
Lung diseases due to organic
dusts
Assistant prof. Dr.Ahmed Hussein Jasim F.I.B.M.S (resp), F.I.B.M.S
(med)

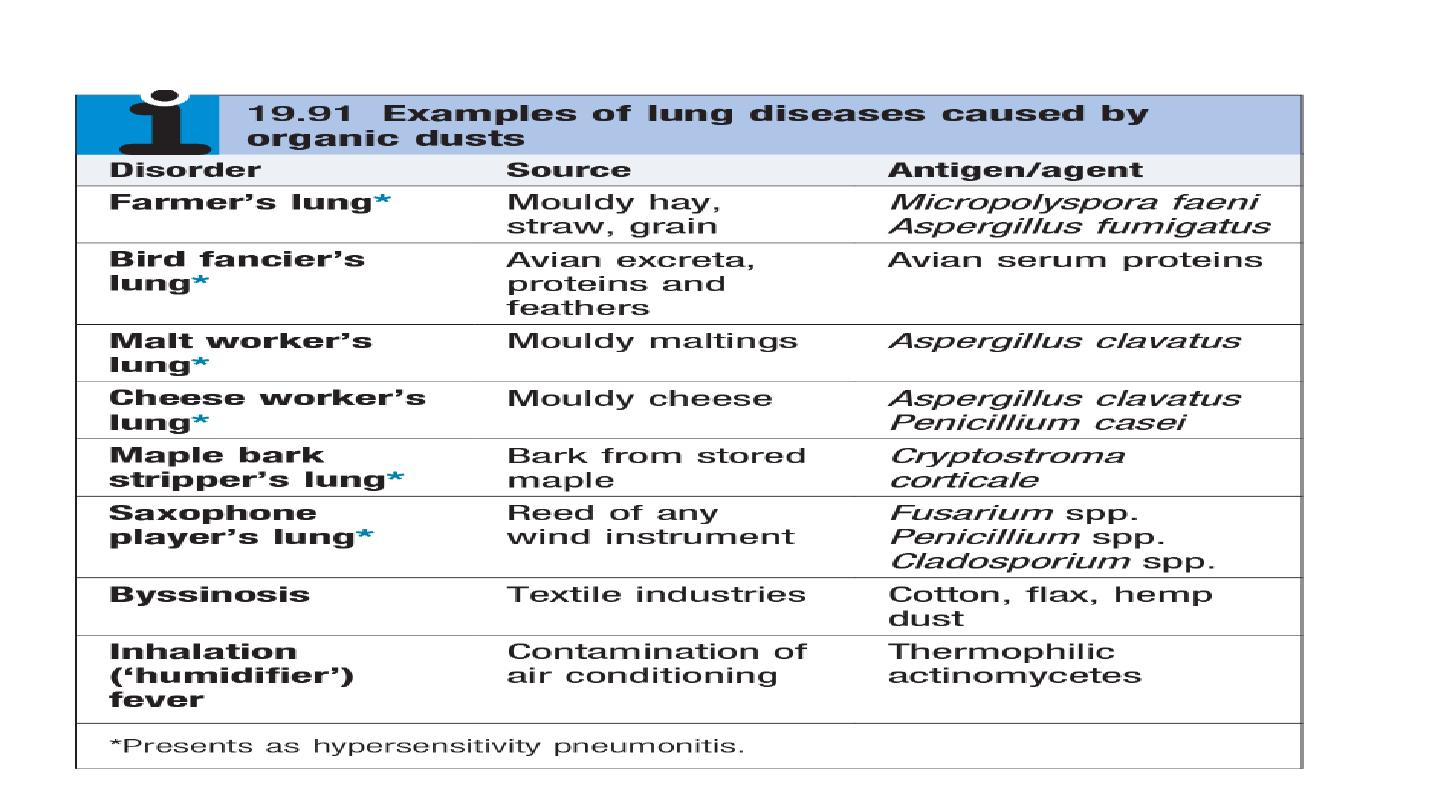
A wide range of organic agents may cause respiratory disorders . Disease results from
a local immune response to animal proteins, or fungal antigens in mouldy vegetable
matter. Hypersensitivity pneumonitis is the most common of these conditions.
Hypersensitivity pneumonitis
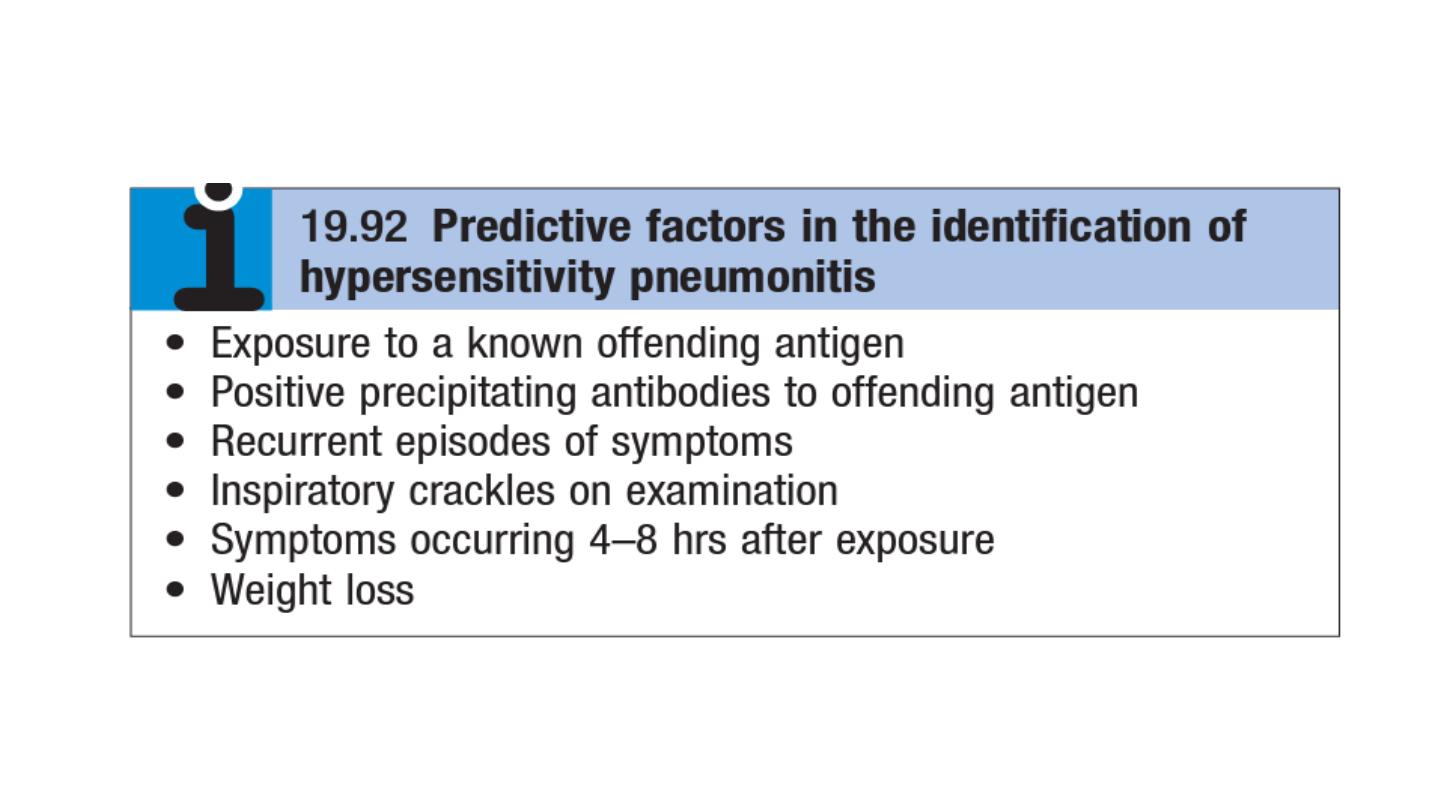
Hypersensitivity pneumonitis (HP; also called extrinsic allergic alveolitis) results from
the inhalation of a wide variety of organic antigens,
which give rise to a diffuse
immune complex reaction in the alveoli and bronchioles.
Common causes include farmer’s lung and bird fancier’s lung.
The pathology of hypersensitivity pneumonitis is consistent with both type III and type
IV immunological mechanisms. Precipitating IgG antibodies may be detected in the
serum and a type III Arthus reaction is believed to occur in the lung, where the
precipitation of immune complexes results in activation of complement and an
inflammatory response in the alveolar walls characterised by the influx of mononuclear
cells and foamy histiocytes. The presence of poorly formed noncaseating granulomas in
the alveolar walls suggests that type IV responses are also important.
there is a lower incidence of hypersensitivity pneumonitis in smokers than non-smokers.
Clinical features
The presentation of HP varies from an acute form to a more indolent pattern,
depending on the antigen load.

Investigations
the chest X-ray typically shows ill-defined patchy airspace shadowing which, given the
systemic features, may be confused with pneumonia.
HRCT is more likely to show bilateral ground glass shadowing and areas of
consolidation superimposed on small centrilobar nodular opacities with an upper and
middle lobe predominance chronic disease, features of fibrosis, such as volume loss,
linear opacities and architectural distortion.
pulmonary function tests show a restrictive ventilatory defect with reduced lung
volumes and impaired gas transfer
BAL fluid usually shows an increase in the number of CD8+ T lymphocytes, and
transbronchial biopsy can occasionally provide sufficient tissue for a confident diagnosis;
Management
cease exposure to the inciting agent. Dust masks with appropriate filters may minimise
exposure and be combined with methods of reducing levels of antigen (e.g. drying hay
before storage).
In acute cases, prednisolone should be given for 3–4 weeks, starting with an oral dose
of 40 mg per day.
OCCUPATIONAL AND ENVIRONMENTAL LUNG DISEASE
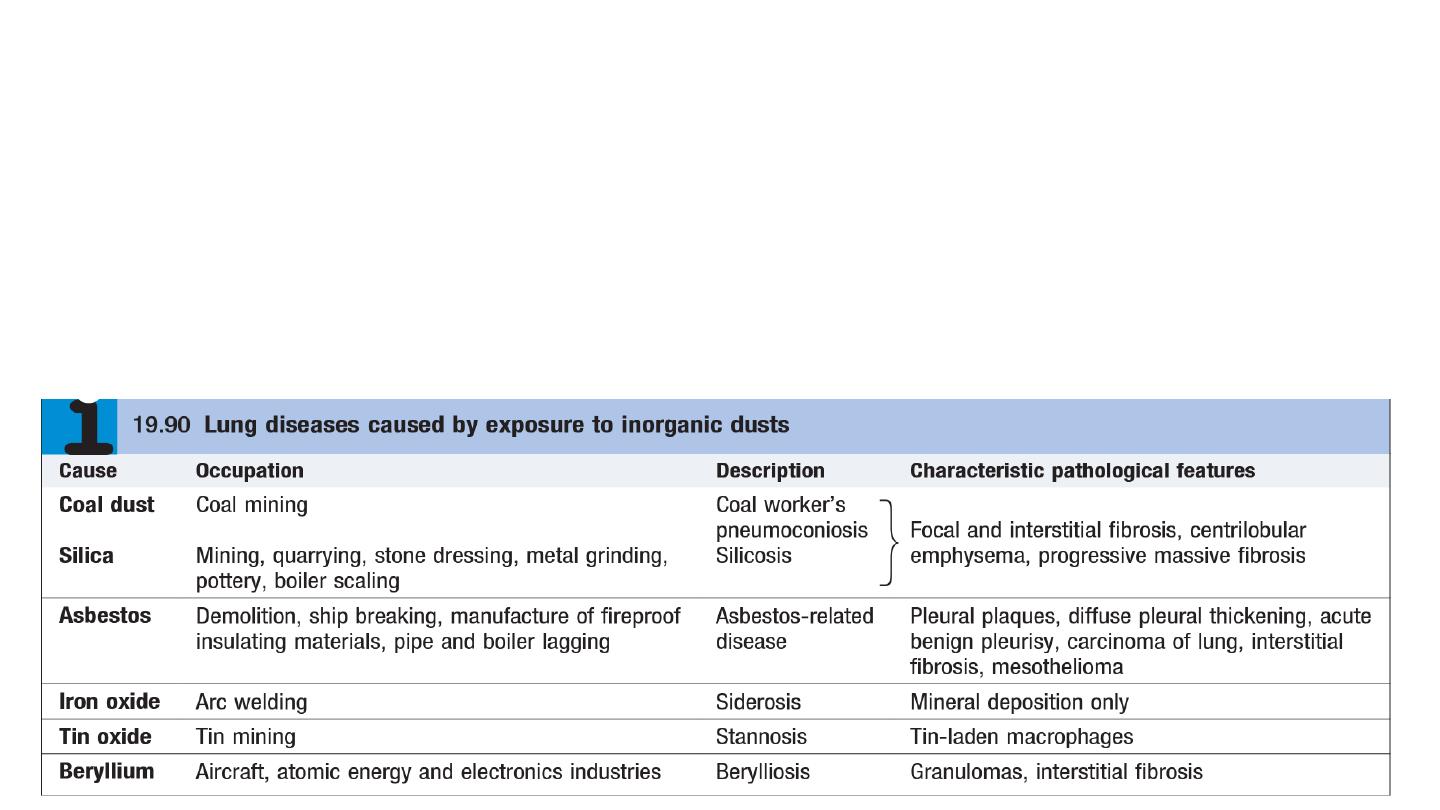
Pneumoconiosis
Pneumoconiosis can be defined as a permanent alteration of lung structure due to the
inhalation of mineral dust and the tissue reactions of the lung to its presence, excluding
bronchitis and emphysema . The most important pneumoconioses include coal worker’s
pneumoconiosis, silicosis and asbestosis.

Asbestos-related lung and pleural diseases
Asbestos is a naturally occurring silicate. Its fibres may be classified as either chrysotile
(white asbestos), which accounts for 90% of the world’s production, or serpentine
(crocidolite or blue asbestos, and amosite or brown asbestos).
Exposure to asbestos may be followed by the development of both pleural and
pulmonary disease, after a lengthy latent period.
1. Pleural plaques
Pleural plaques are the most common manifestation of past asbestos exposure, and are
discrete circumscribed areas of hyaline fibrosis that may occur on the parietal pleura of
the chest wall, diaphragm, pericardium or mediastinum.
2. Acute benign asbestos pleurisy
Benign asbestos pleurisy is estimated to occur in around one-fifth of asbestos workers
but many episodes are subclinical and pass unreported. Repeated episodes may be
followed by the development of diffuse (visceral) pleural thickening.
3. Diffuse pleural thickening
Diffuse pleural thickening (DPT) affects the visceral pleura and, if sufficiently extensive,
may cause restrictive lung function impairment, exertional breathlessness and,
occasionally, persistent chest pain.

4. Asbestosis
Asbestosis is a diffuse parenchymal lung disease. Its development generally requires
substantial exposure over several years, and is rare with low-level or bystander exposure. In
common with other fibrosing lung diseases, asbestosis usually presents with exertional
breathlessness and fine, late inspiratory crackles over the lower zones. Finger clubbing
may be present.
5. Mesothelioma
Mesothelioma is a malignant tumour affecting the pleura or, less commonly, the
peritoneum. Its occurrence almost invariably suggests past asbestos exposure, which may
be low-level. There is typically a long latent interval between first exposure and the
onset of clinical manifestations Pleural mesothelioma typically presents with increasing
breathlessness resulting from pleural effusion, or unremitting chest pain when there is
involvement of the chest wall.
Mesothelioma is almost invariably fatal.

Silicosis
Silicosis results from the inhalation of crystalline silica, usually in the form of quartz, by
workers cutting, grinding and polishing stone. Classic silicosis is most common and
usually manifests after 10–20 years of continuous silica exposure, during which time
the patient remains asymptomatic.
Intense exposure to very fine crystalline silica dust can cause a more acute disease –
silicoproteinosis, similar to alveolar proteinosis
Radiological features are similar to those of coal worker’s pneumoconiosis, with
multiple wellcircumscribed 3–5-mm nodular opacities, predominantly in the mid- and
upper zones. As the disease progresses, PMF may develop Enlargement of the hilar
glands with an ‘egg-shell’ pattern of calcification is said to be characteristic but is
uncommon and non-specific.
Individuals with silicosis are at increased risk of tuberculosis (silicotuberculosis), lung
cancer and COPD. Associations with renal and connective tissue disease have also been
described.
