
BREAST
Ali K. Shaaeli
MB,ChB FACS FRCSI
OCT 2018

SURGICAL ANATOMY
• A thin layer of mammary tissue extends from the clavicle
above to the 7th or 8th ribs below and from the midline to
the edge of the latissimus dorsi posteriorly.
• AXILLARY TAIL; A well-developed axillary tail is sometimes
mistaken for a mass or enlarged lymph nodes or a lipoma.
• The lobule is the basic structural unit of the mammary
gland. they are 10- >100 lobules empty via ductules into a
lactiferous duct(15–20) .
• Each lactiferous duct is provided with a ampulla, a
reservoir for milk.
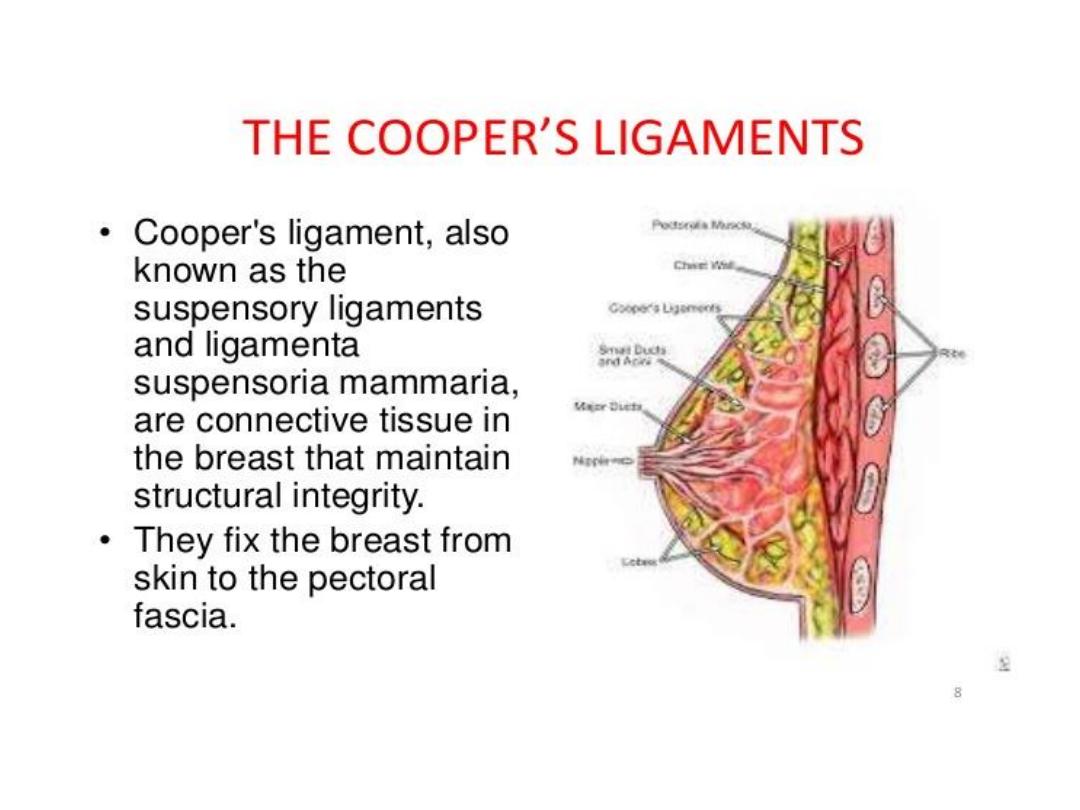
• The ligaments of Cooper are hollow conical projections of
fibrous tissue filled with breast tissue
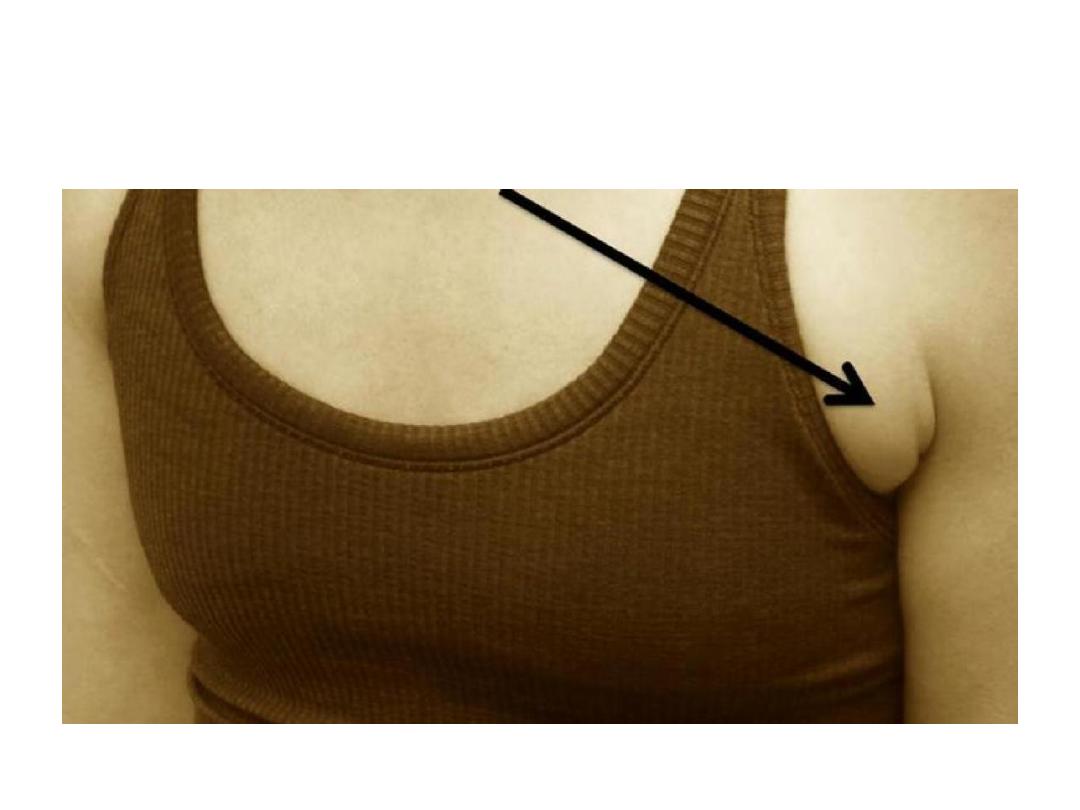
Axillary tail
INVESTIGATION OF BREAST
1-Mammography
• Soft tissue radiographs are taken by placing
the breast in direct contact with ultrasensitive
film and exposing it to low dose of radiation,
so, mammography is a safe investigation.
• The sensitivity of this investigation
increases with age as the breast becomes
less dense.

2-Ultrasound
• Ultrasound is useful in young women with
dense breasts in whom mammograms are
difficult to interpret
• It distinguishing cysts from solid lesions
• ultrasound guided of percutaneous biopsy
of any suspicious mass.

3-Magnetic resonance imaging
MRI
• It can be useful to distinguish scar from
recurrence in women who have had previous
breast conservation surgery for cancer.
• It is used in cases of lobular cancer is diagnosed
to assess for multifocality.
• It is the best imaging modality for the breasts of
women with implants.
• It has proven to be useful as a screening tool in
high-risk women (because of family history).

4-Needle biopsy/cytology
1- FNA Cytology; is obtained using a 21-23G
needle and 10-mL syringe. The aspirate is then
smeared on to a slide.
• (FNAC) is the least invasive technique of
obtaining a cell diagnosis and is rapid and very
accurate.
• However, false negatives do occur, mainly
through sampling error, and invasive cancer
cannot be distinguished from
in situ
disease.

4-Needle biopsy/cytology
2- Core Biopsy; Histology can be obtained under
local anesthesia using a spring-loaded core
needle biopsy device.
• specimen taken by core biopsy allows a
definitive diagnosis,
• Differentiates between duct carcinoma
in situ
and invasive disease
• allows the tumor to be stained for receptor
status.

Triple assessment
• In any patient who presents with a breast
lump or other symptoms suspicious of breast
carcinoma, the diagnosis should be made by
a combination of
1. clinical assessment,
2. radiological imaging and
3. a tissue sample (FNAC or biopsy)
• The positive predictive value (PPV) of this
combination should exceed 99.9 per cent.

THE NIPPLE
• Absence of the nipple is rare and is usually
associated with amazia (congenital absence
of the breast).
• Cracked nipple This may occur during lactation
and be the forerunner of acute infective mastitis.
If the nipple becomes cracked during lactation, it
should be rested for 24–48 hours and the breast
should be emptied with a breast pump. Feeding
should be resumed as soon as possible.

THE NIPPLE
• Eczema;
Eczema of the nipples is a rare
condition and is often bilateral;
• it is usually associated with eczema elsewhere on
the body.
• It is treated with 0.5% hydrocortisone.
• Paget’s disease of nipple;
must be
distinguished from eczema.
• It is caused by malignant cells in the subdermal
layer
• and is usually associated with a carcinoma within
the breast.

Pagets disease

Nipple retraction
simple nipple inversion; This may occur at puberty
or later in life. In about 25% of cases it is bilateral. It
may cause problems with breastfeeding and
infection can occur, especially during lactation.
Recent retraction;
A. A slit-like retraction of the nipple may be caused
by duct ectasia and chronic periductal mastitis.
B. circumferential retraction, with or without an
underlying lump, may indicate an underlying
carcinoma .

Discharges from the nipple
• Discharge can occur from one or more lactiferous
ducts. Management depends on the presence of
a lump
• A clear, serous discharge may be ‘physiological’ in
a parous woman or may be associated with a
duct papilloma or mammary dysplasia.
• A blood-stained discharge may be caused by duct
ectasia, a duct papilloma or carcinoma.
• A black or green discharge is usually the result of
duct ectasia and its complications

Treatment
• to exclude a carcinoma by occult blood test
and cytology.
• Simple reassurance may then be sufficient
but,
• if the discharge is proving intolerable, an
operation to remove the affected duct or
ducts can be performed (microdochectomy).

Bacterial mastitis
• Bacterial mastitis is the most common variety
of mastitis and is associated with lactation in
the majority of cases.
• Lactational mastitis is seen far less frequent.
• Most cases are caused by
S. aureus
• Ascending infection from a sore and cracked
nipple may initiate the mastitis,
• in many cases the lactiferous ducts will first
become blocked by epithelial debris leading to
stasis

Bacterial mastitis
Clinical features
• The affected breast, or a segment of it, presents
the classical signs of acute inflammation.
• Early on this is a generalized cellulitis but later an
abscess will form.
• The presence of pus can be confirmed with
needle aspiration and the pus sent for
bacteriological culture.
• In contrast to other abscess elsewhere,
fluctuation is a late sign.

Breast abscess

Treatment
• During the cellulitis stage the patient should
be treated with an appropriate antibiotic, for
example flucloxacillin or co-amoxiclav.
• Evacuation of the affected side.
• Support of the breast,
• local heat and
• analgesia will help to relieve pain.

Duct ectasia
Pathology
• This is a dilatation of the breast ducts, which is
often associated with periductal inflammation.
• the disease is much more common in smokers.
• In some cases, a chronic indurated mass forms
beneath the areola, which mimics a carcinoma.
• Fibrosis eventually develops, which may cause
slit-like nipple retraction.

Clinical features
• Nipple discharge (of any colour),
• a subareolar mass,
• abscess,
• mammary duct fistula
• and/or nipple retraction.
Treatment
• In the case of a mass or nipple retraction, a carcinoma
must be excluded by obtaining a mammogram and
negative cytology or histology.
• If any suspicion remains the mass should be excised.
• Antibiotic therapy may be tried, the most appropriate
agents being co-amoxiclav or flucloxacillin and
metronidazole.
• cessation of smoking increases the chance of a long-
term cure.
• surgery is often the only option; this consists of
excision of all of the major ducts (Hadfield’s
operation).

ANDI
Aberration of Normal Development
and involution
•
Etiology
The breast is a dynamic structure that
undergoes changes throughout a woman’s
reproductive life and, superimposed upon this,
cyclical changes throughout the menstrual cycle.

Pathology
The disease consists essentially of four features
that may vary in extent and degree in any one
breast:
1- Cyst formation. Cysts are almost inevitable
and very variable in size.
2- Fibrosis. Fat and elastic tissues disappear and
are replaced with dense white fibrous
trabeculae. The interstitial tissue is infiltrated
with chronic inflammatory cells.

Pathology
3 -Hyperplasia of epithelium in the lining of the
ducts and acini may occur, with or without
atypia.
4 -Papillomatosis. The epithelial hyperplasia
may be so extensive that it results in
papillomatous overgrowth within the ducts.

Clinical features
The symptoms of ANDI are many but often
include
• lumpiness (seldom discrete)
• and/or breast pain (mastalgia).

Breast cysts
Clinical features
• These occur most commonly in the last decade of
reproductive life as a result of a non-integrated
involution of stroma and epithelium. They are
often multiple, may be bilateral and can mimic
malignancy. They typically present suddenly and
cause great alarm
Diagnosis
• can be confirmed by aspiration
• and/or ultrasound.

Treatment
• A solitary cyst or small collection of cysts can be
aspirated.
If they resolve completely, and if the fluid is not
blood-stained, no further treatment is required.
• However, 30 per cent will recur, and require
reaspiration.
• If there is a residual lump or
• if the fluid is blood-stained, a core biopsy or local
excision for histological diagnosis is advisable,
which is also the case if the cyst reforms
repeatedly.

Breast cyst US

Galactocoele
• Galactocoele, which is rare, usually presents
as a solitary, subareolar cyst and always dates
from lactation.
• It contains milk and in long-standing cases its
walls tend to calcify.

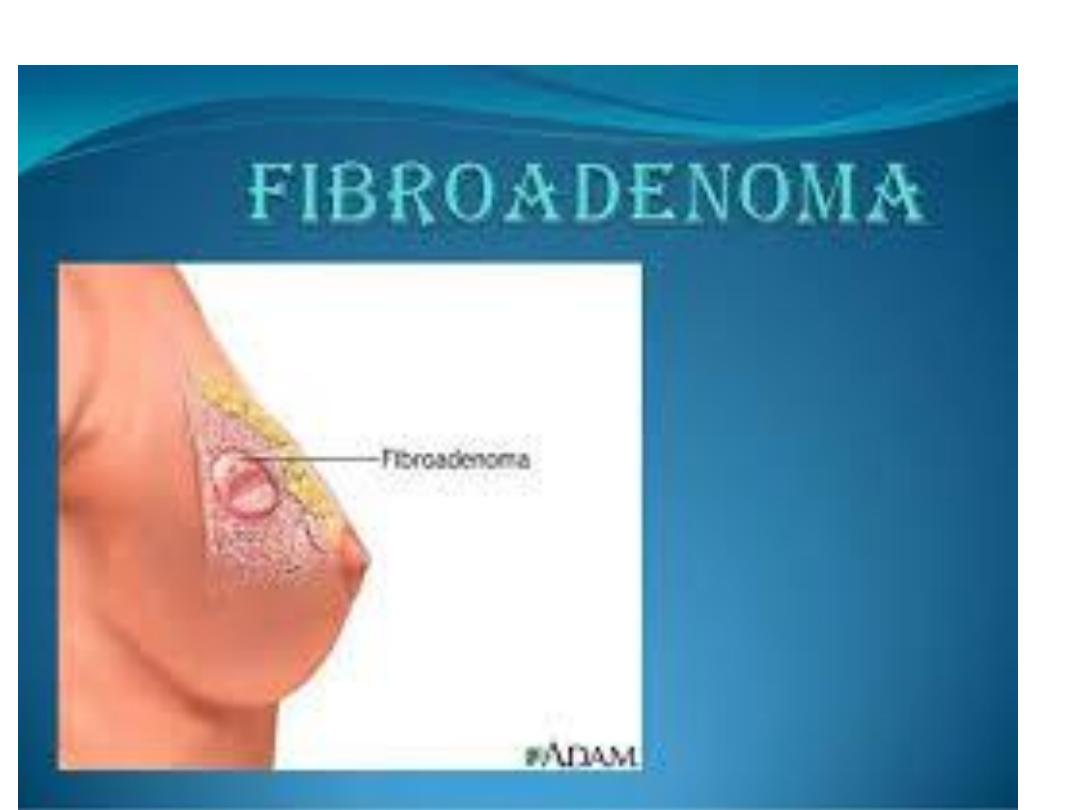
Fibroadenoma
• These usually arise in the fully developed
breast between the
• ages of 15 and 25 years, although occasionally
they occur in much older women.
• They arise from hyperplasia of a single lobule
and usually grow up to 2–3 cm in size.
• They are surrounded by a well-marked
capsule

Treatment
• A fibroadenoma does not require excision
unless
A- associated with suspicious cytology,
B- It becomes very large or
C- the patient expressly desires the lump to be
removed.
Giant fibroadenomas
• occasionally occur during puberty. They are
over 5 cm in diameter and are often rapidly
growing but,
• in other respects, are similar to smaller
fibroadenomas
• common in the Afro-Caribbean population
Treatment
• be enucleated through a submammary
incision.

Gaint fibroadenoma

Phyllodes tumour
• These benign tumours, previously sometimes known as
serocystic disease of Brodie or cystosarcoma phyllodes,
• usually occur in women over the age of 40 years but
can appear in younger women.
• They present as a large, sometimes massive, tumour
• with an unevenly bosselated surface.
• Occasionally, ulceration of overlying skin occurs
because of pressure necrosis.
• Despite their size they remain mobile on the chest
wall.
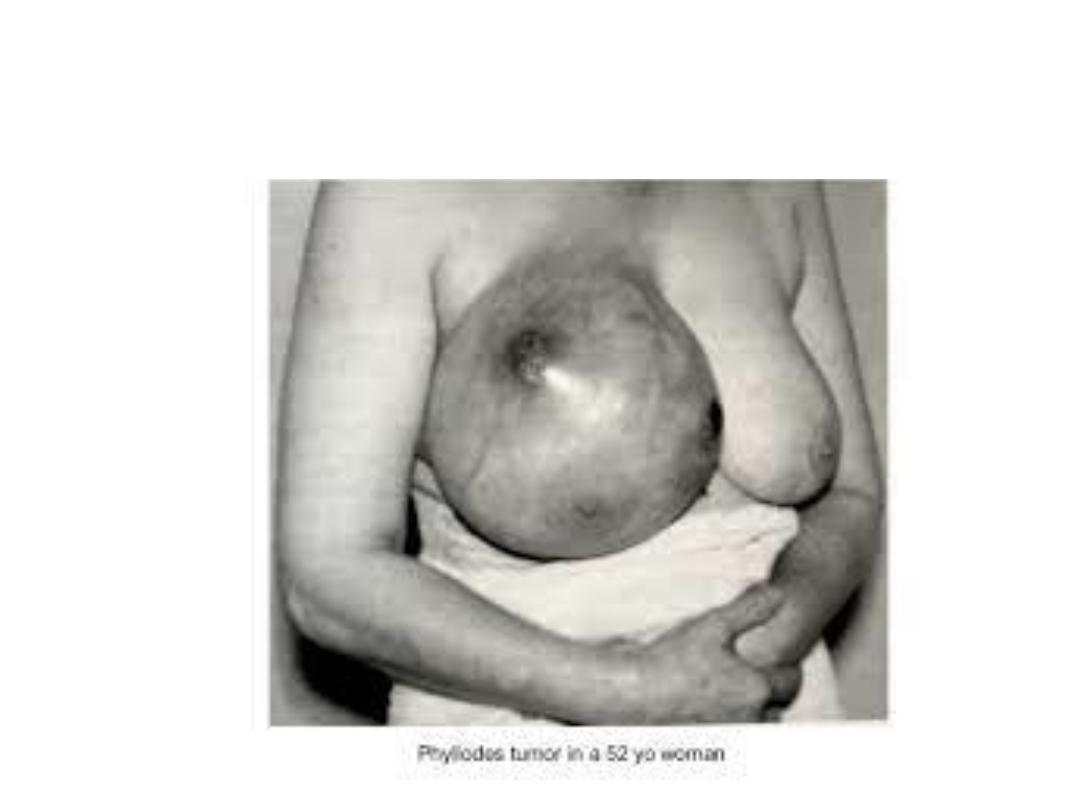
Phyllodes tumor

Pathology
• Histologically, there is a wide variation in their
appearance, with some of low malignant
potential resembling a fibroadenoma and others
having a higher mitotic index, which are
histologically worrying.
• They may recur locally
despite the name of cystosarcomaphyllodes, they
are rarely cystic and only very rarely develop
features of a sarcomatous tumour.
• These may metastasise via the bloodstream.

Treatment
Treatment is
1. Enucleation in young women
2. Wide local excision.
3. Mastectomy; for Massive tumors, recurrent
tumors and those of the malignant type.
