Pre-prosthetic Surgery
After the loss of natural teeth, bony changes in the jaws begin to take place immediately because the alveolar bone no longer respond to stresses placed in this area by the teeth and periodontal ligament. Bone begins to resorbs. The specific pattern of resorption is un- predictable in a given patient because great variation exists among individuals. This resorption tend to effect the mandible more severely than maxilla because of decreased surface area and less favorable distribution of occlusal of force.Objective of pre-prosthetic surgery
The objective of (P.S) is to create proper supporting structures forsubsequent placement of prosthetic appliances. The best iernture
supports has the following characteristic-
1. No evidence of intra oral or extra oral pathologic conditions.
2. Proper inter arch relationship.
3. Alveolar processes that are as large as possible and of proper configuration.
4. No bony or soft tissue protuberances or undercuts
5. Adequate palatal vault form .
6. Proper posterior tuberosity notching.
7. Adequate vestibular depth for prosthesis extension.
8. Adequate bony support and attached soft tissue covering.
Principles of patient evaluation and treatment planning:-
Pre-prosthetic surgical treatment must begin with a thorough history and physical examination of the patient a thorough assessment of overall general health is important especially when considering more advanced pre-prosthetic surgical techniques. Specific attention should also be given to possible systemic disease that may be responsible for the sever degree of bone resorption.Lab. tests such as serum levels of calcium, phosphate, parathyroid hormones and alkaline phosphates May be useful in pinpointing potential metabolic problems that may affect bone resorption.
Examination of the supporting bone should include visual inspection. palpation, radiographic examination, and in some cases evaluation of models. Evaluation of the denture-bearing area of the maxilla. No bony undercut or gross bony protuberances that block the path of denture insertion. Adequate post tuberosity notching must exit for posterior denture stability and peripheral seal.
The remaining mandibles ridge should be evaluated. Visually for overall ridge form and contour, gross ridge irregularities, tori and buccal exostosis. Proper radiographs are an important part of the initial diagnosis and treatment plan. O.P.G technique provide an excellent overview assessment of underlying bony structure and pathologic conditions. (Recontouring of alveolar ridges) The objectives of this procedures Is to provide the best possible tissue contour for prosthesis support.
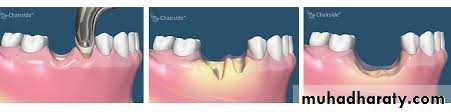
Alveoloplasty associated with removal of multple teeth:
The simplest form of alveoloplasty in combination with multiple exo is carried out after all of the teeth in the arch have been removed á technique is essentially that the bony areas requiring recontouring should be exposed using an envelope type of flap:Amucoperiosteal incision along the crest of the ridge with adequate extension anteroposterior to the area to be exposed then re- contouring can be accomplished with a Rongeur, a bone file, or a bone
bur in a hand piece. Alone or in combination. In any case normal saline irrigation should be used throughout the procedure to avoid overheating and bone necrosis. after that the flap should be re-approximated by digital pressure and the ridge palpated to ensure that all irregularities have been removed.
Intraseptal alveolplasty
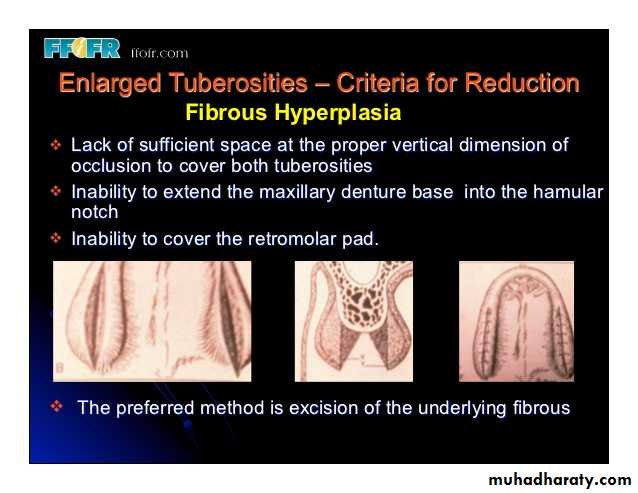
an alternative to the removal of alveolar ridge irregularities by simple alveoloplasty technique is the use of an intraseptal alveoloplasty or Dean's technique involving the removal of intraseptal bone and the repositioning of the labial cortical bone, rather than removal of excessive or irregular areas of the labial cortex.Maxillary tuberosity reduction:-
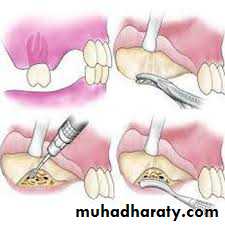
Horizontal or vertical excess ( or both) of the maxillary tuberosity area may be a result of excess bone.Recontouring of the maxillary tuberosity area may be necessary to remove bony ridge irregularities or to create an adequate inter-arch space, Surgery can be accomplished using local anesthesia.
Access to the tuberosity for the bone removal is accomplished by making a crest of incision that extends up to the posterior aspect o Tubrosity area, reflection of a full thickness mucoperiosted flap is completed in both the buccal and palatal direction, bone can be removed using aside-cutting Rongeur or rotary instrument with care taken to avoid perforation of the floor of the maxillary sinus after the appropriate amount of bone has been removed the area should be smoothed with a bone file and irrigated with saline. The mucoperiosted flaps can then be re-adapted
Buccal exostosis and excessive undercuts:-
Excessive bony protuberance and resulting undercut areas are more common in the maxilla than the mandible.Although extremely large areas of bony exostosis generally require removal. But small undercut area or bony buccal protuberance if removed results in a narrowed crest in the alveolaer ridge area and a less desirable area of support for the denture. As well as an area that may be resorbs more rapidly.
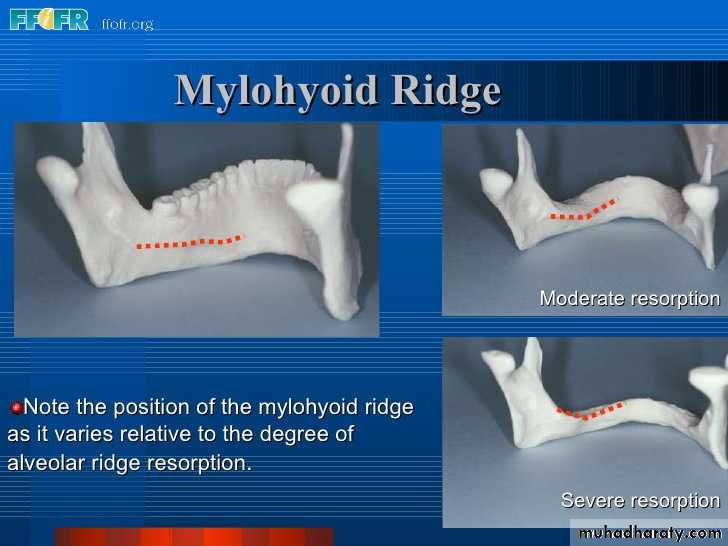
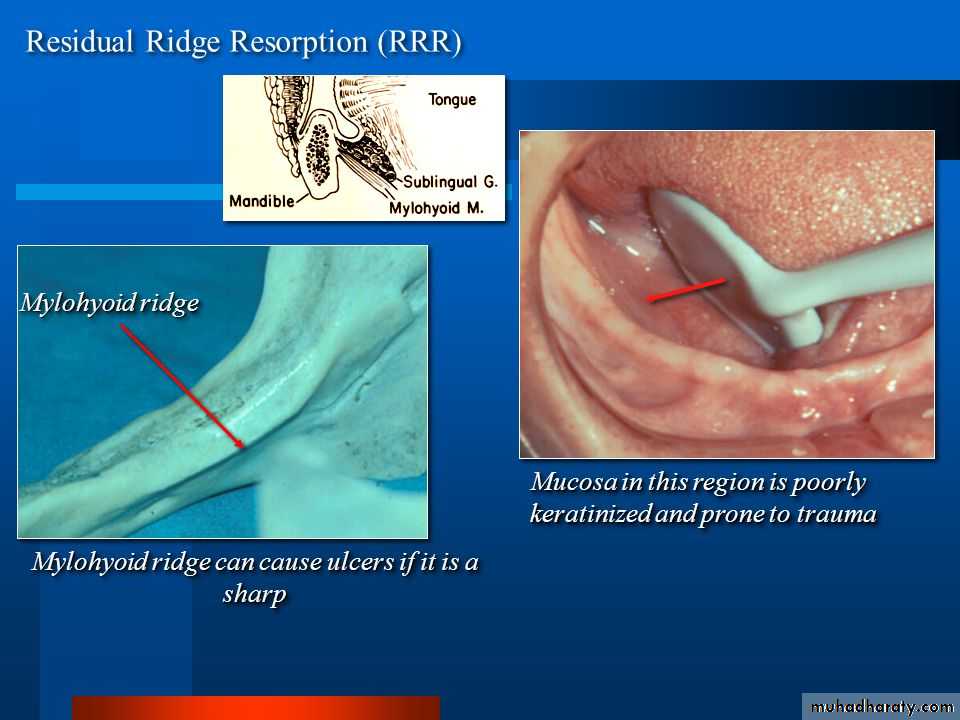
Mylohyoid ridge reduction:-
One of the more common area interfering with proper denture construction in the mandible is the mylohyoid ridge with it's easily damaged covering of mucosa, the muscular attachment to this area often is responsible for dislodging the denture. When this ridge is extremely sharp, denture pressure may produce significant pain in this area.Inferior alveolar, buccal and lingual nerve blocks are required a linear incision is made over the crest of the ridge in the posterior aspect of the mandible. Extension of the incision too far to the lingual aspect should be avoided because this may cause potential trauma to the lingual nerve. A full-thickness mucoperiosted flap is reflected which exposed the mylohyoid ridge area and muscle Attachments. This attachment are removed from the ridge by sharply incising the muscle attachment At the area of bony origin.
When the muscle is released the underlying fat is visible in the Surgical field. After reflection of the muscle a rotary instrument or bone file can be used to remove the sharp prominence of the mylohyoid ridge.
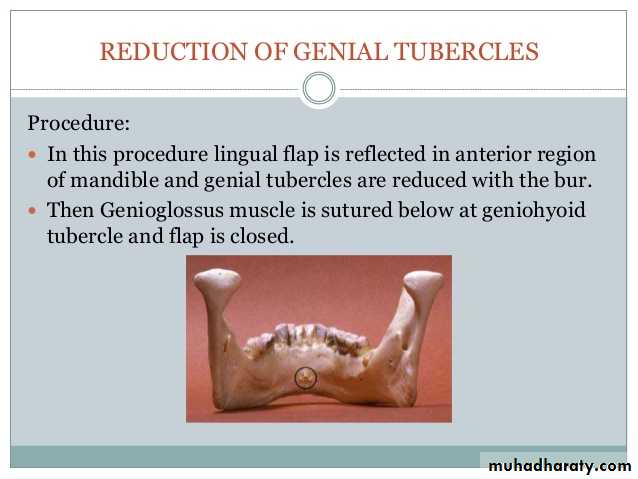
Genial tubercle reduction:-
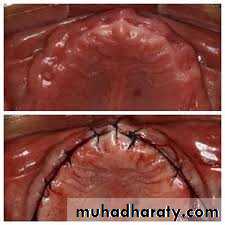
As the mandible begins to undergo resorption. The area of the attachment of the genioglossus muscle in the anterior portion of the mandible may become increasingly prominent. Which require reduction to construct the prosthesis properly. Before a decision to remove the prominence is made consideration should be given to possible augmentation of the anterior border of the mandible rather than reduction of the g. tubercle. If augmentation is the preferred treatment the tubercle should be left to add support to the graft in this area.Maxillary Tori:-
maxillary torus Consist of bony exostosis formation in the area of the palate. The origin of maxillary torus is unclear they are found in 20% of the female population. approximately twice the percentage in males. Tori may have multiple shapes and configurations ranging from a single smooth elevation to a multi lobulated pedunculated bony mass. This bony mass interfere with proper design and function of the prosthesis.Surgical removal began with bilateral greater palatine and incisive blocks a linear incision in the midline of the tours with oblique
vertical releasing incisions at one or both ends is generally necessary.
A full palatal flap can be used to expose the multi lobulated tori then an osteotomy and mallet may be used to remove the bony mass.
For larger tori it is usually best to section the tori into multiple fragments with a bur in a rotary hand piece careful attention must be
paid to the depth of cuts to avoid perforation of the floor of the nose then the mucosa is re approximated and sutured to prevent hematoma
formation some form of pressure dressing must be placed over the area
of the palatal vault.
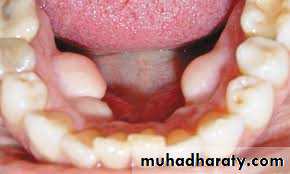
Mandibular tori:-
are bony protuberance on the lingual aspect of the mandible that usually occur in the premolar area. The origins of this bony exostosisare un certain and the growths may slowly increase in size occasionally extremely large tori interfere with normal speech or tongue function during eating. But this tori rarely require removal when they are present after the removal of lower teeth and before the construction of partial or complete dentures. It may be necessary to remove mandibular tori to facilitate denture construction.Soft tissue abnormalities:-
Abnormalities of the soft tissue in the denture-bearing and peripheral tissue area include excessive fibrous or hyper mobile tissue, inflammatory lesions and abnormal muscular and frenula attachments.Un supported hyper mobile tissue
Excessive hyper-mobile tissue without information on the alveolar ridge is generally the result of resorption of the underlying bone ill-fitting denture or both. If a bony deficiency is the primary cause of soft tissue excess then augmentation of the underlying bone is treatment of choice. But if the height of alveolar bone is adequate then excision of hyper mobile tissue is indicated.A local anesthesia is injected removal of hyper mobile tissue consists of two parallel full-thickness flap 'on the buccal and lingual aspects
of the issue to be excised. A periosteal elevator is used to remove the
excess soft tissue from the underlying bone than continuous or interrupted sutures are used to approximate the remaining tissue and
are removed 7 day after surgery.
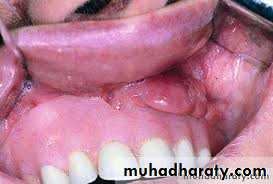
Inflammatory fibrous hyperplasia:-
I.F.H also called epulis or denture fibrosis is a generalized hyperplasic enlargement of mucosa and fibrous tissue in the alveolar ridge or vestibular area. Which aest fitting dentures. most often result from ill- 2 technique can be used either electrosurgical or laser techniques provide good results for tissue excision or by grasping the tissue with tissue forceps. A sharp incision is made at the base of fibrous tissue down to the periosteum the adjacent tissue is gently under mined and re approximated using interrupted or continuous sutures.
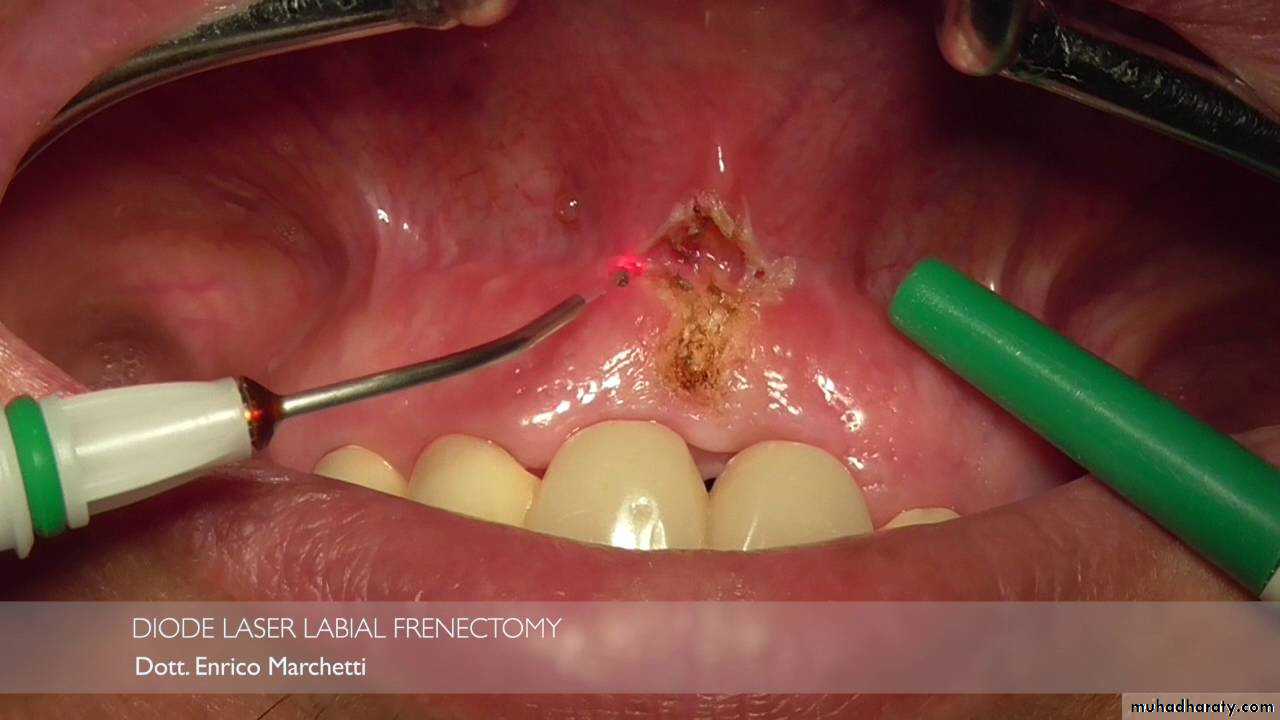
Labial frenectomy:-
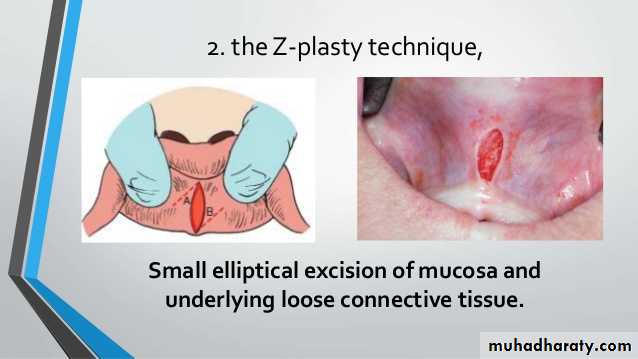
labial frenum attachments consist of thin bands of fibrous tissue covered with mucosa extending from the lip and cheek to the alveolar periosteum. The level of frenal attachments may vary from the height of the vestibule to the alveolar ridge and even to the incisal papilla area in the anterior maxilla.Three surgical technique are effective in removal of frenal attachments:-
1. The simple excision
2. The Z-plasty.
3. A localized vestibuloeplasty with secondary epithelialization.
For the simple excision technique a narrow elliptic in around the frenal area down to the periosteum, The fibrous fernium is sharply dissected from the underlying periosteum and soft tissue then the margins of the wound are gently undermined and re-approximated. Placement of the first suture should be at the maximum depth of the vestibule and should include both edges of mucosa and underlying periosteum.
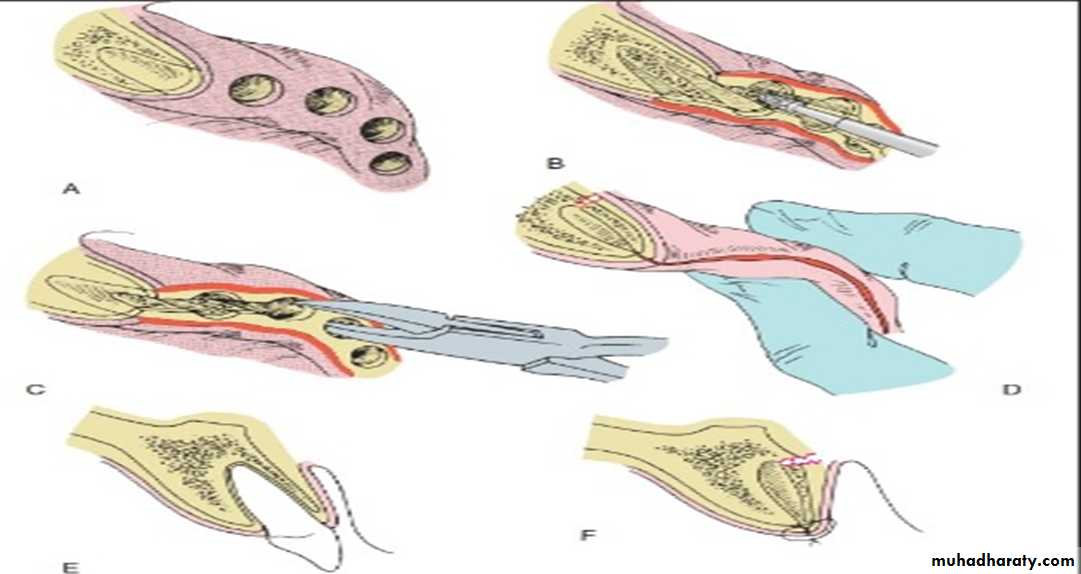
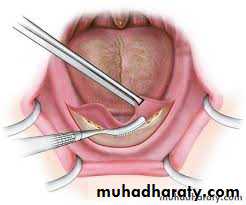
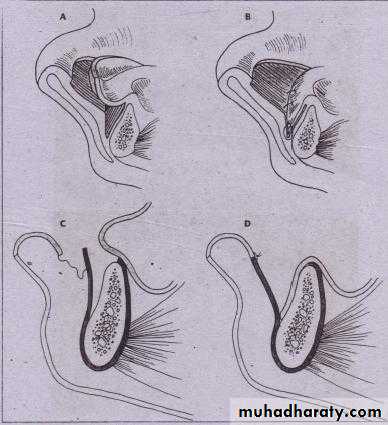
Lingual frenectomy-
An abnormal frenal attachment usually consists of mucosa, dense fibrous connective tissue. This attachment binds the tip of the tongue to the posterior surface of the mandibular alveolar ridge. Surgical release of the lingual frenum requires incising the attachment of the fibrous connective tissue at the base of the tongue in a transverse fashion followed by closure in a linear direction which completely release easy the anterior portion of the tongue.Transpositional flap vestibuloplasty:-
A lingually based flap vestibuloplasty procedure is explained as mucosel flap from the alveolar ridge is elevated from the underlying tissue and sutured to the depth of the vestibule.mandibular augmentation:-
Augmentation grafting adds strength to an extremely deficient mandible and improves the height and contour of the available bone for implant placement of denture-bearing areas. Sources of graft material include autogenous or allogeneic bone and alloplastic materials.Historically autogenous bone has been the most biologically acceptable material used in (M.A). Disadvantages of the use of autogenous bone include the need for donor-site surgery and extensive resorption after grafting. The use of allogenic bone eliminates the need for a second surgical site and has been shown to be somewhat useful in augmenting small area of concavity in the posterior mandible.
The HA alloplastic materials used in boney augmentation of the maxilla and mandible. The. Material is readily available, eliminate the need for donor-site surgery and has been shown to improve long-term maintenance of height and contour. The disadvantage includes tissue dehiscence. migration of the material and neurosensory disturbance have resulted in less frequent use of this material