D. Usama Surgery
Fifth Stage
1
Pleural Disorders L2
Pleural Effusion
Pleural effusion is accumulation of fluid in the pleural space.
Pathophysiology:
Passage of protein free fluid through the pleural membrane depends on hydrostatic and colloid
oncotic pressure across the pleura
Therefore protein free fluid normally flows from the systemic capillaries in the parietal pleura
into the pleural space then to the pulmonary capillaries in the visceral pleura
5-10 L of fluid normally traverse the pleural space over 24 hours. And normally only 15-20 ml of
pleural fluid is present in the pleural space at any given time
Mechanism of abnormal accumulation of pleural fluid:
Increased hydrostatic pressure e.g.; CHF
Decreased plasma oncotic pressure e.g.; hypoalbuminemia
Increased capillary permeability e.g.; pneumonia, inflammatory pleuritis
Increase intrapleural negative pressure e.g.; atelactasis
Impaired lymphatic drainage owing to obstruction of the lymphatics by tumor,
irradiation or fungal infection.
So any disturbance between fluid formation and absorption → pleural effusion
Pleural effusion are divided into transudate and exudate.
Transudative pleural effusion:
Protein poor ultrafiltrate of plasma occurs when there is:
Increase in systemic or pulmonary capillary hydrostatic pressure
Decrease in plasma osmotic pressure
Causes of transudative pleural effusion:
1.
CHF
: most common, 80% of patients with transudate have CHF. CXR → cardiomegally
and bilateral. 75% resolve within 48 hours with the use of diuretics
2. Hypoalbuminemia
3. Liver cirrhosis
4. Renal insufficiency and nephritic syndrome
5. Myxedema
6. Peritoneal dialysis
D. Usama Surgery
Fifth Stage
2
7.
Meig's syndrome
: pleural effusion plus ascitis and ovarian fibroma. It may be transudate
or exudate.
8. Sarcoidosis
Exudative pleural effusion:
Protein rich pleural fluid
Pleural effusion of one or more of the following is considered an exudate:
1. Pleural fluid protein / serum protein > 0.5
2. Pleural fluid LDH / serum LDH > 0.6
3. pH < 7.0
Causes:
1. Neoplastic disease: Lung cancer,Breast cancer, Mesothelioma, Chest wall tumors
2. Infections: Bacterial pneumonia,TB,Fungal, Paracytic
3. Pulmonary infarction
4. Collagen vascular disease: Rheumatoid arthritis,SLE
5. Trauma and hemothorax
6. Gastrointestinal disease: Pancreatitis,Esophageal rupture,Subphrinic abscess
7. Cardiac disease: Post CABG,Pericardial disease
8. Obstetric and gynecological disease: Meig's syndrome,Post partum pleural
effusion,Endometriosis
9. Drug induced: Ergot alkaloids ,Amiodarone
Clinical presentation:
Symptoms:
Asymptomatic
or symptomatic with dyspnea and pleuretic chest pain
Signs:
Inspection: decreased chest wall movement on the affected side
Palpation: Tracheal and mediastinal shift to the contralateral side -
Decreased chest expansion - Decreased vocal fremitus
Percussion: Decrease resonance (stony dullness)
Auscultation: Decrease or absent breath sounds
Diagnosis
1- CXR: concave meniscus sign.About 250-500 ml of fluid must be present to obliterate the
costodiaphragmatic recess
D. Usama Surgery
Fifth Stage
3
2- Pleural fluid analysis
A. Volume :massive effusion seen in(Malignant , CHF&TB)
B. Color:
Straw (pale) color→ mostly transudate
Cloudy → mostly exudate due to high WBC
Yellow → chronic empyema
Milky fluid → chylothorax
Black pleural fluid → aspergillosis
Brownish → rupture of amebic liver abscess into the pleural space
Bloody → Trauma. Pulmonary infarction &Malignancy
C. Glucose : in the pleural fluid is less than serum in: TB ,Empyema &Ca
D. pH: low pH < 7.2 suggest effusion contaminated with bacteria
3- Pleural biopsy
4- Ultrasound
5- CT scan: to detect small abnormalities
6- Bronchoscopy
7- VATS
8- Sputum examination
Management of pleural effusion
1- Treatment of the underlying cause
2- Thoracocentesis
3- Tube thoracostomy + chemical pleurodesis
4- Surgical pleurodesis and pleurectomy
5- Radiotherapy
6- Pleuro-peritoneal shunt
Hemothorax
Presence of blood in the pleural space.
Causes:
I-Traumatic
II-Spontaneous: It is due to:
a. Pulmonary: Necrotizing infection,Pulmonary embolism ,TB, Arterio-venous
malformation
b. Pleural: Torn pleural adhesions,Neoplasm,Endometriosis
c. Neoplasm: Primary neoplasms or Metastatic
d. Blood dyscrasia: Thrombocytopenia ,Hemophilia

D. Usama Surgery
Fifth Stage
4
Clinical presentation
Dyspnea ,chest pain &Syncope
Treatment:
Management of hemothorax depends on:
Rate of bleeding
Amount of bleeding
Underlying cause
Small bleeding usually ceases spontaneously so that only observation is required
Moderate (amount of blood loss is 500 cc or more): thoracostomy.
Continuing active bleeding (200 ml/hr or more):
Open thoracotomy.
VATS
Indications for thoracotomy in hemothorax:
1- Initial chest tube output more than 1500 ml
2- Continuous bleeding 200-300 ml/hr for 3 consecutive hours
3- Retained clot
Chylothorax
The presence of lymph in the pleural cavity
Etiology
I-Trauma
A. Blunt trauma:Sudden hyperextension
B. Penetrating trauma to thoracic duct
C. Surgery: like LN excision
D. Diagnostic procedures : Left central venous line
E. Exaggerated physiological maneuvers:
Vomiting episodes or violent coughing especially after the duct is distended after a fatty meal
can lead to spontaneous chylothorax
II -Neoplasm: Lymphangioma, Lymphosarcoma
III- Infection: TB, Filariasis
IV- Congenital: Thoracic duct atresia, Birth trauma

D. Usama Surgery
Fifth Stage
5
Clinical picture:
Chest pain dyspnea and fatigue
Prolonged leakage lead to
Dehydration
Malnutrition
Decrease immunity
Diagnosis:
1. Aspiration of milky white odorless fluid from the pleural space is virtually diagnostic
Characteristics of chyle
Milky
Alkaline and odorless
Triglyceride (TG) > 110 mg/dl
Cholesterol/TG < 1
2. Lymphangiography
Treatment
1. Tube Thoracostomy
2. Correction of
a. Fluid loss
b. Electrolyte imbalance
c. Nutritional support: TPN and avoid long chain fatty acids
3. Surgical opeative : failure of previous measures after 2 weeks thoracotomy or VATS
(Pleurectomy or Pleuro-peritoneal shunt)
D. Usama Surgery
Fifth Stage
6
Clinical presentation
Asymptomatic or Symptomatic
Dyspnea
Pain
On examination:
Small pneumothorax may have no abnormal finding
Inspection: dyspnea ± cyanosis
decrease or absence chest wall movement
Palpation: Trachea shifted to the other side,Decreased chest wall expansion,Decreased or absent
tactile vocal fremitus
Percussion: hyperresonance (tympanic)
Auscultation: decrease or absent breath sounds
Investigation:
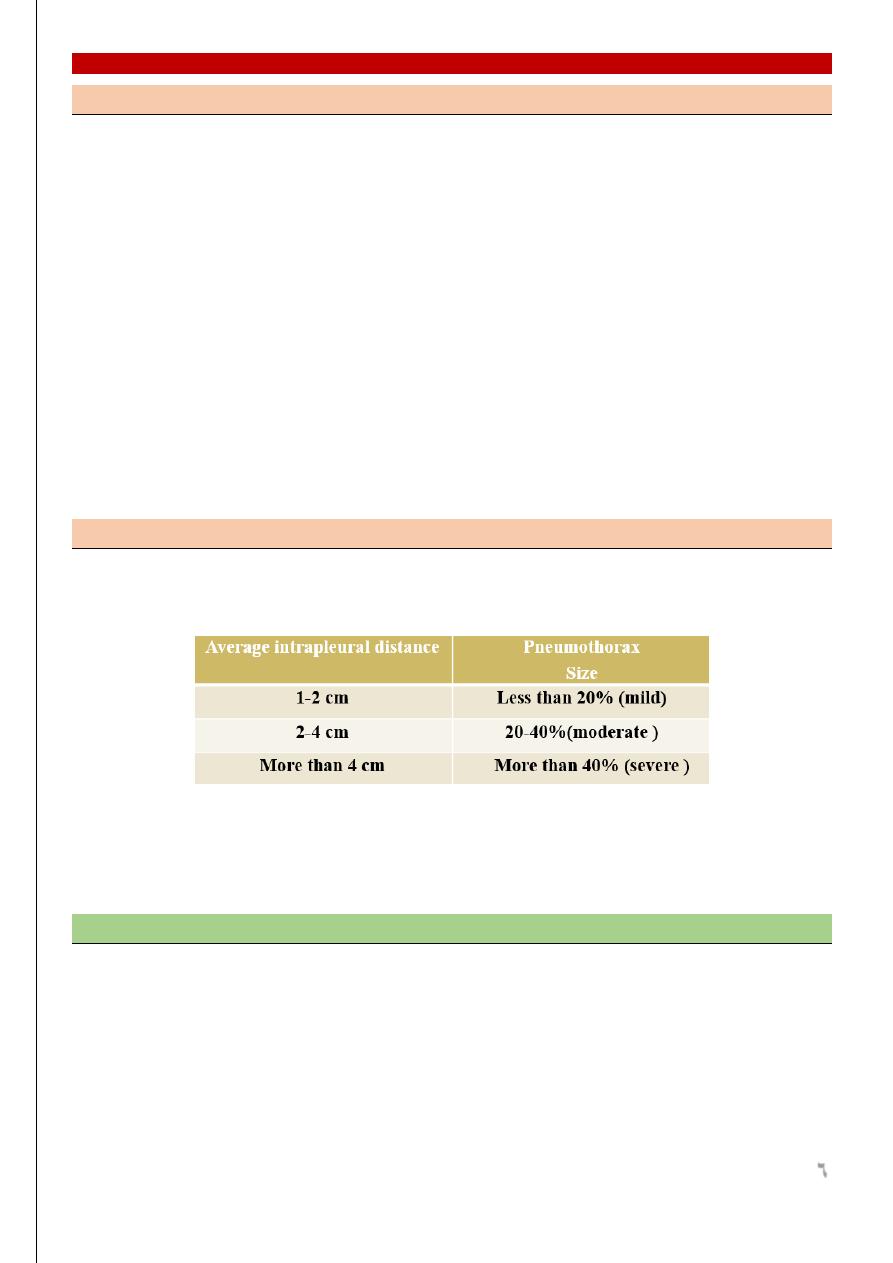
1- CXR: Standard PA view in deep inspiration
Rhea method
2- CT scan
3- Arterial blood gas analysis
4- Pulmonary function test
5- Bronchoscopy
Management
1- Observation: for vey mild or trivial cases
2- Thoracocentesis: for minimum one
3- Chest tube ± suction for moderate cases
4- Chemical pleurodesis via chest tube for recurent pneumothorax
5- Thoracotomy or VATS with blebectomy and pleural ablation or pleurectomy
D. Usama Surgery
Fifth Stage
7
Indication for thoracotomy in pneumothorax
1- Massive air leak that prevent lung expansion
2- Recurrent same side pneumothorax
3- Previous contralateral pneumothorax
4- Bilateral simultaneous pneumothorax
5- Presence of large cyst on CXR or bullae
6- History of previous tension pneumothorax
7- History of Previous pneumonectomy
Mubark A. Wilkins
