
Thrombo-embolism in Pregnancy:
Denotes all vascular occlusive
processes including thrombophlibitis,
phlebothrombosis, septic thrombophlibitis
and embolisation of venous clots to the
lungs.
Phlebothrombosis
: refers to the
formation of a thrombus within the veins,
can occur anywhere in the venous system
but the clinically predominant sites are in
the vessels of the legs giving rise to deep
venous thrombosis and in the lungs
resulting in pulmonary embolism
.

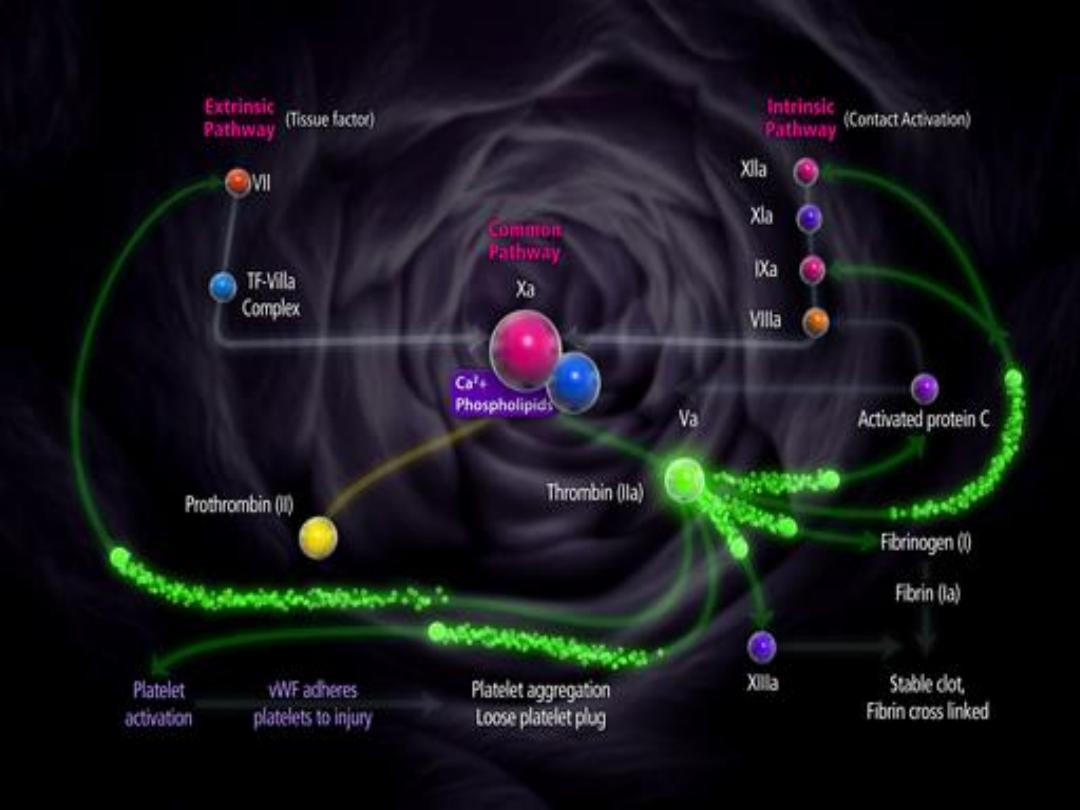
The patho-physiology of venous
thrombosis in pregnancy
related to
increased venous stasis but alterations
in the balance of proteins of the
coagulation and fibrinolytic systems have
a role.
Incidence:
It’s 3- 5 times common in pregnancy
than non pregnant.
Its 3-7 per 10,000 maternities ante-
natal and
6 -12 per 10,000 post- natal.
Cesarean Section increases the incidence
to 1-2%.

Risk factors
Pregnancy is hyper-coagulable state due
to Increased clotting factors during
pregnancy like Factor XI,X,VII,II.
Decreased fibrinolytic activity.
Obesity, Operative delivery.
Restricted activities due to complications
of pregnancy.

Acquired thrombophilia
It’s associated with the
antiphospholipid syndrome .It is
the combination of lupus
anticoagulant (LAC) with or
without, anticardiolipin
antibodies (ACA), with a history
of
recurrent miscarriage
and or
thrombosis
.
Inherited thrombophilias
Protein-C, protein-S, and
Antithrombin III deficiency

Maternal age > 35 years.
Pre-pregnancy weight > 80 kg.
Pre-existing Thrombophilia.
Previous DVT.
Severe varicose veins .
Prolonged bed rest.
Multi foetal pregnancies.
Severe pre-eclampsia.
Caesarean section delivery.
Sepsis, especially pelvic.

Diagnosis:
History:
Clinical presentation.
The symptoms and signs of VTE include
leg pain and swelling (usually unilateral),
lower abdominal pain, low-grade pyrexia,
For PE.dyspnoea, chest pain, haemoptysis
and collapse .
Risk factors.
Medical history
Exam.
Investigations


Compression duplex ultrasound:
It is the primary diagnostic test for
DVT should be undertaken where
there is clinical suspicion of DVT.
If it is negative and there is a low
level of clinical suspicion,
anticoagulant can be discontinue
If it confirms the diagnosis of DVT
anticoagulant treatment should be
continued.

If it is negative and a high level of
clinical suspicion exists, anti-
coagulation continue and
ultrasound repeated in Day 3 and
Day 7 or an alternative diagnostic
test employed. If repeat testing is
negative, anticoagulant should be
discontinued.
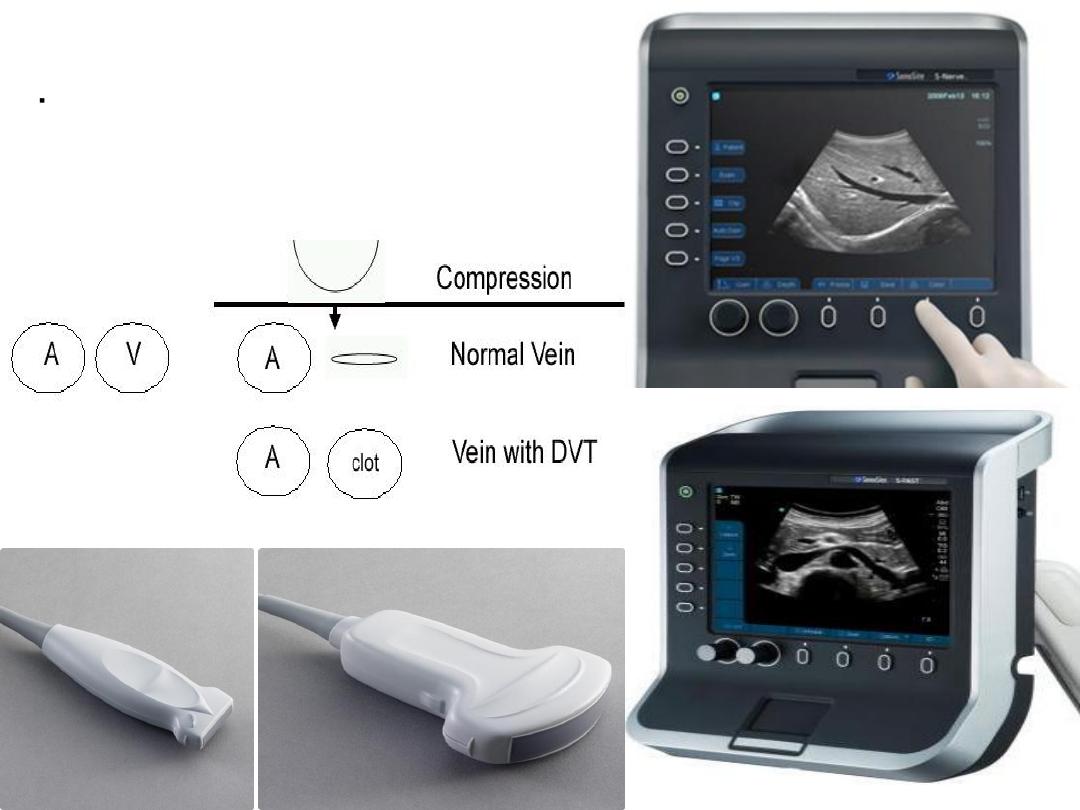
High resolution B-mode
ultrasound system
l Linear array transducers:
3-5 MHz - Large legs
5-10 MHz – Small legs
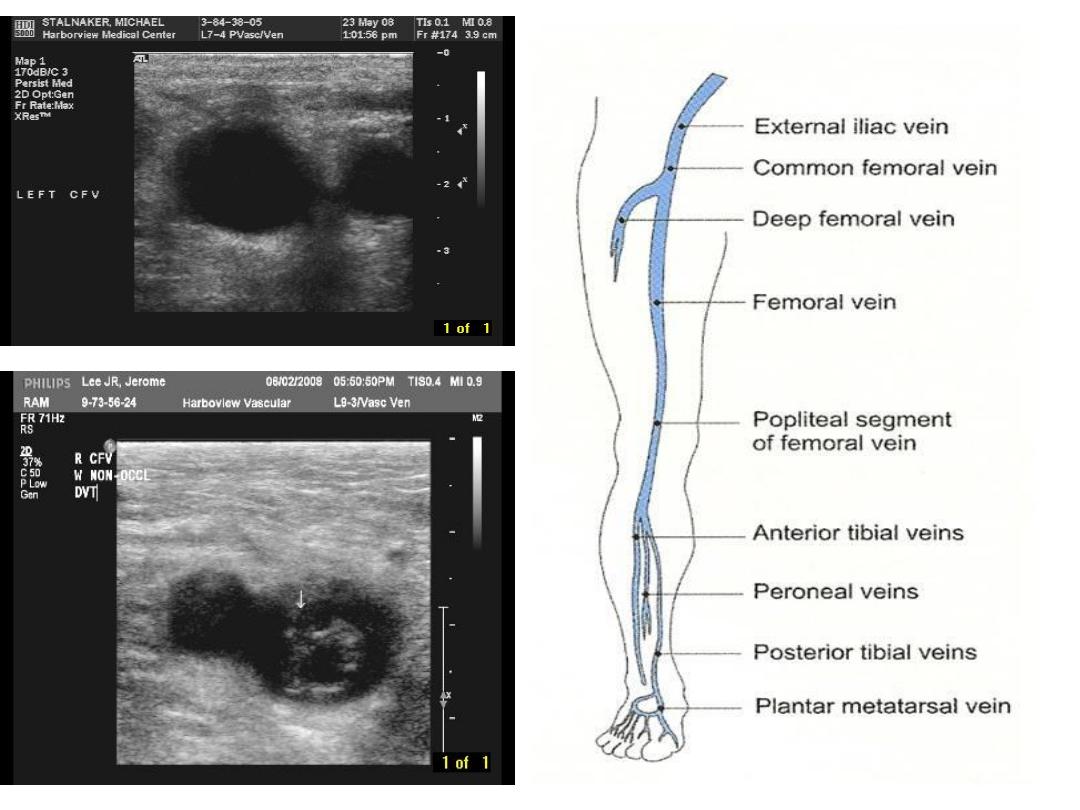

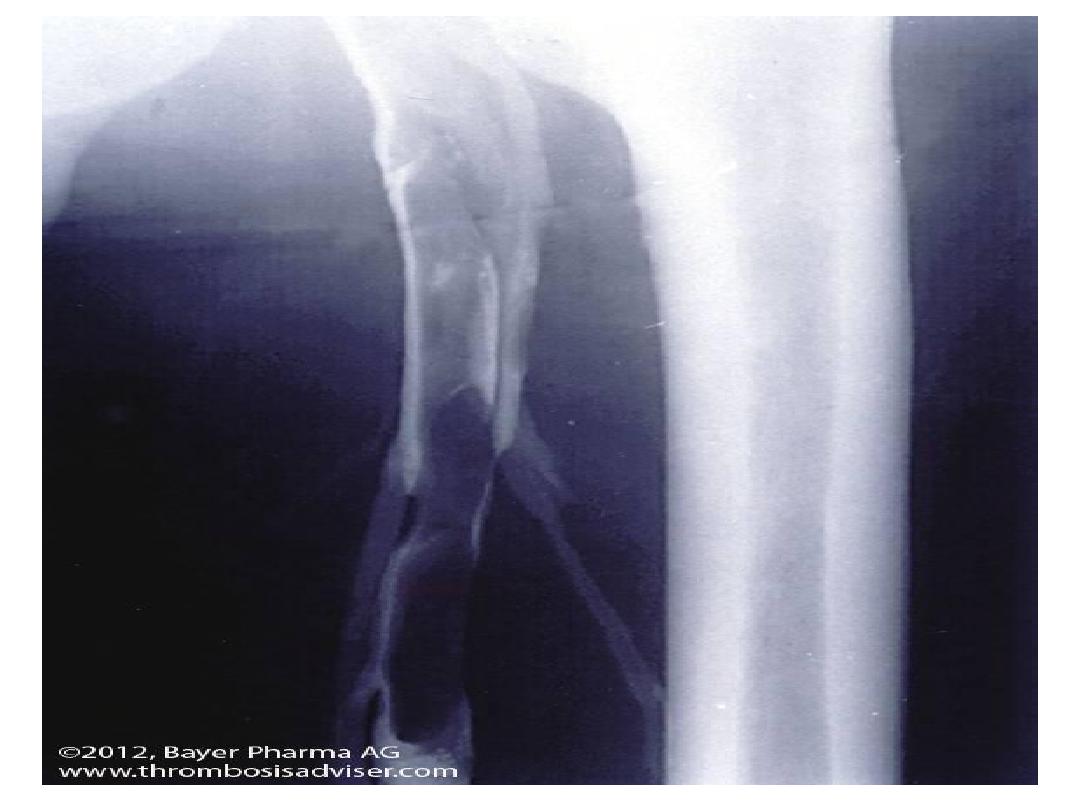
Venography:
it is an invasive procedure, requiring the
injection of a contrast medium and the
use of X-ray, is not preferable during
pregnancy.
It’s best when iliac vein thrombosis is
suspected (if back pain and swelling of
the entire limb).
Magnetic resonance venography or
Conventional contrast venography may
be considered.

Full blood count.
Coagulation screen.
D- dimer :should not been performed in
acute VTE in pregnancy.
Blood urea and electrolytes
Liver function test
Performing a thrombophilia screen prior to
therapy is not routinely recommended

For PE: with symp.&signs ,CXR ,ECG.
If no symptoms do ,CT Pulmonary
angiography ,Ventilation –perfusion scan
:
carries a increased risk of childhood
cancer compared with CTPA (1/280,000
versus less than 1/1,000,000) but has a
lower risk of maternal breast cancer
(lifetime risk increased by up to 13.6%
with CTPA, background risk of 1/200).
Pulmonary angiography The average fetal
radiation dose with CTPA is less than 10%
of that with V/Q scanning

Chest X-ray
Chest X-ray is normal in over 50%
ofpregnant women with proven PTE,
Abnormal CXR + susp.PE do CTPA
abnormal features caused by PTE include
atelectasis, effusion, focal opacities,
It may identify other pulmonary disease
such as pneumonia, pneumothorax or
lobar Collapse. regional oligaemia or
pulmonary oedema

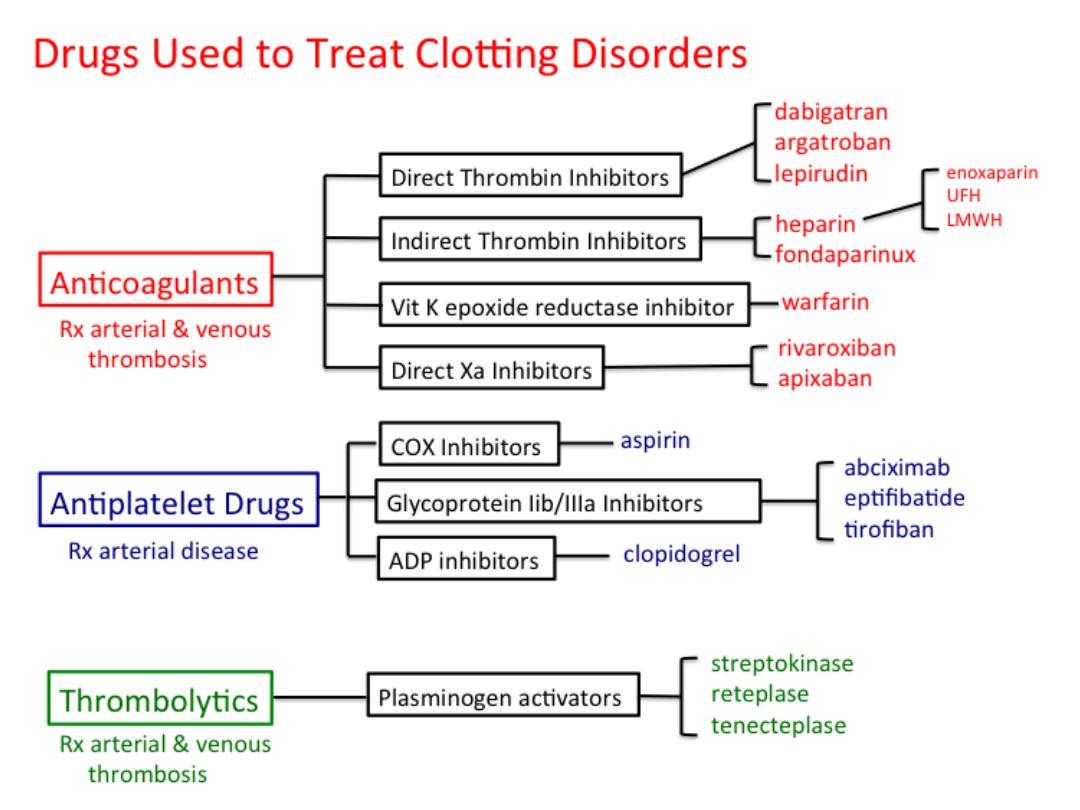
Anticoagulant therapy
:
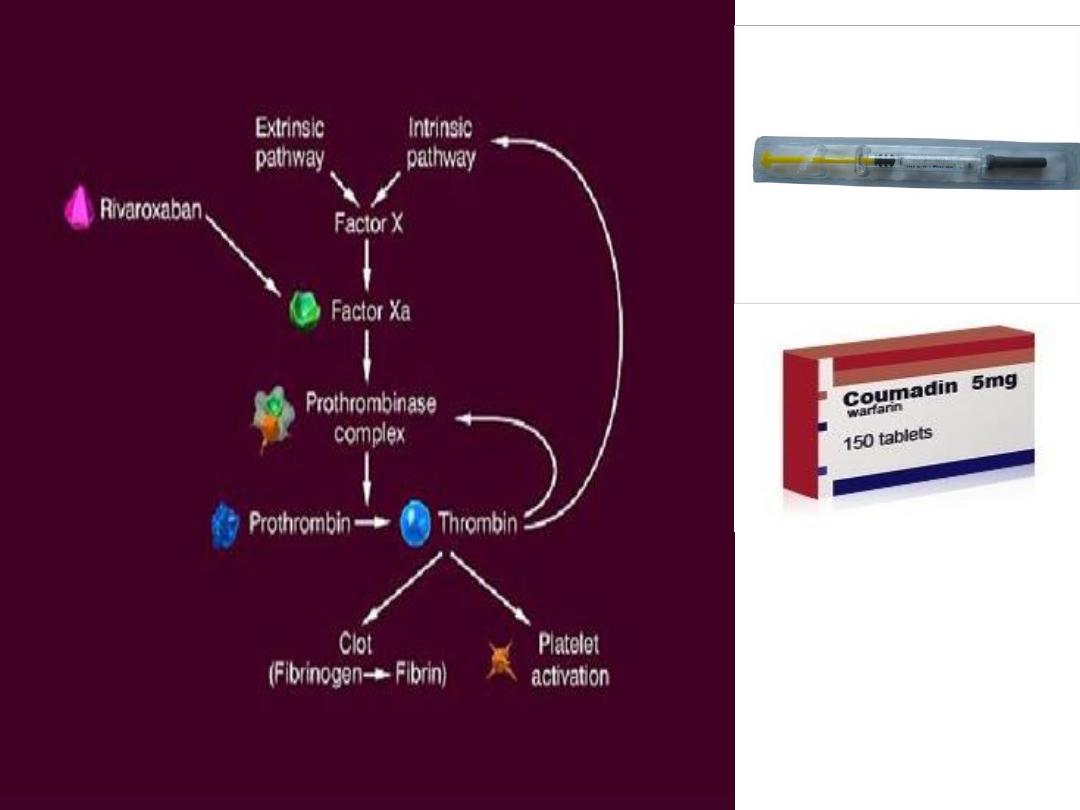
1- Heparin;
It does not cross the placenta, not
teratogenic.
.Un-fractioned Heparin prolongs the
activated partial thromboplastin time
(APTT).
While LMW heparins affect factor X activity.
it’s effect can be stopped within hours .
It’s prolonged therapy for more than 6
months may be associated with
idiosyncratic reaction, thrombocytopenia
and higher risk of osteoporosis
.

In clinically suspected DVT or PTE,
treatment with LMWH should be
given until the diagnosis is excluded
by testing.
Treatment of VTE in pregnancy:
Dose: (enoxaparin 1 mg/kg twice
daily; dalteparin 100 units /kg twice
daily).

When delivery is planned, LMWH
maintenance therapy should be
discontinued 24 hours before planned
delivery, or when labor established.
Regional anesthetics or analgesic
techniques should not be undertaken
until at least 24 hours after the last
dose of therapeutic LMWH.

A thromboprophylactic dose of
LMWH should be given by 3 hours
after a caesarean section (more
than4 hours after removal of the
epidural catheter).
The epidural catheter should not be
removed within 12 hours of the
most recent injection.

Anticoagulant prophylaxis
Women had non-estrogen related
DVT or associated with temporary
risk factor no ante-natal
prophylaxis.
Prophylaxis in the peurperium.
Women with a history of DVT
occurring during pregnancy or
recurrent DVT are given prophylactic
LMW heparin ante-natal .
Women with a history of recurrent
DVT or DVT occurring in the non-
pregnant state + thrombophilias, or
+ve family history or multiple risk
factors offered anticoagulant
prophylaxis ante-natal and post-
natal for 6 weeks.
Women with artificial heart valves
definite history of previous
pulmonary embolism require full
anticoagulation throughout
pregnancy and post-natal.

2- Oral Anticoagulant,
Warfarin:
It prolongs the prothrombin time (PT).
It crosses the placenta and can cause limb
and facial defects characteristic embryo-
pathy in the first trimester, central nervous
system abnormalities at any trimester, fetal
hemorrhage and neonatal haemorrhage
Neither heparin (un-fractionated or LMWH)
nor
warfarin is contraindicated in breastfeeding.

PE , Once suspected, early
intervention by full I.V. anticoagulant
therapy may be life saving. Full I.V.
heparinization is immediately
started, with supportive oxygen
therapy.
Management should involve a
multidisciplinary resuscitation team
including senior physicians,
obstetricians and radiologists.
.
