Lecture 11 pathology LIVER 3
rd
Stage
1
Anatomy
Wedge shaped organ formed by 4 lobes (Rt., Lt., caudate& quadrate lobes)
normal adult liver weight is 1400_1600 gm ,(2.5%) of the body weight .
blood flow : 60_70% portal vein , 30_40% hepatic artery
Microarchitecture :
1-2 mm hexagonal lobules oriented around central veins. The acini are
triangular in shape with the central vein at the apices & terminal twings of
hepatic artery & portal vein at the base .
Hepatocytes form plates or cords arranged radially around central veins.
Those situated near portal tract are referred to as "limiting plates ".
Vascular sinusoids are formed between hepatocytes cords .They are lined
by discontinuous endothelial cells which demarcate an extrasinusoidal
space (space of Disse).
"Ito cells ": fat containing cells of mesenchymal origin are found in the space
of Disse .The vitamin A is mainly stored within these cells .
"Kupffer cells : are attached to the luminal surface of endothelial cells .
Bile canaliculi :are formed by grooves in the plasma membrane of facing
cells, these begin in the centrilobular region & progressively join to drain
into the canal of Hering which are terminal parenchymal tributaries of bile
duct system .
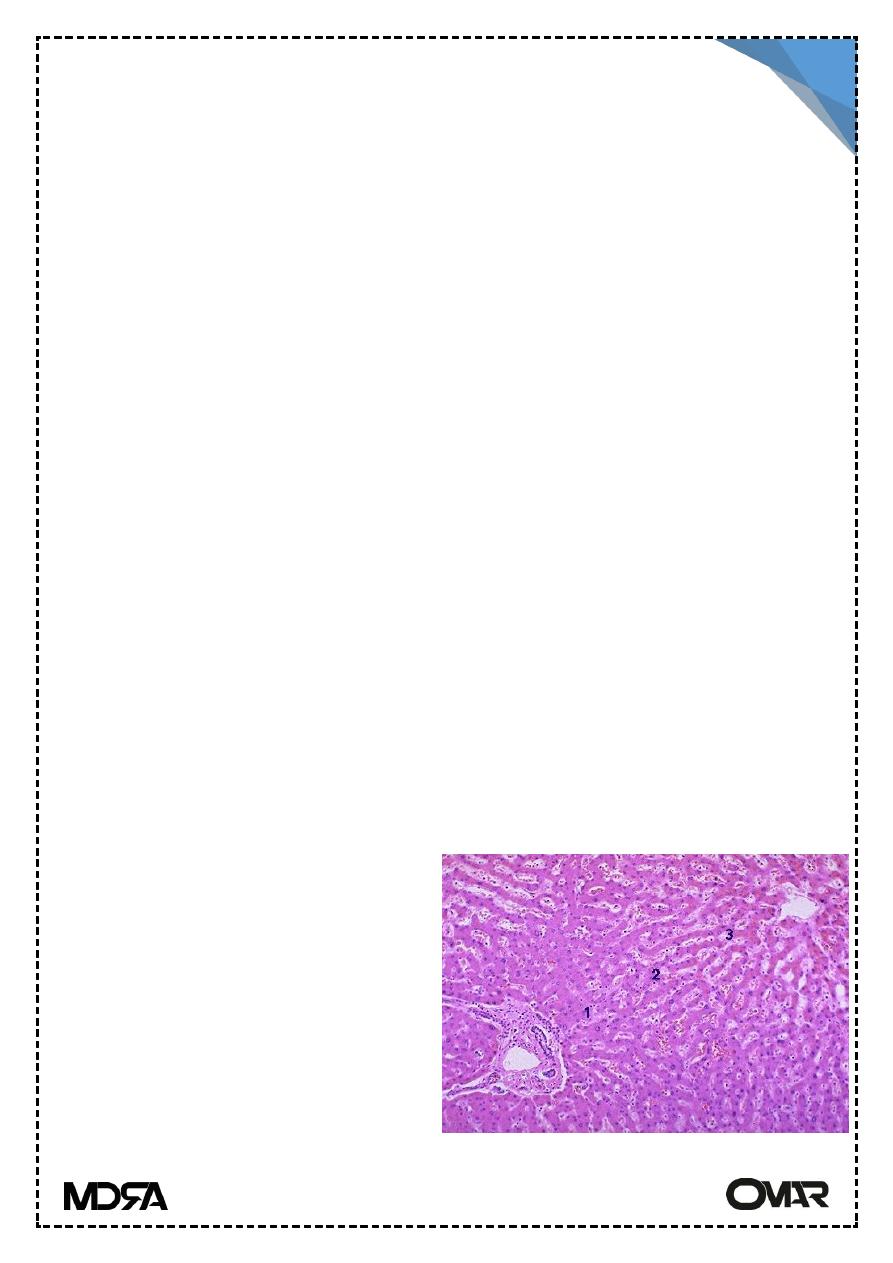
Liver is divided into lobules. The
center of the lobule is the central
vein. At the periphery of the
lobule are por tal triads.
the liver can be divided into three
zones, based upon oxygen supply.
Zone 1 encircles the portal tracts
where the oxygenated blood from
hepatic arteries enters. Zone 3 is
Lecture 11 pathology LIVER 3
rd
Stage
2
located around central veins, where oxygenation is poor. Zone 2 is located
in between
Morphological patterns of hepatic injury :-
1- Degeneration & intracellular accumulation :
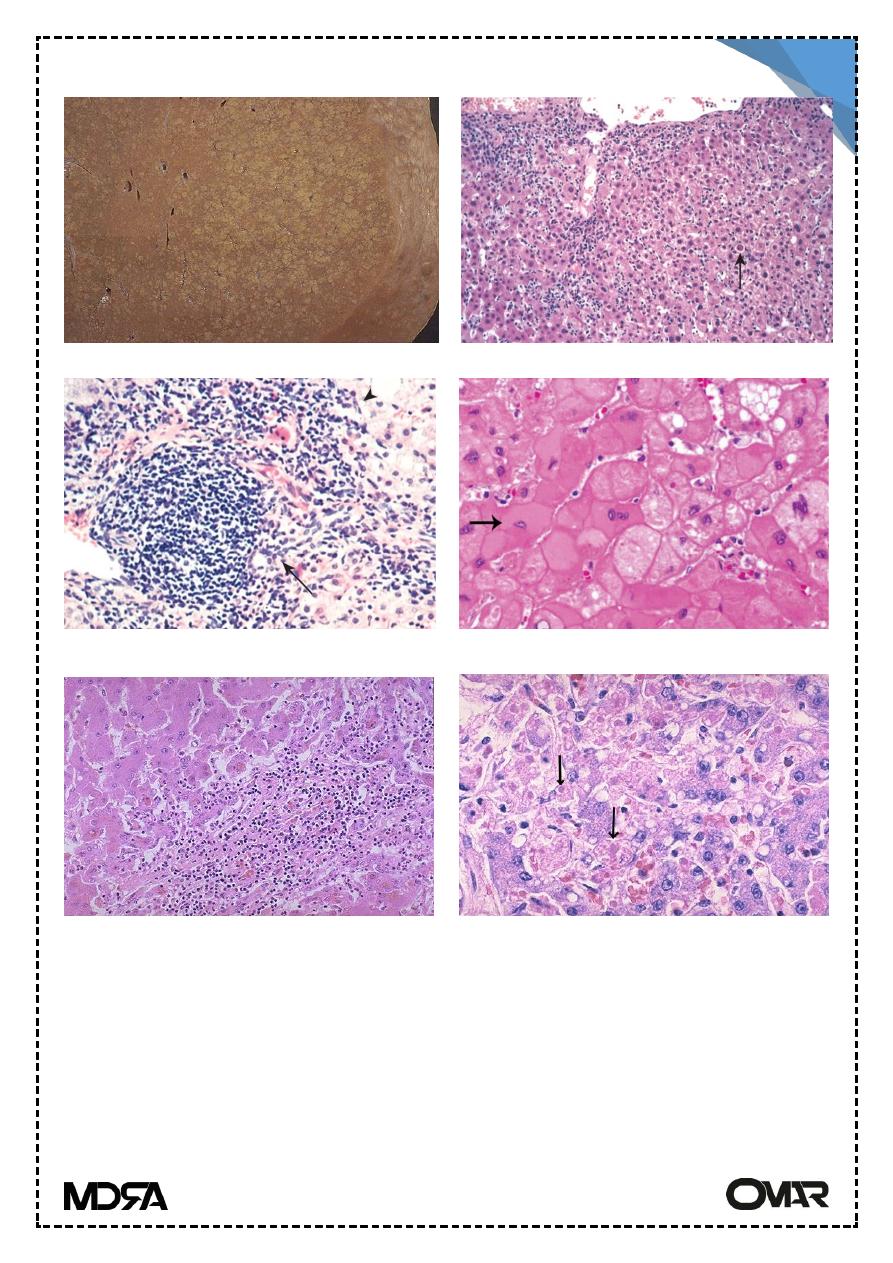
A. Ballooning degeneration : a swollen edematous appearance with
irregularly clumped cytoplasm & large clear spaces following toxic or
immunological insult .
B. Foamy degeneration : a diffuse foamy swollen appearance due to
retained biliary material .
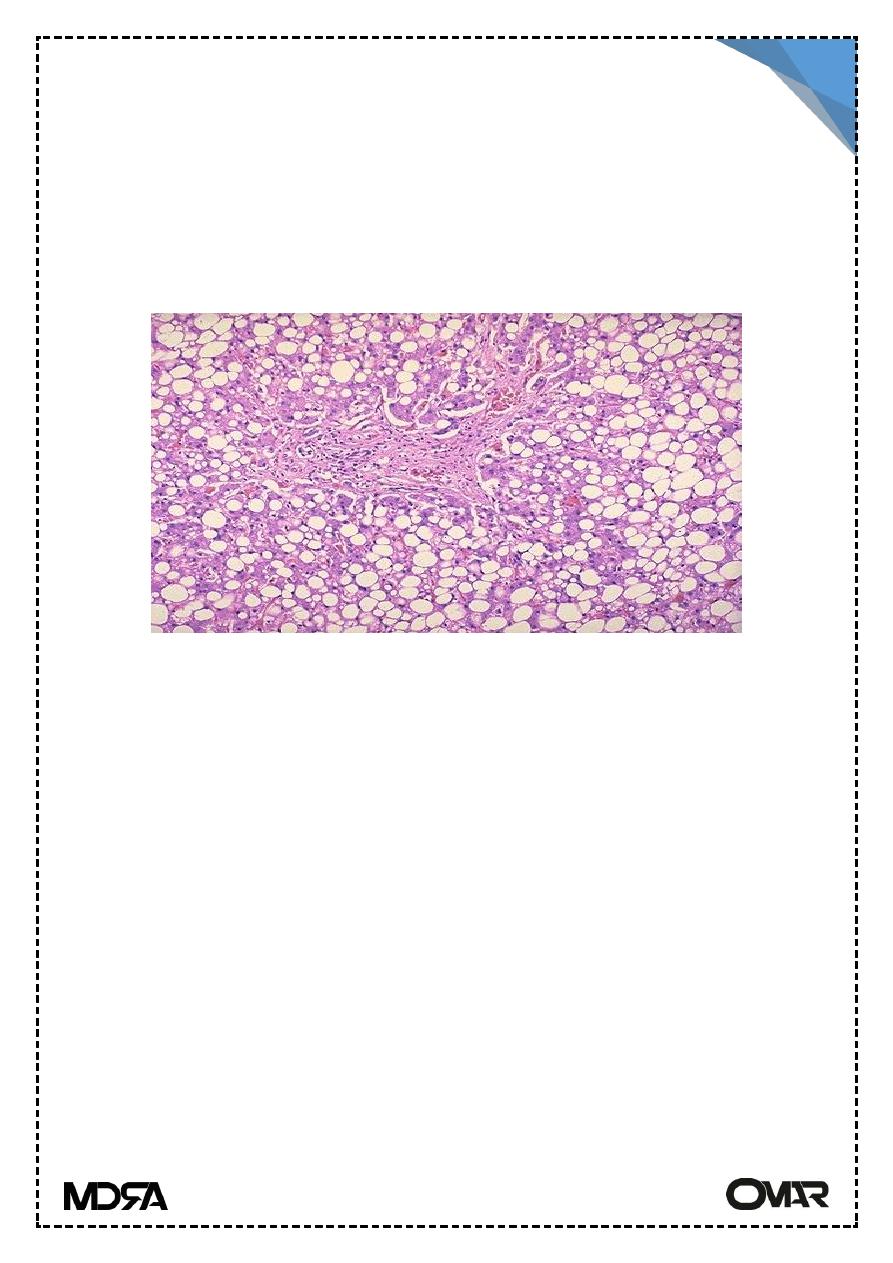
C. Steatosis : accumulation of fat droplets within hepatocytes
.Microvesicular multiple tiny droplets that are do not displace the nucleus
. Macrovesicular ; single large droplet that displace the nucleus .
Deposition of iron & copper
2- .Ncrosis& Apoptosis :
A.Ischemic coagulative necrosis: hepatocyts are poorly stained
mummified with lysed nuclei .
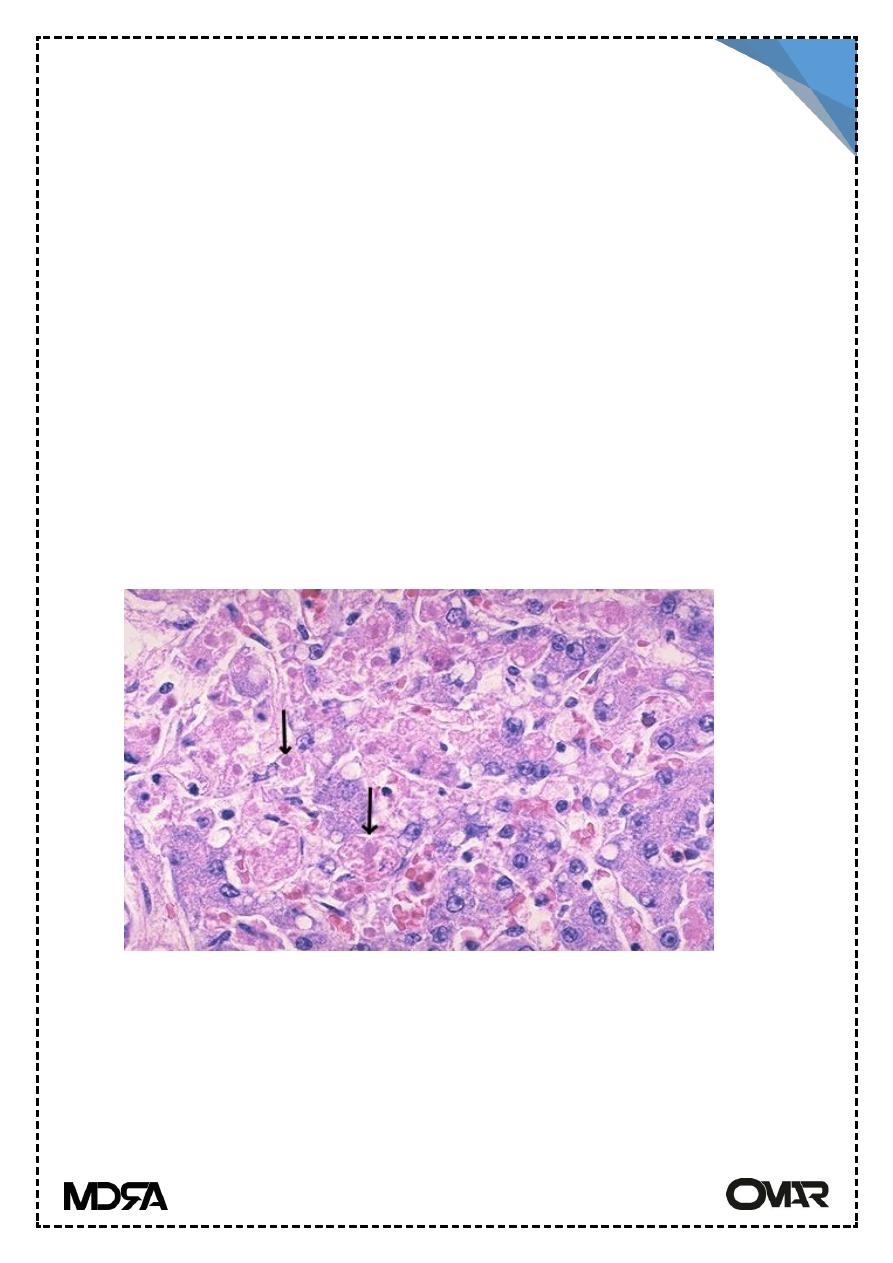
Ballooning degen.& Coucilman body
Lecture 11 pathology LIVER 3
rd
Stage
3
B.Coucilman bodies : isolated hepatocytes round up to form shrunken
,pyknotic & intens ly eosinophilic bodies when cell death is toxic or
immunologically mediated . Nuclei are fragmented (apoptosis) .
Lytic necrosis :hepatocytes osmotically swell & rupture .
o Centrilobular necrosis : in hepatocytes around the central vein
immediately .(ischemia, drugs& toxic reaction)
o Midzonal& periportal necrosis:rare ,periportal occur in eclampsia of
pregnancy
o Focal necrosis : limited to the interface between periportal parenchyma
&inflamed portal tract.
o Bridging necrosis : in severe inflammatory injury , necrosis of contiguous
hepatocytes may span adjacent lobules in a portal _ portal ,portal _
central or central_central fashion .
o Submassive necrosis : entire lobule .
o Massive necrosis : most of liver , accompanied by liver failure
o Macroscopic abscesses : disseminated bacterial or candidal infection .
3- Inflammation :
Injury to the liver associated with influx of acute or chronic inflammatory
cells .(e.g. hepatitis )
Lecture 11 pathology LIVER 3
rd
Stage
4
4- Regeneration :
Which occurs in all but the most fulminant diseases . Proliferation is seen
as mitoses ,thickening of the cords & disorganization of the parenchymal
structure .The liver cells are stable cells ; they gain the ability to divide
(mitoses) after any injury or need .
5- Fibrosis :
Is generally an irreversible consequence of hepatic damage it forms in
response to inflammatory process or direct toxic insult to the liver .
The liver is subdivided into nodules & regenerating hepatocytes
surrounded by scar tissue termed (cirrhosis) an end form of liver disease .
Viral Hepatitis
Clinical presentation
It may be asymptomatic or associated with malaise, weakness, nausea,
anorexia.
Laboratory finding:
Markedly elevated alanine aminotransferase (ALT) & asparatate
aminotranferase (AST). Serum alkaline phosphatates may be mildly elevated.
Systematic viral infections can involve liver including infections
mononucleosis (EBV), CMV & herpes viruses, unless other wise specified viral
hepatitis is reserved for infection of the liver by group of viruses called
hepatotropic viruses , the main viruses are hepatitis A & E transmitted by fecal-
oral route & hepatitis B,C & D (transmitted by panenteral route), (table 1) .
Hepatitis A (HAV) : (Infectious hepatitis)
Is a self limiting disease transmitted by fecal-oral contamination may
occurs as endemic disease in countries with low level of hygiene & sanitation.
Clinically it's mild or asymptomatic & affecting mostly children.
HAV is an RNA entrovirus of the picorna group incubation period of 2-6
wks followed by fever, malaise, and anorexia. Jaundice appear 1 wk later
Lecture 11 pathology LIVER 3
rd
Stage
5
remaining for 2 wks. Fecal shedding of the virus in the stool start 2-3 wks before
& 1 wk after the onset of Jaundice.
HAV never causing chronic hepatitis or carrier state. Specific antibody
against HAV of IgM type appear at the onset of symptoms (marker of acute
infection) few months it will be decline & the appearance of IgG antibody which
give immunity against reinfection. (value of vaccination). viral shedding in stool
stops with the rise of IgM titre.
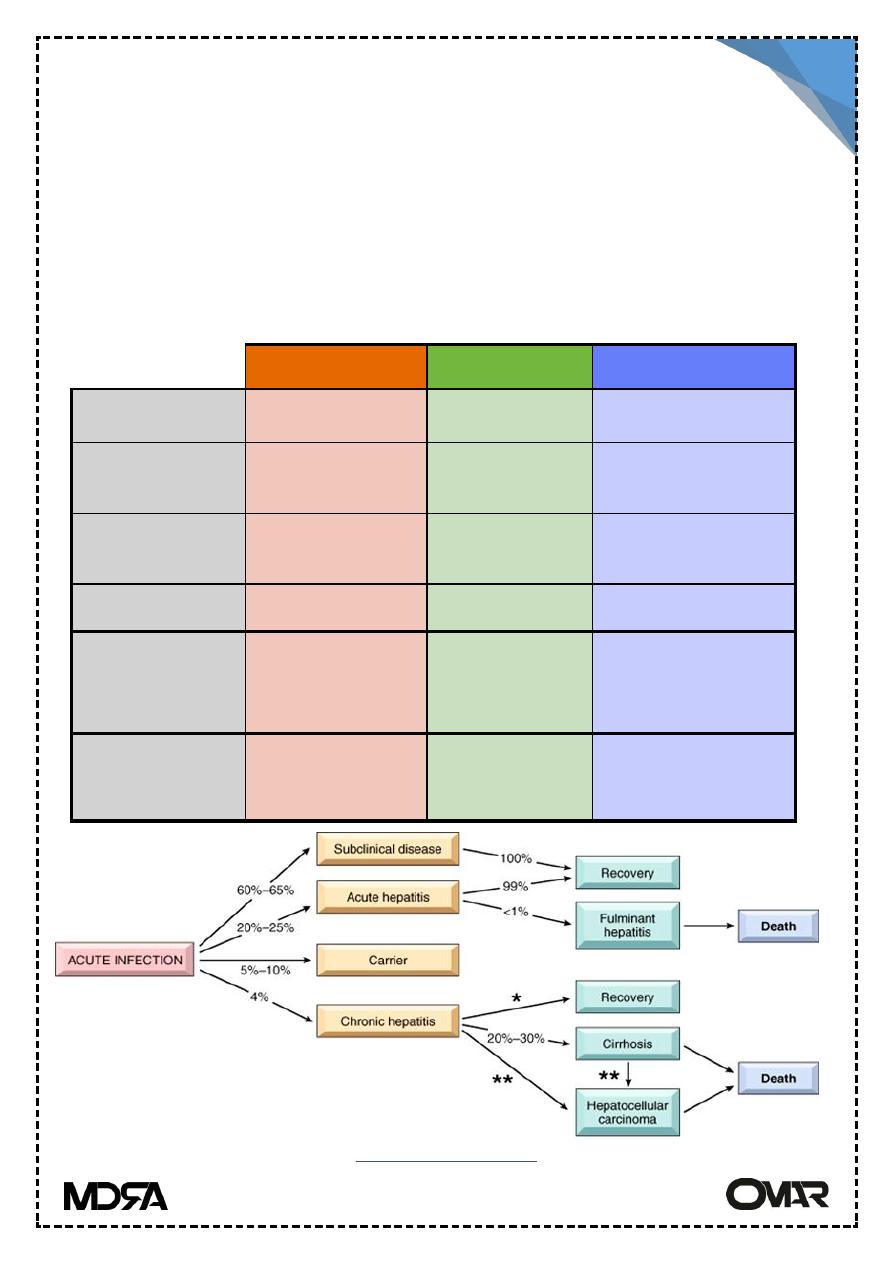
Hepatitis A
Hepatitis B
Hepatitis C
Transmission
Fecal-oral
Parenteral
Parenteral
Chronic
Hepatitis
None
5%
>85%
Fulminant
hepatitis
0.1%
0.1-1.0%
Rare
Carcinoma
No
Yes
Yes
Other stuff
50% of people
> 50 are +
Vaccine
effective
Most
common
reason for liver
transplant
Bottom line
Benign,
self-
limited disease
Most recover;
small % die
Nasty! Almost 10%
die
Hepatitis B outcomes
Lecture 11 pathology LIVER 3
rd
Stage
6
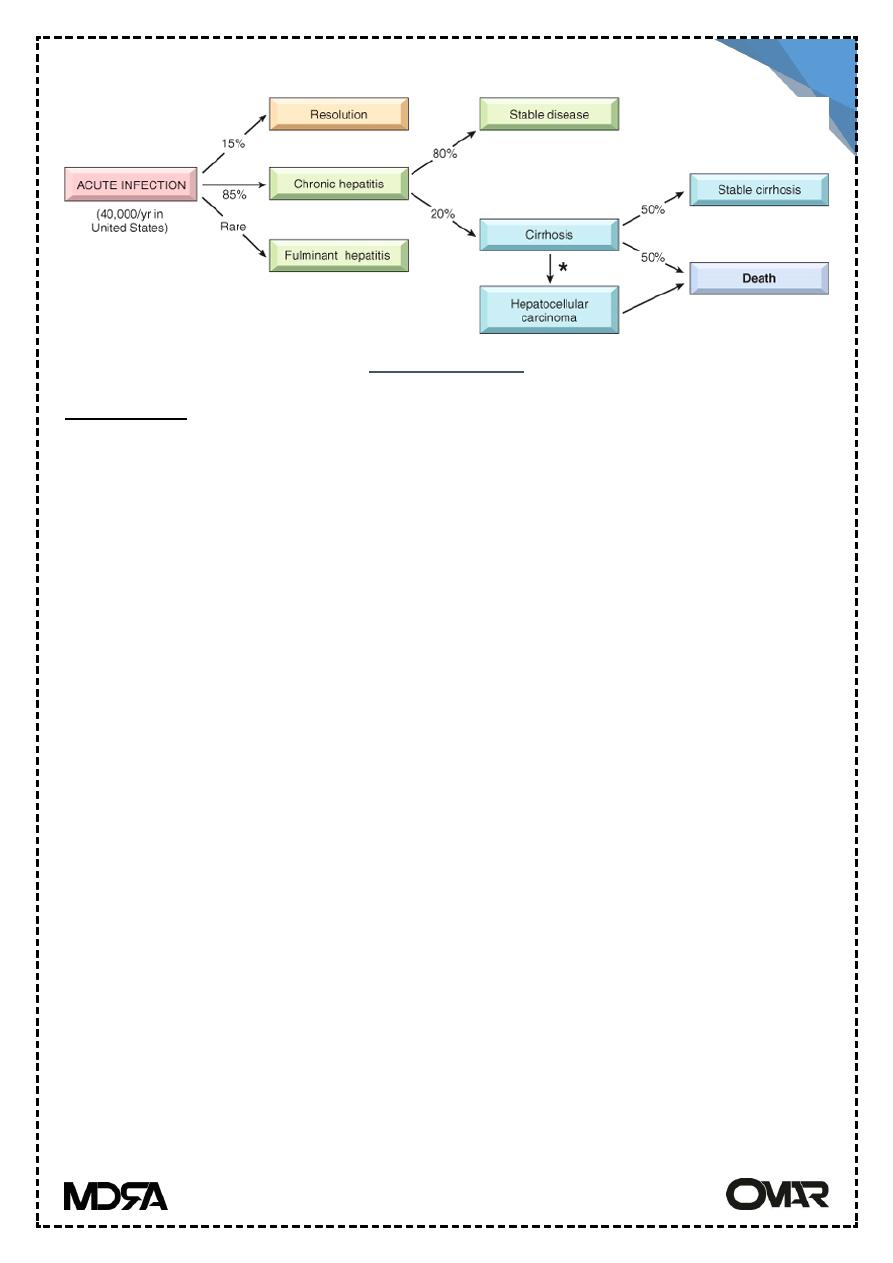
Hepatitis C outcomes
Hepatitis B (Serum Hepatitis)
Hepatitis B virus HBV is a DNA virus of the hepadna group, infective virus
is transmitted in blood, semen & saliva . Transfusion, blood products, dialysis,
needle-stick accidents among health care workers, intravenous drug abuse &
homosexual activity represent the primary risk categories of HBV infection.
Inoculation occurs in breaks in the skin & mucous membrane , vertical
transmission from mother to child is also seen, I.P is 6-8 weeks.
The viral genome encodes
Anucleocapsid core protein (HBc Ag ,hepatitis B core Ag) .
Envelop glycoprotein (HBs Ag, hepatitis B surface Ag).
A DNA polymerase which exhibit reverse transcriptase activity .
A protein from the x region (HBX) act as transcriptional transactivator ,is
necessary for viral replication ,play a role in hepatocellular carcinoma.
Serum hepatitis can produce :-
Acute hepatitis with complete recovery.
Chronic non progressive hepatitis. (subclinical )
Chronic disease ending in cirrhosis in less than 1% of cases
Fulminant hepatitis with massive liver necrosis .
a symptomatic carriers state
Lecture 11 pathology LIVER 3
rd
Stage
7
Viral hepatitis
Acute viral hepatitis
Chronic viral hepatitis
Chronic viral hepatitis: ground-glass hepatocytes
Interface hepatitis Interface hepatitis
Carrier state :
The presence of HBs Ag in serum for 6 months after initial detection . the
patient may be asymptomatic.
*the persistence of HBs Ag, HBe Ag & HBV DNA with anti HBc Ab indicates
chronic replication & progressive liver damage.
Lecture 11 pathology LIVER 3
rd
Stage
8
Serological tests
1.HBs Ag appear before onset of symptoms peaks during disease& decline to
very low levels in 3-6 months .
2.HBe Ag ,HBV DNA,DNA polymerase appear after HBs Ag all signify active
replication
3. Anti-HBc IgM appears shortly before onset of symptoms , during months it's
replaced by IgG anti –HBc.
4. IgG anti –HBs appear after disappearance of HBs Ag & rise when acute
disease is over. It may lasts for life conferring immunity.
Bacterial Infection of Liver
three main routes:
Ascending spread from colonization of the biliary tract by bacteria.almost
always follow biliary obstruction
Infection ascending in the portal vessels (portal pyaemia) into the liver from
a focus of sepsis in the abdomen, e.g. abscess caused by complicated
appendicitis
Systemic blood spread in septicaemia.
TB infection of the liver is seen in miliary tuberculosis.
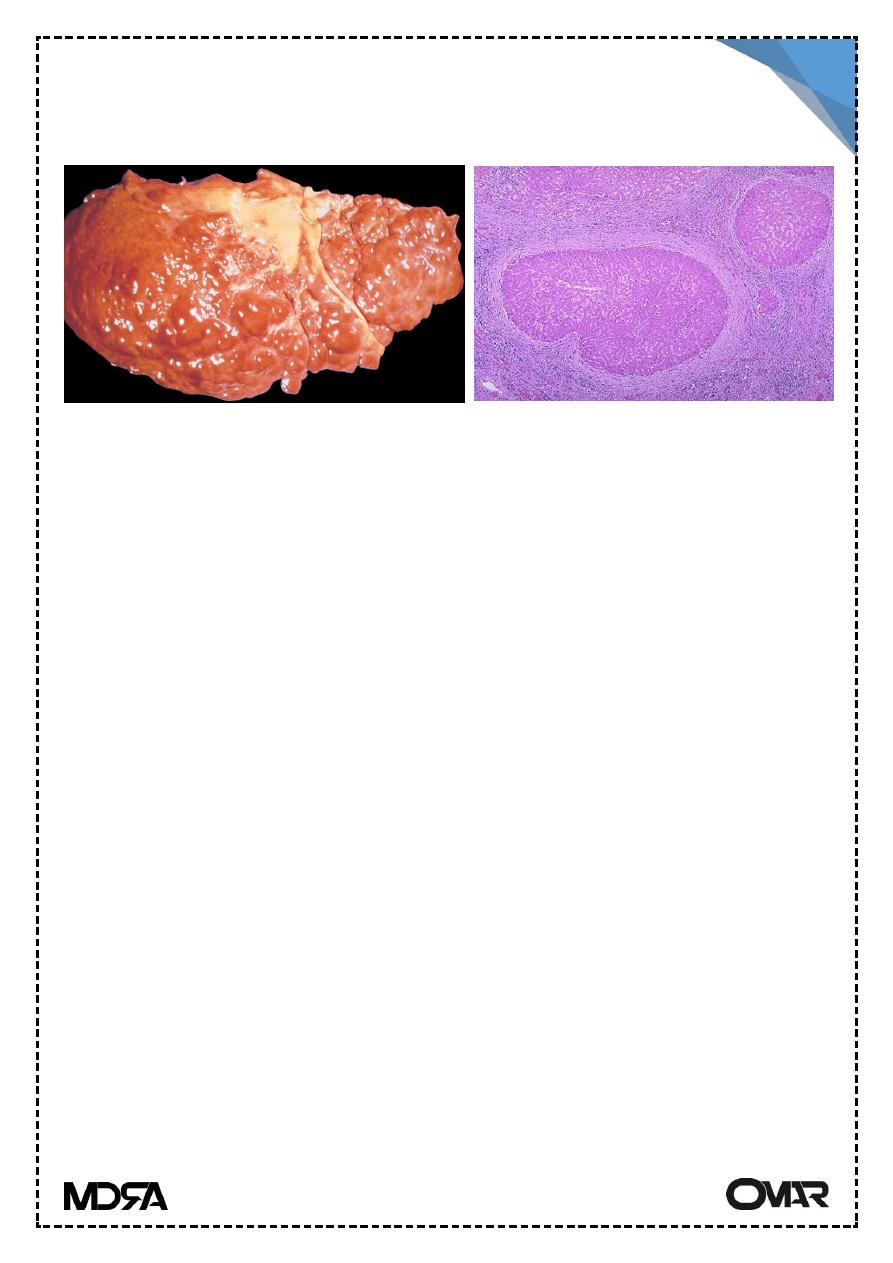
Cirrhosis :
Among the top ten causes of death in the western world .
Characteristics:
Bridging fibrosis : delicate bands or broad scars replacing multiple lobules
Parenchymal nodules :caused by regeneration of encircled hepatocytes
.small < 3mm _several cm (macronodules )
Disruption of architecture of the entire liver parenchymal injury & fibrosis
are diffuse.If the injury is focal , there is no cirrhosis .Nodularity is important
Lecture 11 pathology LIVER 3
rd
Stage
9
for the diagnosis, it reflect a balance between the regeneration & scarring .
fibrosis is irreversible.
Cirrhosis
Common
Alcoholic liver disease
Cryptogenic (no cause found on investigation)
hepatitis B and hepatitis C viruses
Uncommon
Autoimmune chronic hepatitis and PBC
Chronic biliary obstruction (biliary cirrhosis)
Cystic fibrosis
Treatable but rare
Haemochromatosis
Wilson's disease
Rare
Αl –antitrypsin deficiency
Galactosaemia
Glycogenosis Type IV
Tyrosinaemia
Lecture 11 pathology LIVER 3
rd
Stage
10
Pathogenesis :
In the normal liver interstitial collagens type I&III are concentrated in the
portal tracts & around central veins ,
occasional bundles found in the space of Disse .
In cirrhosis , delicate septal tracts are formed by deposition of type I&III
collagen in the lobules .
There is loss of sinusoidal endothelial fenestration with impairment of
hepatocellular secretion of proteins & continued fibrous deposition in the
space of Disse of normal parenchyma .
The source of excess collagen is the perisinusoidal hepatic stellate cells (Ito
cells), become activated & transform into myofibroblast-like cells .
Sources of collagen synthesis stimulation :
o Inflammatory cytokines : produced from chronic inflammation ( TNF-α
& TGF-β & IL-1).
o Cytokine production of stimulated endogenous cells (kupff.cells
,endothelim,hepatocytes & bile duct epith . cells).
Blood delivery to hepatocytes is compromised .Hepatocytes are stimulated
to regenerate within a spherical nodules .
Disruption of the interface between portal tracts & parenchyma obliterate
the biliary channels → jaundice .
Clinical features
Clinically silent .
Non-specific clinical signs & symptoms : anorexia, wt. loss, weakness,
&frank debilitation .
Hepatic failure, is precipitated by hepatic metabolic load as in systemic
infection or GI bleeding .
Hepato-pulmonary syndrome : imbalance of pulmonary blood flow .
Lecture 11 pathology LIVER 3
rd
Stage
11
Complications
The main consequences of cirrhosis:
Reduced hepatocyte function (decreased synthesis of protein & failure of
detoxification.
Disturbance of blood flow through the liver, causing portal hypertension
with all its complications
Reduced immunity and increased susceptibility to infection
Increased risk of development of hepatocellular carcinoma
Increased risk of development of portal vein thrombosis
Acute liver failure
Chronic liver failure
Death is due to :
Progressive liver failure.
portal hypertension & it's complication .
Hepatocellular carcinoma.
Hepatic Failure
the result of sudden & massive hepatic destruction or the end point of
progressive damage to the liver.80-90% of hepatic functional capacity
should be lost .
Morphological Alterations:
Massive hepatic necrosis due to fulminant viral hepatitis , drugs &chemicals
such as acetaminophen (paracetamol), halothane, anti-TB drugs
(rifampicin&INH), antidepressant MAOinhibitors ,industrial chemicals
(CCl4)&mushroom poisoning.The damage to the liver is either direct toxic
damage to the hepatocyts, or combination of toxicity &inflammation
hepatocytes destruction .
Lecture 11 pathology LIVER 3
rd
Stage
12
Chronic liver disease : chronic hepatitis & alcoholic liver disease ending in
cirrhosis.
Clinical features
Hypoalbuminemia→ peripheral edema .
Hyperammonemia→ cerebral compromise .
Fetor hepaticus → musty sweat & sour body odor.
Spider angiomas (talengectasia) & palmar erythema due to ↓ metabolism
of estrogen & hyperestrogenemia
male hypogonadism & gynecomastia .
Coagulopathy : decrease synthesis of clotting factors (II,VII,IX&X)
*Severely impaired liver function leads to multiple organ failure
*Two complications are important :
Hepatic encephalopathy : disturbances in consciousness,fluctuating
neurologic signs due to abnormal neurotransmission in CNS, related to
increase blood ammonia which impair neuronal function & promote
generalized brain edema .
Hepatorenal syndrome : appearance of acute renal failure in sever liver
disease with no intrinsic morphologic or functional cause for renal failure .
