Endocrine System
pituitary gland
Lect-1
Pituitary or Master Gland
posterior lobe
Neurohypophysis
Modified glial
cells.
anterior lobe (80%)
adenohypophysis
Anterior Lobe
Acidophil:
1- Somatotrophs:growth hormone
GH somatotropin
2- Mammotroph: lactogenic hormone
Prolactin
Basophils:
1- Thyrotrophs: thyroid-stimulating hormone
TSH.
2- Corticotrophs: adrenocorticotropic hormone
ACTH
3- Gonadotrophs: follicle-stimulating hormone
FSH
and luteinizing hormone
LH
Chromophobe: 15-20% of cells, non secretory.
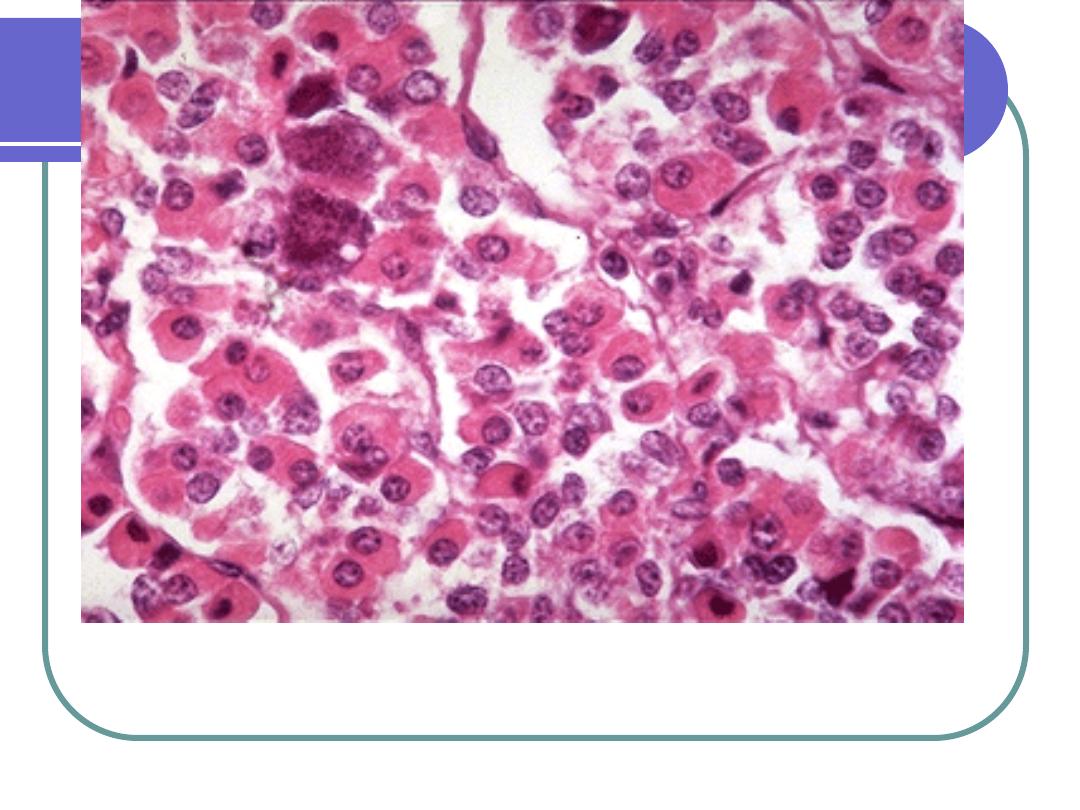
Normal anterior pituitary gland (pars distalis) - High power Note the
mixture of cell types, including the red-staining acidophils, purple-
staining basophils, and the chromophobes, whose cytoplasm stains only
weakly. The
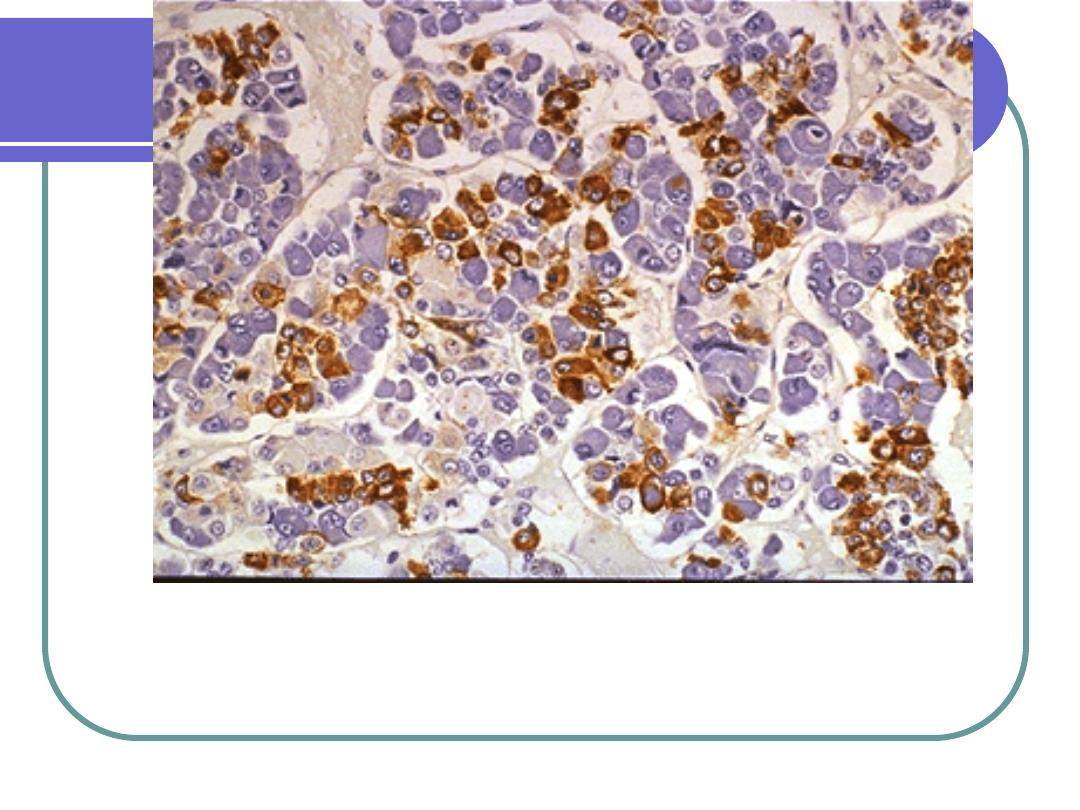
Normal anterior pituitary gland, immunohistochemical stain for growth
hormone (hGH) - Medium power somatotrophic (hGH-secreting) cells
have been labeled with an antibody to hGH. The antibody, in turn, has
been linked to a chromogen that stains the somatotrophic cells brown.
Hormones regulated by:
1.
hypothalamus
2.
releasing/inhibiting factors
3.
feedback effects of hormones
released by target glands
Anterior Pituitary:
In response to certain stimuli the pre
formed hormones are released directly
into the systemic circulation through the
venous channels of the pituitary.
Posterior Pituitary
:
Posterior Lobe
Secrets two peptide hormons
antidiuretic hormone
ADH
decrease ADH causes increase urine
output
increase ADH causes decrease urine
output
oxytocin
stimulates contraction of pregnant uterus,
labor, and childbirth
stimulates milk secretion
Posterior Pituitary
1.
ADH, or vasopressin
2.
Oxytocin
Acts as storage & releasing site for
hormones made by hypothalamus
Clinical manifestations of
pituitary diseases:
1- hyperpituitarism.
2- Hypopituitarism.
3- local mass effects.
Hormonal Alterations
What causes endocrine pathology?
1.
Feedback systems fail
2.
Gland releases too much or too little
3.
Hormones degraded/inactivated
4.
Receptor-associated disorders
5.
Intracellular disorders
Without this system:
No reproduction.
No metabolic activity.
We wouldn’t grow!!
Thyroid diseases occur
Causes:
Inflammatory Lesions
Trauma
Stem tumor
Surgical transection
Interruptions in system
Pituitary Diseases
Posterior:
1.
SIADH
2.
Diabetes Insipidus
Anterior:
1.
Hypopituitarism
2.
Hyperpituitarism
Syndrome of Inappropriate
Antidiuretic Hormone (SIADH)
Persistent release of ADH unrelated to plasma osmolarity.
Etiology:
Small cell lung ca (part of paraneoplastic syndrome)
Thymoma, carcinoma of pancreas and lymphoma
pituitary surgery, CVA and CNS infections
Infectious pulmonary disease, pneumonia and
brucellosis
Drugs
SIADH
Pathophysiology:
1.
Abnormally ↑ levels ADH secreted
(without normal physiologic stimuli causing
hormone release)
2.
Continuously ↑ reabsorption of
H
2
O
1.
“water intoxication” symptoms
3.
Water retention
4.
Extracellular fluid volume ↑, result in
hyponatremia and hemodilution.
SIADH
Clinical Manifestations:
2.
Symptoms:
depends on degree of hyponatremia.
anorexia, fatigue, altered mental status.
vomiting, abdominal cramps.
Muscle twitching, convulsions
3.
Signs:
serum hypo-osmolality; hyponatremia
↑ urine osmolality
Diabetes Insipidus
(ADH deficiency )
Inability to concentrate urine result in
polyuria, polydepsia and hypernatremia.
3 Forms:
1.
Neurogenic/central
2.
Nephrogenic form
3.
Psychogenic form
Diabetes Insipidus
Pathophysiology:
1.
Insufficient ADH production
2.
Large volumes dilute urine excreted
3.
↑ plasma osmolality
4.
Polydipsia
Diabetes Insipidus
Clinical Manifestations:
(neurogenic DI)
Caused by surgery or radiation, severe
head injury and idiopathic.
1.
Diuresis, significant
2.
Polyuria, polydipsia
Anterior Pituitary Disorders
Hypopituitarism:
Hypo function of the anterior pituitary
gland that result from hypothalamic
lesion or primary pituitary disturbance.
Accompanied by evidence of posterior
pituitary dysfunction in a form of
diabetes insipidus.
ETIOLOGY:
1.
Tumors and other mass lesions include pituitary
adenomas.
2.
Traumatic brain injury and subarachnoid hemorrhage.
3.
Pituitary surgery or radiation.
4.
Pituitary apoplexy.
5.
Ischemic necrosis of pituitary and Sheehan’s syndrome.
6.
Rathke’s cleft cyst.
7.
Empty sella syndrome.
8.
Genetic defects.
9.
Hypothalamic lesions, as tumors, as
craniopharyngeoma, gliomas and germinoma.
10.
Inflammatory disorders and infections.
clinically
1.
Absent selective pituitary hormones
2.
Complete hormonal failure
Sheehan’s syndrome
Pathophysiology:
Sudden infarction of the anterior lobe precipitated
by obstetric hemorrhages or shock: during preg:
1.
Physiologic expansion of the gland is not
accompanied by increase in blood supply.
2.
Vascular gland (↑ size, ↑ risk injury with anoxia).
3.
Further reduction by obstetric hemorrhage cause
Vasospasm
of artery supplying gland
4.
Sustained vasospasm = ischemic tissue necrosis
5.
Edema
6.
Expands into sella tunica
7.
Pituitary has excessive fibrin in vessels
Hypopituitarism
Clinical Manifestations:
Depend on hormone affected
Panhypopituitarism
GH deficiency in adult non apparent but in children
result in dwarfism and retarded sexual
development.
ACTH deficiency: life threatening\ Cortisol
deficiency.
Hypogonadism: amenorrhea, atrophy of gonads,
loss of pubic and axillary hair, sterility, and
recession of hair lines.
TSH deficiency result in hypothyroidism.
Testicular atrophy
Non secretary adenoma
About 20-25% of the diagnosed pituitary
tumors are non functioning clinically and
come to clinical attention due to LOCAL
effects including abnormalities in the visual
fields, headaches, or hypofunction of one of
the target endocrine organs under pituitary
control as hypothyroidism or hypogonadism.
Generally these are large tumors and
looks histologically as null cell
adenomas or oncocytomas.
EMPTY SELLA SYNDROME
Uncommon condition caused most often by
herniation of the arachnoid through a defect
in the diaphragma sellae due to large
aperture or other defect result in pressure
atrophy as a result of CSF pressure creating
an appearance of empty sella.
Also can be caused by Sheehan's
syndrome or surgical radiation ablation.
Most cases are subclinical and rarely
present as hypopituitarism.
Hypothalamic suprasellar tumors
Extremely uncommon but may induce hypofunction or
hyperfunction of the anterior pituitary.
Most are gliomas and craniopharyngiomas.
CP are vestigial remnants of the Rathke’s pouch and
mostly affect children and young adults and usually
benign. But it encroaches on optic chiasm or nerves or
rarely on 3rd ventricle or base of brain.
3-4 cm, encapsulated, solid or cystic, with calcification in
¾ of patients.
Histologically simulate the enamel organ of the tooth, thus
called as adamantinomas or ameloblastomas looks as
cords of stratified squamous epithelium embedded in
loose fibrous stroma.
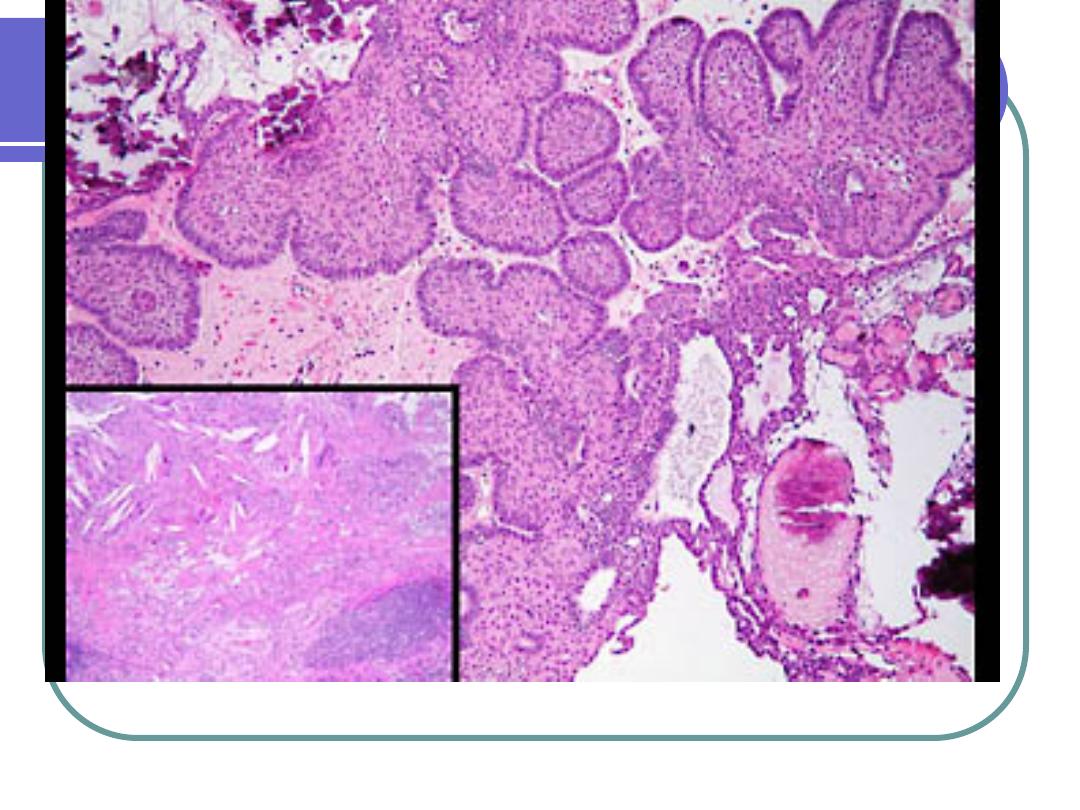
Craniopharyngeoma - Low power keratinizing squamous cells,
calcifications, cholesterol crystals, fibrosis, chronic inflammation,
gliosis, and a peripheral layer of columnar cells.
Pituitary adenomas and
Hyperpituitarism
Caused by adenomas until proved otherwise,
rarely by carcinoma or hypothalamic lesion.
Pituitary Adenomas
Classified according to hormon produced by
neoplastic cells.
35-60 years peak.
Microadenomas if less than 1 cm, in diameter and
macroadenoma if more than 1 cm.
Some produce more than one hormone.
Some are nonfunctioning destroy the pituitary and
cause hypopituitarism.
Also may present due to local effects as:
Involves impingement of optic chiasma,
occulomotor, trigeminal nerves )visual field
defects).
Hypothalamic involvement: disturbs wakefulness
center, thirst, temp, appetite (with enlargement of
sella turcica seen by x-ray CT scan or MRI.
Rarely cause increased intracranial pressure.
Morphology of Pituitary Adenomas
Variable pattern of growth
May be small, hormonally inactive, incidental
findings
May be small but cause hormone excess and
these are called as MICROADENOMAS less than
10 mm.
May be rapidly growing mass lesions as
MACROADENOMAS more than 10 mm.
Generally are poorly encapsulated.
Microscopically are formed of fairly uniform sheets
of cells.
If hemorrhage it is called as pituitary apoplexy.
The Spectrum: Pituitary Tumors
Microadenoma:
Incidental finding or the
cause of serious disease
Macroadenoma
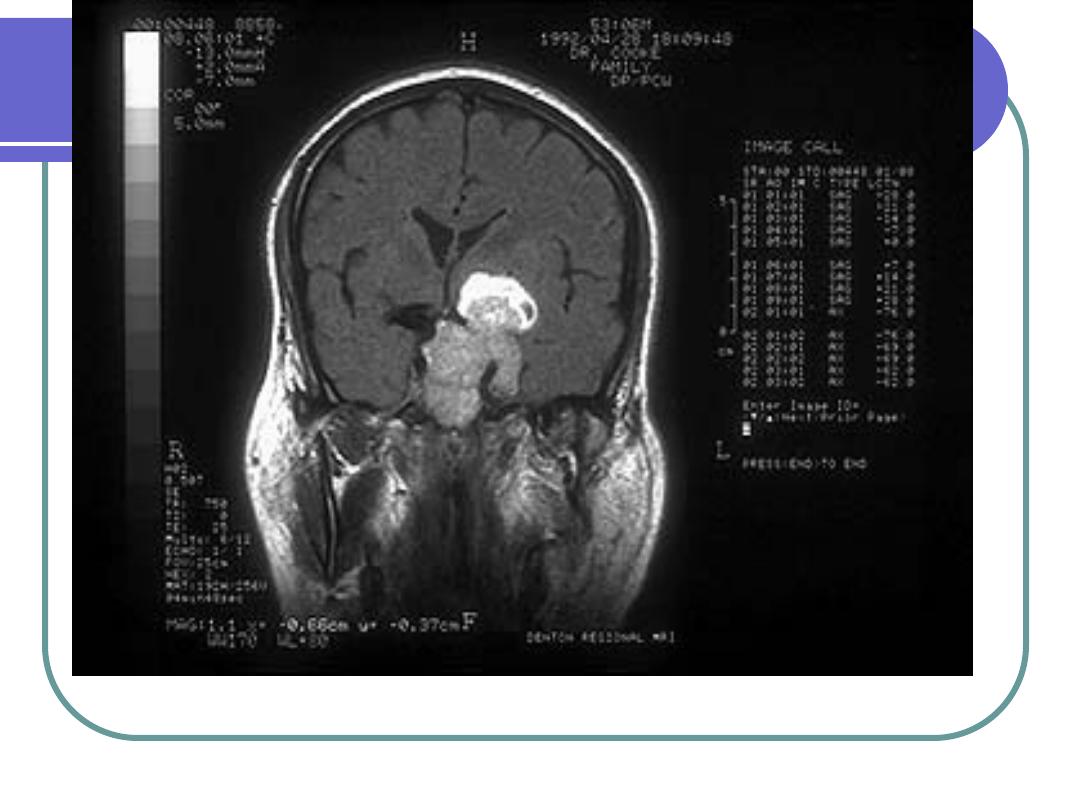
This MRI demonstrates a large lesion involving the sellar and suprasellar
regions. The patient has been injected with contrast material, which
causes this particular mass to enhance as a bright (white) lesion
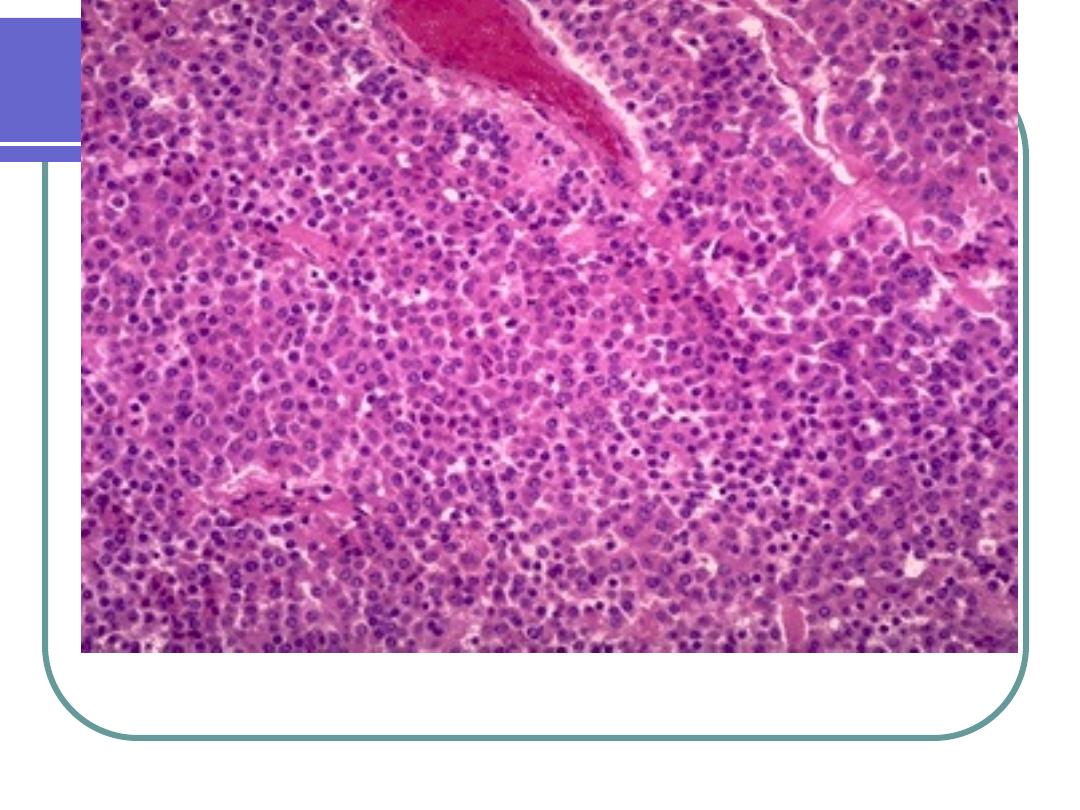
Note the monomorphic cellular proliferation. The cells are growing in a
diffuse pattern and lack the characteristic nesting architecture of the
normal anterior pituitary gland
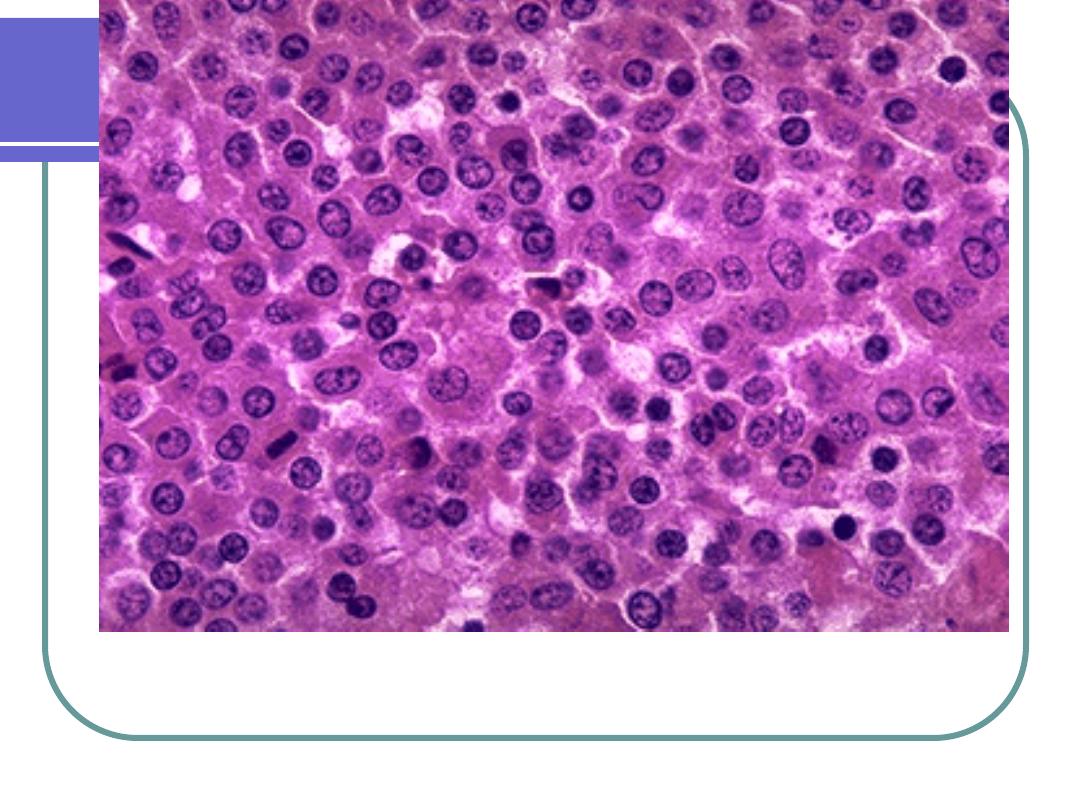
At higher magnification, the comparatively uniform, amphophilic
(amphophilic means that the color is somewhere in no-man's-land
between eosinophilic and basophilic) staining pattern of the neoplastic
cells is apparent
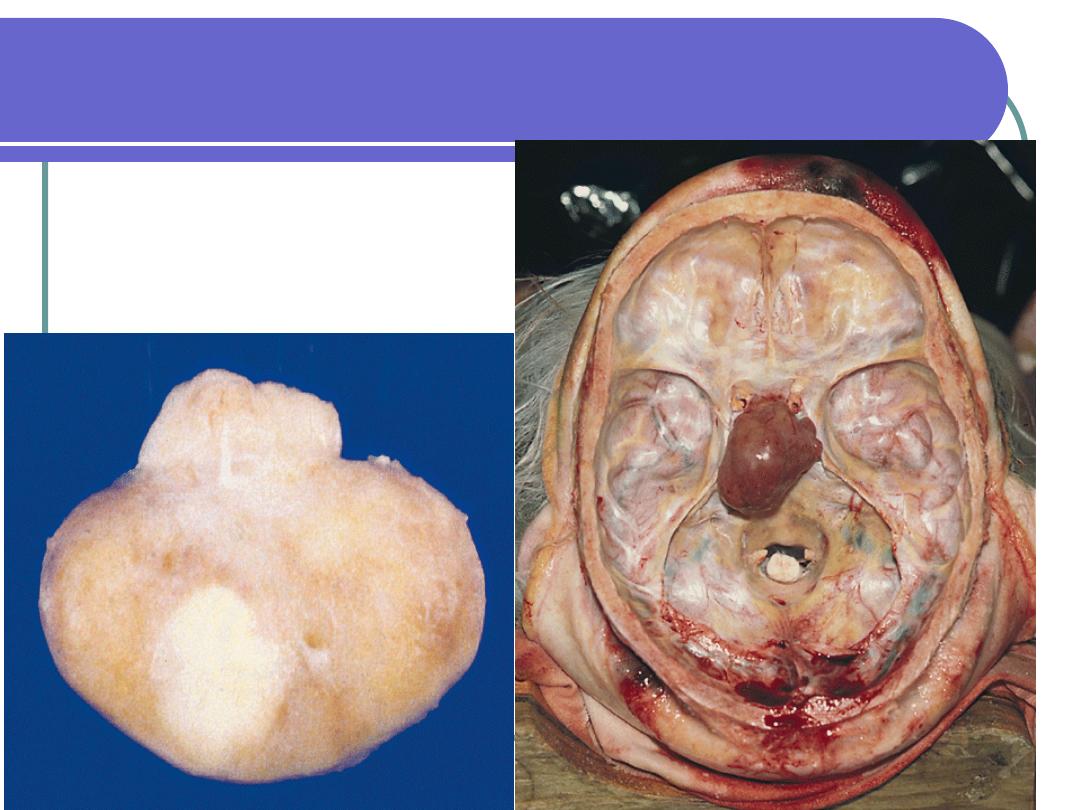
This specimen shows a pituitary adenoma discovered incidentally in a patient who
died of unrelated causes. Pay special attention to the relationship between the
adenoma and adjacent structures in order to better understand some of the presenting
clinical manifestations of mass lesions in the pituitary region
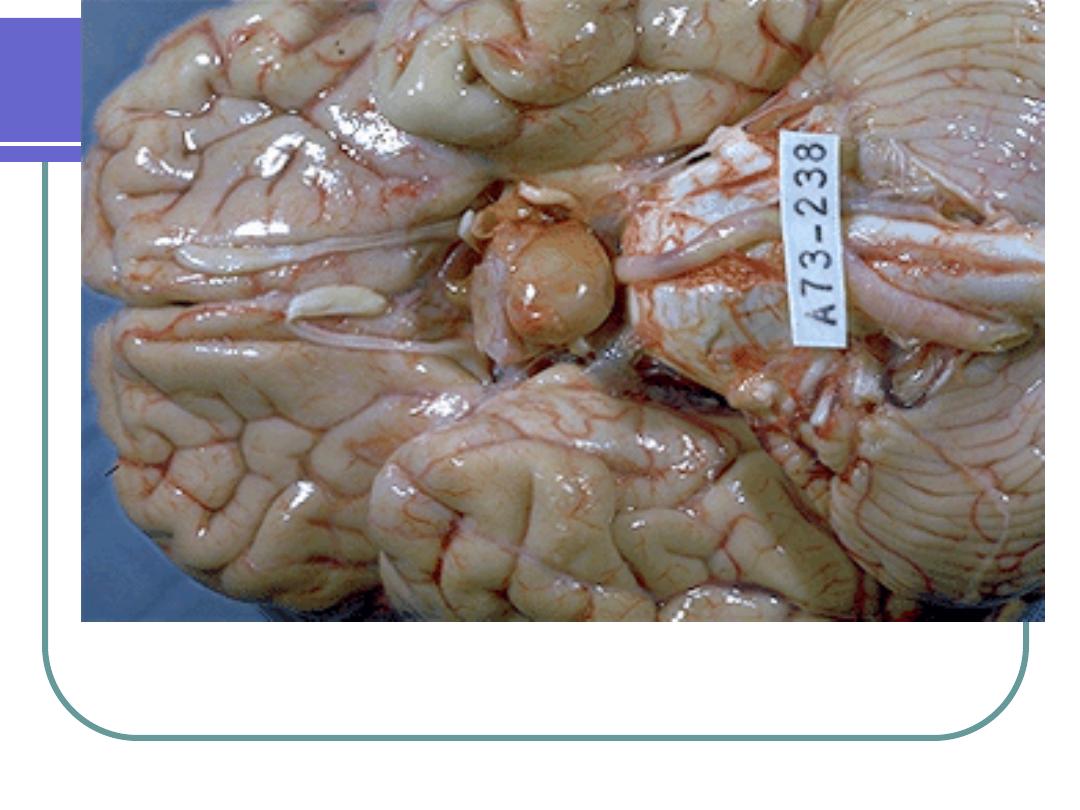
Brain showing pressure effect of pituitary adenoma - Gross, ventral
surface. The pituitary adenoma has been removed to demonstrate local
changes due to the mass effect of the tumor. Note the depressed area just
anterior to the mammillary bodies,
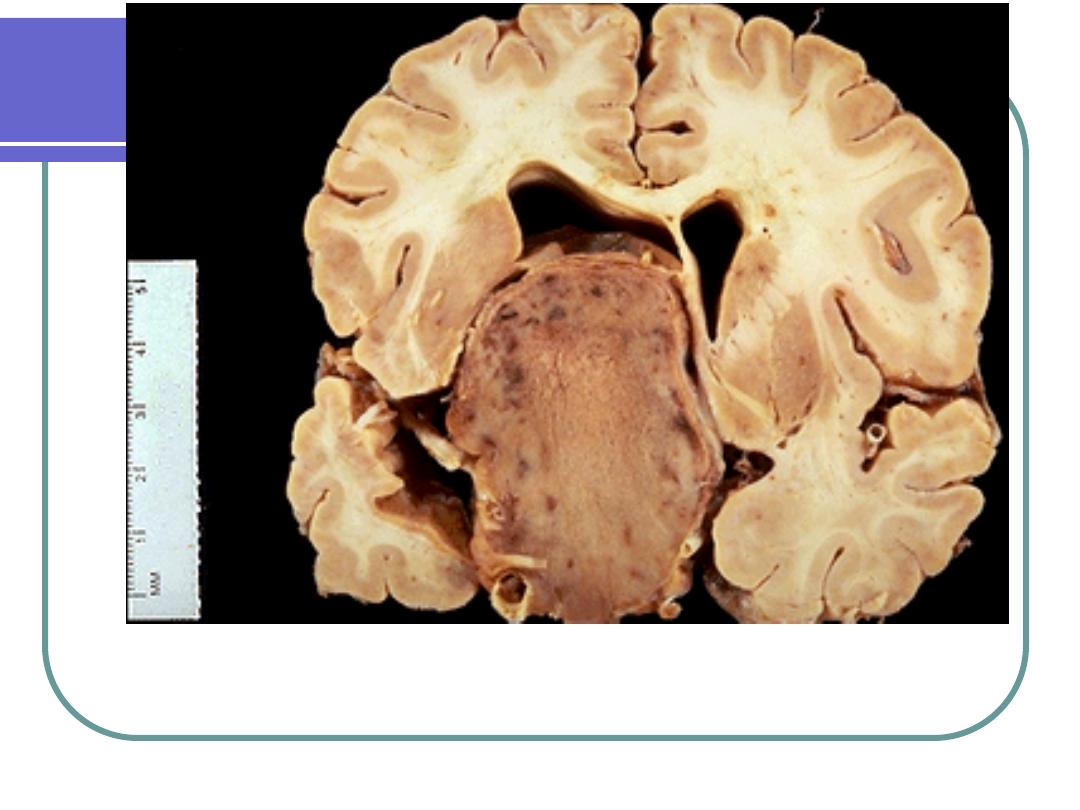
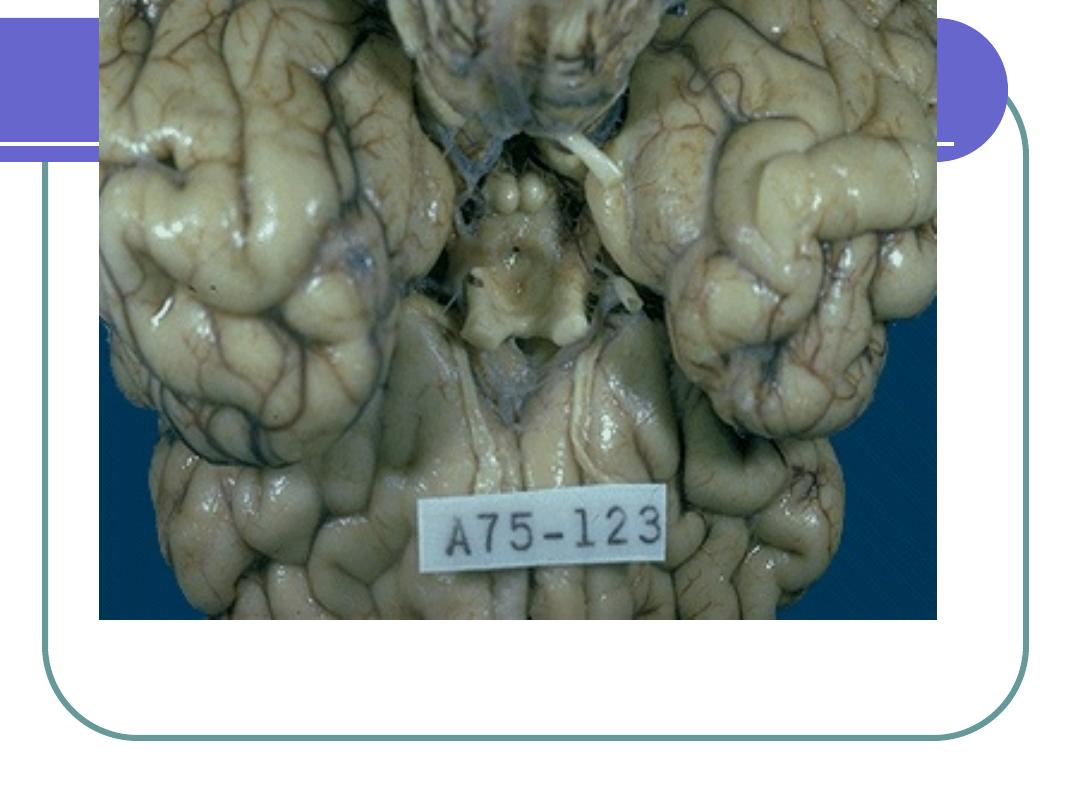
Brain and pituitary adenoma - Gross, coronal section This specimen shows an
advanced pituitary adenoma. The adenoma has grown far beyond the
confines of the sella turcica, has markedly distorted the left lateral ventricle,
and encases the internal carotid artery
Genetic abnormalities with PA
1.
G protiens = signal transduction from
receptor to intracellular adenyl cyclase,
that generate second messengers
cAMP. Mutations in G protein result in
cell proliferation.
2.
Four genes in familial PA as MEN1.
3.
P53.
Acromegaly and somatotropic
adenomas
Uncommon
Exposure to high levels of GH
Etiology:
GH-secreting pituitary adenoma
Acidophilic macroadenoma
Adults 40-50’s
In children cause gigantism
Progressive
Acromegaly
1.
Adenoma secretes GH
2.
Adults: epiphyseal plates are closed
3.
↑ connective tissue proliferation; bony
proliferation
4.
GH→↑ phosphate reabsorption in renal
tubules (mild hyperphosphatemia)
5.
Impaired CHO metabolism, ↑ metabolic
rate
6.
Hyperglycemia leads to insulin
resistance (eventually DM)
Acromegaly
Clinical Manifestations:
Enlarged tongue
enlarged/overactive sebaceous & sweat
glands
coarse skin, body hair
Bone changes (see pictures)
arthralgia, arthritis, backache
Diabetes mellitus
Prolactinoma
Prolactinomas: pituitary tumor, secretes
prolactin.
Most common type of pituitary tumors.
2/3 are macroadenomas of acidophilic cells
Prolactin controlled by hypothalamus via
dopamine secretion.
Hyperprolactinemia
30% pituitary tumors secrete prolactin
Prolactin
Prolactin can be ↑ also by:
Hypothalamic lesions
renal failure
primary hypothyroidism
breast stimulation
venipucture
Drugs (dopamine blocking effect as methyldopa
and reserpine), estrogens, tricyclic antidepressants
Presents with hypogonadism, in both males and
females and galactorrhea in females and
amenorrhea (1/4 of cases of amenorrhea due to
hyperploactinemia).
Corticotroph tumors
Small basophilic microadenoma.
Increased ACTH causes adrenal
hypersecretion of cortisol and production of
Cushing’s disease.
Other functioning adenomas
Gonadotrophs 6% with increased levels
of FSH or LH and hypogonadism.
Thyrotroph adenoma is uncommon.
Carcinoma
is rare and most are non functioning and
associated with lymph node, bone and
liver metastasis
