
CARCINOMA OF BREAST
ALI K. SHAAELI
MB,CH FACS, FRCSI
Nov. 2018

CARCINOMA OF BREAST
• 1 in every 12 women will develop the disease
during their lifetime.
• The incidence is expected to continue rising
as the population ages

Etiological factors
1- Geographical
• Carcinoma of the breast occurs commonly in the Western world,
accounting for 3–5% of all deaths in women. In developing countries it
accounts for 1–3% of deaths.
2- Age
• Carcinoma of the breast is extremely rare below the age of 20 years but,
thereafter, the incidence steadily rises so that by the age of 90 years
nearly 20% of women are affected.
3- Gender
• Less than 0.5% of patients with breast cancer are male.
4- Genetic
• It occurs more commonly in women with a family history of breast cancer
than in the general population.
• Breast cancer related to a specific mutation accounts for about 5% of
breast cancers
Etiological factors
5- Diet
• Because breast cancer so commonly affects women in the ‘developed’ world,
dietary factors may play a part in its causation.
• A high intake of alcohol is associated with an increased risk .
6- Endocrine
• Breast cancer is more common in nulliparous women and breast feeding is
protective.
• Having a first child at an early age, late menarche and early menopause are
protective
• It is known that in postmenopausal women, breast cancer is more common
in the obese. This is thought to be because of an increased conversion of
steroid hormones to oestradiol in the body fat.
• oral contraceptive pill and HRT, have a role in the development of breast
cancer.
7- Previous radiation
• It is higher risk in women who have been treated with mantle radiotherapy
as part of the management of Hodgkin’s disease.
Pathology
• Breast cancer may arise from the epithelium of the duct
system any where from the nipple end of the major
lactiferous ducts to the terminal duct unit. The disease may
be 1- entirely
in situ
2-or invasive cancer.
• The degree of differentiation of the tumor is usually
described using three grades
: well differentiated,
moderately differentiated or poorly differentiated
• Previously, descriptive terms were used to classify breast
cancer (‘scirrhous’, meaning woody, or ‘medullary’,
meaning brain-like). More recently, histological descriptions
have been used. These have been shown to have clinical
correlations.

Current nomenclature
• Ductal carcinoma is the most common variant
• lobular carcinoma occurring in up to 15% . Invasive
lobular carcinoma is commonly multifocal and/or
bilateral
• Inflammatory carcinoma is a fortunately rare, highly
aggressive cancer that presents as a painful, swollen
breast, which is warm with cutaneous edema. This is
the result of blockage of the subdermal lymphatics
with carcinoma cells. Inflammatory cancer usually
involves at least one-third of the breast and may mimic
a breast abscess.

Current nomenclature
• Carcinoma
in situ
is pre-invasive cancer that has
not breached the epithelial basement membrane.
is becoming increasingly common because of the
advent of mammographic screening.
• Ductal Carcinoma
in situ
(DCIS) or
• Lobular carcinoma in Situ (LCIS), the latter often
being multifocal and bilateral. Both are markers
for the later development of invasive cancer.

The spread of breast cancer
1- Local spread
• The tumor increases in size and invades other
portions of the breast. It tends to involve the skin
and to penetrate the pectoral muscles and even
the chest wall if diagnosed late.
2- Lymphatic metastasis
• Lymphatic metastasis occurs primarily to the
axillary and the internal mammary lymph nodes.
• Tumors in the posterior one-third of the breast
are more likely to drain to the internal mammary
nodes.

The spread of breast cancer
• The involvement of lymph nodes represents a marker
for the metastatic potential.
• Involvement of supraclavicular nodes and of any
contralateral lymph nodes represents advanced
disease.
3- Spread by the bloodstream
•
It is by this route that skeletal metastases occur, In
order of frequency, the lumbar vertebrae, femur,
thoracic vertebrae, rib and skull are affected and these
deposits are generally osteolytic.
• Metastases may occur in the liver, lungs and brain and,
occasionally, the adrenal glands and ovaries;

Clinical presentation
• breast cancer is found most frequently in the upper
outer quadrant .
• Most breast cancers will present as a hard lump, which
may be associated with the nipple retraction.
• As the disease advances locally there may be skin
involvement with peau d’orange
• frank ulceration and fixation to the chest wall.
• About 5% of breast cancers in the UK will present with
either locally advanced disease or symptoms of
metastatic disease. This figure is much higher in the
developing world.
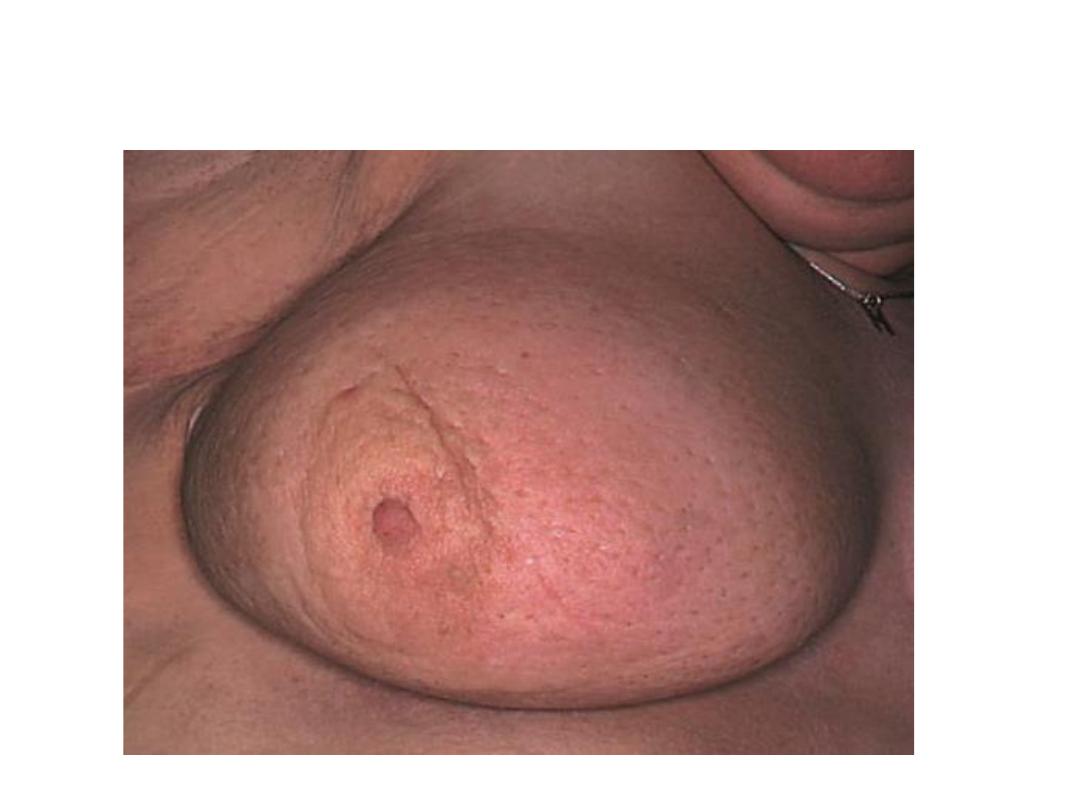
peau d’orange

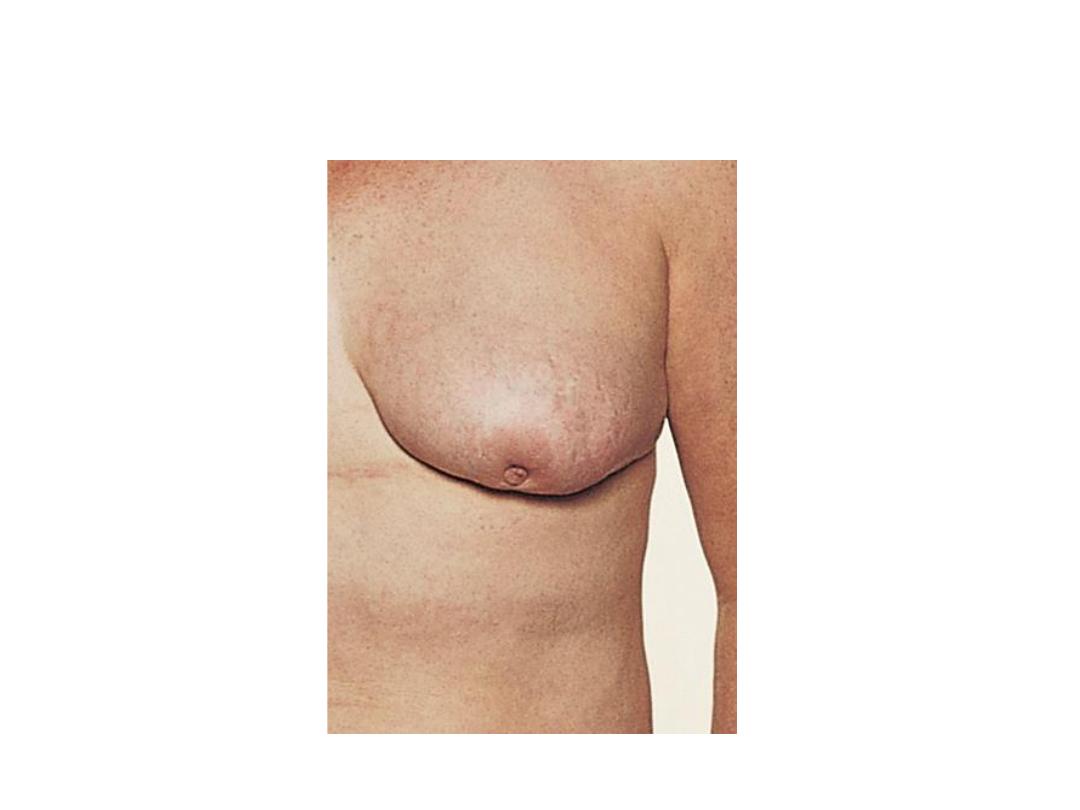
Malignant ulcer

Malignant ulcer
Nipple retraction

Staging
• Tis Carcinoma in situ
• T1 Tumor less than 20 mm in greatest dimension
• T2 Tumor >20 mm but ≤50mm in greatest dimension
• T3 Tumor >50 mm in greatest dimension
• T4 Tumor of any size with direct extension to the
chest wall and/or to the skin (ulceration or skin
nodules)
• N0 No regional lymph node metastases

Staging
• N1 Metastases to movable ipsilateral level I, II axillary
lymph node(s)
• N2 Metastases in ipsilateral level I, II axillary lymph nodes
that are clinically fixed or matted;
• N3 Metastasis in ipsilateral infra-clavicular (level III axillary)
lymph node(s) with or without level I, II axillary lymph node
involvement.
• M 0 No clinical or radiographic evidence of distant
metastases
• M1 Distant detectable metastases as determined by classic
clinical and radiographic means and/or histological
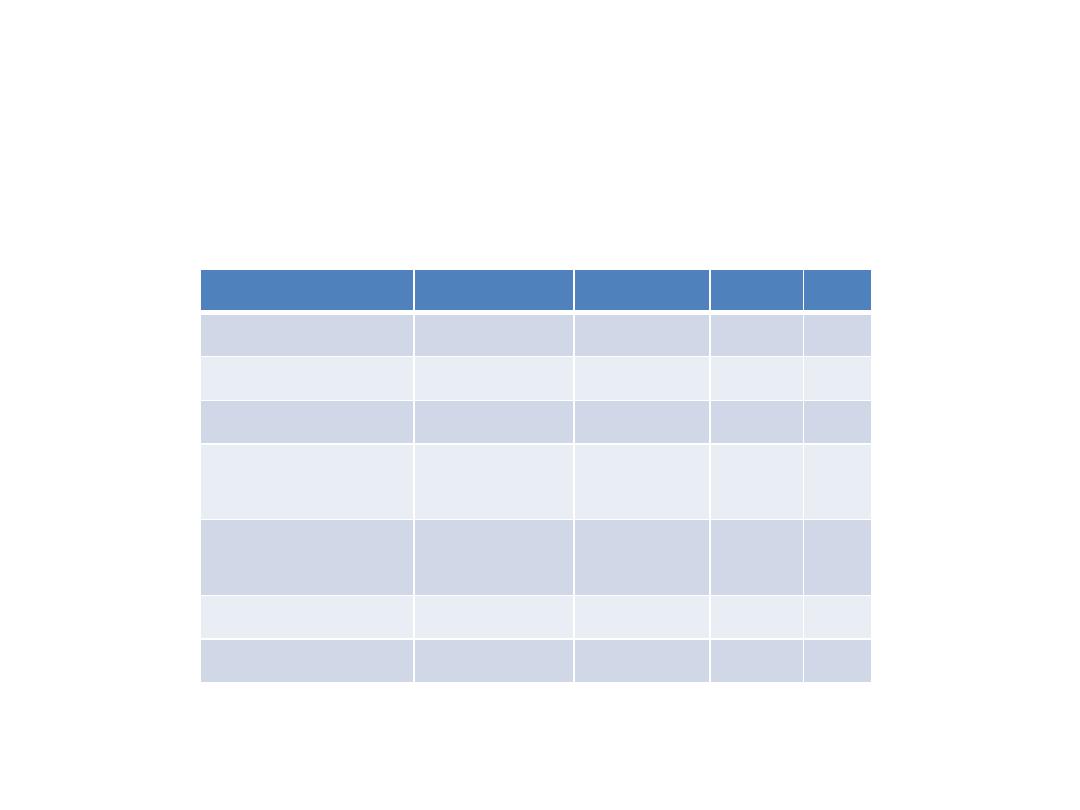
TNM stage grouping
early carcinoma are limited to breast and axilla which are
I,IIA&B and IIIA
Stage
T
N
M
STAGE I
Early
T1
N0
M0
STAGE IIA
early
T2
N0
M0
STAGE IIB
Early
T2
N1
M0
STAGE IIIA
Early
T3
N1,
N2
M0
STAGE IIIB
Late
T4
N1,
N2
MO
STAGE IIIC
Late
any T
N3
MO
STAGE IV
late
any T
any N
M1
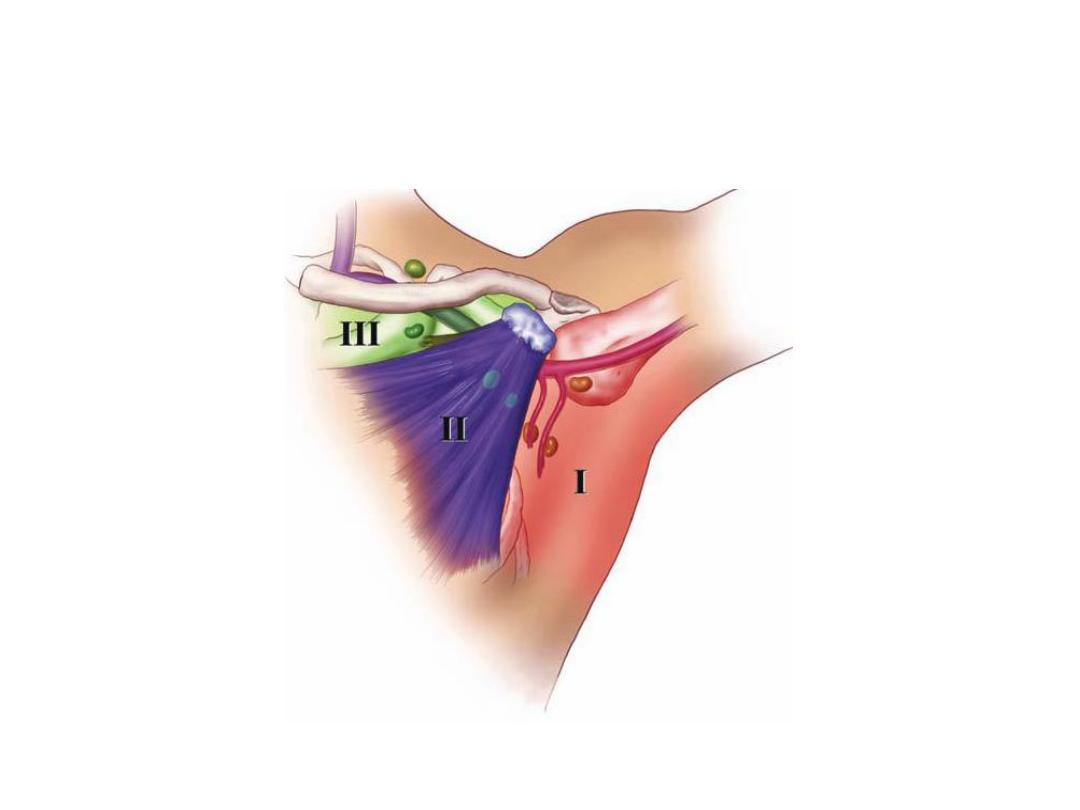
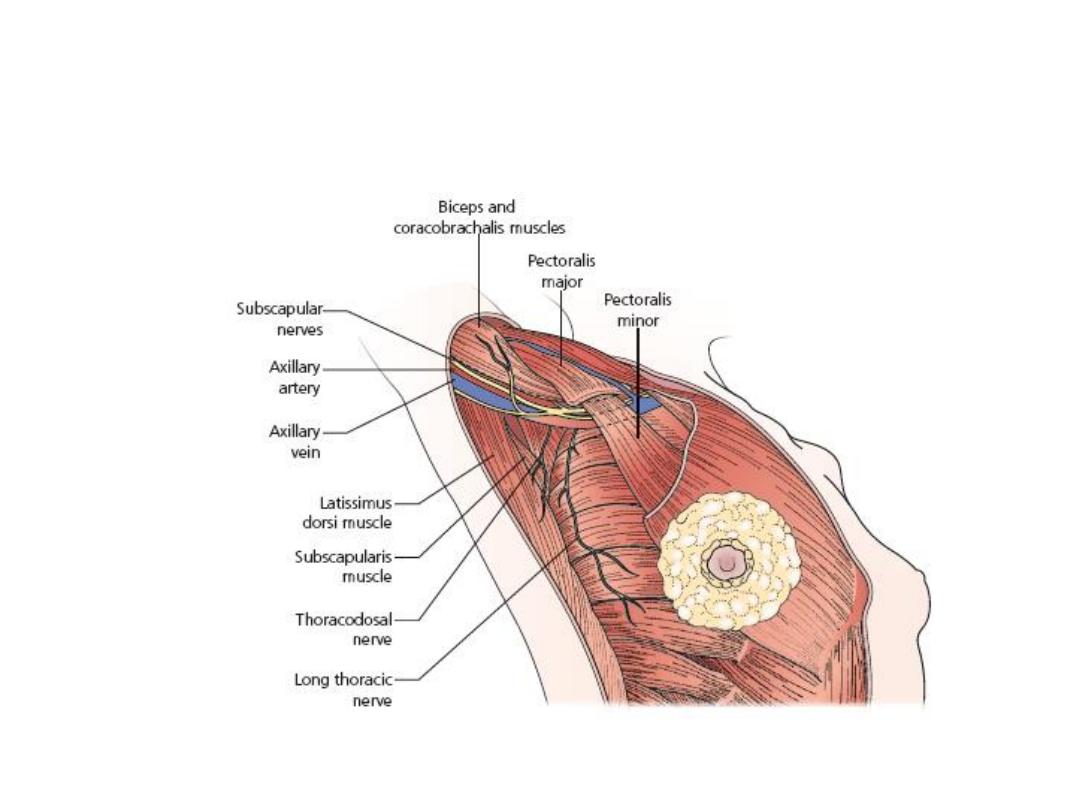
Axillary lymph nodes
Treatment of cancer of the breast
• The two basic principles of treatment are to reduce the
chance of local recurrence and the risk of metastatic
spread.
• Treatment of early breast cancer will usually involve
surgery with or without radiotherapy.
• Systemic therapy such as chemotherapy or hormone
therapy is added if there are adverse prognostic factors
such as lymph node involvement, indicating a high
likelihood of metastatic relapse.
• Locally advanced or metastatic disease is usually
treated by systemic therapy to palliate symptoms, with
surgery playing a much smaller role.

The multidisciplinary team approach
• good doctor–patient communication plays a
vital role in helping to alleviate patient
anxiety.
• Participation of the patient in treatment
decisions is of particular importance in breast
cancer when there may be uncertainty as to
the best therapeutic option.

The multidisciplinary team approach
• As part of the preoperative and postoperative
management of the patient it is often useful to
employ the skills of a trained breast counselor
and also to have available advice on breast
prostheses, psychological support and
physiotherapy.
• In many specialist centers the care of breast
cancer patients is undertaken as a joint venture
between the surgeon, medical oncologist,
radiotherapist and allied health professionals
such as the clinical nurse specialist.

Local treatment of early breast cancer
• Local control is achieved through surgery and/or
radiotherapy
• Surgery still has a central role to play in the management of
breast cancer but there has been a gradual shift towards
more conservative techniques
• It was initially hoped that avoiding mastectomy would help
to alleviate the considerable psychological morbidity
associated with breast cancer, but , about 30% of women
develop anxiety and depression following both radical and
conservative surgery. After mastectomy women tend to
worry about the effect of the operation on their
appearance and relationships, whereas after conservative
surgery they may remain fearful of a recurrence.
Local treatment of early breast cancer
Mastectomy is indicated for large tumors , central tumors
beneath or involving the nipple, multifocal disease, local
recurrence or patient preference.
• The modified radical (Patey) mastectomy is more
commonly performed, The breast and associated structures
are dissected
en bloc
and the excised mass is composed of:
1-the whole breast;
2- a large portion of skin, the center of which overlies the
tumor but which always includes the nipple; all of the fat,
fascia and lymph nodes of the axilla.
• Simple mastectomy; involves removal of only the breast
with no dissection of the axilla.
Patey mastectomy

Patey mastectomy

Patey mastecomy

Conservative breast cancer surgery
• This is aimed at removing the tumor plus a rim of at 1mm- 1 cm of
normal breast tissue. This is commonly referred to as a wide local
excision.. A quadrantectomy involves removing the entire segment
of the breast that contains the tumor. Both of these operations are
usually combined with axillary surgery, usually via a separate
incision in the axilla. There is a somewhat higher rate of local
recurrence following conservative surgery, even if combined with
radiotherapy, but the long-term outlook in terms of survival is
unchanged.
• Patients whose margins are involved should have a further local
excision (or a mastectomy) before going on to radiotherapy.
• Conservative Excision of a breast cancer without radiotherapy leads
to an unacceptable local recurrence rate

Sentinel node biopsy
• This technique has become the standard of care in the
management of the axilla in patients with clinically
node-negative disease. The sentinel node is localized
peroperatively by the injection of patent blue dye and
radioisotope labelled albumin in the breast.
• The recommended site of injection is in the subdermal
plexus around the nipple although some still inject on
the axillary side of the cancer. The marker passes to the
primary node draining the area and is detected visually
and with a hand-held gamma camera.

Radiotherapy
• Radiotherapy to the chest wall after mastectomy is
indicated in selected patients in whom the risks of local
recurrence are high.
• This includes patients with large tumors and those with
large numbers of positive nodes or extensive
lymphovascular invasion.
• There is some evidence that postoperative chest wall
radiotherapy improves survival in women with node-
positive breast cancer.
• It is conventional to combine conservative surgery with
radiotherapy to the remaining breast tissue.

Adjuvant systemic therapy
• It is now widely accepted that the outcomes of
treatment are predetermined by the extent of
micro-metastatic disease at the time of diagnosis.
• Variations in the radical extent of local therapy
might influence local relapse but probably do not
alter long-term mortality from the disease.
• However, systemic therapy targeted at these
putative micro-metastases might be expected to
delay relapse and prolong survival.

Adjuvant systemic therapy
• the appropriate use of adjuvant chemotherapy or hormone therapy
will improve relapse-free survival by about30% , which ultimately
translates into an absolute improvement in survival 10% at 15
years.
• lymph node-positive and many higher risk node-negative women
should be recommended adjuvant combined chemotherapy.
• Women with hormone receptor positive tumors will obtain a
worthwhile benefit from about five years of endocrine therapy,
either tamoxifen if premenopausal or the newer aromatase
inhibitors (anastrozole, letrozole) if postmenopausal.
• It is no longer appropriate to give hormone therapy to women with
oestrogen or progesterone receptor- negative disease.

Hormone therapy
• Tamoxifen has been the most widely used
‘hormonal’ treatment in breast cancer. it has now
been shown to reduce the annual rate of
recurrence by 25%, with a 17% reduction in the
annual rate of death.
• The beneficial effects of tamoxifen in reducing
the risk of tumors in the contralateral breast have
also been observed, as has its role as a
preventative agent.
• the optimal duration of treatment five years is
preferable.

Hormone therapy
• Other hormonal agents These include the LHRH
agonists, which induce a reversible ovarian
suppression.
• the oral aromatase inhibitors (AIs) for
postmenopausal women.
• There is an increase in bone density loss with
patients on an AI and a bone density scan is
advised prior to commencement with treatment
of underlying osteopenia or osteporosis.

Chemotherapy
• Chemotherapy using a first-generation regimen such as a
six monthly cycle of cyclophosphamide, methotrexate and
5-fluorouracil (CMF) will achieve a 25% reduction in the risk
of relapse over a 10- to 15-year period.
• modern regimens include an anthracycline (doxorubicin or
epirubicin) and the newer agents such as the taxanes.
• Chemotherapy was once confined to premenopausal
women with a poor prognosis but is being increasingly
offered to postmenopausal women with poor prognosis
disease as well.
• Chemotherapy may be considered in node negative
patients if other prognostic factors, such as tumor grade,
imply a high risk of recurrence.
Chemotherapy
• The effect of combining hormone and chemotherapy is additive
although hormone therapy is started after completion of
chemotherapy to reduce side effects..
• neoadjuvant is being used in many centers for large but operable
tumors that would traditionally require a mastectomy .The aim of
this treatment is to shrink the tumor to enable breast-conserving
surgery to be performed.
• Newer ‘biological’ agents will be used more frequently as molecular
targets are identified – the first of these, trastuzamab (Herceptin),
is active against tumors containing the growth factor receptor c-
erbB2. Other agents currently available include bevacizumab, a
vascular growth factor receptor inhibitor, and lapitinab, an oral
combined growth factor receptor inhibitor.

Thank you
