
Endocrine Physiology
Posterior pituitary hormones
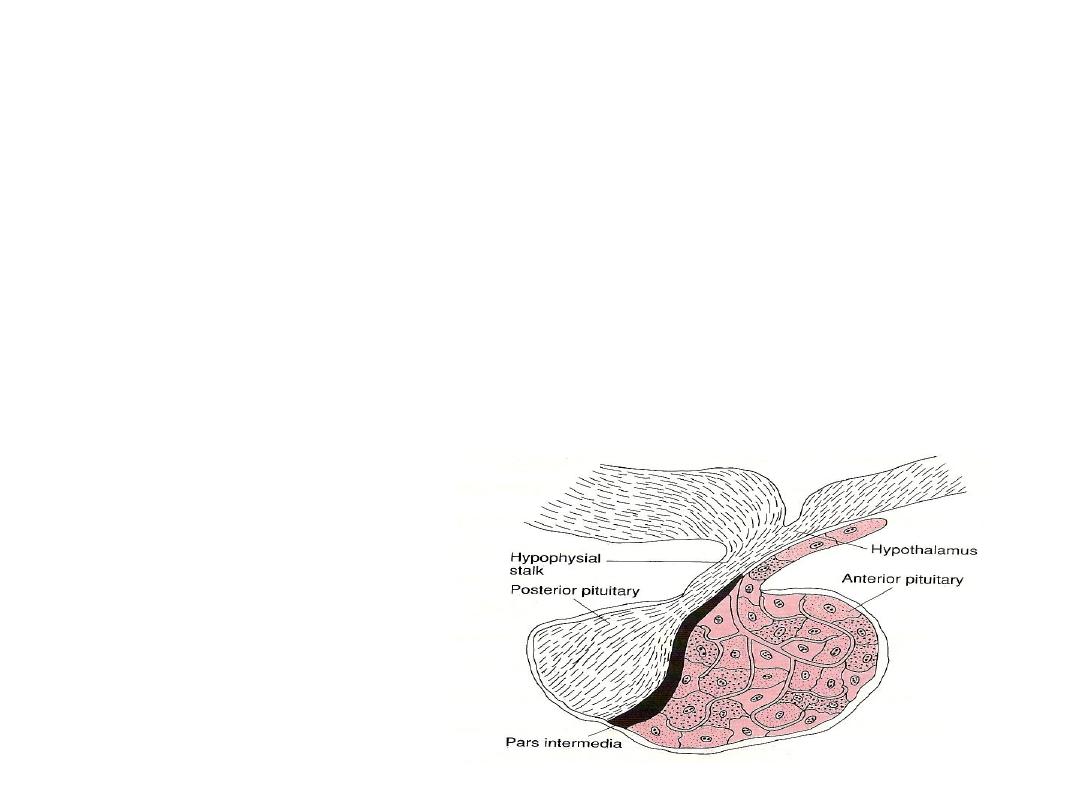
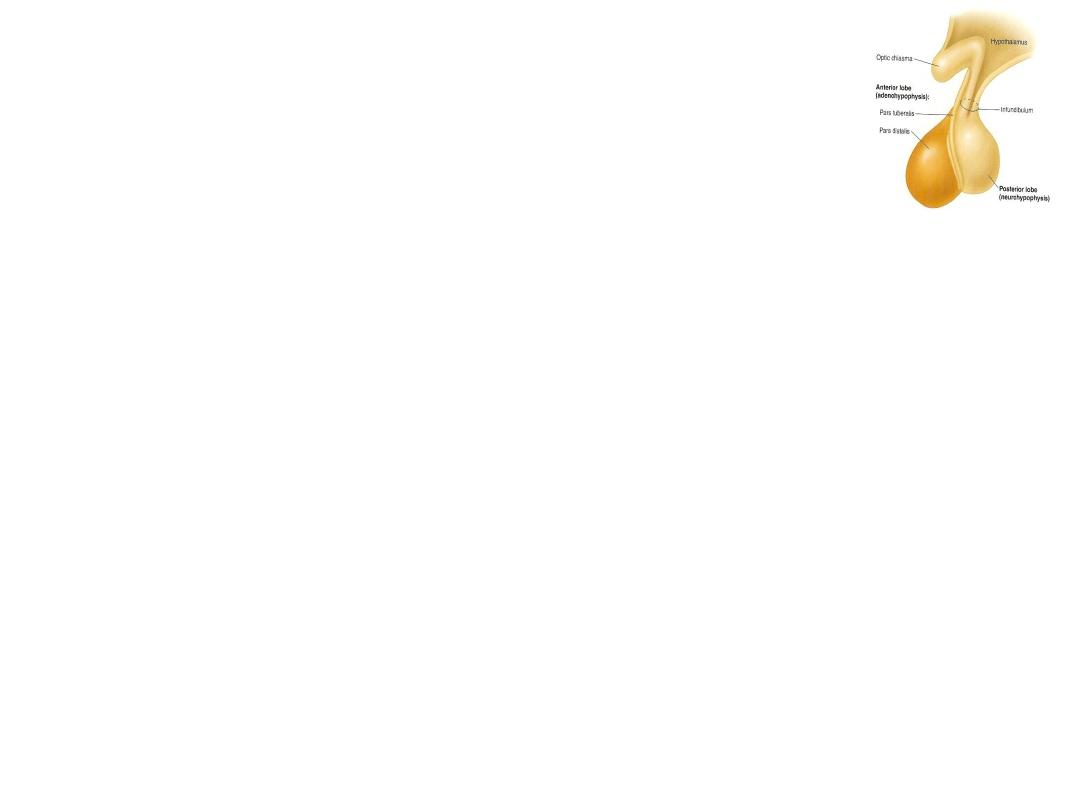
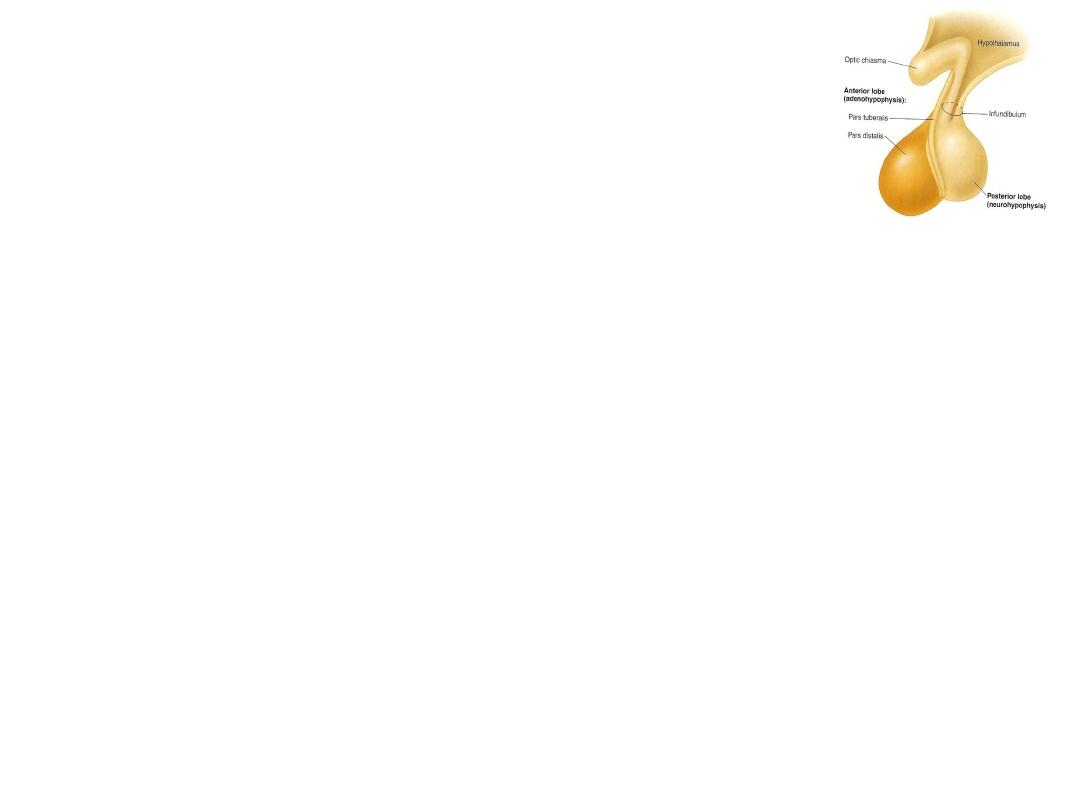
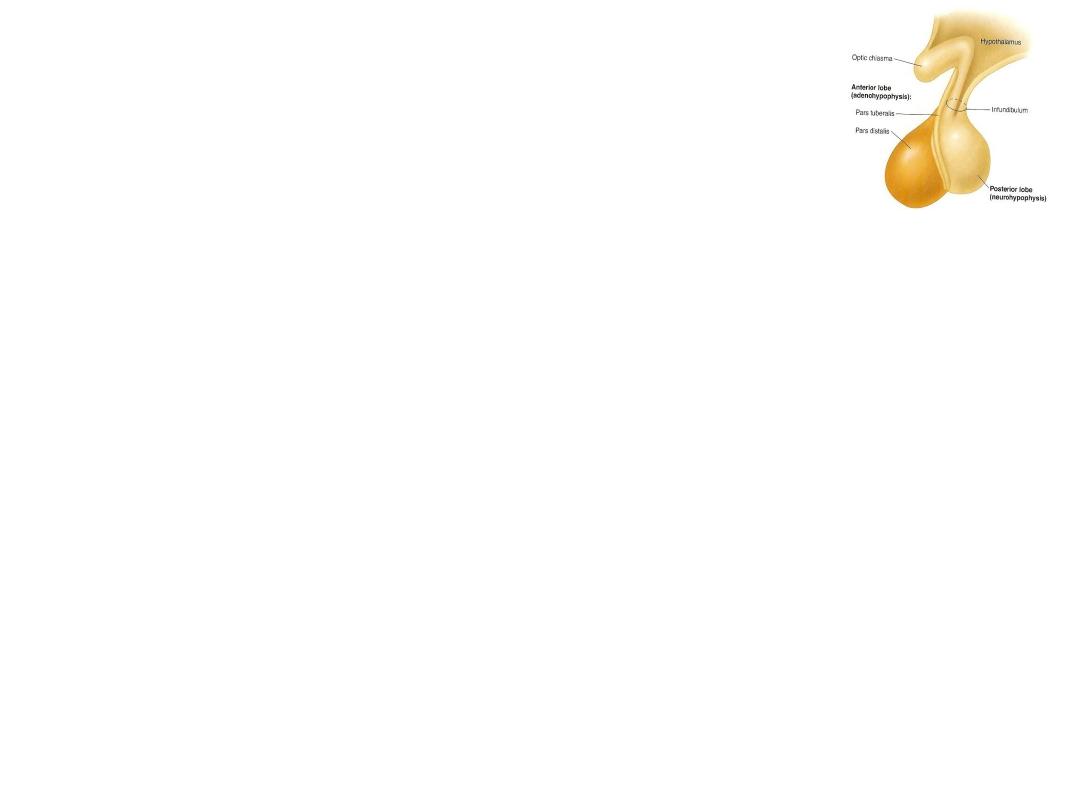
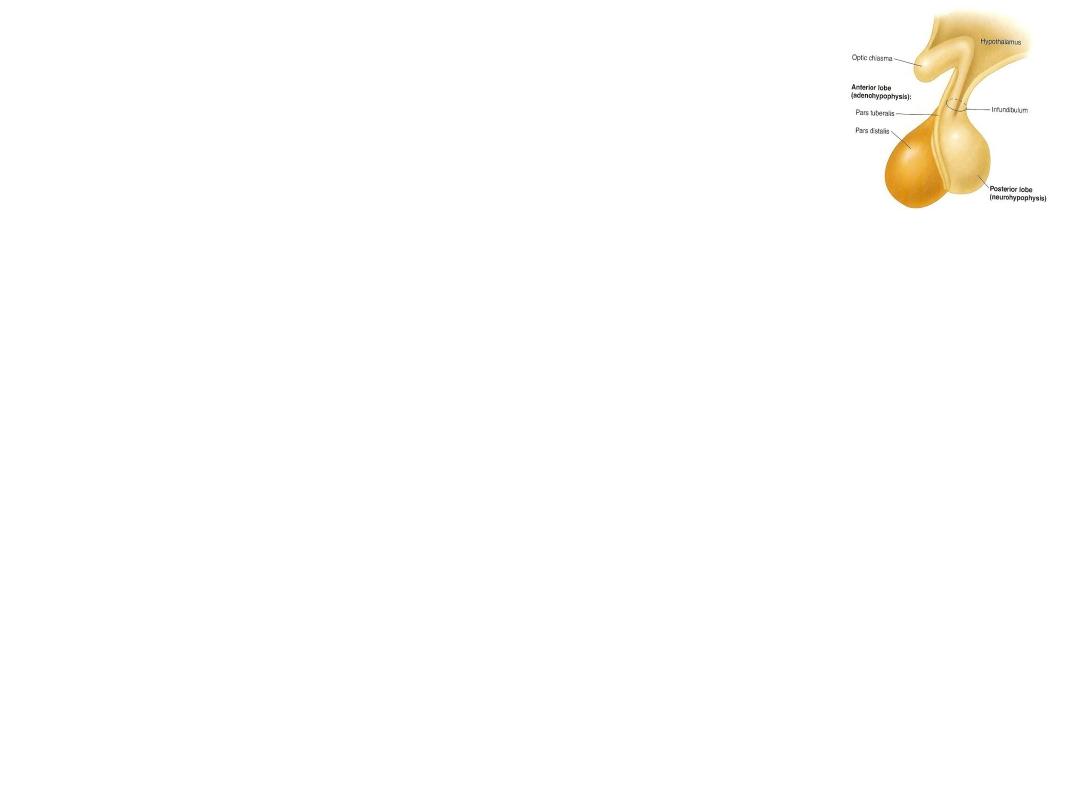
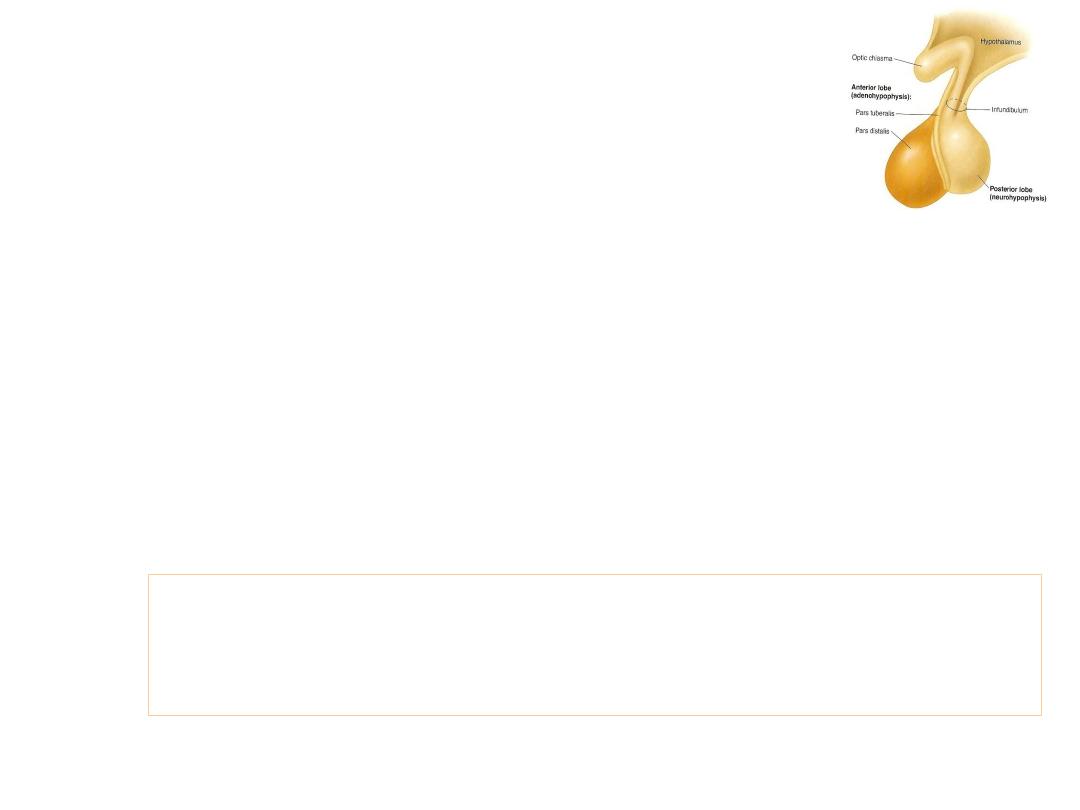
The posterior pituitary gland
Composed mainly of cells
called ‘Pituicytes’, which
act as packing & supporting
cells.
Stores & releases hormones
into the close capillaries.
These hormones are
produced in hypothalamus.
The posterior pituitary gland hormones
Posterior pituitary gland releases 2 hormones:
1. Antidiuretic hormone (ADH), or arginine vasopressin
(AVP).
2. Oxytocin
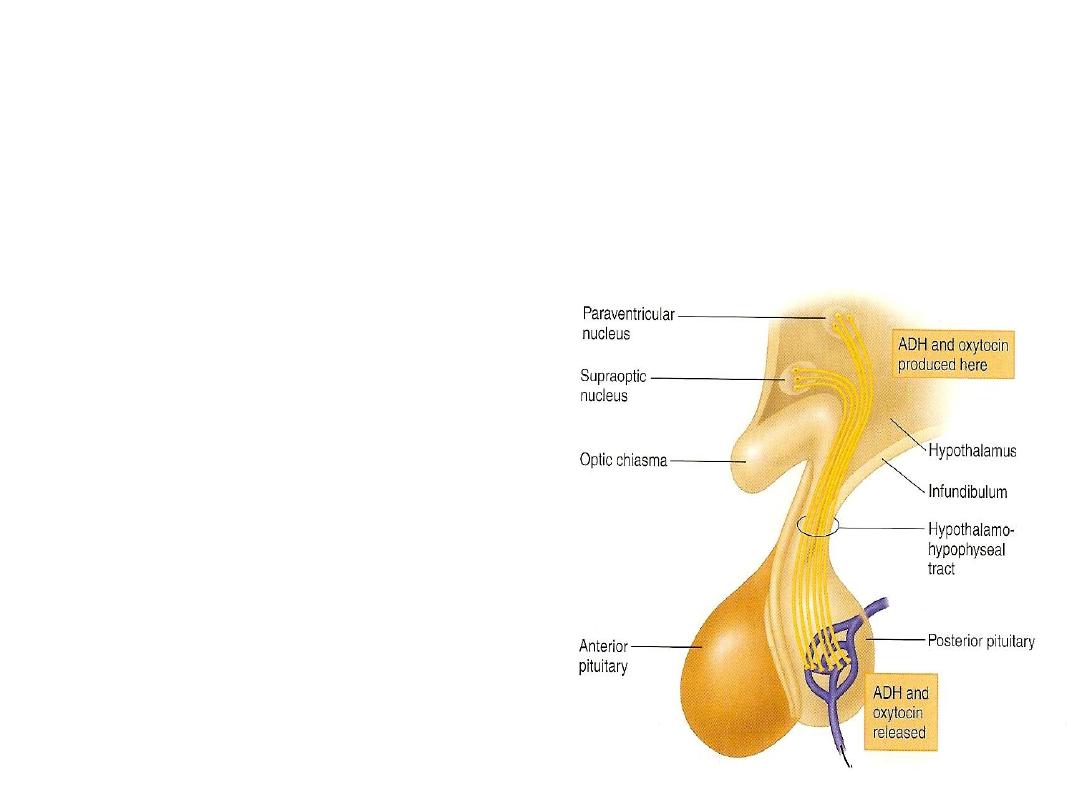
Both hormones are produced in hypothalamic nuclei:
- Supraoptic nucleus
(ADH + 1/6 oxytocin)
- Paraventricular nucleus
(Oxytocin + 1/6 ADH)
The posterior pituitary gland hormones … cont.
Both hormones are polypeptides, each contains 9
amino acids.
•
Both are transported slowly along the
‘hypothalamo-hypophyseal tract’
in combination
with carrier protein called ‘neurophysin’, to the
nerve endings in the posterior pituitary gland where
they are stored.
The posterior pituitary hormones –
1. ADH (vasopressin):
Antidiuretic hormone (ADH), or arginine vasopressin
(AVP), is produced mainly in SON of hypothalamus.
ADH activates (2) second messenger systems:
1. cAMP
2. IP
3
/Ca
2+
Action of ADH
ADH has 2 main effects:
1.
water re-absorption (retention) by distal tubules
& collecting ducts of the kidneys
decrease
osmotic pressure of the blood.
* This effect is regulated by V
2
receptors, through the
action of cAMP.
2.
Contraction of vascular smooth muscles
generalized
vasoconstriction.
* This effect is regulated by V
1
receptors, through the action
of IP
3
/Ca
2+
.
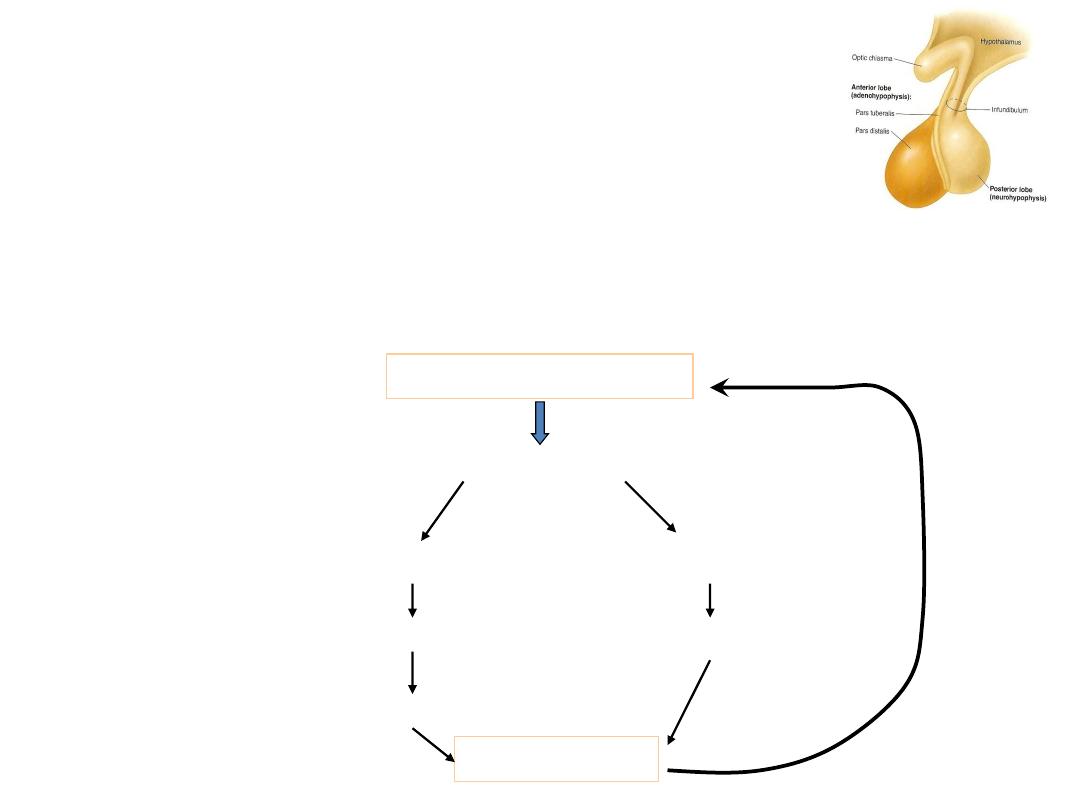
Control of ADH release
1.
in osmotic pressure of the ECF (
in plasma
osmolality), as in dehydration which will stimulate
osmoreceptors in the hypothalamus
ADH.
Hyperosmolarity of ECF
Receptors in
hypothalamus
More ADH release
Thirst
Collecting ducts of kidneys
Reabsorption of water
Water intake
Dilution of ECF
-ve feedback
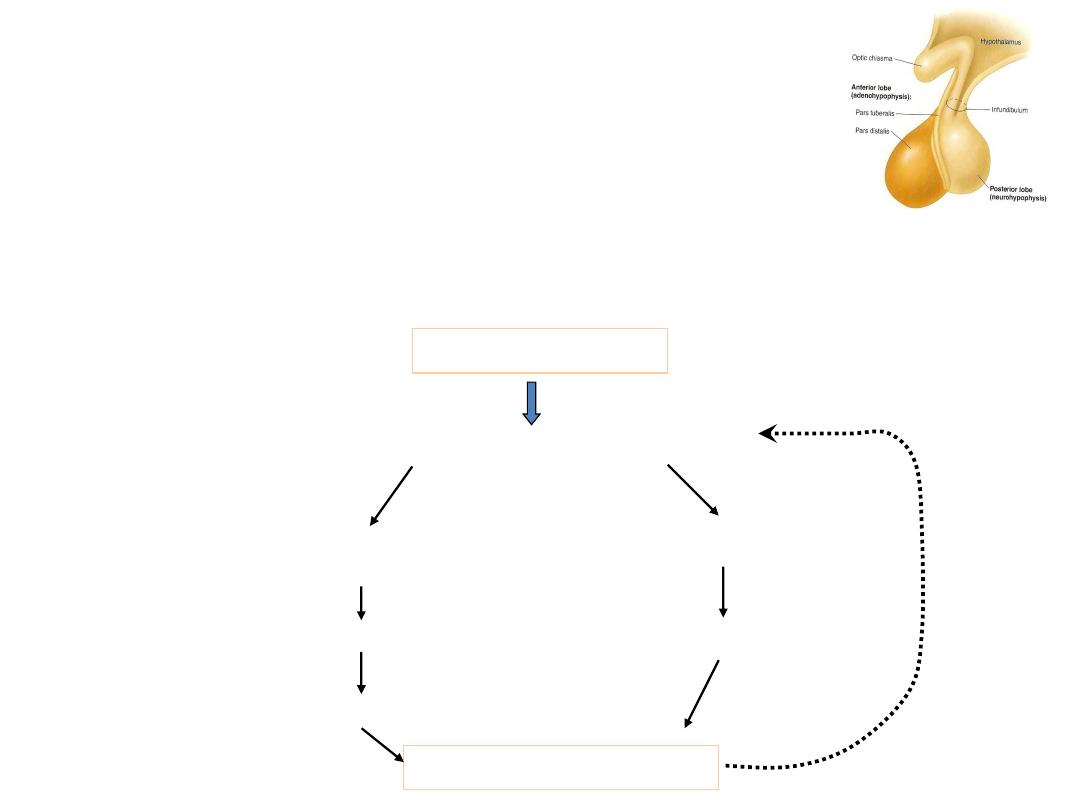
Control of ADH release … cont.
Loss of ECF volume
Less pressure in Rt.
atrium & great vessels
Less nerve impulse to
the hypothalamus
Thirst
More ADH release
More water reabsorption by kidneys
Water intake
Maintains ECF volume
2.
blood volume (
10%)
stimulate mechanoreceptors in
the great arteries (aorta & carotids) & right atrium
ADH.
Control of ADH release …cont.
3.
arterial blood pressure, due to
blood volume
ADH.
4.
Age:
ADH secretion
water retention & hyponatremia.
5.
Pain, emotional stress & physical trauma
ADH secretion.
6.
Drugs, e.g. morphine, barbiturates, & nicotine
ADH
secretion.
7.
Alcohol
ADH secretion.
Abnormalities of ADH release –
Hyposecretion:
Lack of ADH
Diabetes insipidus.
2 types of DI:
a.
Neurogenic (central, or cranial)
…
Problem in Hypothalamus or Post pituitary
gland; could be 1ry or 2ry.
R/: ADH.
b. Nephrogenic
…resistance of V
2
receptors
in collecting ducts of the kidneys.
- No ADH is needed as treatment.
Symptoms:
Polyurea
20 L/day (N
1.5 L/d), Polydepsia,
specific gravity of urine (diluted urine),
plasma osmolality.
Abnormalities of ADH release –
Hypersecretion:
ADH
, ‘Schwartz-Bartter Syndrome’:
- occurs after surgery.
- adenoma, ectopic kidney.
- Bronchial carcinoma.
Signs & Symptoms:
- Hyponatremia, i.e. [Na+]
extracellularly to 110 mM.
(N = 140 mM); resulting in:
- Mental confusion.
- Coma.
- Death, due to ventricular fibrillation.
The posterior pituitary hormones –
2. Oxytocin:
Produced mainly in the paraventricular nucleus
of the hypothalamus.
Action of oxytocin
1.
Contraction of smooth muscles of the uterus
enhance labor.
2.
Contraction of mammary gland myoepithelial cells of
the alveoli & the ducts
Ejection of milk as a reflex in
lactating women.
3.
In men
ejaculation.
Remember: Oxytocin is concerned with releasing or
ejection of milk, while prolactin is concerned with
synthesis & production of milk.
Control of oxytocin release
1.
Stimulation
(
suckling reflex)
oxytocin.
2.
Visual or auditory stimuli from the baby
oxytocin secretion.
3.
Distension of uterus & stretching of cervix during delivery
oxytocin release.
4.
Psychological & emotional factors, e.g. Fear, anxiety & pain
oxytocin.
5.
Alcohol
oxytocin secretion.
6.Hormones: a. progesterone
uterine sensitivity to oxytocin.
b. estrogen
uterine sensitivity to oxytocin.

