Fifth Stage
Orthopedics
Dr. Haider – Lecture 6
1
Spine fractures
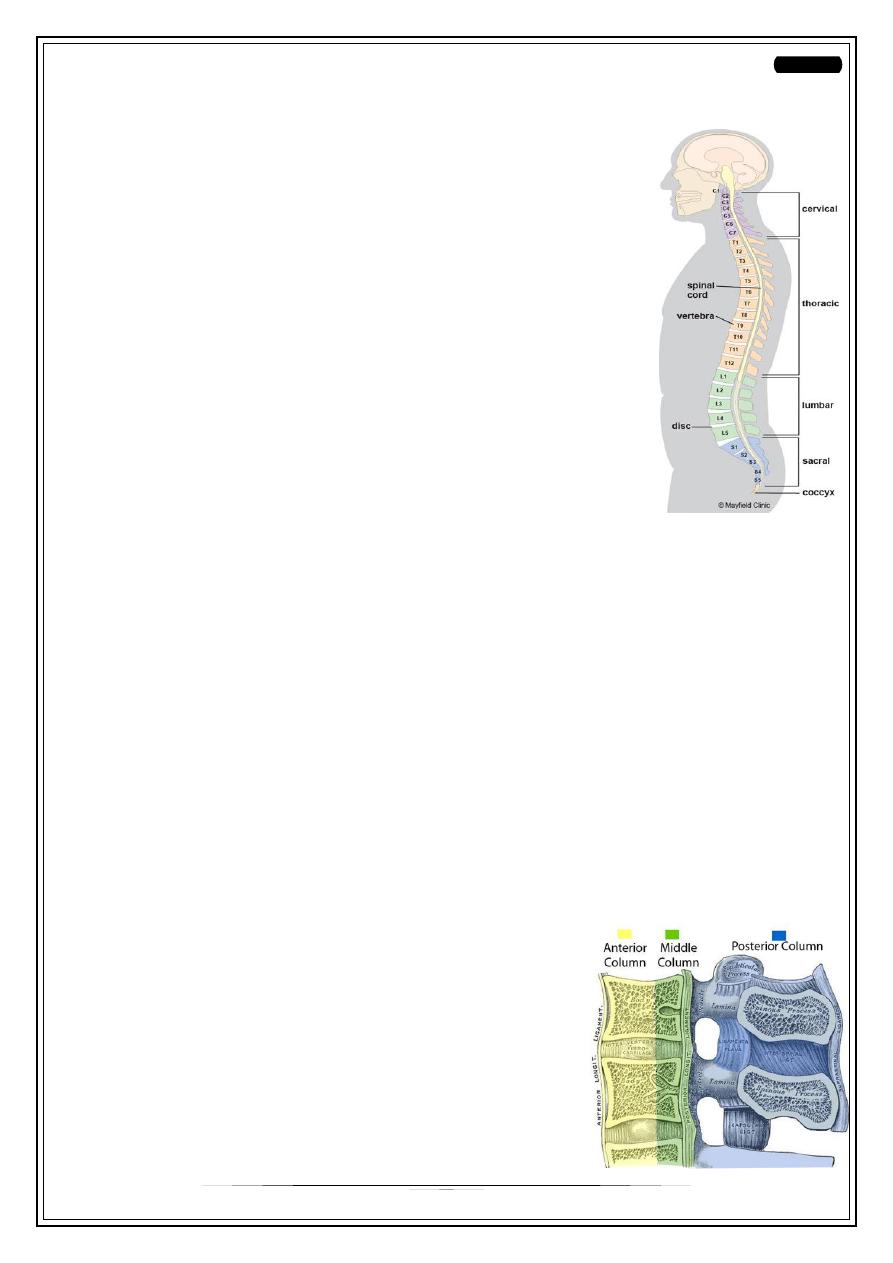
Anatomy :
• Cervical - 7 vertebrae
• Thoracic - 12 vertebrae
• Lumbar - 5 vertebrae
• Sacral - 5 fused vertebrae
• Coccyx - 4 fused vertebrae
Incidence:
4-5 per 100,000.
18 - 35 years.
Male\ Female = 4:1
Neurologic injury -> 25% of cases.
65% of TL#s occurs between the T9&L2 vertebrae. (thoracolumbar Junction) ..
Why ?
• The transition from a relatively rigid thoracic kyphosis to a more mobile lumbar
lordosis occurs at T11–12.
• The lowest thoracic ribs (T11 and T12) provide less stability at the
thoracolumbar junction region compared to the upper thoracic region, because
they do not connect to the sternum and are free floating.
Etiology
• High energy trauma like RTAs
• Fall from height
• gunshot wound and missile injuries
• osteoporosis
• tumors
• other underlying conditions that weaken bone
Classification:
Denis Three column theory :
•
The vertebral column is divided into three columns
1. ANTERIOR
2. MIDDLE
3. POSTERIOR Columns
2
When the spine injury is considered unstable? :
1. When more than one column involved
2. Anterior vertebral height loss > 50%.
3. Canal compromise > 50%.
4. Kyphosis>20degrees.
5. Neural compression.
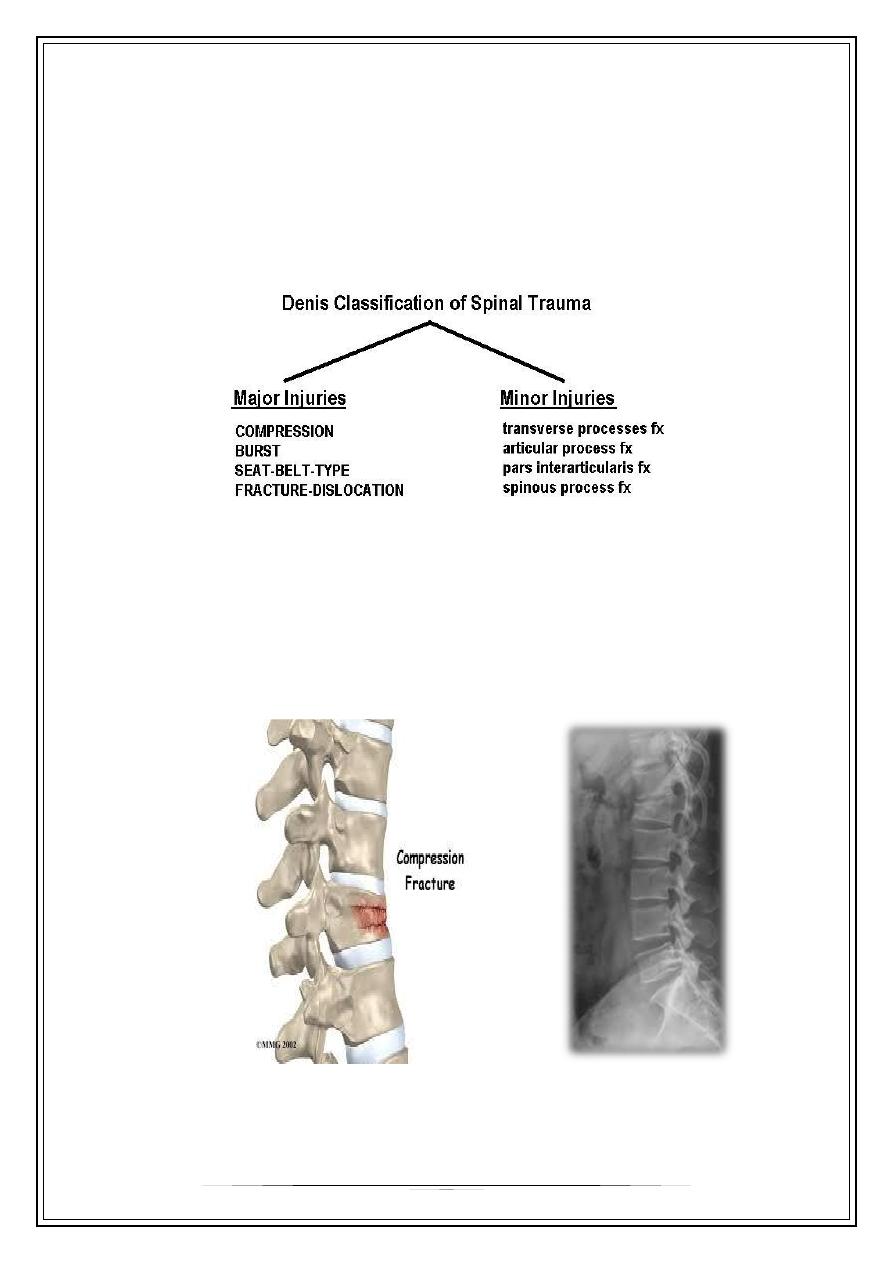
Compression( wedge ) fracture
•
45% of TL#s
•
Failure of anterior column
•
The middle column is intact and acts as a hinge.
•
Low risk of Neurological deficits .
3
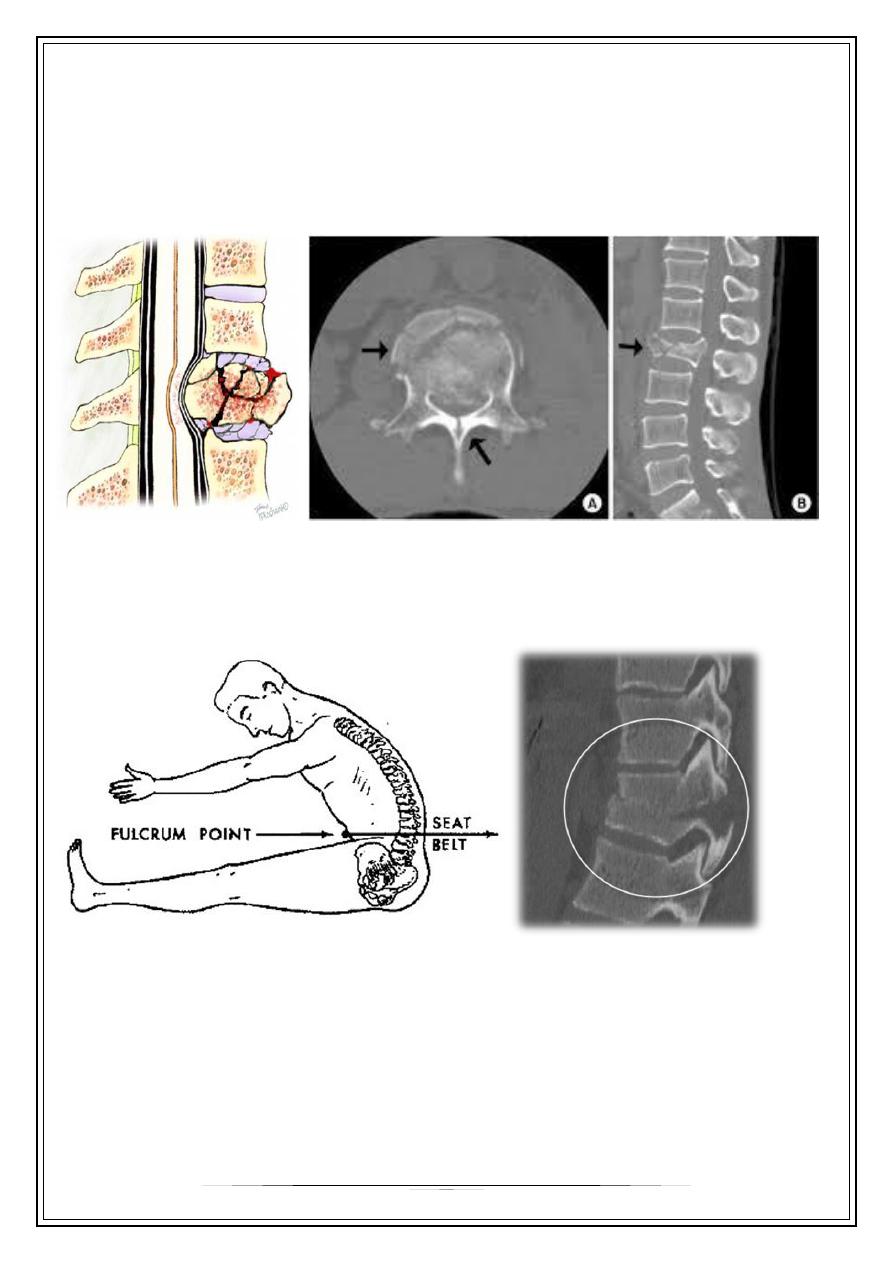
Burst fractures
• 15 % of TL#s
• Anterior&middle column failure. (Axial compression)
• Most common at T/L junction
• Neurological deficit incidence is higher.
FLEXION-DISTRACTION = SEAT-BELT-TYPE = CHANCE #:
• Posterior &middle columns failure. (hyperflexion then tension forces)
• Anterior columnà functions like a hinge.
Fracture-Dislocation:
•
Failure of all columns (compression, tension,rotation, or shear).
•
anterior hinge is disrupted.
•
Dislocation.
•
the highest incidence of neurological deficit.

4
Approach to Spine Trauma
Pre Hospital Care:
• Proper extraction &Immobilization
-
Cervical collar
- Hard board (log roll)
- Sand bag and Tape
• Airway protection.
• Rapid & safe transfer à for suitable facilities.
Log rolling:
Emergency Assessment
•
Primary survey : ABCs
•
Secondary Survey:
•
Brief history (Mechanism, movement, position)
•
Examination : The inspection and palpation of the spine should include the search
for: Swellings, Tenderness , skin bruises, lacerations, ecchymoses , open wounds ,
hematoma and spinal (mal)alignment
5
Neurogical examination :
•
Neurological injuries may be complete or incomplet
•
Complete - flaccid paralysis + total loss of sensory & motor functions
•
Incomplete - mixed loss
- Anterior spinal cord syndrome
- Posterior spinal cord syndrome
- Central cord syndrome
- Brown sequard’s syndrome
- Cauda equina syndrome
Investigations :
•
plain X-rays: - A-P & Lateral views
•
CT
•
MRI studies
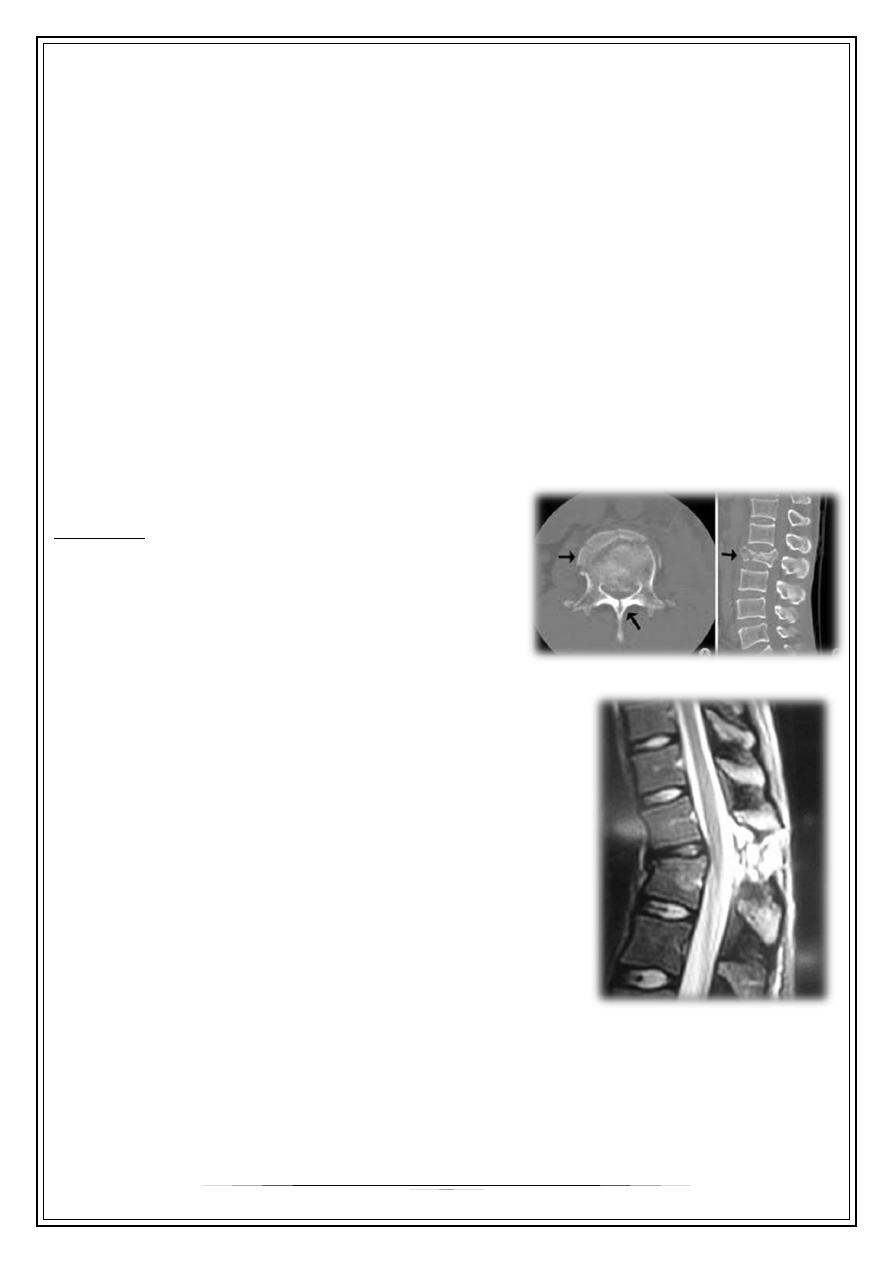
CT Scan :
Accurate assessment of bone.
1- Comminution.
2- Canal compromise.
MRI :
Accurate assessment of soft tissue.
1. Neurological or cord injury .
2. Ligament injury.
3. Disc herniation.
4. Hematoma.
Treatment of spine injuries
Goals :
•
Maximise neurological recovery .
•
Maintain or restore spinal alignment.
•
Obtain a healed and stable spinal column.
•
Prevent future deformity.
6
Spinal Cord Injury medical treatment
•
Methylprednisolone 30mg/kg iv bolus over 15min. 5.4 mg/kg/h infusion over 23
hrs
•
Proton pump inhibitor
•
LMW Heparin ( thrombo prophylaxis )
Non-operative treatment :
Indications:
•
Ant. vertebral height loss < 50%.
•
Canal compromise < 50%.
•
kyphosis<20degrees.
•
No neurological compromise
•
Strict bed rest for 3- 4 weeks.
•
Bracing for 6-8 weeks.
•
Pain killers
•
Patient care
Operative treatment :
•
Ant. vertebral height loss > 50%.
•
Canal compromise > 50%.
•
Kyphosis>20degrees.
•
Neural compression ( especially if progressive ).
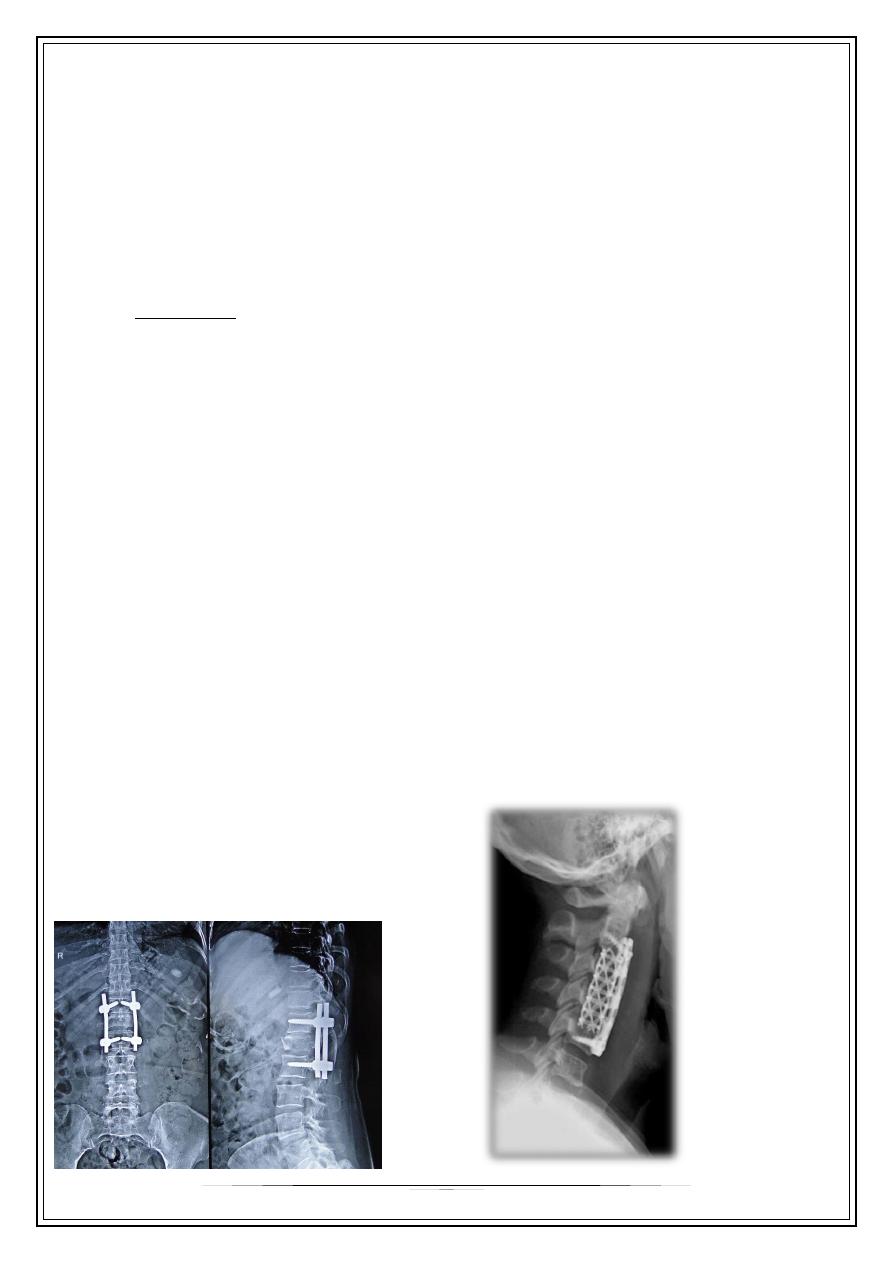
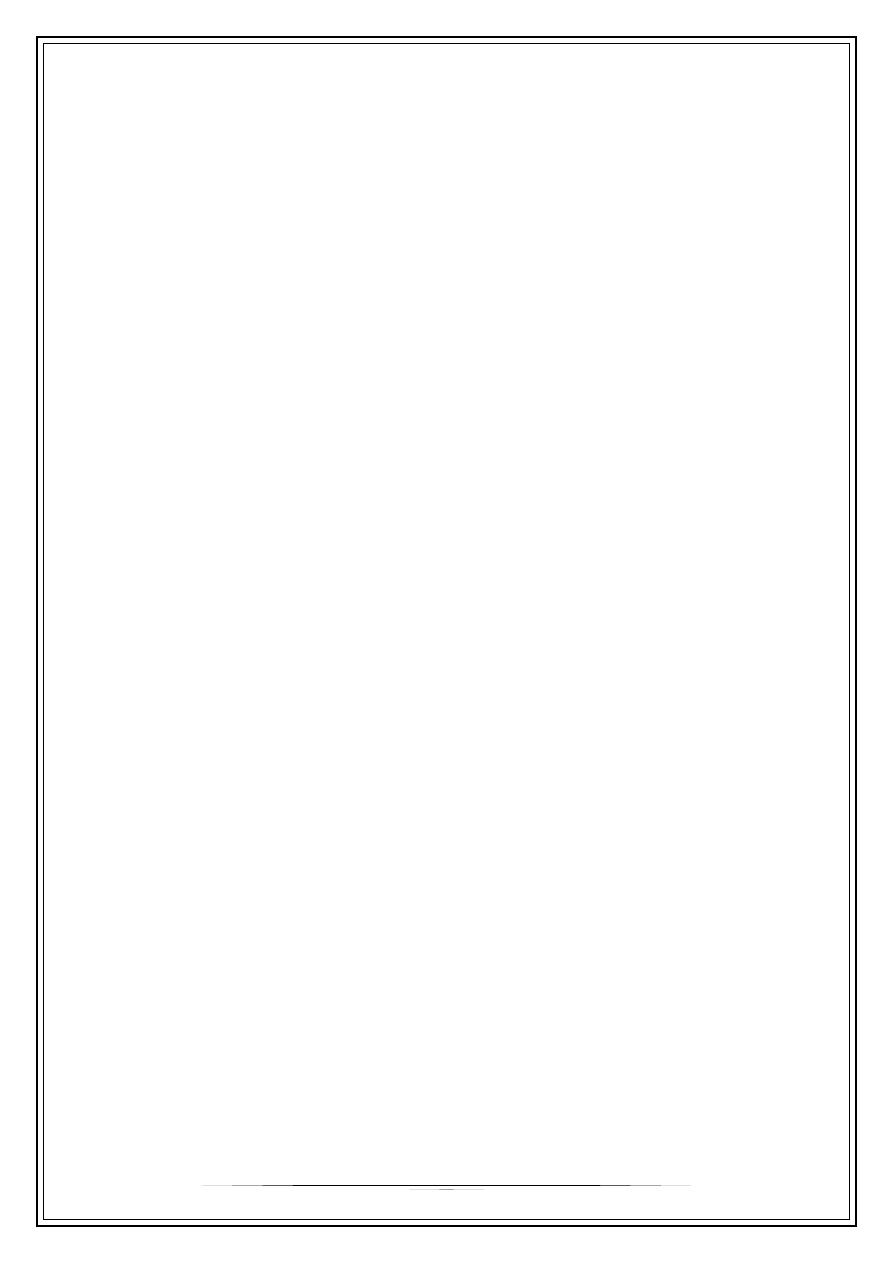
Surgical options
•
Posterior Fixation
•
Anterior Fixation
•
Combination of both
7
Rehabilitation
•
DVT prevention.
•
Bed sore prevention: Postural change/2h, Air mattress, High protein diet.
•
Chest physiotherapy.
•
Bladder dysfunction: Intermittent cath.
•
Bowel dysfunction: high fluids, fibers, Prokinetic.
•
Spasticity: Stretching exercises, Baclofen.
Thank you,,,
