HEMODYNAMIC DISORDERS
Dr. Mustafa Salah MSc; FIBMS PathEMBOLISM
is a detached intravascular solid, liquid, or gaseous mass, carried by blood to a site distant from its point of originTypes of emboli - Thrombo-emboli - Fat and bone marrow - Gas (air, nitrogen) - Athero-emboli - Tumor fragments - Foreign body (bullet)
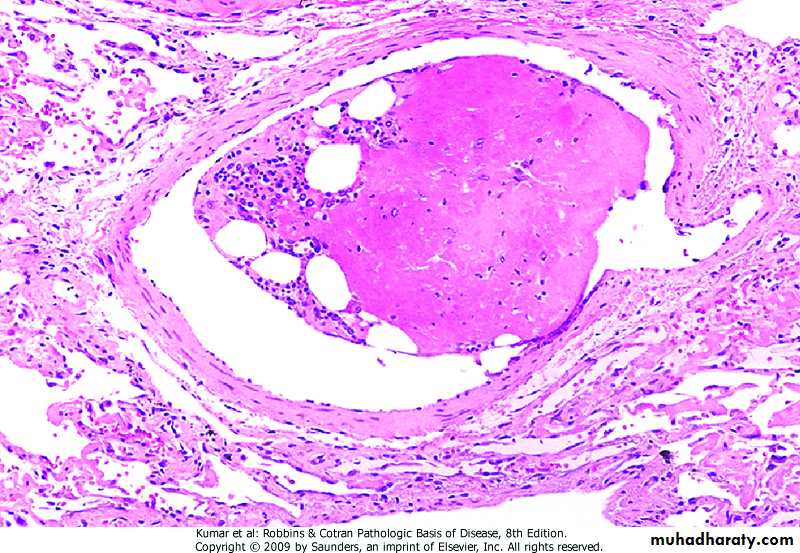
Pulmonary Thrombo-Embolism
• In most instances, deep leg vein thrombi are the source, depending on the size of the embolus, it;• - may occlude main pulmonary artery
• - may impact across the bifurcation (saddle embolus)
• - may pass into the smaller arterioles
• - may enter the systemic circulation (para-doxical embolism)
Clinical consequences of pulmonary embolism - most pulmonary emboli are silent - sudden death (acute corpulmonale) - obstruction of medium-size arteries> pulmonary hemorrhage - obstruction of small end-arterioles> infarction - multiple emboli over time> chronic corpulmonale
Systemic Thrombo-Embolism
Sources;- Intra-cardiac mural thrombi
- Aortic aneurysm- Thrombi on ulcerated atherosclerotic plaques
- Fragmentation of vegetation
- Paradoxical emboli
-15% are of unknown origin
Main sites involved in embolism:
- Lower extremities (75%) - Brain (10%) - Intestines - Kidneys - Spleen - Upper extremitiesFat Embolism
May result from- Fractures of long bones
- Soft tissue trauma and burns
Clinical features
- Pulmonary insufficiency
- Neurologic symptoms
- Anemia
- Thrombocytopenia
- Symptoms appear within 1 to 3 days
Fat Embolism
Pathogenesis of fat embolism - Mechanical obstruction - Biochemical injury (release of fatty acids from fat globules)
Visualization of fat globules in tissue sections require: - Frozen sections - Fat stains (Sudan black, Oil-red-O)
Gas Embolism
Air may enter the circulation during- Obstetric procedures
- Chest wall injury
More than100 cc is required to have a clinical effect
The bubbles produce physical obstruction to vessels>infarction
Decompression Sickness
Type of gas embolism in people who are exposed to sudden changes in atmospheric pressure (deep sea divers)If air is breathed at high pressure, high amount of gas (nitrogen), is dissolved in the blood and tissue
If the diver ascends (depressurizes) too rapidly, nitrogen expands in tissues and bubbles out of solution in the blood to form gas emboli
Decompression Sickness
Clinical features:- Muscle and joint pain - Respiratory distress - Infarctions in various tissues - Caisson disease (chronic decompression syndrome), presents as infarctions of the heads of the femurs, tibia, and humeri
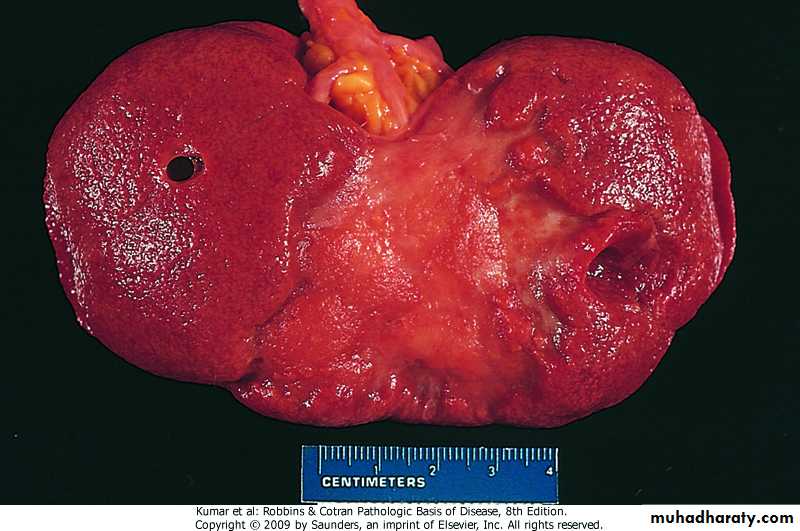
INFARCTION
Ischemic necrosis due to occlusion of either artery or vein
Causes:- Thrombosis or embolism (99%)
- Local vasospasm
- Expansion of atheroma
- Extrinsic compression of a vessel (tumor, twisting, edema, hernia)
- Traumatic rupture of vessel
INFARCTION
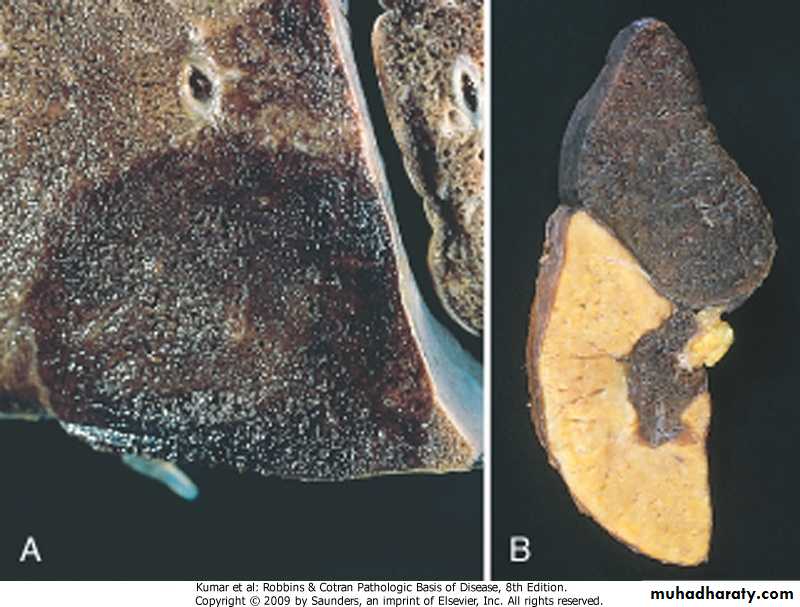
Morphology - Most infarcts are wedge-shaped, with occluded vessel at the apex and periphery of the organ forming the baseInfarcts are classified on the basis of:
INFARCTION
At the outset, all infarcts are poorly defined and slightly hemorrhagic, in few days, they become more firm and brownMost infarcts are replaced by scar tissue
In septic infarcts, abscess is produced
INFARCTION
Red infarcts occur in: - Venous occlusion (testis, ovary) - Loose tissue - Tissues with dual circulation - Previously congested tissues - Re-established blood flowWhite infarcts occur in: - Arterial occlusion - Solid organs with end-arteries
A. Hemorrhagic infarct lung B. white infract spleen
INFARCTIONClinical correlation of infarction -Consequences can range from no or minimal effect, all the way to death of a tissue or even the individual
- Factors that influence the outcome . Nature of the vascular supply . Rate of development of occlusion… slow … sudden . Vulnerability to hypoxia . Oxygen content of blood
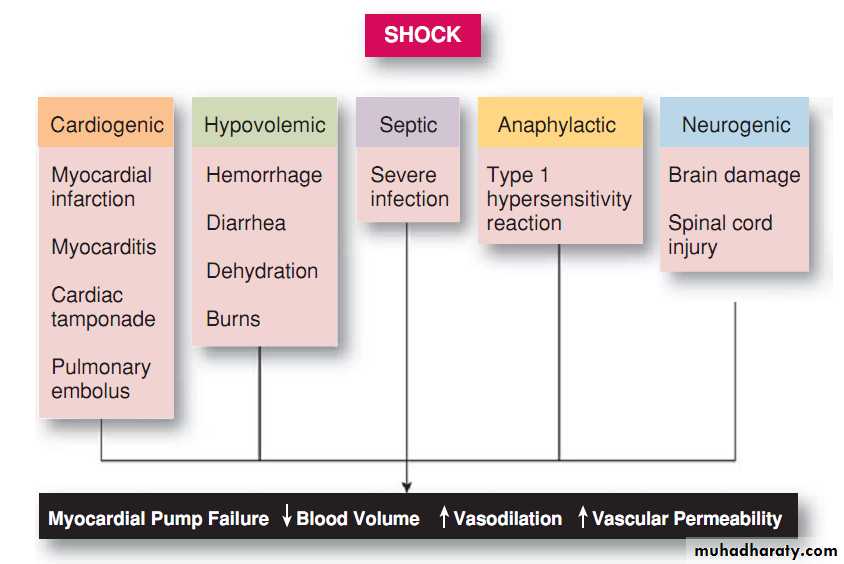
SHOCK
Shock is pathological state of life-threatening hypoperfusion of vital organs and cellular hypoxia, due diminished cardiac output or reduced effective circulating blood volumeie: resulting in: - Hypotension - Impaired tissue perfusion - Cellular hypoxia
Initially, cellular injury is reversible; if shock is sustained>cell death.Stages of shock
I. Stage of Compensation (initial nonprogressive stage )Decreased cardiac output cause reflex sympathetic stimulation, which increases the heart rate (tachycardia) and causes peripheral vasoconstriction that maintains blood pressure in vital organs (brain and myocardium).
Vasoconstriction in renal arterioles decreases the pressure and rate of glomerular filtration, with resulting decreased urine output (oliguria).
Stages of shock
II. Stage of Impaired Tissue Perfusion (progressive stage )Prolonged excessive vasoconstriction, impairs tissue perfusion and oxygenation.
Impaired tissue perfusion;
Promotes anaerobic glycolysis, leading to production of lactic acid and lactic acidosis.Produces cell necrosis, which is most apparent in the kidney; causing acute renal tubular necrosis and acute renal failure.
In the lung, hypoxia causes acute alveolar damage with intra-alveolar edema, hemorrhage, and formation of hyaline fibrin membranes (shock lung, or adult respiratory distress syndrome [ARDS]
In the liver, anoxic necrosis of the central region of hepatic lobules may occur.
Ischemic necrosis of the intestine is important because it is frequently associated with hemorrhage or release of bacterial endotoxins that further aggravate the shock state.
Stages of shock
III. Stage of Decompensation
As shock progresses, decompensation occurs.
Widespread vasodilation and stasis result and lead to a progressive fall in blood pressure to a critical level.
Cerebral hypoxia causes brain dysfunction (loss of consciousness).
Myocardial hypoxia leads to further diminution of cardiac output, and death may occur rapidly.
Morphological changes in shock
Changes are those of hypoxic injury,Most particularly involved organs, (brain, heart, lungs, kidneys, adrenals, gastro-intestinal tract)
Clinical features:
- In hypovolemic and cardiogenic shock, the patient presents with: . Hypotension . Weak rapid pulse . Cool, clammy, and cyanotic skin-In septic shock, the skin initially is warm and flushed
Prognosis
-Varies with the cause of shock and its duration;The best is in young with hypovolemic shock
The worst is in an old with cardiogenic shock and that with septic shockThank you