Oral Ulcers
Lecture 6 - 7Dr. Lana Shabur Talabani
• Definition
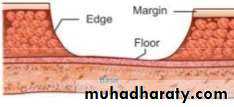
• Ulcer has been defined as a deeper crater that extends through the entire thickness of surface epithelium and involves the underlying connective tissue.• Parts of an ulcer
• Margin :
• Margin is the border or transitional zone of skin around an ulcer.• Edge:
• Edge is the mode of union between the floor and the margin of• ulcer.
• Floor:
• Floor of ulcer is the exposed surface of the ulcer, we look for
• Oral ulcers Diagnosis
• Multiple ulcers:• Acute
• chronic
• recurrent ulcers
• single ulcer
• Classification
• ACCORDING TO ETIOLOGY• Local Trauma
• Trauma due to sharp and malposed teeth
• Trauma due to restoration
• Trauma from injecting needle
• Infections
• Viral• Herpes Simplex
• Herpes Zoster
• Chicken Pox
• Small Pox
• Measles
• Hand foot mouth disease
• Herpangina
• AIDS
• Bacterial
• Tuberculosis
• Syphilis
• ANUG
• Fungal Infection
• Candidiasis• Histoplasmosis
• Blastomycosis
• Classification
• Allergy
• Local ( Stomatitis Venenata)• Systemic ( Stomatitis medicamentosa)
• Neoplastic
• Squamous cell carcinoma• Mucoepidermoid carcinoma
• Basal cell carcinoma
• Melanoma
• Malignant Lymphoma
• Systemic
• Blood disorder
• Agranulocytosis
• Cyclic Neutropenia
• Leukemia
• Classification
• Traumatic Ulcer
• Most common oral ulcer• Caused by : Mechanical , Chemical & Thermal
• Etiology
• Repeated trauma from tooth brushing• Drugs – Narcotic drugs
• Denture induced
• Self-inflicted in decerebrate and comatose patients
• Placement of fixed acrylic tongue stent
• Features :
• Tender in the area of lesion
• Borders : Raised and reddish
• Base : Yellowish white necrotic that can be easily removed
• Ulcer on vermilion border of lip – crusted surface because of absence of saliva
• Etiology• Management
• Heals in 10 days• Fluocinonide (0.05 %) or triamcinolone (0.1 %) acetonide in a emollient base before bedtime
• Base protects the denuded tissue from contamination and corticosteroid therapy tends to arrest inflammatory cycle
• Oral Bandage materials : Hydroxypropyl methylcellulose also promote healing
• Chlorhexidine mouthrinse
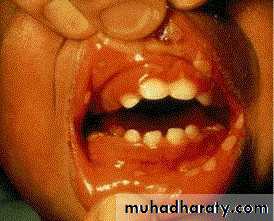
• 1ry herpes simplex
• Onset: after 6 months ,Peak within 2-3 years
• Clinical features:• Prodrome :1-2 days before appearance of local lesions fever ,headache ,lymphadenopathy, malaise, vomiting)
• generalized acute marginal gingivitis
• multiple vesicles turn to painful, bilateral ulcers surrounded by erythematous halo
• mainly keratinized gingiva
• mainly at anterior area of oral cavity
• Acute multiple ulcers
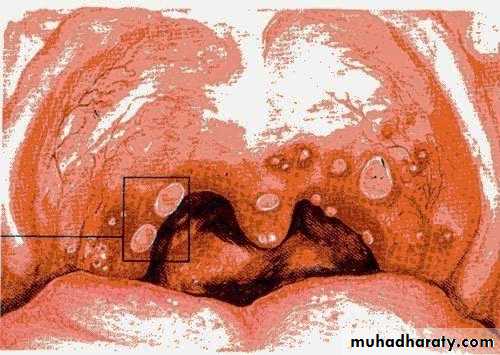
• 2. Herpangina
• By coxsackie virus A4 Affect children from 3-10 years, peak from June to October• Clinical picture :
• prodrome ,milder than herpes simplex (fever , anorexia, malaise)
• sore throat ,dysphagia
• ulcers mainly at post .area of oral cavity (soft palate , tonsils ,posterior pharynx)
• ulcers smaller than herpes
• at post area and more painful.
• no marginal gingivitis
• mainly in epidemics
• 3. Hand- foot and mouth disease
• Caused by coxsakievirus A16,from 8 months to 33 years ,75%under 4 years.
• Clinical picture:• low grade fever
• oral vesicles and ulcers more extensive than herpes(mainly palate, buccal mucosa)
• macules and papules on extensor surface of hand and feet.
• examine hands and feet for maculopapular lesions and vesicles if there is acute stomatitis and fever
• 4. Chicken pox
• 1ry infection of varicella –zoster virus:
• Cutaneous lesions:• Maculopapular lesion then turn to vesicles on erythematous base
• Oral lesions ,not diagnostic
• 5. Herpes zoster (shingles)
• Clinical picture:• Prodrome: 2-4 days (shooting pain, paresthesia,burning sensation) along the course of the nerve
• unilateral vesicles on erythematous base, appears as clusters along the course of the nerve.
• the most diagnostic manifestation is the unilateral appearance of lesions
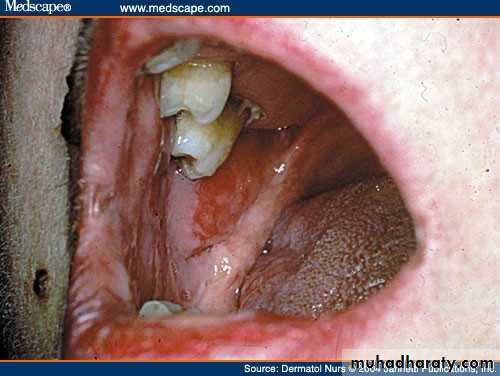
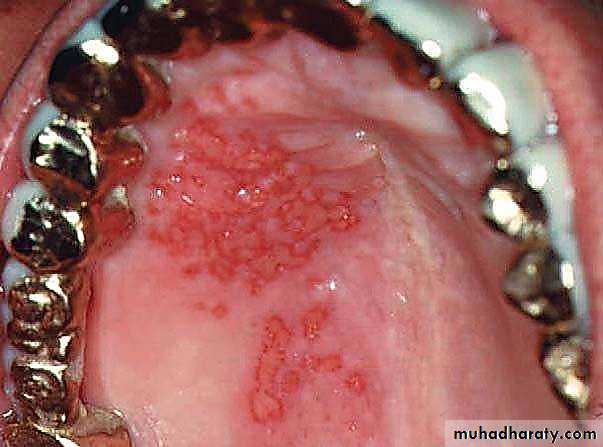
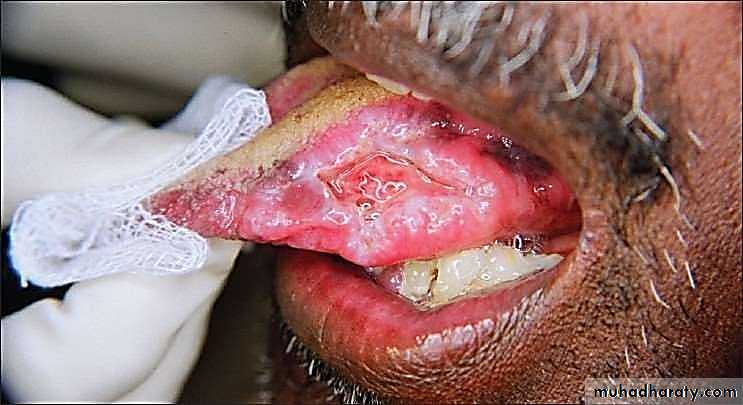
• 6. Erythema multiforme
• Affects children and young aged Rare after 50• Clinical picture :
• No prodrome ,systemic and local lesions appear together, with very rapid onset.
• oral lesions
• bullae or vesicles on erythematous base ,then rupture.
• lesions orally are anywhere but lips are more prominent, and rare gingival involvement most diagnostic), where lips are extensively eroded and large portion are denuded of epithelium.
• E.M lesions are large, irregular, deep and often bleeds and there are tissue remnants
• Erythema Multiforme
• It is an acute, self-limited, inflammatory mucocutaneus disease that manifests on skin and often oral mucosa.
• It represents a hypersensitivity reaction to infectious agents (HSV, mycoplasma and Chlamydia pneumonia) or medications (NSAIDS, anticonvulsants)
• Classic skin lesions : ‘target’ or ‘iris’ lesions
• Ulceration and crusting is common in lip and ulcers on oral mucosa
• Cutaneous lesions:
• Appears on hands and feet• ,extensor surface.
• Macules ,papules ,vesicles, or bullae
• target lesion or Iris lesion (central bulla or pale surrounded by edema or erythema)
• B. Chronic multiple ulcers
• 1. Pemphigus vulgaris• 1. Cutaneous lesions:
• Thin walled bullae arising on normal skin and mucosa.
• Bullae breaks rapidly leaving erosions and continuously spread peripherally.
• The mostly diagnostic manifestation:
• apply pressure to bullae extend peripherally nikolysks sign
• B. Chronic multiple ulcers
• 2. oral lesions:• usually presents 4 month before cutaneous lesions
• Clinical manifestations: classical bulla on uninflammed area ,then rapidly breaks leaving irregular erosions and ulcers ,that extend peripherally.
• leaves denuded area
• Mainly at buccal mucosa•
• Differential diagnosis
• Its chronic appearance differentiate it from (H.S,H.Z and E.M)• From R.A.S that its lesions are recurrent and heals rapidly, but pemphigous lesions extends peripherally and takes a period of weeks to months.
• lesions of pemphigus not small ,rounded and symmetrical like R.A.S and viral ulcers, and there is detached epithelium at the peripheries.
• +ve nikolysks sign
• bullae extend peripherally
Management of pemphigus vulgaris:
• High doses of systemic corticosteroids (1-2mg/kg/dl).• Adjuvant therapy : adjuvant drugs are immunosuppressie drugs like mycophenolate mofetil, azathioprine, cyclophosphamide, and cyclophosphamide pulse therapy
• Prednisolone tablets
• Dapsone
• Recalcitrant cases are treated rituximab
• 2. Mucous membrane pemphigoid
• Age over 50.• Mainly mucosal surfaces( eye- oral cavity)
• Clinical manifestation:
• Desquamative gingivitis.
• vesicles that rupture leaving erosions that spread peripherally more slowly and self limited than pemphigus.
• +ve nikolyskis sign
• no cutaneous involvement.
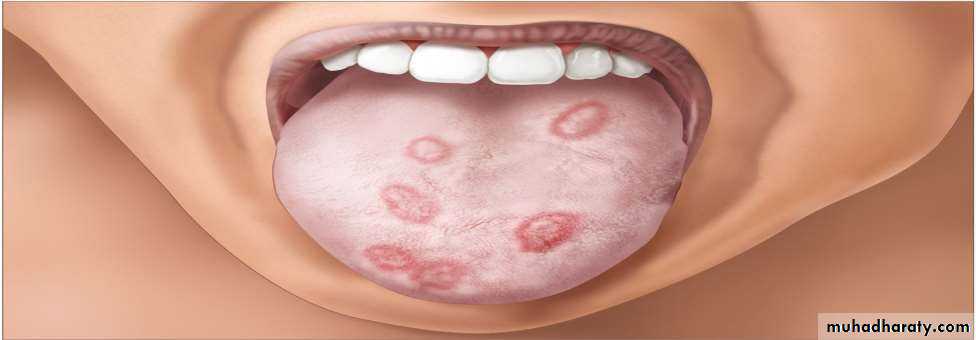
• C. recurrent oral ulcers
• RECURRENT ORAL ULCERS• Recurrent Aphthous Ulcer
• RIHS : Recurrent intraoral herpes simplex Major Aphthous ulcer• Herpetiform Aphthae
• 1. Recurrent aphthous stomatitis• Mostly begin during the 2nd decade
• Clinical picture:
• Prodrome :from 2-48 hrs before ulcer appear burning sensation)
• Localized erythema then small white papule then ulcerates
• not preceded by vesicles, uniform, rounded ,painful covered by yellowish membrane and surrounded by erythematous halo about 10mm).
• no tissue remnants on borders, (there are no vesicles.)
• mainly on lining mucosa rare on keratinized mucosa
• Minor
• Major aphthous: (1- 5cm)• Appears on keratinized and non keratinized mucosa.
• Indurated base ,everted edges, very painful and leave scar.
• Takes more than a month to heal.
• major
• Herpetiform• (least common)
• Dozens or hundreds of ulcers about 1-2 mm, very painful surrounded by erythematous halo.
• herpetiform
• Comparison of Clinical Features• RAU
• RIHS
• Location:
• Nonkeratinized mucosa
• Keratinized Mucosa
• Initial Lesion :
• Erythematous macule or papule
• followed by necrosis and ulceration
• Cluster of small discrete vesicles without red erythematous halo. Vesicles rupture to form small,punctate ulcers
• Mature lesion :
• Shallow ulcer with yellow necrotic
• center
• Smooth border and red halo
• Shallow ulcer but many in number
• and border is scalloped• 2. Behcets disease
• Between 20-40 Diagnosis:• oral recurrent ulcers (minor aphthae)at least 3 times within 12 months + 2 of the following:
• recurrent genital ulcers
• eye lesions: (uveitis,retinal vasculitis , corneal inflammation)
• skin lesions: maculoppapular lesions,erythema nodosum (reddish ,painful, tender lumps )
• +ve pathergy test :cutaneous hyperactivity to intra-cutaneous injection, within 24 hrs)
• (appearance of small red bump or pustule)
• Erythema nodosum
Pathergy test
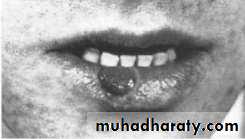
• 3. Recurrent herpes simplex• 1. recurrent herpes labialis common (cold sores, fever blisters (. by fever, menstruation, u.v, emotional stress
• Clinical picture:
• Prodrome, tingling and burning sensation then edema and clusters of vesicles at mucocutaneous junction and spread to skin ,then coalesce and weep exudate and then rupture and crust
• 2. recurrent intraoral herpes: vesicles turn to ulcers ,mainly keratinized mucosa (gingiva –hard palate)
• Recurrent Intraoral Herpes Simplex
• After primary infection HSV enters a latent stage and later becomes reactivated by various stimulae and recur as a vesiculoulcerative lesion on the skin, perioral tissue, and oral mucosa• Herpetic Whitlow is an occupational disease of practising dentists and dental workers.
• This may be contracted while working on a patient with the herpetic lesion• Lesions of finger are recurrent and may spread to whole hand
• Syphilitic Ulcer
• Veneral disease caused by motile spirochete Treponema Pallidum• Primary Lesion – Chancre (solitary)
• Secondary lesions – numerous macules, papules, condylomas, or combinations
• Tertiary lesions – Gumma and interstitial glossitis
• Chancre
• Develop 3 weeks after inoculation and may persist upto 2 months• Primary oral lesion occurs most often on the lips, on tip of the tongue, in tonsillar region, or on the gingivae – commencing as macules and papules and then ulcerate
• Mature chancre measure from 0.5-2cm and have narrow, copper coloured, slightly raised borders with reddish brown base or center
• Chancre is extremely contagious
• Management : Systemic Penicillin from the early days
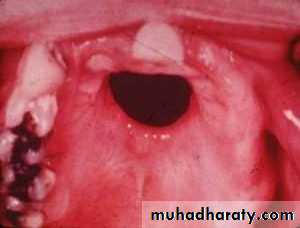
• Gumma
• Occur in midline of the palate or tongue starting as small firm nodular masses and often growing to several centimeters• Necrosis commences within the nodules and produces ulceration in the surface epithelium
• Occasionally necrosis is destructive, causing perforation of palate and formation of persistent oronasal fistula.
• Ulcer secondary to systemic disease
• Uncontrolled Diabetes• Uremia
• Blood Dyscrasias ( Pancytopenia, Leukemia, Neuropenia, sickle cell anemia)
• The ulcers are tender, usually demarcated, and shallow with a narrow erythematous halo and yellowish necrotic material
• A painful regional cervical lymphadenitis is almost invariably present.
• Some Chronic oral ulcer
• Clinical features• Diagnosis
• Drug-induced ulcers
• Erosive lichen planus• Pemphigus vulgaris
• Mucous membrane pemphigoid Lupus erythematosus• Reiter's syndrome
• Tuberculosis
• Single, isolated ulcers, located on the side of the tongue, surrounded by an erythematous halo and resistant to usual treatments• Areas of atrophy, erosions or painful ulcers, generally resistant to conventional treatments
• Bullae appear in oral cavity (posterior region), forming painful ulcers with necrotic fundus and erythematous halo Spontaneous onset of bullae that readily rupture, giving rise to
• a highly painful ulcerated area (most common areas are palate and gingiva)
• Erythema and oral ulcers, without induration and accompanied by whitish striae and a tendency to bleeding Arthritis, urethritis, conjunctivitis and oral ulcers similar to
• those of recurrent aphtous stomatitis
• Primary tuberculosis: deep, irregular, persistent and painful ulcer on the tongue, with rolled border and granulation tissue in the fundus
• Secondary tuberculosis: chronic ulcer, painful and indurated
• Erosive Lichen Planus
• Mucous membrane pemphigoid• Tuberculous ulcer
• Pemphigus Vulgaris
• Histoplasmosis
• Most common fungal disease caused by organism Histoplasma Capsulatum• Three forms :
• Acute Histoplasmosis
• Chronic Histoplasmosis
• Disseminated Histoplasmosis
• Most oral lesions of histoplasmosis occur with the disseminated form of the disease
• Solitary, variably painful ulcerations of several weeks duration
• Margins : Firm, rolled margins• Clinically it may be confused with malignancy.
• Drug induced ulcers
• Single, isolated ulcers, located on the side of the tongue, surrounded by an erythematous halo and resistant to usual treatments.• widespread mucositis and ulceration, mainly caused by cytotoxic drugs used for anti-tumor chemotherapy
• cytotoxic drugs include 5-fluorouracil, methotrexate, bleomycin, and cisplatin.
• NSAIDs are popular drugs that are well-known to induce oral ulcerations• Differential list of Short term Ulcers
• Differential list of Short term Ulcers• Traumatic Ulcer
• RAU, RIHS, and herpetiform ulcers
• Ulcer as a result of odontogenic infection
• Ulcer occuring as a herald disease of generalized mucositis or vesiculobullous disease
• Ulcer secondary to noninfectious systemic disease
• Differential List of Persistent Ulcer
• Differential List of Persistent Ulcer• Traumatic ulcer
• Ulcer from odontogenic infection
• Major aphthous ulcer
• Squamous cell carcinoma
• Ulcer secondary to systemic disease
• Ulcer in HIV disease
• Traumatized tumour that does not ulcerate
• Low grade mucoepidermoid tumor
• Metastatic tumor
• Keratoacanthoma
• Necrotizing sialometaplasia
• Systemic mycosis
• Chancre
• Gumma
• Other rarities