Gram Positive Bacilli Listeria monocytogenes
Listeria monocytogenesListeria monocytogenes is a food-borne zoonotic pathogen that can cause serious human infections, particularly in neonates, pregnant women and elderly people or immunocompromised.
It’s widespread in the environment and has been recovered from soil; water; vegetation; and animal products, such as raw milk, cheese, poultry, and processed meats.
Listeria monocytogenes
Pathogenicity:Small gram-positive rods, non spore forming,
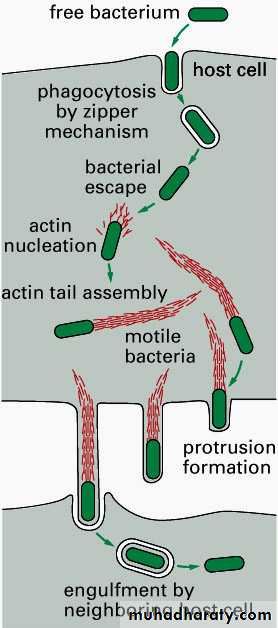
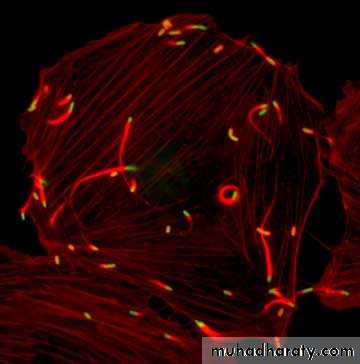
Beta hemolytic on blood agar,Tumbling motility in broth; actin jet motility in cells, (End over end).
The motility test rapidly differentiates Listeria from diphtheroid normal skin flora
Motile at 22-28 ºC & not motile at 37 ºc.
Gram stain in the blood
Gram stain from a culture
Gram stain in the blood
Gram stain from a cultureβ-Hemolysis: Listeria on sheep blood agar (SBA)
Blood Cultures
Listeria monocytogenes
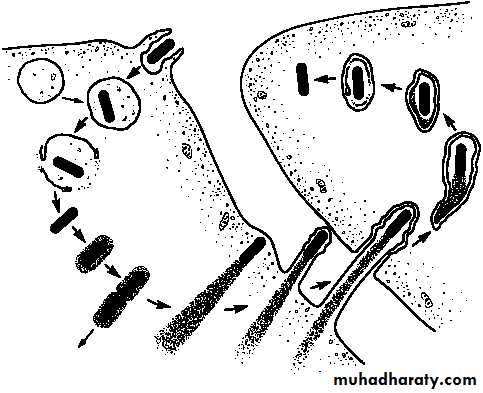
Pathogenicity:Facultative intracellular, survival inside the host cells is due to inhibition and lysis of phagosome by forming pores (mediated by Listeriolysin O).
It can be growing and surviving over a wide range of environmental condition
It can survive at refrigerator temperature 4 ºC (Cold growth) and under condition of low pH and high salt.
Listeria monocytogenes
Pathogenicity:It can grow in refrigerated food and can tolerate preserving agents,
Mode of transmission: Contaminated food (raw milk, MC) followed by vertical transmission (mother to fetus),
Direct cell-to-cell spread is due to host cell actin polymerization (mediated by listeriopods).
Listeria monocytogenes
Pathogenicity:Enter to the body by ingestion of the contaminated food such as cheese, fruit or vegetable,
adhesion proteins (Ami, Fbe A and Flagella proteins) that help the bacteria for contact on epithelial cell suffers.
After phagocytosis, the bacteria enclosed in a phagolysosome when the low pH activates the bacterium to produce Listeriolysin O two phospholipases
Listeria monocytogenes
Pathogenicity:Lead to lyses the membrane phagolysosome and allows the bacteria to escape in to the cytoplasm of epithelial cell.
The organisms proliferate, and Act A, another Listerial surface protein, induces host cell actin polymerization, which propels them to the cell membrane.
Pushing against the host cell membrane, they cause formation of elongated protrusions called filopods.
These filopods are ingested by adjacent epithelial cells, macrophages, and hepatocytes, the listeriae are released.
Listeria monocytogenes
Pathogenicity:
The listeria are released and the cycle begins again.
Listeria can move from cell to cell without being exposed to antibodies.
It escapes from the phagocytic vacuole by elaborating a membrane damaging toxin called Listeriolysin O.
The organisms induce a reorganization of cellular actin such that short filaments and actin-binding proteins adhere to the bacteria, creating a comet like “tail.”
Listeria monocytogenes
Pathogenicity:Bacterium-produced membrane-degrading phospholipases then mediate the passage of the organism directly to a neighboring cell, allowing avoidance of the extracellular milieu, including cells of the immune system.
Iron an important virulence factor, listeria produce siderophores and are able to obtain iron from transferrin.
Listeria monocytogenes
The macrophage of a neonate oran immunosuppressed patient
The macrophage of an
immune competent person.
Listeria monocytogenes
Clinical Symptoms:• Listeriosis (human, peaks in summer):
• Healthy adults and children: generally asymptomatic or diarrhea with low % carriage
• Pregnant women: symptomatic carriage, septicemia characterized by fever and chills; can cross the placenta in septicemia.
• Neonatal disease:
• Early-onset: (granulomatosis infantiseptica) in utero transmission; sepsis with high mortality; disseminated granulomas with central necrosis.
Listeria monocytogenes
Clinical Symptoms:• Neonatal disease:
• Late-onset: 2–3 weeks after birth from fecal exposure; meningitis with septicemia.
• In immunocompromised patients.
• Septicemia and meningitis (most common clinical presentation).
• Listeria meningitis most common cause of meningitis in renal transplant patients and adults with cancer.
Listeria monocytogenes
Clinical Symptoms:• Neonatal disease:
• Late-onset: 2–3 weeks after birth from fecal exposure; meningitis with septicemia.
• In immunocompromised patients.
• Septicemia and meningitis (most common clinical presentation).
• Listeria meningitis most common cause of meningitis in renal transplant patients and adults with cancer.
Listeria monocytogenes
Laboratory Diagnosis:Blood or CSF culture at 4˚C; CSF for Gram stain, catalase positive.
Shows tumbling type of motility
Motile at 25°C but nonmotile at 37°C (Differential motility)
Growth improves if cultured in thioglycollate broth at 4°C (cold enrichment)
Media: Blood agar, chocolate agar, PALCAM agar (selective medium)
Anton test: Instillation to rabbit eye causes conjunctivitis.
Listeria monocytogenes
Treatment:
DOC: Ampicillin (also penicillin),
Alternative: Cotrimoxazole (if allergic to penicillin),
Cephalosporin not effective,
EM & fluorescent micrograph of
L. monocytogenes(with actin “comet” tail)
1. Internalin induces uptake
2. LLO to escape3. ActA for actin-based motility
4. Protrusion
5. LLO + two
PLCs for release