Infective endocarditis
Pathophysiologytypically occurs at sites of preexisting endocardial damage
virulent or aggressive organisms (e.g. Staphylococcus aureus) can cause endocarditis in a previously normal heart
Many acquired and congenital cardiac lesions are vulnerable to endocarditis, particularly areas of endocardial damage caused by a high-pressure jet of blood
The avascular valve tissue and presence of fibrin and platelet aggregates help to protect proliferating organisms from host defence mechanisms
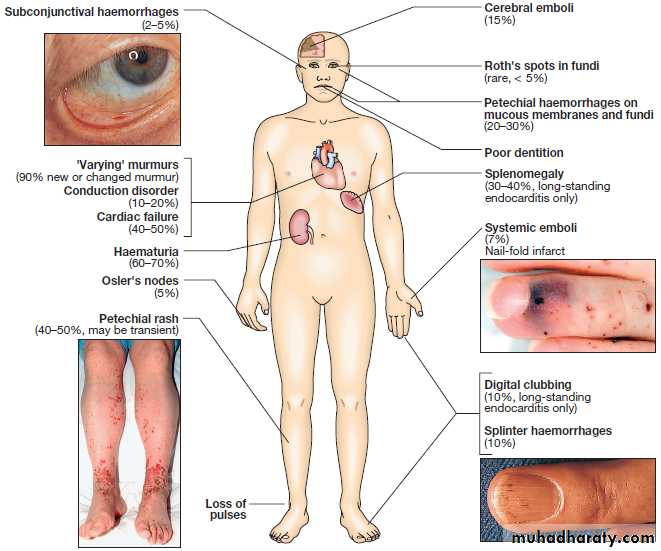
vegetations composed of organisms, fibrin and platelets grow and may become large enough to cause obstruction or embolism
Extracardiac manifestations, such as vasculitis and skin lesions, are due to emboli or immune complex deposition
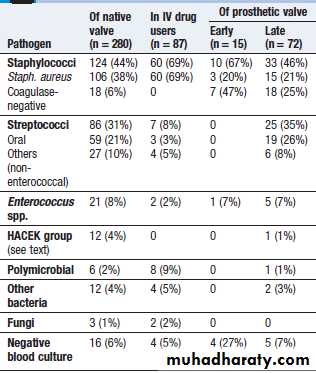
Microbiology
Over three-quarters of cases are caused by streptococci or staphylococciStrep. milleri and Strep. bovis endocarditis is associated with large-bowel neoplasms.
Staph. aureus has now overtaken streptococci as the most common cause of acute endocarditis
Post-operative endocarditis .The most common organism is a coagulase-negative staphylococcus (Staph. epidermidis)
Q fever endocarditis due to Coxiella burnetii, : contact with farm animals. The aortic valve is usually affected and there may also be hepatitis, pneumonia and purpura. Life-long antibiotic therapy may be required.
HACEK are slow-growing, fastidious organisms that are only revealed after prolonged culture and may be resistant to penicillin.
Brucella
Yeasts and fungi (Candida, Aspergillus)
Microbiology of infective endocarditis
Incidence
5 to 15 cases per 100 000 per annum50% of patients are over 60 years
rheumatic heart disease in 24%congenital heart disease in 19%
other cardiac abnormalities (calcified aortic valve, floppy mitral valve) in 25%
32% were not thought to have a pre-existing cardiac abnormality
Clinical features
Subacute endocarditis
Acute endocarditisPost-operative endocarditis
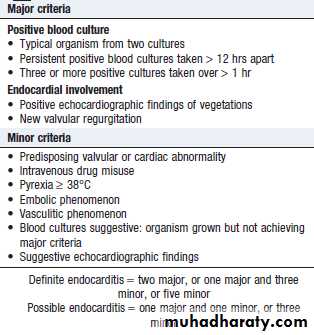
modified Duke criteria
Investigations
Blood cultureEchocardiography
ESR , CRP , CBC
ECG
CXRManagement
The case fatality of bacterial endocarditis is approximately 20 %A multidisciplinary approach increases the chance of better outcome
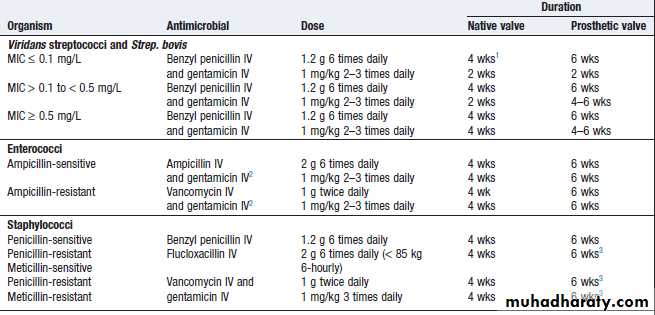
Empirical treatment depends on the mode of presentation, the suspected organism, and whether the patient has a prosthetic valve or penicillin allergyIf the presentation is acute, flucloxacillin and gentamicin are recommended, while for a subacute or indolent presentation, benzyl penicillin and gentamicin are preferred
In those with penicillin allergy, a prosthetic valve or suspected meticillin-resistant Staph. aureus (MRSA) infection, triple therapy with vancomycin, gentamicin and oral rifampicin should be considered
A 2-week treatment regimen may be sufficient for fully sensitive strains of Strep. viridans and Strep. bovis, provided specific conditions are met
Conditions for the short-course treatmentof Strep. viridans/bovis endocarditis
• Native valve infection• MIC ≤ 0.1 mg/L
• No adverse prognostic factors (e.g. heart failure, aortic regurgitation, conduction defect)
• No evidence of thromboembolic disease
• No vegetations > 5 mm diameter
• Clinical response within 7 days
Antimicrobial treatment of common causative organisms in infective endocarditis
Indications for cardiac surgery ininfective endocarditis
• Heart failure due to valve damage• Failure of antibiotic therapy (persistent/uncontrolled infection)
• Large vegetations on left-sided heart valves with evidence or‘high risk’ of systemic emboli
• Abscess formation
N.B. Patients with prosthetic valve endocarditis or fungal endocarditis often require cardiac surgery.
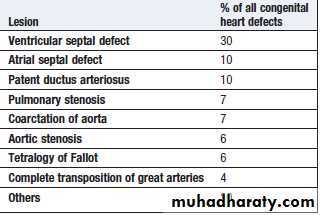
CONGENITAL HEART DISEASE
Aetiology and incidence
0.8% of live births
Maternal infection or exposure to drugs or toxins may cause congenital heart disease.
Rubella , alcohol , SLEGenetic or chromosomal abnormalities, such as Down’s syndrome , Marfan syndrom and Digeorge syndrom
Clinical features
Clinical signs vary with the anatomical lesionSymptoms may be absent, or the child may be breathless or fail to attain normal growth and development
Some defects are not compatible with extrauterine life
Features of other congenital conditions, such as Marfan’s syndrome or Down’s syndrome, may also be apparentEarly diagnosis is important because many types of congenital heart disease are amenable to surgery
Central cyanosis and digital clubbing
Growth retardation and learning difficulties
SyncopePulmonary hypertension and Eisenmenger’s syndrome
Pregnancy• Obstructive lesions (e.g. severe aortic stenosis): poorly tolerated and associated with significant maternal morbidity and mortality.
Cyanotic conditions (e.g. Eisenmenger’s syndrome): especially poorly tolerated and pregnancy should be avoided.
Surgically corrected disease: patients often tolerate pregnancy well.
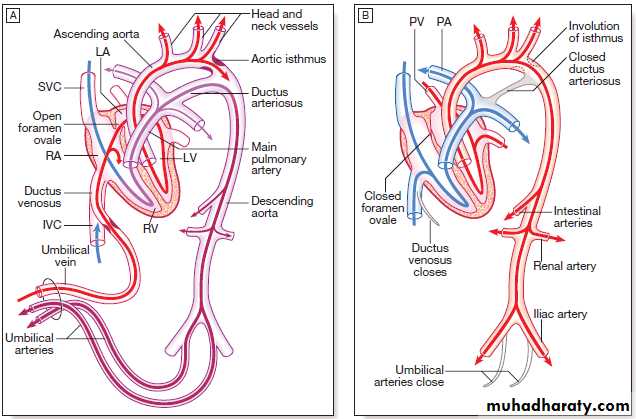
• Children of patients with congenital heart disease: 2–5% will be born with cardiac abnormalities, especially if the mother is affected.Persistent ductus arteriosus
Aetiology
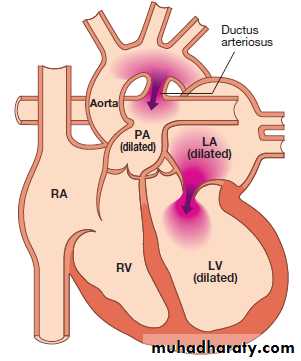
Normally, the ductus closes soon after birth but sometimes fails to do so
Persistence of the ductus is associated with other abnormalities and is more common in females.there will be a continuous arteriovenous shunt
50% of the left ventricular output is recirculated through the lungsClinical features
small shunts there may be no symptoms for yearswhen the ductus is large, growth and development may be retarded
cardiac failure may eventually ensue, dyspnoea being the first symptomcontinuous ‘machinery’ murmur is heard
Persistent ductus with reversed shuntingManagement
A patent ductus is closed at cardiac catheterisation with an implantable occlusive device
Pharmacological treatment in the neonatal period (prostaglandin synthetase inhibitor (indometacin or ibuprofen)Coarctation of the aorta
Aetiologyoccurs in the region where the ductus arteriosus joins the aorta, i.e. at the isthmus just below the origin of the left subclavian artery
twice as common in males and occurs in 1 in 4000 children
associated with other abnormalities, most frequently bicuspid aortic valve and ‘berry’ aneurysms of the cerebral circulationAcquired coarctation of the aorta is rare but may follow trauma or occur as a complication of a progressive arteritis (Takayasu’s disease)
Clinical features and investigations
coarctation is an important cause of cardiac failure in the newbornsymptoms are often absent when it is detected in older children or adults
Headaches , weakness or cramps in the legs , BP is raised in the upper body
Radiofemoral delay , systolic murmur may be be heard posteriorly or in the aortic area with ejection click due to bicuspid AV
CXR …… 3 sign and rib notching
ECG ….LVH
Echo. …..Confirm the diagnosis
MRI is the best imaging modality
Management
In untreated cases, death may occur from left ventricular failure, dissection of the aorta or cerebral haemorrhage.Surgical correction is advisable in most cases
Patients repaired in late childhood or adult life often remain hypertensive or develop recurrent hypertension later onRecurrence of stenosis may occur as the child grows and this may be managed by balloon dilatation and sometimes stenting
Coexistent bicuspid aortic valve, which occurs in over 50% of cases, may lead to progressive aortic stenosis or regurgitation, and also requires long-term follow-up.
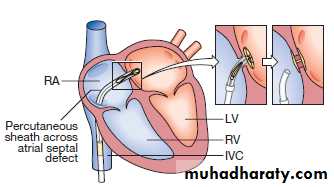
Atrial septal defect
one of the most common congenital heart defectstwice as frequently in females
Most are ‘ostium secundum’ defects
Ostium primum’ defects result from a defect in the atrioventricular septum and are associated with a ‘cleft mitral valve’ (split anterior leaflet).
Pulmonary hypertension and shunt reversal sometimes complicate atrial septal defect, but are less common and tend to occur later in life
Clinical features and investigations
SymptomsAsymptomatic
Dyspnea
Chest infection
HF
Arrythmias , AF
Signs
Wide fixed splitting S2Systolic flow murmur
Diastolic flow murmur
Investigations
ECG :- RBBB , RAD and in case of primum defect LAD
CXR : cardiomegaly ; pul plethora , prominent PA
Echo :- shows the defect , RV and PA dilatationTEE
TEEManagement
Atrial septal defects in which pulmonary flow is increased 50% above systemic flow (i.e. flow ratio of 1.5 : 1) are often large enough to be clinically recognisable and should be closedCath or surgery
Severe pulmonary hypertension and shunt reversal are both contraindications to closureVentricular septal defect
AetiologyCongenital and acquired
Embryologically, the interventricular septum has a membranous and a muscular portion
Most congenital defects are ‘perimembranousthe most common congenital cardiac defect, occurring once in 500 live births.
Acquired ventricular septal defect may result from rupture as a complication of acute MI or, rarely, from trauma.Clinical features
pansystolic murmur, usually heard best at the left sternal edge but radiating all over the precordiummaladie de Roger :- small defect producing loud murmur in the absence of other haemodynamic disturbance
Congenital ventricular septal defect may present as cardiac failure in infants, as a murmur with only minor haemodynamic disturbance in older children or adults, or, rarely, as Eisenmenger’s syndrome
If cardiac failure complicates a large defect, it only becomes apparent in the first 4–6 weeks of life
The chest X-ray shows pulmonary plethora and the ECG shows bilateral ventricular hypertrophy.
Echo .
Management and prognosis
Small ventricular septal defects require no specific treatmentHF : digoxin and diuretics
Persisting failure is an indication for closure of the defect by cath. or surgeryExcept in Eisenmenger’s syndrome, long-term prognosis is very good in congenital ventricular septal defect
Tetralogy of Fallot
Aetiology
The embryological cause is abnormal development of the bulbar septum that separates the ascending aorta from the pulmonary artery
The defect occurs in about 1 in 2000 births and is the most common cause of cyanosis in infancy after the first year of life.
Clinical features
Children are usually cyanosed but this may not be the case in the neonateThe subvalvular component of the RV outflow obstruction is dynamic and may increase suddenly under adrenergic stimulation
Fallot’s spells
In older children, Fallot’s spells are uncommon but cyanosis becomes increasingly apparent, with stunting of growth, digital clubbing and polycythaemia
Fallot’s sign : Some children characteristically obtain relief by squatting after exertion
On examination, cyanosis with a loud ejection systolic murmur in the pulmonary area
cyanosis may be absent in the newborn or in patients with only mild right ventricular outflow obstruction (‘acyanotic tetralogy of Fallot’)
Investigations and management
ECG … RVHCXR … boot shaped heart
Echo … Dx
The definitive management is total surgical correction
If the pulmonary arteries are too hypoplastic, then palliation in the form of a Blalock–Taussig shuntThe prognosis after total correction is good
ICD is sometimes recommended in adulthood.