
Lecture 15 pathology PANCREAS 3
rd
Stage
1
Exocrine Pancreas
• About 85-90% of the pancreas is the exocrine pancreas that secretes
enzymes important for the process of food digestion, 10-15% is the
endocrine pancreas consist of islets of Langerhan's which secrete insulin,
glucagon.
DISEASES OF EXOCRINE PANCREAS:
Acute pancreatitis
Inflammation of the pancreas associated with acinar cell injury, it is
characterized by acute onset of abdominal pain resulting from enzymatic
necrosis & inflammation of the pancreas . Typically pancreatic enzymes are
elevated in serum & urine. The release of pancreatic lipases causes fat necrosis
in and around the pancreas & with damage to the blood vessels causes acute
hemorrhagic pancreatitis.
Morphology
4 main changes are associated with A.P:
Proteolytic destruction of pancreatic substance .
Necrosis of blood vessels with subsequent hemorrhage .
Necrosis of fat by lipases .
Acute inflammatory reactions .

Lecture 15 pathology PANCREAS 3
rd
Stage
2
Acute pancreatitis
The most characteristic microscopic feature is the presence of fat necrosis
which may spread throughout the abdominal cavity. These deposits may be
evident as calcification on abdominal X-ray.
Pancreatic pseudocyst is a common complication of acute pancreatitis which
does not contain epithelial lining.

Lecture 15 pathology PANCREAS 3
rd
Stage
3
Pathogenesis
4 major etiologic factors are involved in A.P
Metabolic
Alcohol
Hypercalcemia
Drugs (e.g. thiazide diuretics)
Mechanical
Gall stones
Trauma
Surgery
Vascular
Shock
Atherosclerosis & embolism
Infectious
Mumps
The tissue lesions of acute pancreatitis suggest autodigestion of pancreas
by activated pancreatic enzymes released from the cells with resultant
proteolysis, lipolysis & weakening of blood vessels .
Activated trypsin convert other proenzymes to activate enzymes,
prekallikrein to kallikrein activated kinin system & clotting system, leading to
local inflammation , thrombosis & systemic clotting disturbances.
Mechanism for activation of pancreatic enzymes:
1. Cholelithiasis with impaction in ampulla of Vater result in obstruction &
increased ductal pressure.
2. Alcohol :chronic alcohol ingestion causes secretion of protein - rich
pancreatic fluid which predispose to formation of calcified protein plugs.
3. Acinar cell injury: direct injury from alcohol, viruses, drugs, trauma &
ischemia
Clinical features
A.P is a medical emergency acute abdomen, intense abdominal pain with
upper back radiation, peripheral vascular collapse & shock.

Lecture 15 pathology PANCREAS 3
rd
Stage
4
Chronic pancreatitis
Termed chronic relapsing pancreatitis . Is characterized by repeated
attacks of mild to moderate pancreatic inflammation with continuous loss of
pancreatic panenchyma & replacement by fibrous tissue.
Most commonly affecting middle-aged men especially alcoholics. Biliary
tract diseases play less important role in chronic pancreatitis than acute form,
but hypercalcemia predispose to chronic pancreatitis. Many patients have no
apparent predisposing factors.
Pathogenesis
Hypersecreation of protein from acinar cells with no excess fluid secretion
causing precipitation of proteins with admixed with cellular debris to form
ductal plugs, those plugs may enlarge in alcoholics to form "stones" containing
ca- carbonate, end in calcification & ductal obstruction & atrophy of the
draining pancreatic lobules.
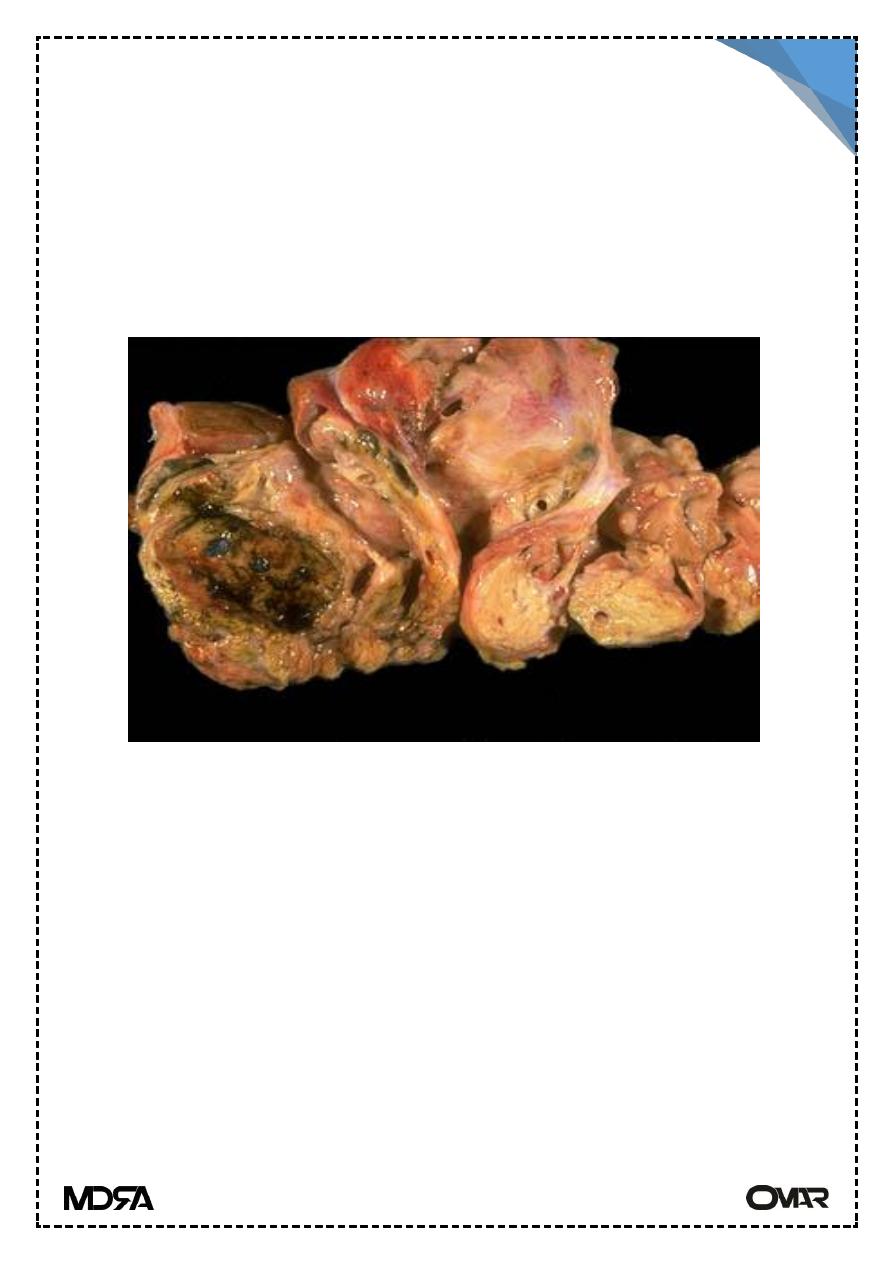
Morphology
Irregularly distributed fibrosis, reduced number & size of acini with
sparing of islets of Langerhan's with obstruction of pancreatic ducts, foci of
calcification, stones may be present (chronic calcifying pancreatitis) in
alcoholics.
Chronic obstructive pancreatitis with impacted stones around ducts.
Pseudocytes formation is common clinically: silent, or recurrent attack of
abdominal pain.
Late complications: diarrhea (malabsorption), steatorrhea, diabetes.
Pseudocytes:
Localized collection of fluid representing pancreatic secretion, almost
always arising from bouts of acute or chronic pancreatitis not contain epithelial
lining but fibrous inflammatory wall, usually unilocular.
Lecture 15 pathology PANCREAS 3
rd
Stage
5
TUMORS
Benign tumors :
Benign tumors of the pancreas are rare
Cytadenomata are the main benign tumor of exocrine pancreas, they are
painless, slowly growing tumor, multilocular, mucin-secreting (benign
mucinous cytadenoma) or serous –secreting (benign serous cyst adenoma).
Pancr pseudocyst
Malignant tumors
Carcinoma of the exocrine pancreas, almost always arising from ductal
epithelial cells.
Epidemiology
5% of all cancer death in U.S with an increasing incidence (due to smoking,
diet, chemical carcinogens) occur in 6th -8th decade, smoker> nonsmoker,
diabetics> non-diabetics.
Morphology
• Gross distribution head 60%, body 15%, tail 5% diffuse 20%. Maybe small or
ill defined or large up to 10 cm with extensive local invasion & metastasis.

Lecture 15 pathology PANCREAS 3
rd
Stage
6
Carcinoma of the head of the pancreas, the ampullary region is invaded &
obstructing the bile outflow.Carcinoma of the body & tail not obstructs the
biliary tract & remains silent
Microscopically
Adenocarcinomas arising from ductal epithilum, mucus secreting, many
have abundant fibrous stroma. Most are moderately differentiated.
Clinically :
Pain in the epigastrium is usually the first symptoms.
Obstructive Jaurdice (carcinoma head of the pancreas)
Migratory thrombophlebitis.
Biochemical tests: CEA (carcinoembryonic antigen) & CA19-9 antigen are
elevated in the serum but are not specific for carcinoma of pancreas.
Pancreatic carcinoma

Lecture 15 pathology PANCREAS 3
rd
Stage
7
Spread & metastasis :
Local causing obstructive Jaundice or invasion of duodenum,
Lymphatic, to adjacent lymph nodes
Hematogenous, to the liver
Prognosis
Prognosis of carcinoma of pancreas is extremely poor, only 10% of
patients survive the first year after diagnosis.
Palliative surgery are performed to bypass the obstruction of the bile
duct, relieving Jaundice & for obstruction of duodenum.
Islet cell tumor
• A-Insulinoma (hyperinsulinism):β-cell tumors are the most common of islet
cell tumors, they are benign.
• Clinical triad :
Attacks of hypoglycemia (blood glucose less than 50mg/dl)
CNS manifestations (confusion ,stupor ,loss of consciousness).
Attacks are precipitated by fasting or exercise &relieved by feeding or i.v.
glucose .
B-Gastrinoma (Zollinger-Ellison syndrome)
Hypersecretion of gastric acid with severe peptic ulceration in 90-95% of
patients, duodenal, gastric & jejunal.
