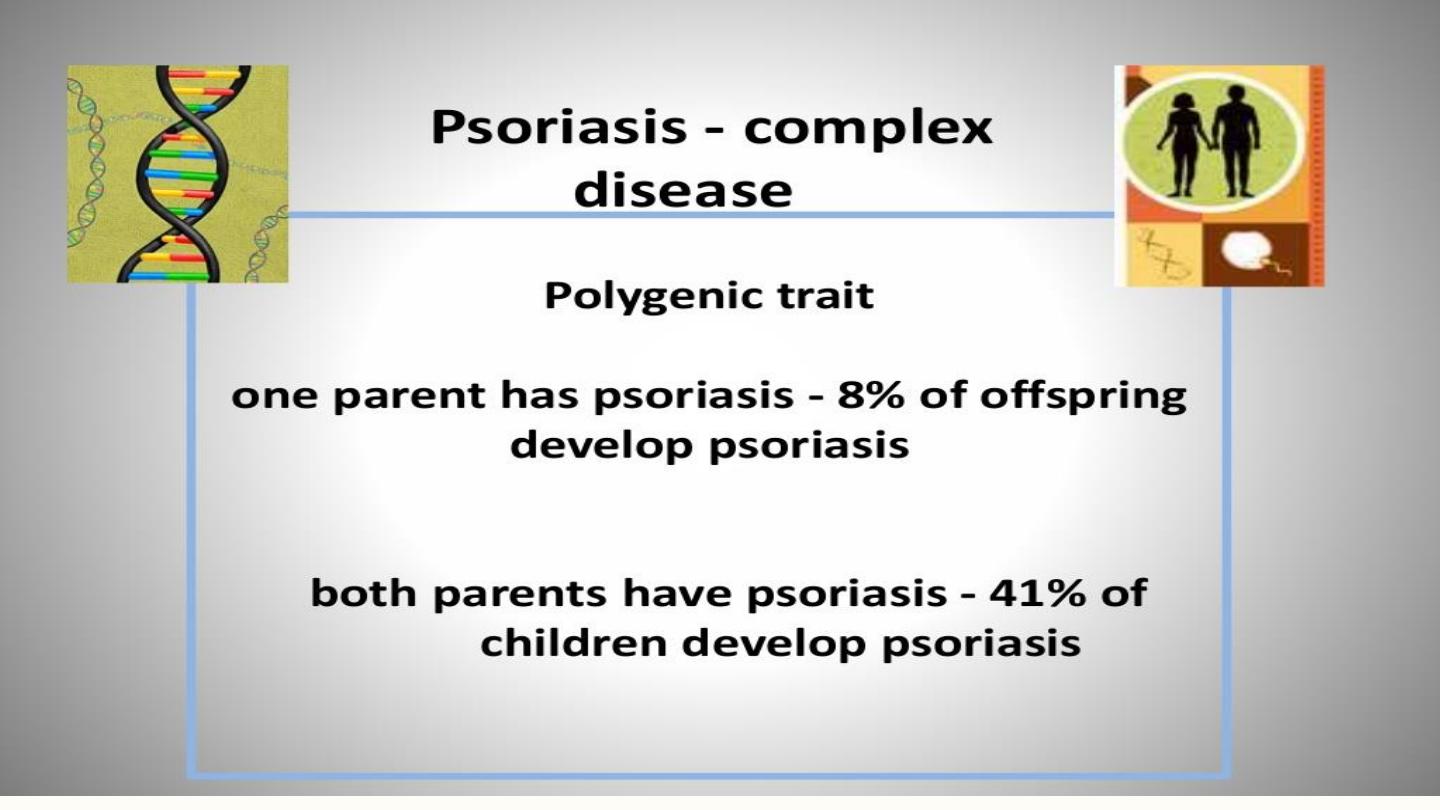
Familial component, many relatives affected, increased in
successive generations, multifactorial inheritance.

Psoriasis is a T cell mediated
auto-immune disease
Current hypothesis:
– Unknown skin antigen stimulate immune response
– Antigen-specific memory T cells are primary mediators
– Leading to impaired differentiation & hyper proliferation of
keratinocytes

Triggering factors in susceptible patients
– 1-Infection:
β hemolytic strept.
Throat infection
precede guttate
psoriasis.

2-Trauma:
positive Kobner’s phenomenon
3)emotion:
in 50% stress worsen psoriasis
especially in children
4- Drugs:
antimalarials, lithium,
β blockers worsen
psoriasis, stopping
steroids causes
rebound of the rash.
– Metabolic
5-

6-Hormonal
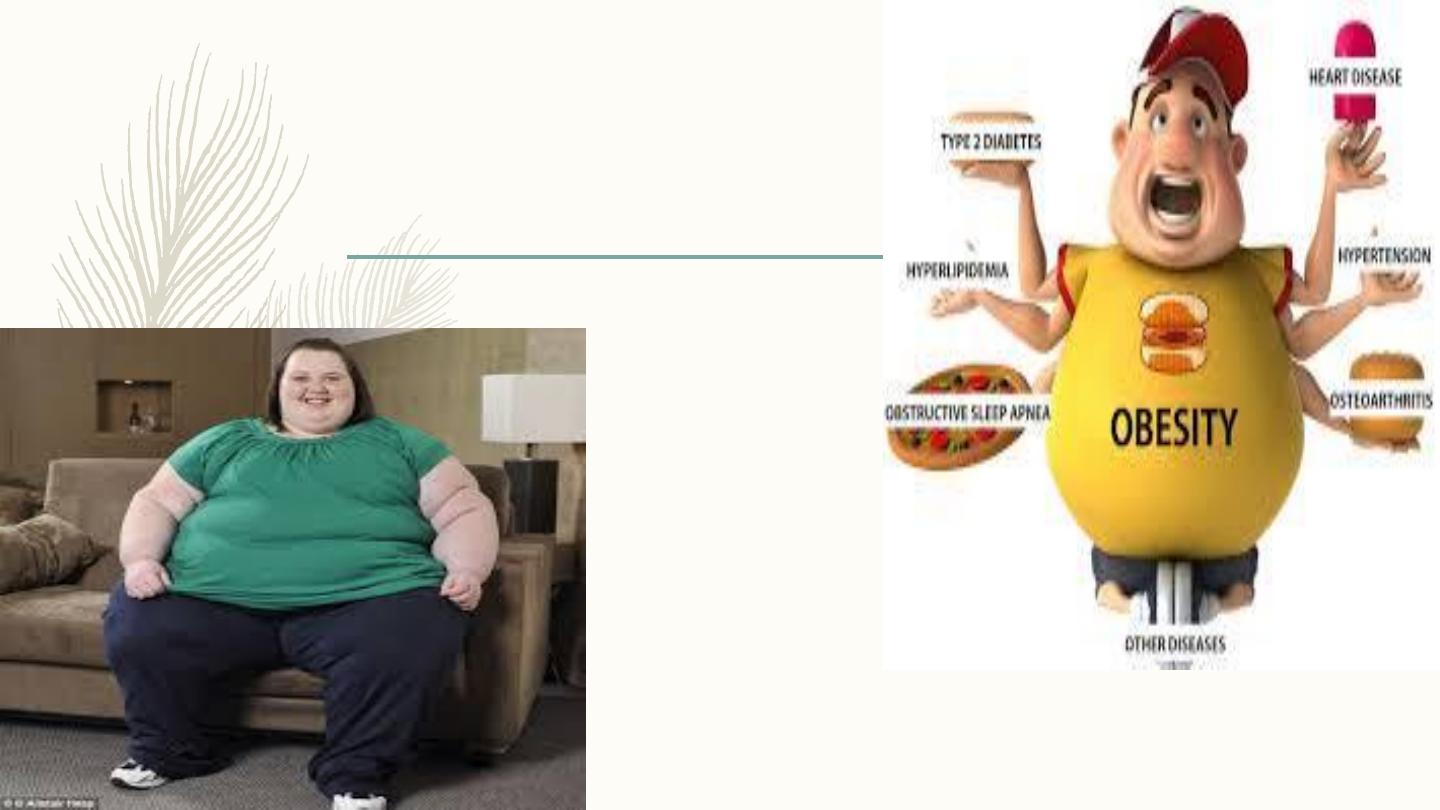
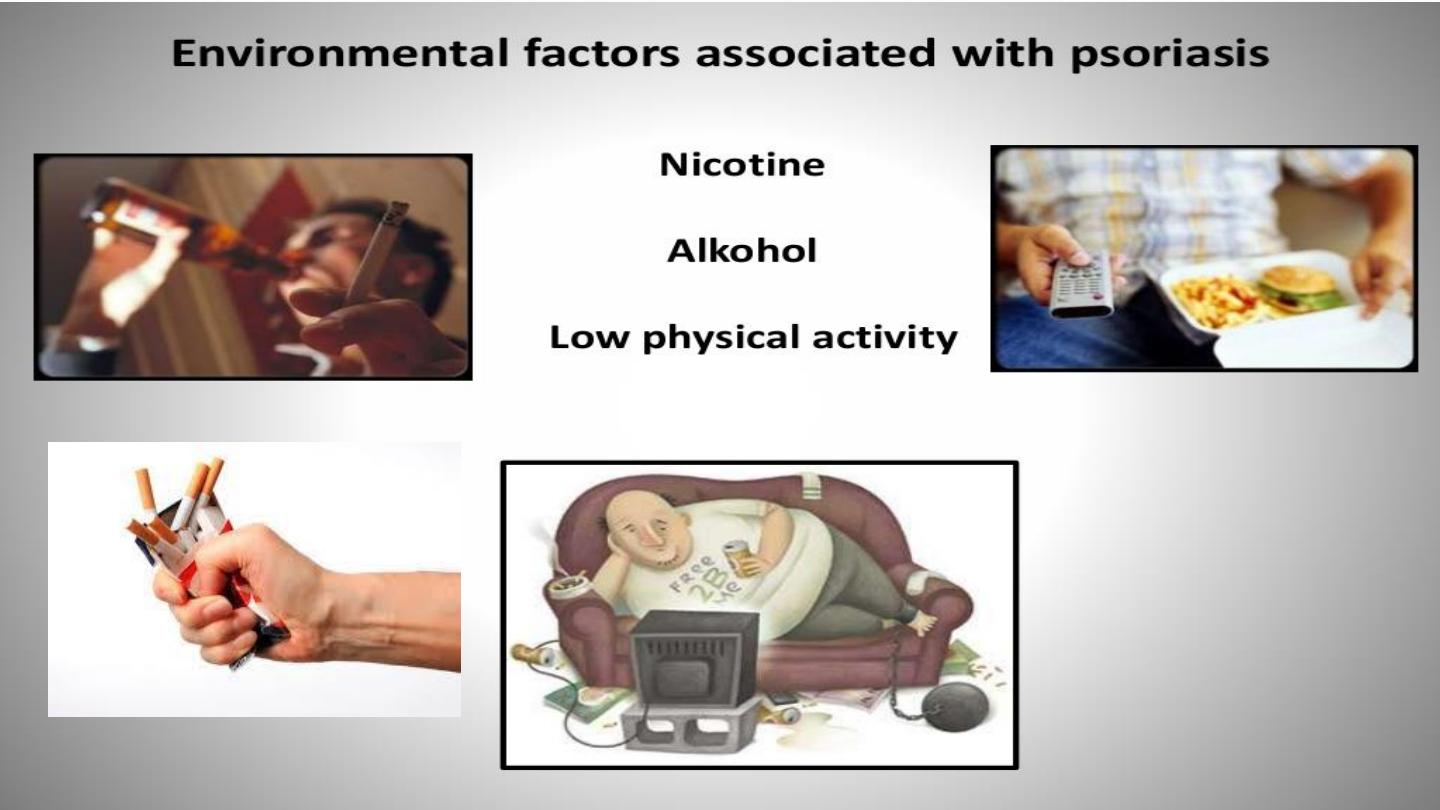
Role of obesity
– doubles the risk of psoriasis
– BMI correlate with psoriasis severity

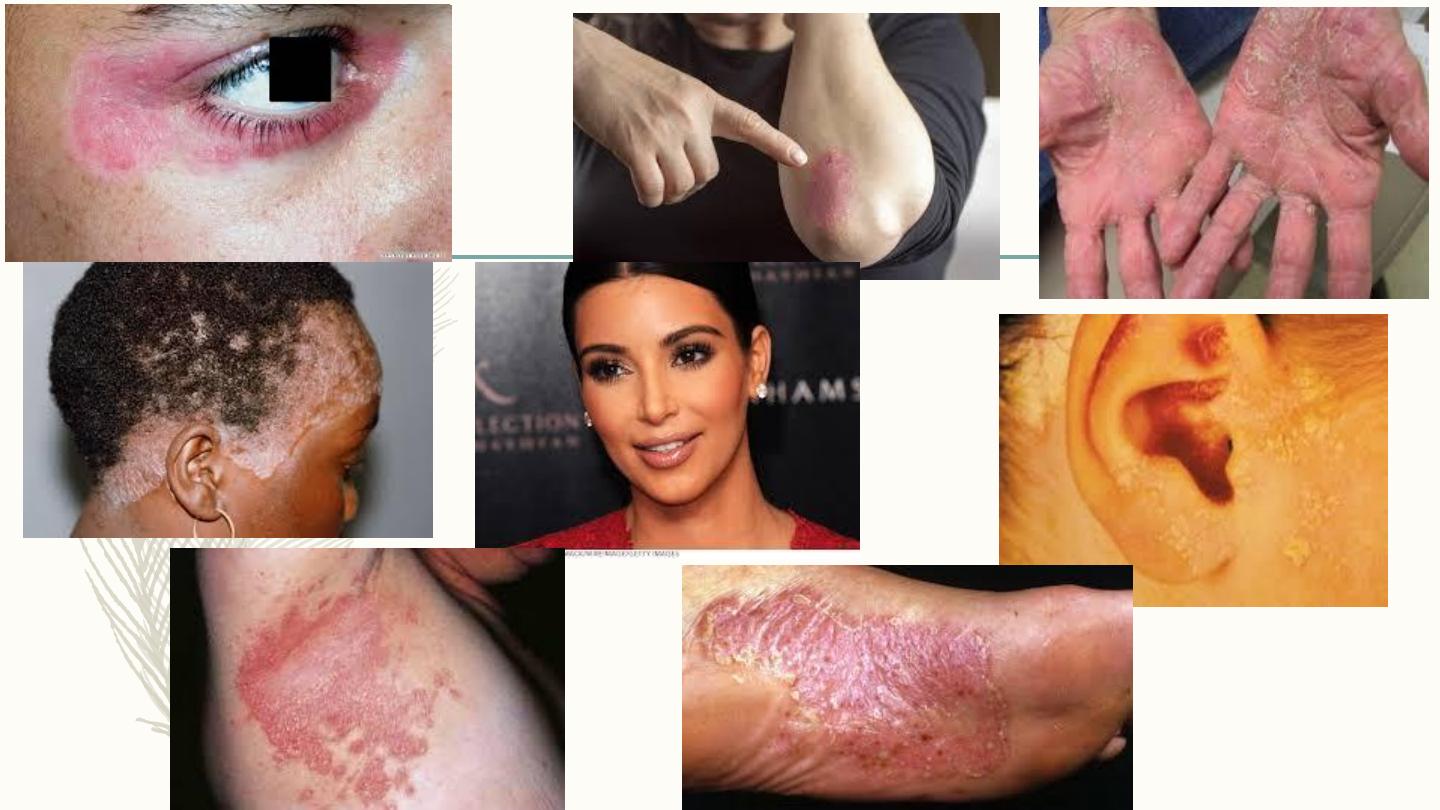
Clinical features
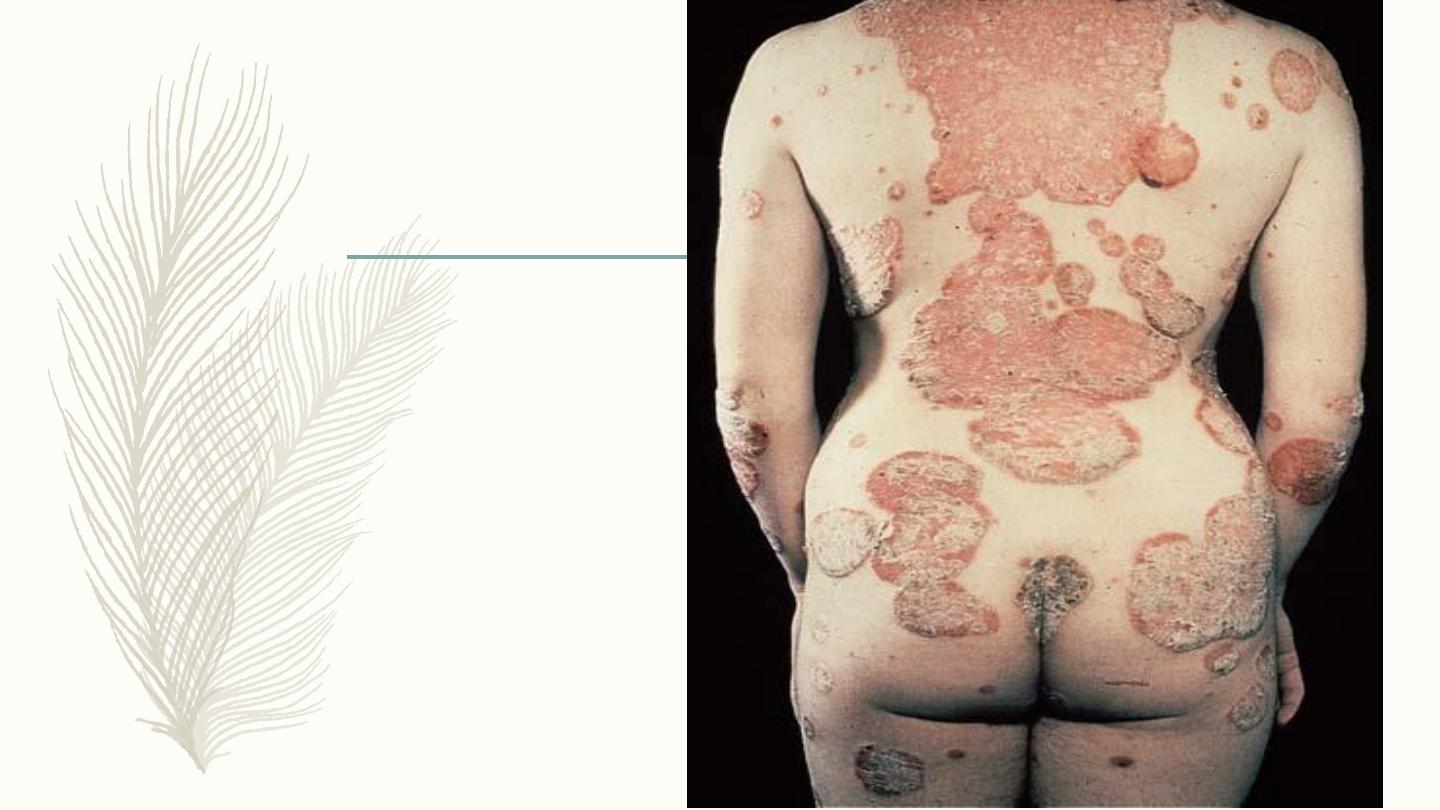
Well-demarcated, sharply defined
erythematous (salmon pink)
plaques covered by silvery
white scales
Usually symmetrical
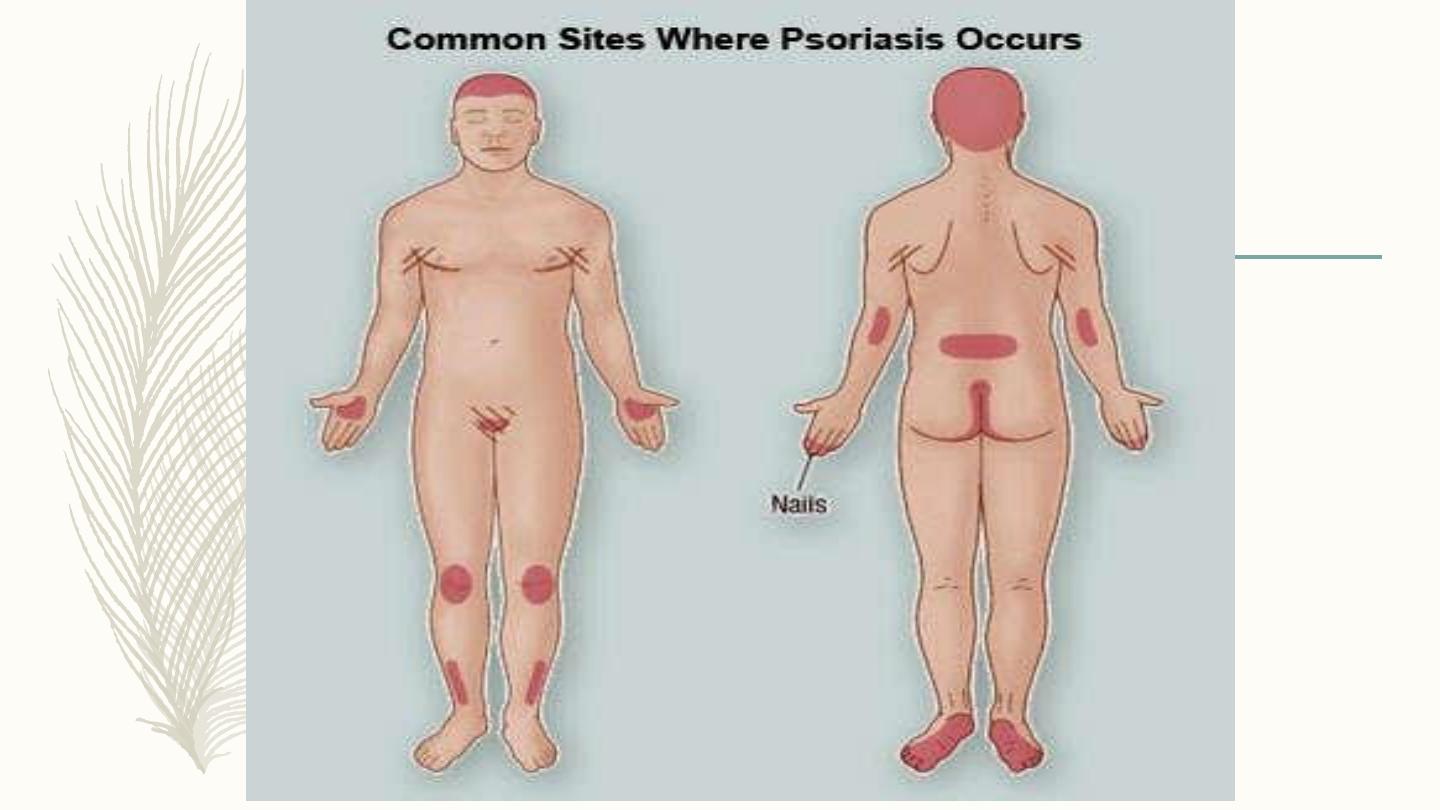

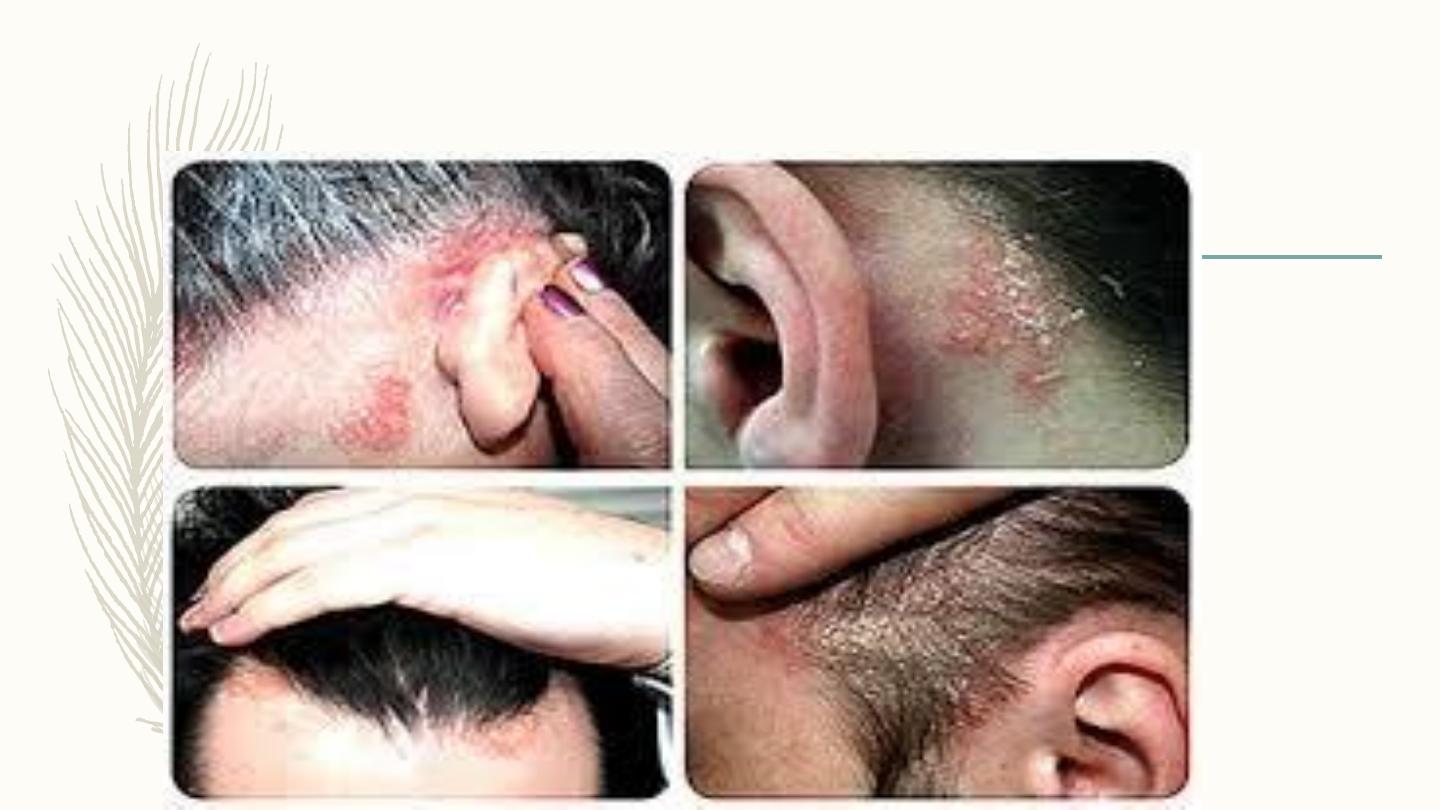
Scalp psoriasis


Koebner’s phenomenon

The commonest complaint is
scaling
– scaling
Followed by:
– itching

Third is
– Redness of skin
Next is
– Tightness of skin
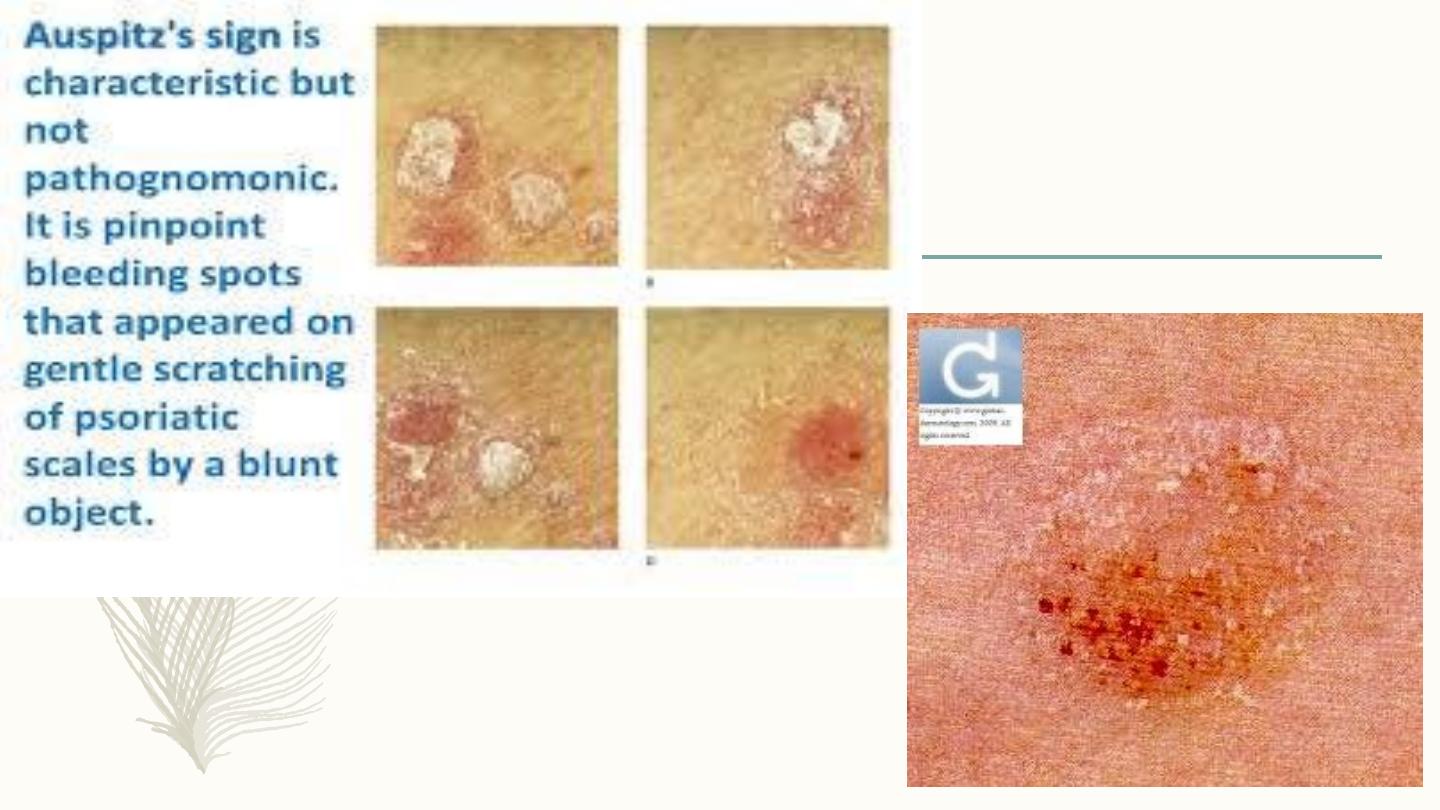
Bleeding
is the 5th

Burning
the 6
th
complaint
Last is
Fatigue
Types of psoriasis
– Chronic plaque psoriasis
– The commonest type 85%
– Can be extensive

Guttate psoriasis
– Numerous small lesions about 1cm
– Usually less scaly
– Trunk & proximal limbs
– Usually patients less than 30
– Often preceded by strept URTI.
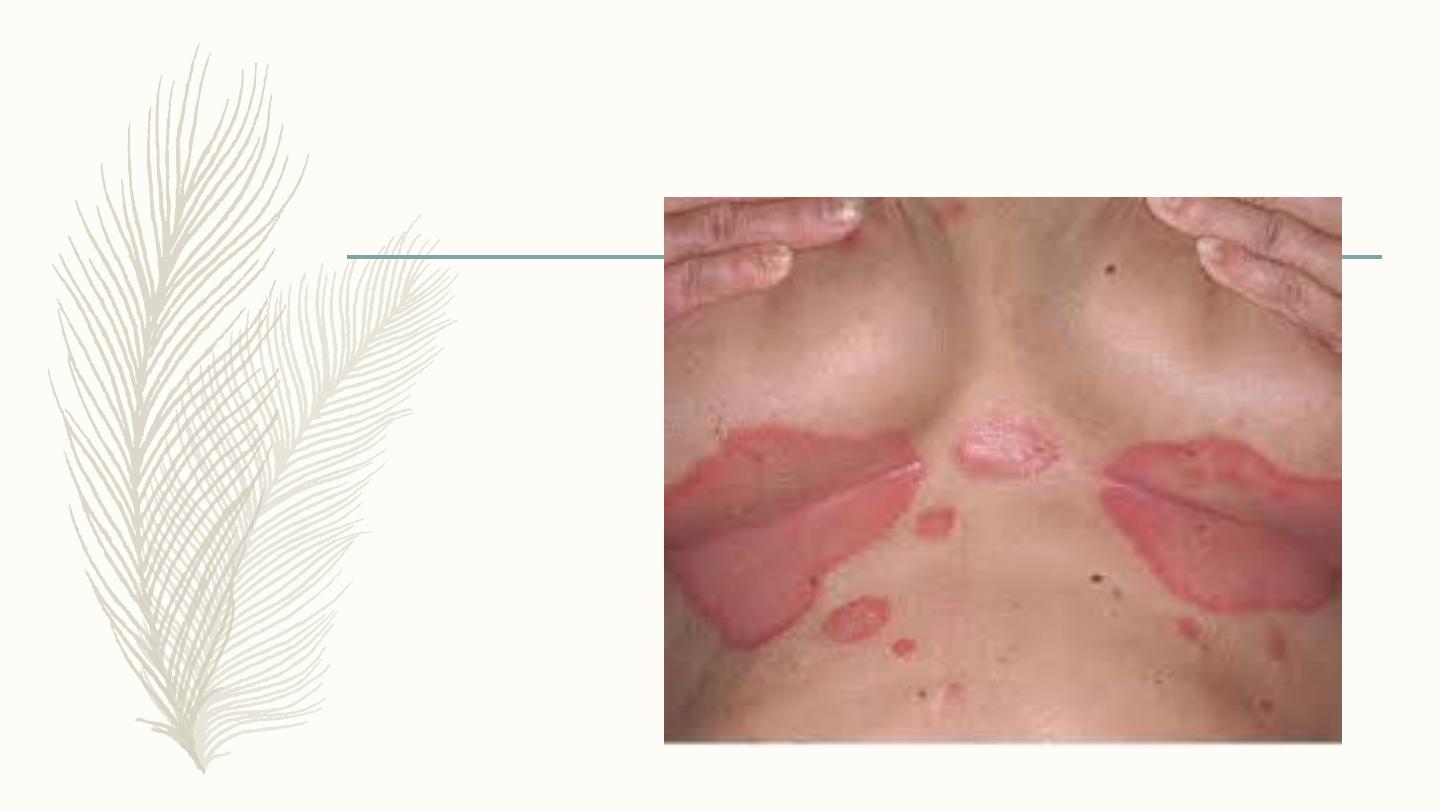
Flexural psoriasis
– In body folds
– Less scaly
– Often miss DX if no
other signs of psoriasis

Napkin psoriasis
– 2-8 months old babies
– disappear by topical treatment
– Might reappear in adult life.
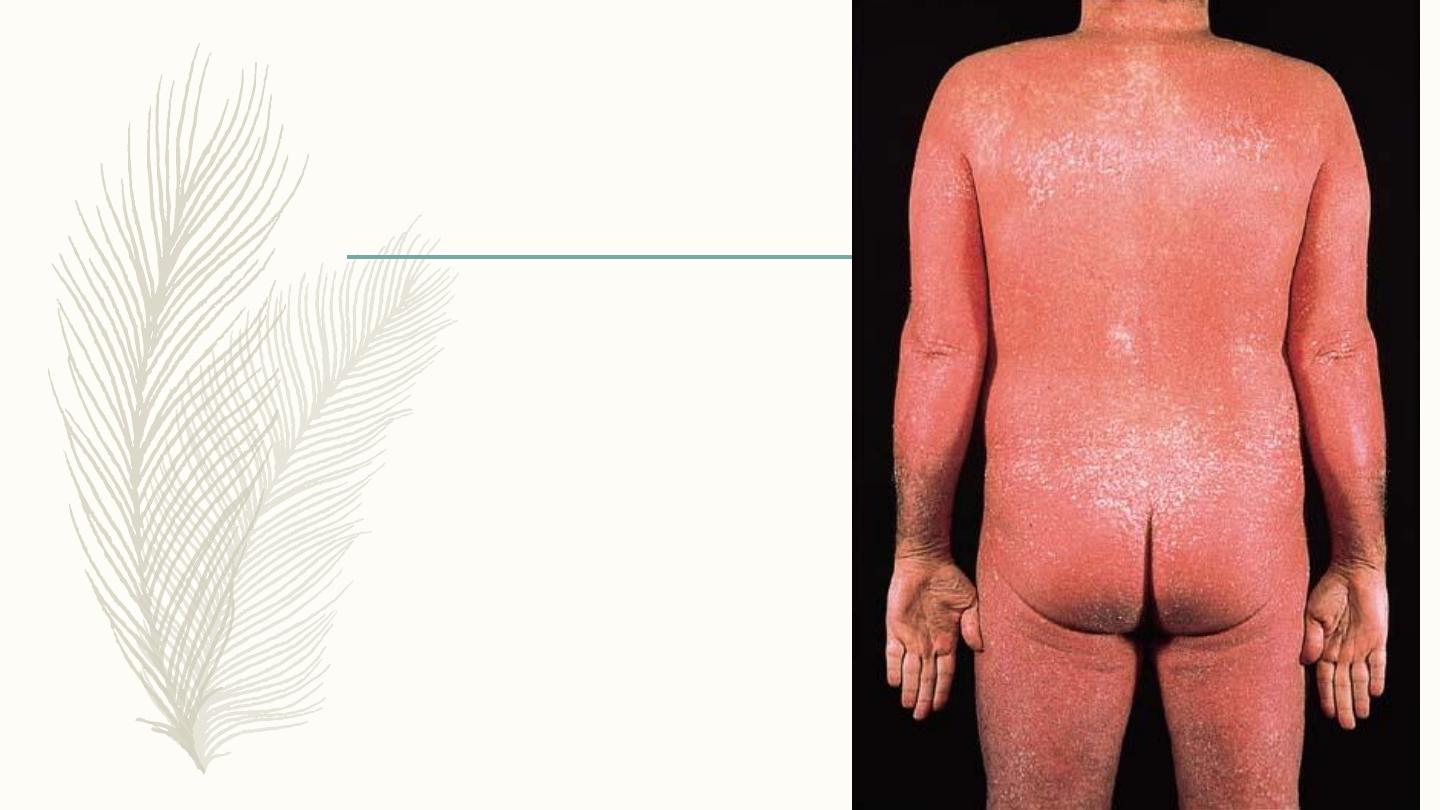
Erythrodermic psoriasis
– Uncommon
– More than 90% of skin surface
– Can evolve from chronic or eruptive
– Fever, hypo & hyperthermia,
dehydration
– Complications: Heart failure,
infections, malabsorption, & anaemia

Pustular psoriasis
– Localized:
more common
On palms & soles
– Generalized:
Associated with fever

Palmoplantar psoriasis
– Can be hyperkeratotic or
pustular
– Difficult to distinguish from
chronic eczema or tinea
May be aggravated by trauma


Nail changes in psoriasis
1) Distal onycholysis.
2) Random pitting from parakeratosis of proximal matrix.
3) Oil spots which are yellow areas of subungual
parakeratosis
4) Salmon patches due to nail bed psoriasis.
5) Subungual hyperkeratosis resembling onychomycosis.

Nail psoriasis

Psoriatic arthritis
• In 5-10% of psoriatics
• Rare before age 20
• Rheumatoid factor -ve arthritis
• 5 types either peripheral or central, often
overlap

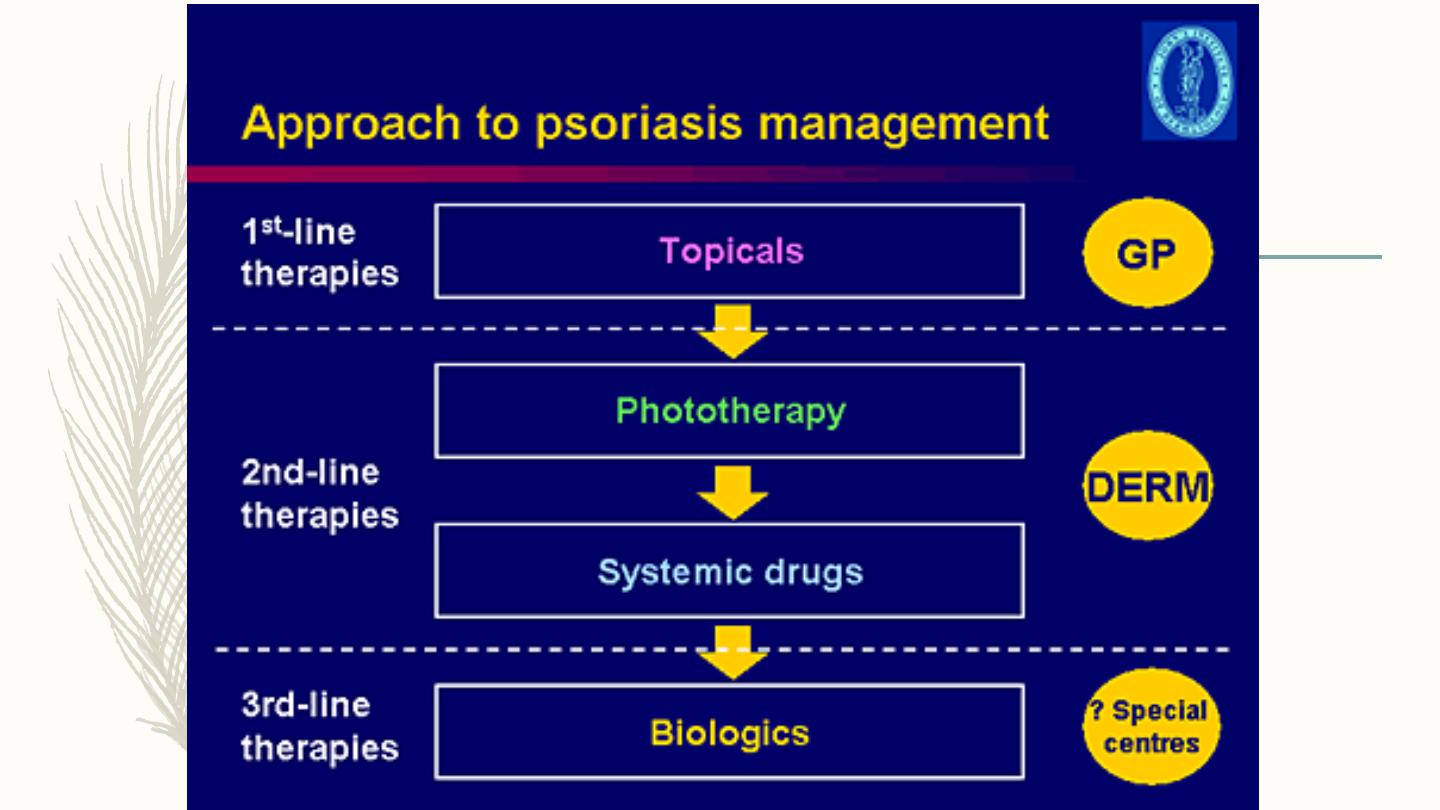
Treatment
– Reassurance, explanation are vital
– Psoriasis is not contagious
– No cure, so the aim is to induce remission or making it more
tolerable
– Spontaneous remission in 50% of cases
– Quit smoking
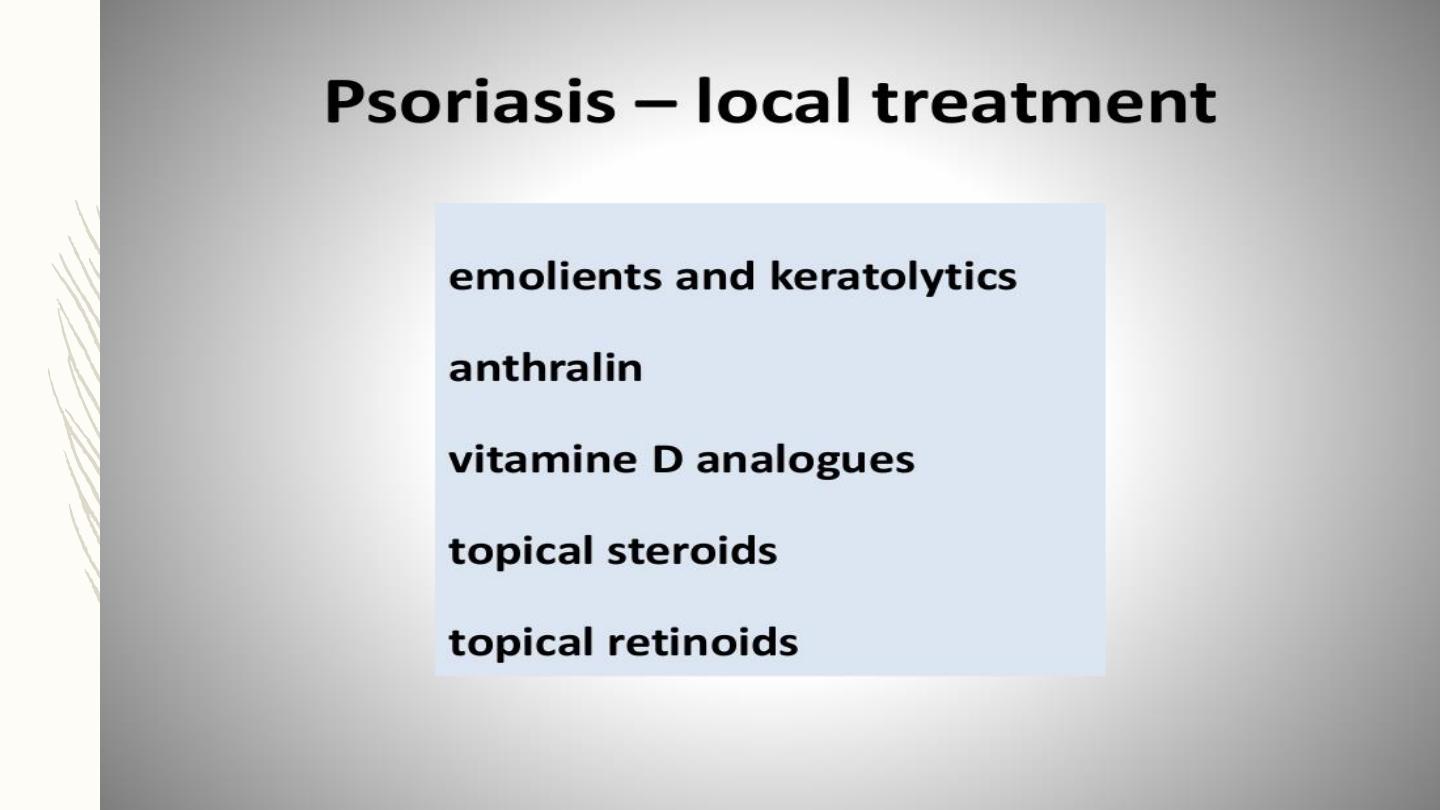

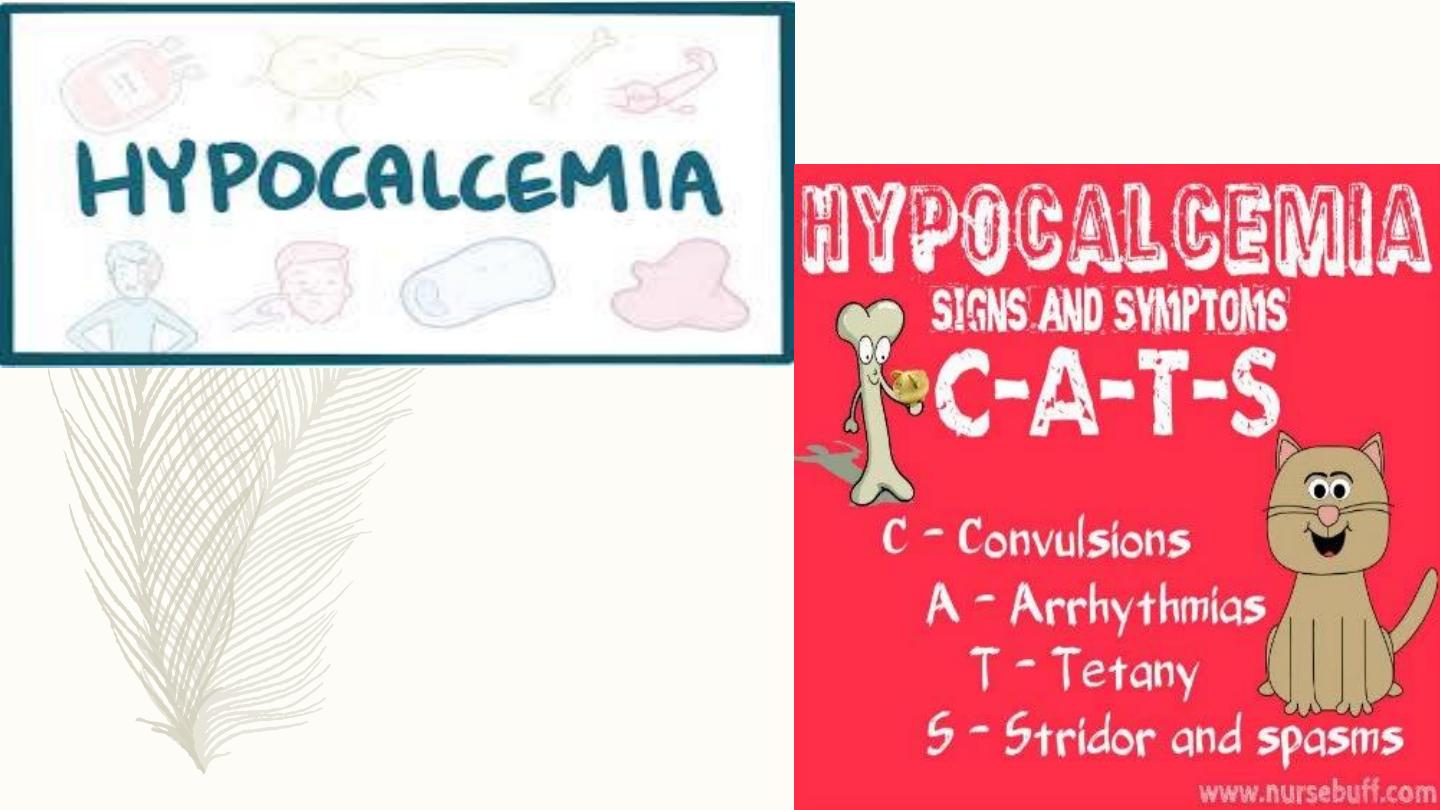
calcipotriol
– vitamin D agonist, only reduce thickness & scaling of the plaques
– Irritant so combined with steroid to get a greater response, fewer
S.E., +steroid sparing

Topical corticosteroids
– Most commonly used
– clean & effective
– but frequent S.E.
1-as dermal atrophy
2-tachyphylaxis
3-early relapse
4- precipitation of pustular type

Indications of topical steroids:
1)On face, ears & flexures
2) Patients can’t tolerate tar, dithranol, etc, due to
allergic or irritant reaction
3)Unresponsive psoriasis of scalp, palm & sole
4) Patients with minor, localized type
5) In combination with other modalities

Light therapy
– Most patients benefit from sunlight
– UVR is the main treatment for moderate to severe psoriasis.
– S.E. include sunburn & increased risk of skin CA
– Artificial UVB by fluorescent bulbs, either narrow band(311nm.)
or broad band
– Max. effect achieved at MED (min. dose to induce erythema in a
test patch after 24h)
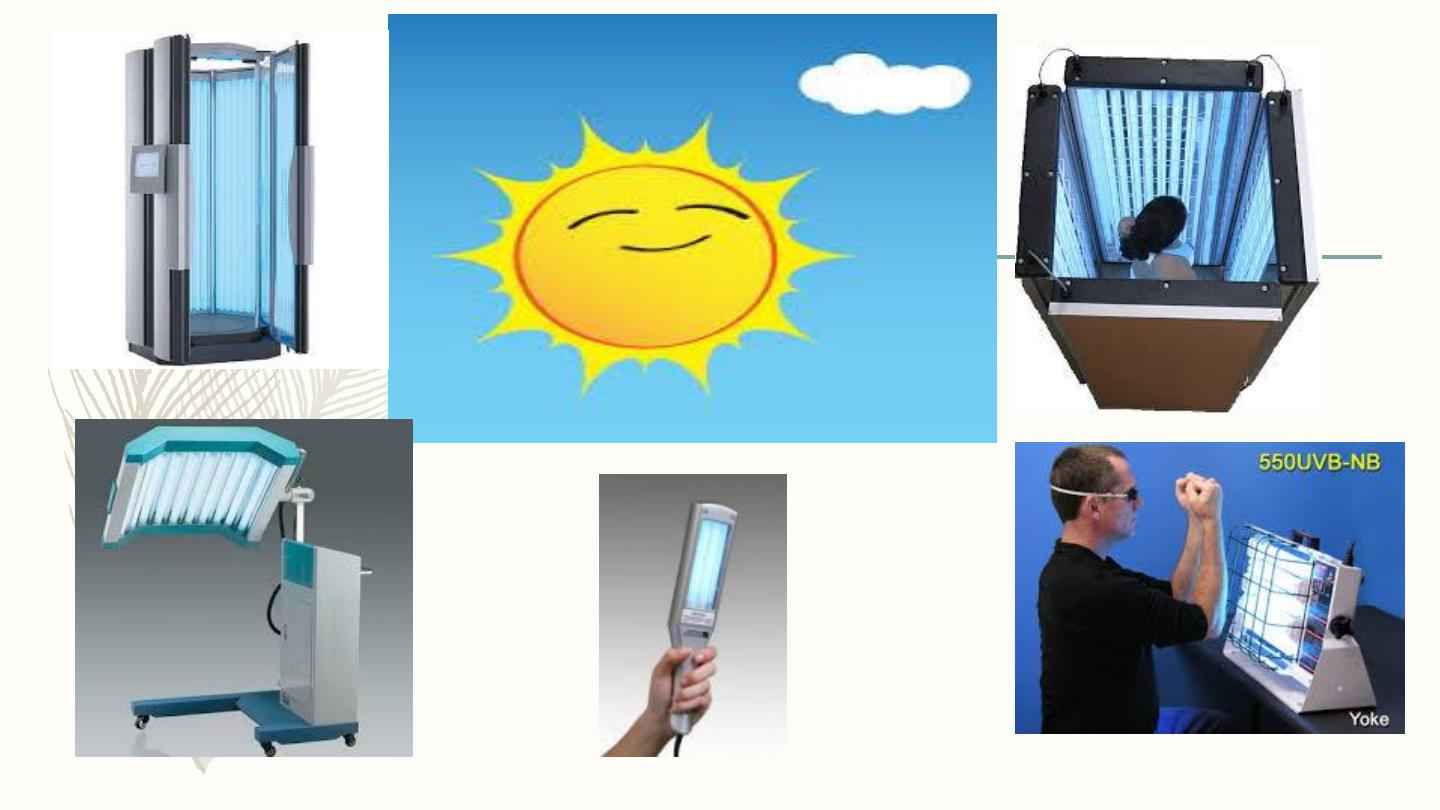

PUVA
– Psoralens are natural phtosensitizers
– High intensity, long wave UVR( UVA), given 2 hours after
ingestion of 8-methoxy psoralen, twice weekly
– 20-25 sessions are needed, +maintenance doses
– Clearance ‘ll occur in 75% of patients
– Not for young patients
– UVR resistant glasses worn for24 hours


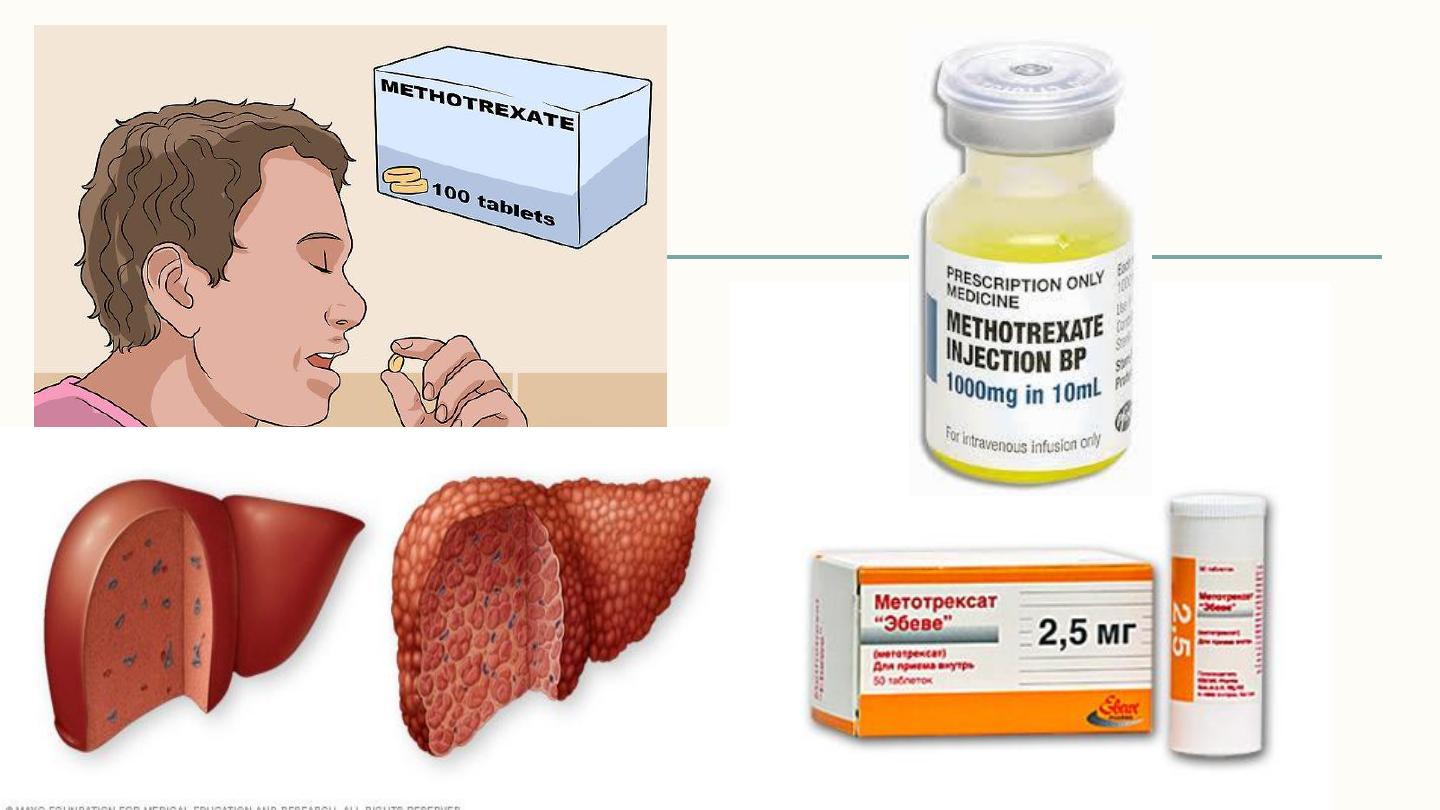
Methotrexate
• Folic acid antagonist, inhibit DNA synthesis in S phase
• Given orally or parentally , 7.5-15mg, once weekly
• Minor S.E. nausea & malaise in 1
st
.24hr.
• Serious S.E. are liver toxicity, marrow suppression,
teratogenicity & male oligospermia
• Should monitor liver, renal & marrow function, before &
during treatment

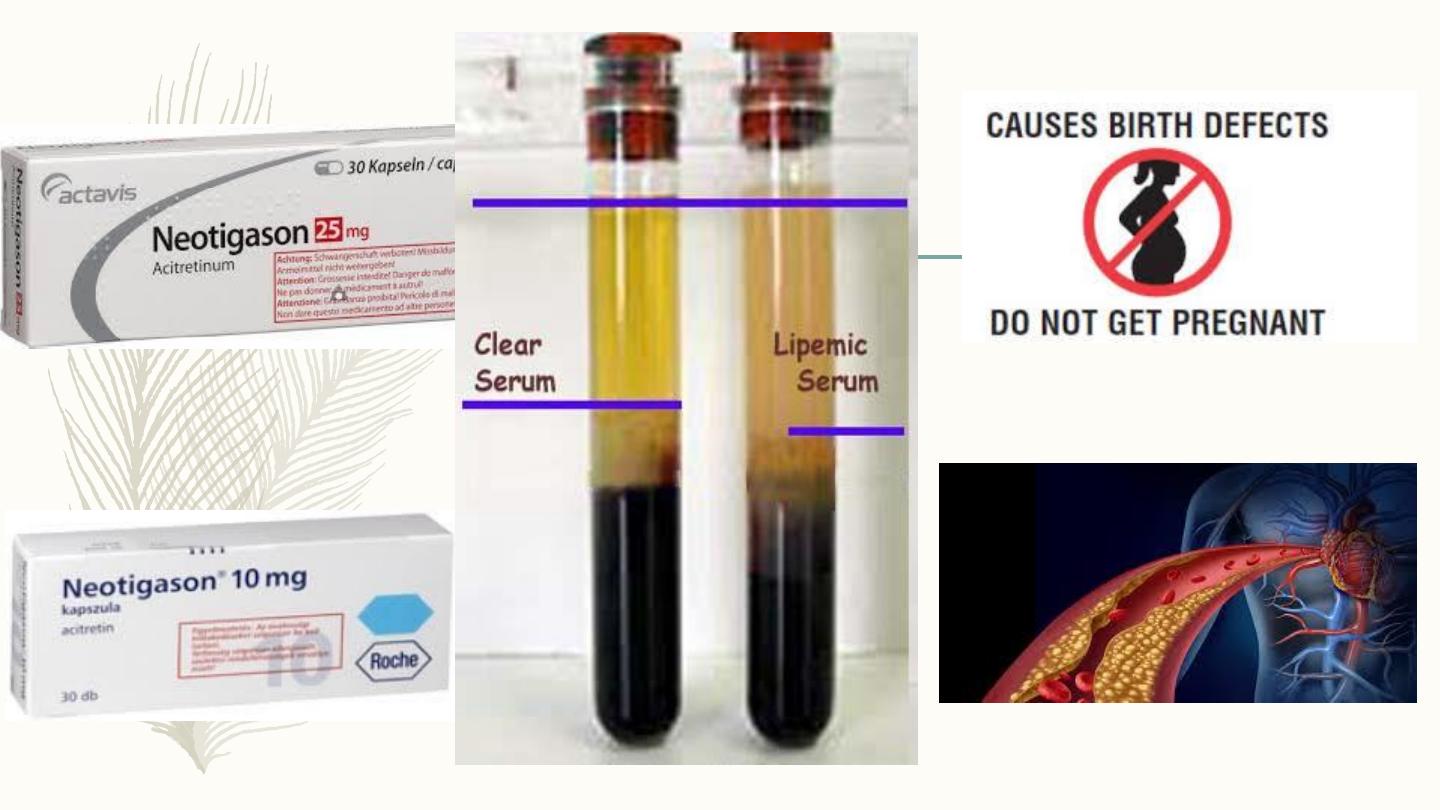
Neotigasone (=Acitretin)
– Acitretin is vitamin A analougue
– Especially effective in pustular psoriasis of palms& soles, also
in plaque psoriasis.
– Frequent minor S.E. as dryness of skin & m.m., pruritis, hair
fall, & paronychia.
– Serious S.E. are hyperlipidemia especially of triglycerides &
teratogenicity
– Can be combined with PUVA

Cyclosporine
– Inhibits cell mediated immunity
– Very effective in psoriasis
– Serious S.E. as hypertension, renal damage,
persistent viral warts & a risk of skin cancer.


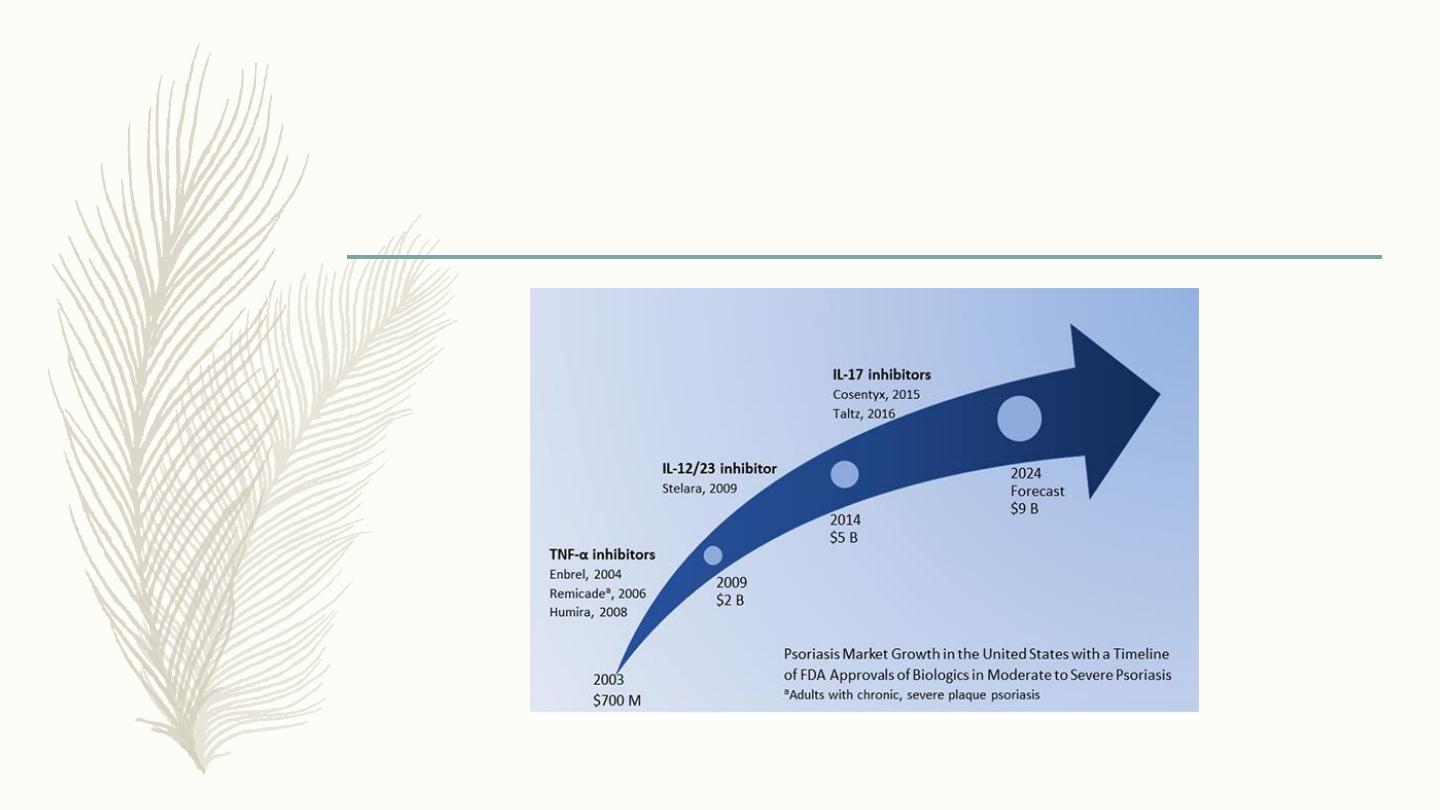
Biologics
– Biologics: new, monoclonal antibodies to key pathological pathways in
psoriasis
– Against T.N.F. α(alpha)
– Against receptors involved in T-cell trafficking as interleukin 12/23(IL-12/IL-
23) blockade agents
– Interleukin 17-A
– Expensive, requires careful consideration of medical Hx, disease severity &
monitoring of infections