General Management
Of Facial InjuriesThe modern management of trauma is based on a firm understanding of the pathophysiology of trauma and an understanding of how patients actually die. This understanding has led to the development of several trauma systems, of which the Advanced Trauma Life Support (ATLS). It provides a systematic approach that should ensure that life-threatening and subsequent injuries are identified and managed in an appropriate and timely manner.
Principles of ATLS management:ABCDE of assessment (Rapid Primary Survey) (First, do no harm)Concept of the 'golden hour (i.e. time is of the essence)Need for frequent reassessment of evolving injuriesImportance of understanding the mechanism of injury
IMMEDIATE TREATMENTthe immediate treatment should be directed to the patient's general medical condition. It consists of : (Rapid Primary Survey ABCDE)* Airway with cervical spine control* Breathing and ventilation (oxygenation)* Circulation and control of hemorrhage* Disability assessment of neurological deficit (associated head injuries)* Exposure and Environmental control (Vision Threatening Injuries VTI)
The Airway:Obstruction of the patient's airway will lead rapidly to asphyxia and death and it is therefore the clinician's first concern. The most important factor controlling the patency of the air way in a patient with facial injuries is the level of consciousness.
The following measures is required:
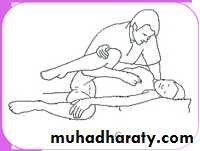
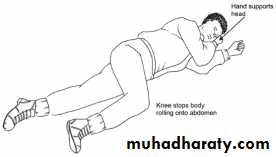
• Placing the head on his side .
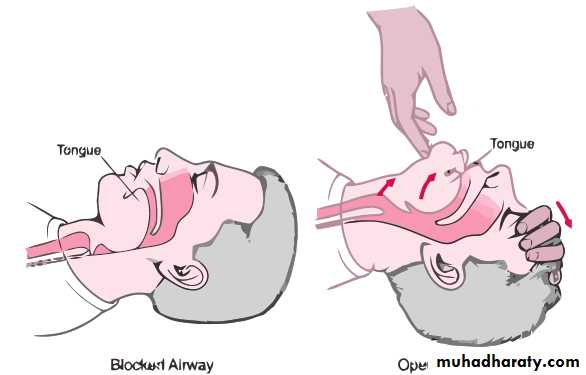
improving airways by 'Jaw Thrust Technique', however, this may be difficult to do in a conscious patient with mandibular fractures. It may also aggravate oral bleeding and usually painful for the patient .A fully oriented patient frequently wants to sit up with the face held forward.
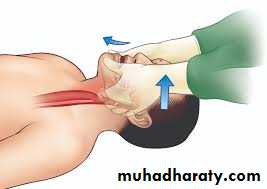
Chin thrust
Jaw Thrust2) Securing the airway by clearing the mouth and nasopharynx from dentures or portions of dentures together with avulsed, loose or broken teeth. Blood and mucus should be cleared using a wide bore blunt-ended sucker.
3) In Le Fort fractures, the upper jaw may have been pushed downwards and backwards so that the soft palate is resting upon the dorsum of the tongue and occlude the oral airway. In such cases two fingers are inserted behind the hard palate and the upper jaw is pulled gently upwards and forwards to enable the patient to breathe through the mouth.
4) Nasopharyngeal airway (armored soft latex nasopharyngeal tubes) can facilitate the management of patients with Le Fort II and III fractures and the nose is cleared with a suction apparatus.
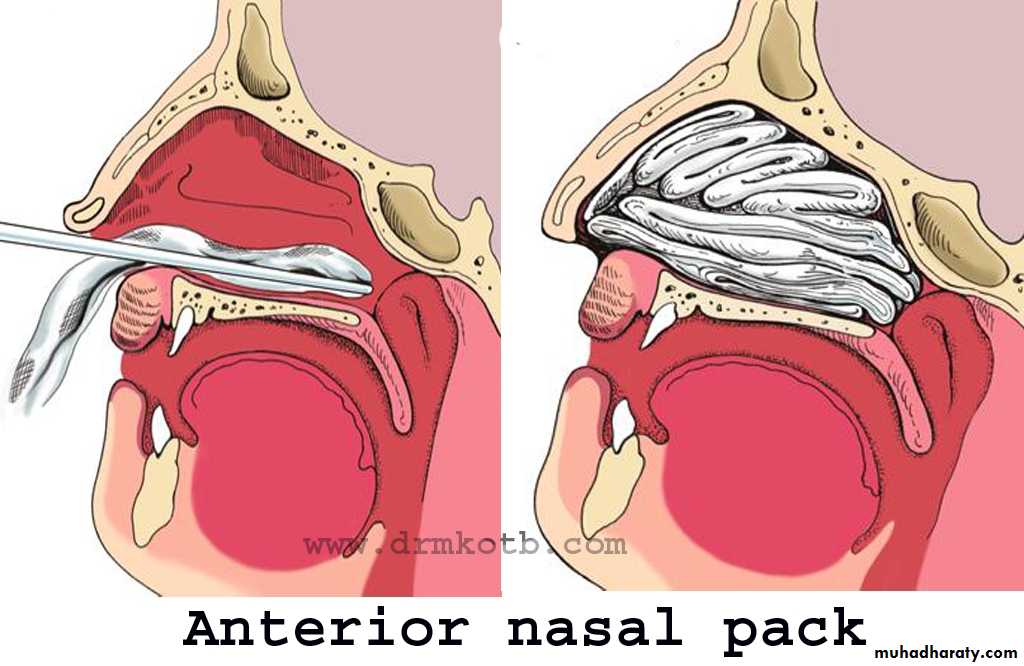
5) A resting nasal hemorrhage by anterior or posterior nasal packing for Le Fort II and III fractures and with severe injuries to the nasal complex in which the nares are blocked with blood clot or bleed profusely which cause occlusion of the nasal airway.
6) Back ward displacement of tongue due to bilateral fracture mandible.
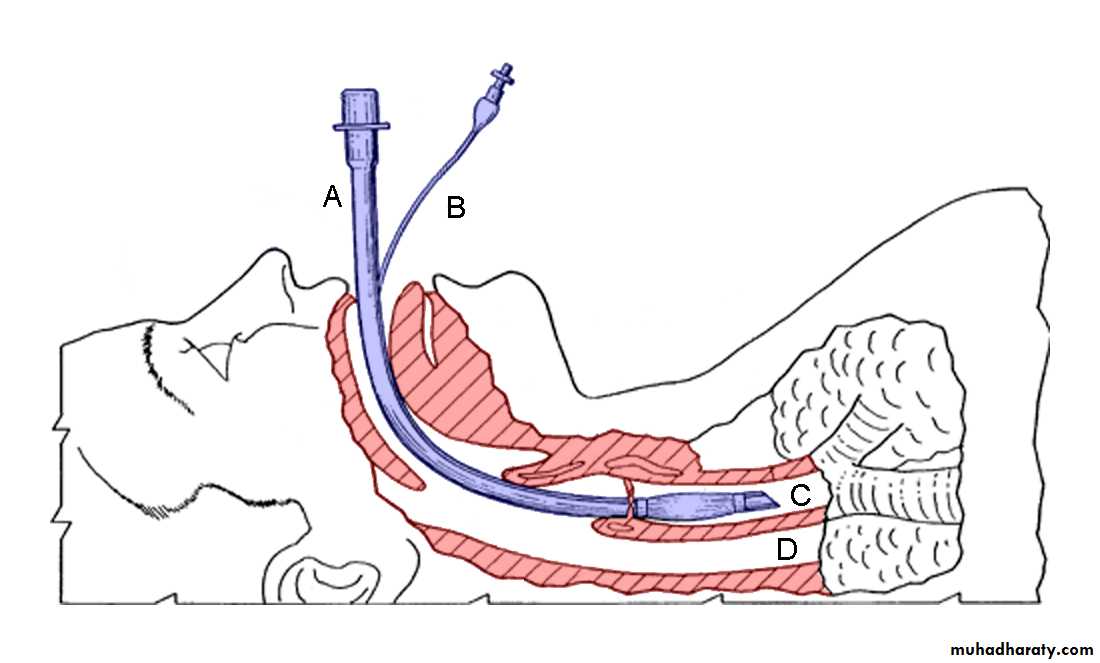
7) Continuous supervision is necessary either by the operator or by an experienced member of nursing staff. The lips should be coated with sterile petroleum jelly to prevent them from adhering together.8) Endotracheal Intubation may be required to ensure a patent airway in most patients with fractures of the middle third. The problems of airway maintenance are increased considerably in the unconscious Patient.
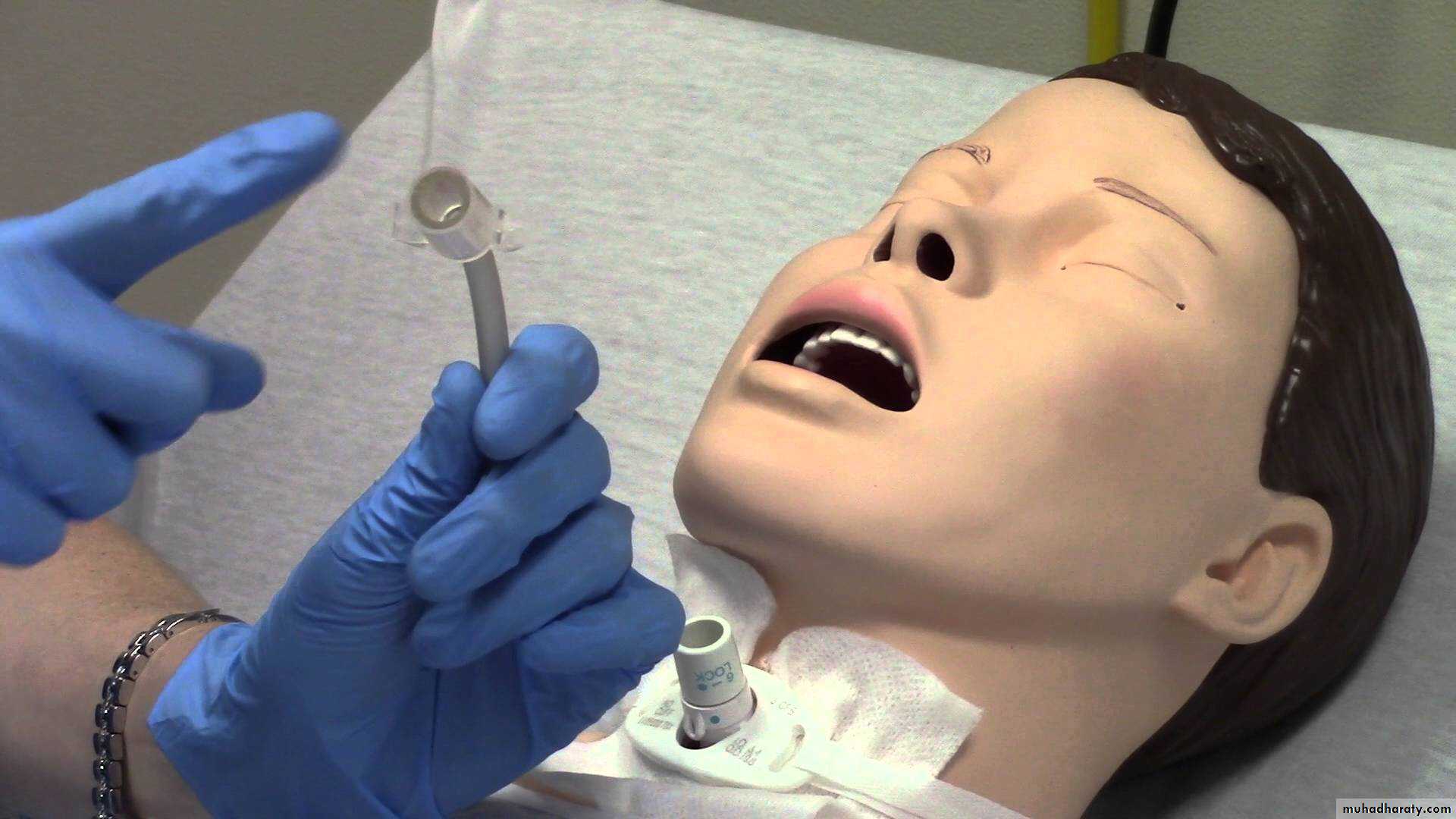
9) Tracheostomy: emergency incision into the trachea (tracheostomy) should never be necessary if effective medical skill is available, that is where an endotracheal tube can be passed. The indications for tracheostomy in maxillofacial injuries are:
• When prolonged artificial ventilation is necessary, e.g. some severeassociated head and chest injuries.
• To facilitate anesthesia for surgical repair in certain major injuries.
• To ensure a safe postoperative recovery after extensive reparativesurgery.
• Following obstruction of the airway from laryngeal edema oroccasionally direct injury to the base of the tongue and oropharynx..
• Serious hemorrhage into the airway particularly when further secondary hemorrhage is a possibility.
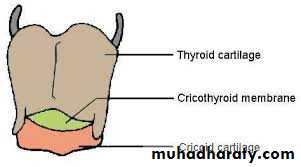
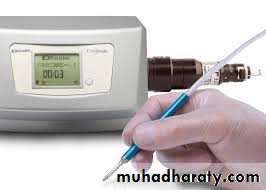
I. Surgical cricothyroidotomy is advocated through incision of the cricothyroid membrane. A slightly smaller size tracheostomy tube ie. Cuffed size (4 or 5) being maintained for 24 hours and replaced with tracheostomy. The complication is glottic and sub-glottis stenosis.2. Needle cricothyroidotomy by 12 G venflon with 10 ml syringe.
Hemorrhage:The majority of fractures of the facial skeleton are closed injuries, and in spite of the extensive nature of the skeletal damage, severe hemorrhage is unusual when there are extensive soft-tissue lacerations, particularly after missile injury, these require urgent attention as local blood loss can be considerable.
Control of hemorrhage:
Significant bleeding from external wounds, such as the scalp, can simply be controlled with pressure or any strong suture to hand. A continuous suture is both quick and effective. In the scalp, full thickness 'bites' are required to ensure the vessels are included in the layer. Obvious bleeding vessels should be secured with artery forceps, ligated if possible, and temporary pressure dressing applied.• Early intubation should again be considered, not only to protect theairway, but also to allow effective control of bleeding.
Epistaxis of some degree is an inevitable consequence of injury to the central middle third of the face.1- It is usually stops spontaneously or is easily controlled by lightlypacking the nose via the anterior nares 'anterior nasal pack.
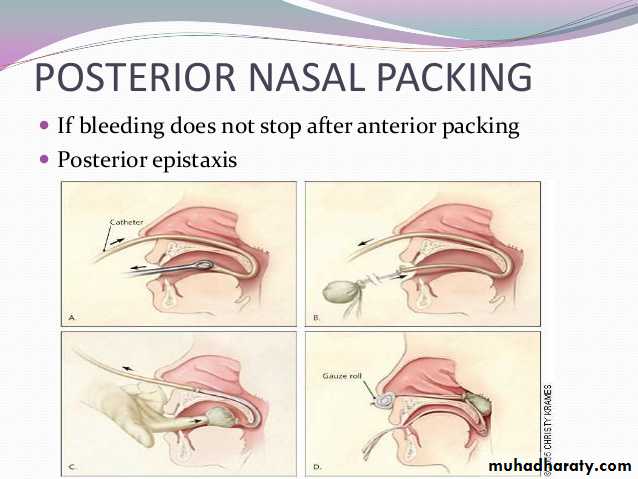
2- Profuse hemorrhage into the nasopharynx from terminal branches of the maxillary artery occurs on very rare occasions in association with Le Fort fractures. This may be life -threatening both from the point of view of actual blood loss and also obstruction of the airway. A postnasal pack is needed in this situation as a matter of extreme urgency.
How long packs are left in situ will depend on the clinical status of thepatient, but around 24-48 hours is usual. If hemorrhage persists despite these interventions it is important to consider coagulation abnormalities that can occur during prolonged resuscitation associated with major blood loss.
Ligation of external carotid artery and ethmoidal arteries via the neckand orbit respectively
(if bleeding continues despite all previous measures ) Endovascular radiological intervention (super selective embolization) is considered now as the preferred approach. It has been extensively reported as very Successful with clear advantages over surgery.
* Shock:Acute circulatory collapse is not usually a prominent feature of a fracture of the facial skeleton, and if such a patient is severely shocked the possibility of the coexistence of some other more serious injury should be suspected.
Surgical Hemostasis(choice of use depend on the site and nature of injury and hemorrhage)A. Mechanical procedures1. digital pressure
2. pressure packs (e.g. dry or wet swabs) 3. vascular hemostat (mosquito artery forceps)
4. clamps 5. ligatures (ligation e.g. trans-fixation suture for large arteries) 6. tourniquets 7. bone wax
B. Thermal agents1. Heating:1) Cautery :cause denaturation of proteins result in coagulation of large areas of tissue. Is either actual (conduct heat) or electrocautery (alternative current)2) Direct current (20-100 mA)3) High power argon-laser for superficial erosions
2. Cooling:1) Direct cooling (e.g. iced saline)2) Extreme cooling (cryogenic surgery) -20 to -180 C° cause cryogenic necrosis of small arterioles and venules (e.g. CO2 liquid-50 c, and Nitrogen liquid-150 to -180
3) Generalized hypothermia down to 35 C, this reduce blood flow to visceral organs but cause shivering and ventricular fibrillation.
C. Chemical agents1. Adrenaline & Noradrenaline2. Turpentine or Tannic acid (applied on gauze packs)3. Oxidized regenerated cellulose (Surgicel)4. Gelfoam (gelatin foam)5. Microcrystalline collagen6. Thrombin & Russell viper venom
PRELIMINARY EXAMINATIONThis is the secondary survey. After the operator has established a satisfactory airway and controlled hemorrhage, a full examination of the patient should be carried out (top-to-toe examination
Head InjuryThe cranium should be palpated and inspected for evidence of lacerations and bony damage and the level of consciousness determined.A simple scale of level of consciousness is:I. Fully conscious.II. Drowsy with disorientation, but responds rationally to questions and requests.III. Semiconscious responding irrationally to spoken questions and requests.IV. Unconscious but responding purposefully to painful stimuli.V. Unconscious with decerebration reflex response to pain.
The assessment of the patient's consciousness can be made by noting the patient's response using the simple A VPU scale:A. responds Appropriately (Awake)V. responds to Verbal stimuliP. responds to Painful stimuliU. doesn't respond (Unconscious)This coupled with an assessment of the pupil reaction, allows rapid assessment of the degree of head injury.
The Glasgow Coma Scale (GCS):Points are awarded using the criteria given in the scale to give a total score between (3 deeply unconscious and unresponsive) to (15 fully conscious, alert and oriented). Any patient with a GCS score of less than 8 should be considered as severe head injury unable to protect their airway (i.e. Below Eight Intubate). Those with a GCS score 9-12 are considered to have a moderate head injury and a GCS of 13-15 indicates a minor head injury.
Eyes
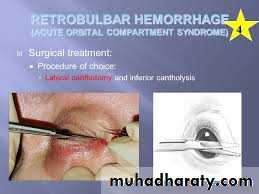
Any physical injury to the globe. Vision, pupil size and reaction to light should be recorded.Signs and symptoms of orbital Compartment Syndrome (Retrobulbar 0edema) or Retro bulbar haemorrhage
Treatment o (compartment syndrome:
medical with Mannitol I gm/kgacetazolamide 250-500 mg to - reduce intra-ocular pressure
3-4 mg/kg i.v. dexamethasone to reduce edema &vascular spasm), while Retro bulbar hemorrhage- require evacuation through lateral canthotomy as emergency before surgery), Irreversible ischemia of the visual pathway can occur within 1 hour, and permanent visual loss (blindness) within 1 -1/2- 2 hours.
Sign and symptoms of compartment syndrome:
1. Pain (increasing)2. Decreasing visual acuity3. Diplopia with developing ophthalmoplegia (paralysis of ocular muscles)4. Proptosis5. Tense globe6. Subconjunctival oedema /chemosis7. Dilated pupil and pale optic disc8. Loss of direct light reflex (relative afferent pupillary defect)The spineIt should be assumed that any significant maxillofacial injury may be associated with a cervical spine injury. Care, therefore must be taken when the head and neck are manipulated during maintenance of the airway, examination and radiology. A lateral view of the cervical spine showing all cervical vertebrae must be examined and if there is a high index of suspicion, then cervical anteroposterior and open mouth odontoid views should also be taken. Confirmation of a cervical spine injury may require simple tomography or computed tomography (CT) scanning.
The limbsRapid palpation of the limbs for deformity or bony tenderness should preceed the recording of reflexes. Abdomen and chest Examination by inspection and palpation will determine whether there is a possibility of visceral injury or fracture of the chest wall or pelvis. The first urine specimen should be examined for the presence of blood. The operator will by this time have enough information to call for any assistant he may require from other specialties.
Soft Tissue LacerationSoft tissue facial injuries fall into three main groups:1. Hematomas.2. Simple lacerations.3. Lacerations involving specialized structures or organs.
Stepwise options for the Primary management of traumatic tissue loss1. Immediate replacement of avulsed tissue as a free graft.2. Dress wound and allow to heal by secondary intention.3. Direct closure under an acceptable degree of tension.4. Partial or full thickness skin graft.5. Immediate reconstruction with a free composite graft (e.g. some nasal defects).6. Local or regional flap.7. Avulsion of scalp/ear/ nose: consider replantation using microsurgical techniques.
HISTORY AND LOCAL EXAMINATIONHistory of the injury and description of the patient's symptoms :1. If the patient is unconscious or confused, any relevant facts concerning the accident and the subsequent management of the patient must be obtained from eye-witnesses, ambulance men, or medical and dental practitioners who may have attended the patient following the injury.2. If the patient is conscious and co-operative a history can be obtained, but as patients with facial injury may experience some difficulty in talking owing to the pain and mobility of the fractures the interrogation should be brief at this stage.
3. It is prudent to ask if loss of consciousness has occurred and, in thatevent, whether the patient can remember up to the moment of theaccident or whether there is a memory gap. Retrograde amnesia is failure to remember up to the time of injury and anterograde amnesia is loss of memory following the accident, both are indicative of cerebral damage.4. It is also important to inquire whether the patient has any difficulty in breathing or swallowing and whether he has a headache or pain elsewhere in the body.5. Information as to whether the patient was being treated with insulin, steroid , or anticoagulant prior to the accident is also most important.
Local Clinical Examination of the Facial injury
washing by warm waterinspection Eternally. oedema. ecchymosis, and soft-tissue lacerations., Any obvious bony deformitie haemorrhage, or cercbrospinal fluid leak should be recorded.
Palpation. Gentle palpation
Inspection Intra-orally.
CONTROL OF PAINthere is surprisingly little pain from maxillofacial injuries. It is extremely important to avoid giving powerful analgesics which:1) Depress the level of o consciousness and respiration.
2) Morphine also depresses the couch reflex and so encourage theaspiration of blood into the trachea.3) It causes constriction of the pupil (miosis), which may mask an early sign of the rise in intracranial pressure (as in cerebral hemorthage).4) Masks pain which may be due to intra-abdominal or intra-thoracic1njuries.
It is, however, most important to minimize discomfort in the early stages after injury, as a patient is readily exhausted by efforts both to keep his airway clear and to obtain nourishment. Local toilet, support of mobile fractures, posture, and availability of suction and administration of intravenous fluids are all of great importance in the early care of the patient. The most useful drug for sedation in such cases is Diazepam (Valium) given intravenously. Only about 10mg are usually necessary and this drug may be combined with 15-30mg of Pentazocine (Fortral) as an analgesic.