AntePartumHaemorrhage
(APH)
It is genital tract bleeding after 24 weeks of pregnancy and before
delivery of baby. (Bleeding in the 3
rd
TM )
Incidence ;3% of all pregnancies.
Causes:
A. Placental causes
Placenta praevia (1%)
Abru ptio placentae (placental abruption) 1%
Vasa praevia
B. Local cause in the vagina and cervix
Cervicitis
Cervical carcinoma
Vaginal trauma
Vaginal infection
Cervical ectropion
C. Other causes is PTL and ruptured uterus
How to reach a dx:
History:how much bleeding, triggering factors, associated pain or
contraction,fetal movement, last cervical smere.
Examination :pulse, BP,is the uterus soft or tender , fetal heart
auscultation ,CTG, speculum vaginal exam after exclusion of pp.
Investigation:full blood count, coagulation screen, cross 6 units of
blood,U\S.
Placenta praevia
Placenta praevia: A placenta that has implanted into the lower
segment of the uterus.

( The lower segment can be defined as that part of the uterine wall
used to be the isthmus before pregnancy, and within 8 cm of the
internal cervical os at term )
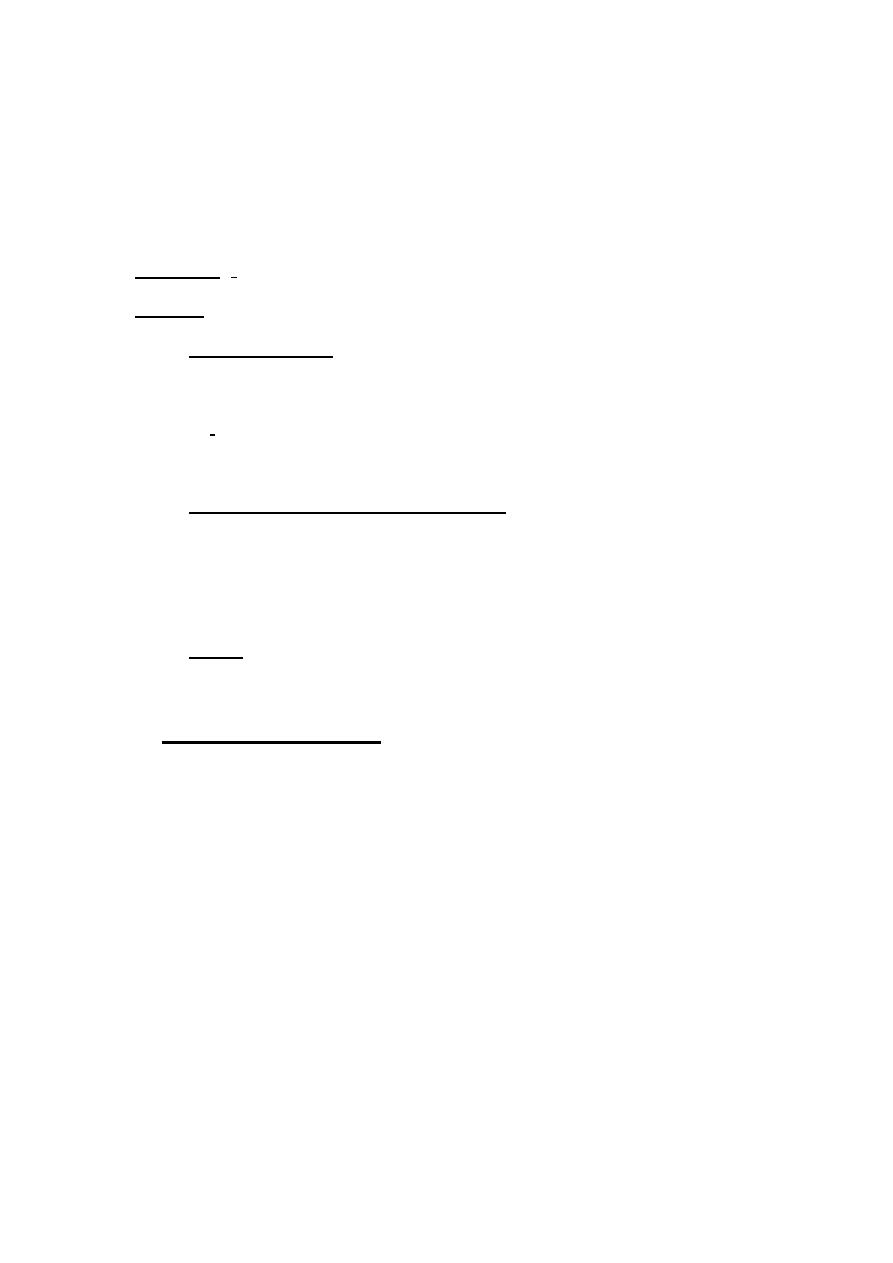
It can be classified as either
major
in which the placenta covering
the internal cervical os or
minor
when the placenta is sited within
the lower segment of uterus, but does not cover the internal os,
replacing the old classification.
The main
risk factors
are increasing age and parity ,previous uterine
surgery), prior P.P (4-8% recurrence rate) ,assisted conception and
structural uterine anomalies.
In women with previous C/S the placenta may implant and thus
invades into the previous scar and called morbidly adherent placenta
and there are 3 types:
1-
placenta accreta
: placenta adherent to the uterine wall.
2-
placenta increta
:placenta invading the uterine wall.
3-
placenta percreta
: placenta invading through the uterine wall.
Old classification of pp
Diagnoses:
clinical presentation:
1- Recurrent episodes of painless bright red vaginal bleeding. Mean GA
at presentation is 30 wks
2- Asymptomatic (10% of cases of P.P are diagnosed incidentally by U/S)
3-A persistent malpresentation or high head in late pregnancy after 37
weeks.
4-pp may present as placental abruption.
The uterus is soft and non tender,
the digital exam is contra
indicated.
Diagnosis is almost exclusively done by U/S whether abdominal or
vaginal U/S
An ultrasound scan will show the position of the placenta clearly within
the uterus. If the placenta lies in the anterior part of the uterus and reaches
into the area covered by the bladder, it is known as a low-lying placenta
(before 24 weeks) and placenta praevia after 24 weeks.

Management
:
1- Admit to hospital, ABC.
2- Insert a broad-bore i.v. cannula and start an infusion of normal saline if
shocked patient and arrange for emergency C/S
3- Take blood for cross-matching and haemoglobin estimation.
4- Avoid all digital vaginal examinations.
5- Perform ultrasound as soon as possible to identify the cause of
bleeding.
6- Cross-matched blood should be kept permanently available.
7-pationt should be admitted for observation and not allowed home until
at least 24 hrs has passed without further bleeding .those pts with major
pp who had recurrent bleeding should be admitted as in patients from 34
weeks. If the woman is anaemic and no longer bleeding and the baby is
<37 weeks then she should be transfused aiming for a haemoglobin of
>10.5g/dl. This can be repeated as necessary until the baby reaches
maturity when delivery should be by Caesarean Section. Don’t forget
steroid and anti –D.
8- At 36–37 weeks’ presentation, a final ultrasound should be performed
and acted upon:
(a) major placenta praevia should have a Caesarean section between 37
and 38 weeks’ gestation by an experienced obstetrician
(b) Regarding the low lying placenta (placental margin within 2 cm from
internal os) it is safe to wait until labour vaginal delivery is not
contraindicated unless there is vaginal bleeding ( C/S).
AS ARULE, the GOAL is to obtain fetal maturation without
compromising the mother health, delivery indicated If GA is
reaching 37-38 weeks ,massive bleeding > 1500 ml and continuing
significant bleeding .
If bleeding is severe the delivery by emergency C/S regardless of
GA ( don’t forget preparation of 4-6 units of blood)
If the bleeding is not profuse ( or small repetitive attacks) the
expectant management is the rule until 36-37 weeks (anemia should
be corrected if present) then deliver by elective C/S after checking the
fetal lung maturity.
COMPLICATIONS AND PROGNOSIS:
MATERNAL
1-The major cause of death in women with placenta praevia now is
postpartum haemorrhage (PPH). PPH is common because the lower
segment does not contract and retract as in the upper segment. This
may lead to an emergency hysterectomy if the bleeding cannot be
stopped
2-Antepartum and intrapartum bleeding is constant threat to the
woman
3-DIC
4-Another risk is the placenta accreta, increta or percreta ( adherent
placenta) which require cesarean hysterectomy.
FETAL
Bleeding from placenta praevia is maternal in origin.
The risks to the fetus are prematurity, malpresentation and abnormal
lie
Placental abruption
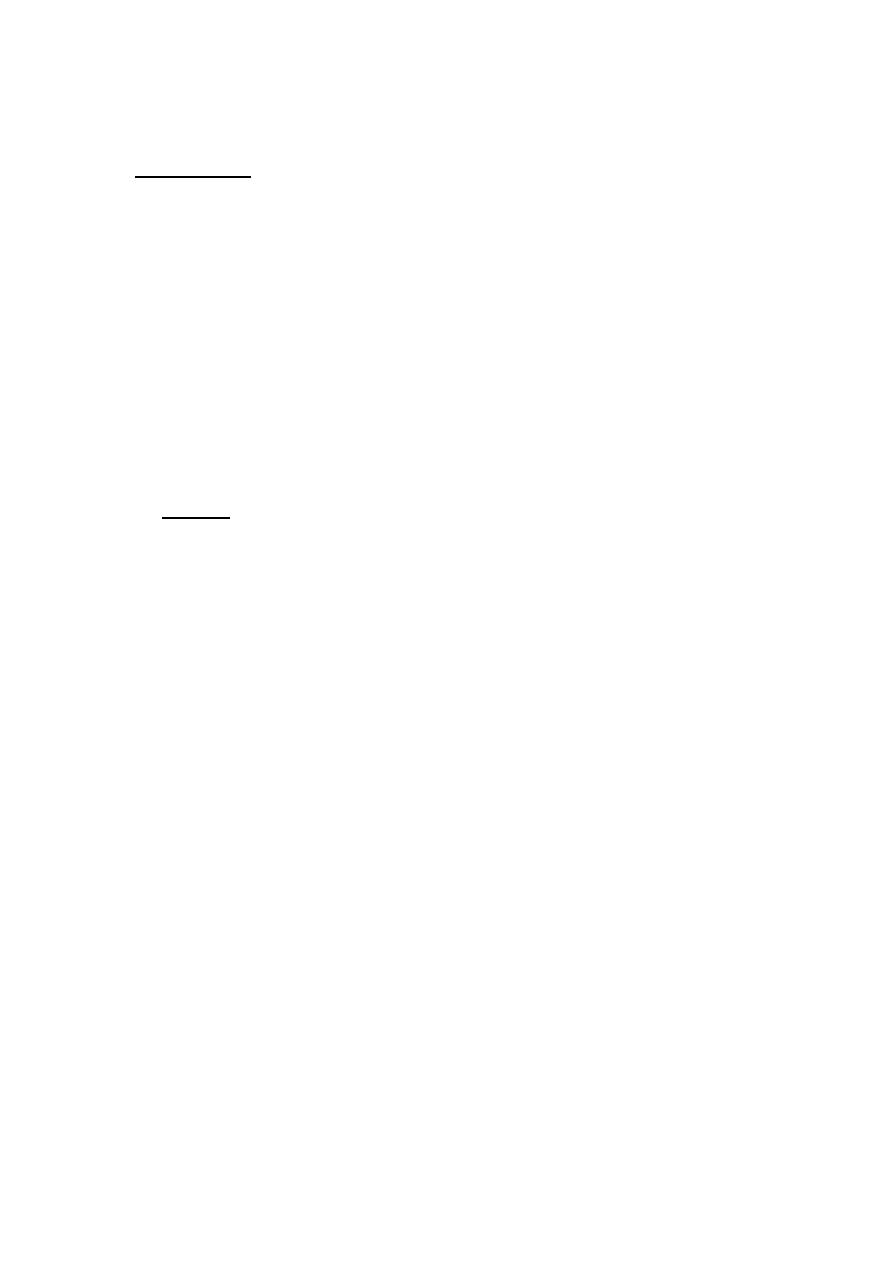
It is a premature separation of the placenta leading to bleeding from
the placental bed of a normally sited placenta. It can be revealed or
concealed.
Aetiology and risk factors:
The causes of abruption are not known but the following factors are
associated:
1-Proteinuric maternal hypertension ,fetal growth restriction, due to
defective trophoblast invasion.
2-Multiparity
3-Trauma. ECV and seat belt injuries (rarely).
4-Overstretched uterus (polyhydramnios, multiple pregnancy) at the
time that the membranes rupture (sudden decompression).
5-Previous placental abruption.
6-PROM
7-Smoking, cocaine use, alcohol and folate deficiency
8-anticoagulant therapy.
Diagnoses
clinical presentation
1- MAJOR ABRUPTION
Women present with abdominal pain and vaginal bleeding. The
blood loss that is visible (revealed haemorrhage) is often less than the
degree of shock. (present with varying degree of shock).
On examination:
1 The uterus is woody hard; due to tonic contraction.
2 tender uterus
3 The fetal parts cannot be felt.
4 fetal movement may be decreased or the fetus may be dead.
5 CTG may demonstrate a non reassuring or abnormal FHR pattern.
2- MINOR ABRUPTION
Minor abruptions are often not diagnosed until after delivery. They
may present with:
• Mild abdominal pain associated with uterine tightening (contractions).
• APH.
• There may be uterine tenderness.
Occasionally U\S demonstrate the presence of retroplacental clots but it is
un reliable diagnostic tool.
Management
Major placental abruption is a life-threatening condition for both the
mother and the baby.
If the fetus is still alive:
• ABC: Insert two large-bore i.v. cannulae and infusion of normal
saline/colloid.
• Send blood for cross-match of 4 units, haemoglobin and coagulation
studies.
• Immediate Caesarean section if necessary to save the baby’s life
• there is high risk of postpartum haemorrhage (BE CAREFUL).
• Adequate fluid replacement following the Caesarean section.
• Monitor urine output
If the fetus is dead, then the woman should be allowed to deliver
vaginallyvitally stable .

This usually happens rapidly (within 4–6 hours) as the abruption
stimulates labour.
If not in labour induce it if not contraindicated.
C/S if there is obstetrical indication
• Epidural analgesia is contraindicated because of the risk of
coagulopathy If a coagulopathy has developed or the woman starts to
bleed, she should be managed in conjunction with a consultant
haematologist.
(a) Give fresh frozen plasma.
(b) Ask the blood bank to get 6 units of platelets ready.
The consumptive coagulopathy begins to improve immediately after
uterine evacuation and resolve within 4–6 hours of delivery of the
placenta.
Complications and effects of placental abruption
1-Hypovolemic shock :There is a tendency to under estimate the
blood loss either due to concealed hge or in cases of hypertension.
Central venous pressure monitoring is helpful in blood loss assessment
and accurate fluid replacement.
2-DIC
3-Acute renal failure:secondary to poor renal perfusion,hypovolemia
,hypotension and DIC.the prognoses is excellent.
4-fetomaternal hge: which is imp in Rh negative pts.so we should do a
kelihauer test.
5-perinatal mortality:influenced by size of abruption , interval to
delivery,GA and other associations like FGR or PE.
6-FGR: in cases of recurrent chronic abruption.

Vasa praevia
It is acondition when fetal vessels traverse the fetal membranes over the
internal cervical os.
It is usually suspected when either spontaneous or artificial rupture
of membrane accompanied by painless fresh vaginal bleeding from
rupture of the fetal vessels ,so the lost blood is fetal in origin and
the fetus can rapidly exsanguinate ; so should be managed
immediately once suspected by emergency C\S if the baby still
alive.
