Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 6
P a g e
1
Brain tumors
Glioma:
•
Typically appears as a solitary, irregular mass, surrounded by oedema
•
Compression or displacement of the ventricles
•
The CT attenuation values of the tumour itself are usually low, but may be high or
mixed.
•
Some, particularly the low grade tumours, may be very densely calcified.
•
Partial enhancement with intravenous contrast medium, sometimes only the outer
portion enhances, giving a so called ring enhancement pattern.
•
AT MRI, same as for CT. The essential features are a mass, often with adjacent
oedema.
•
Calcification is less evident than in MRI.
In general, the tumour is lower in signal intensity than the normal brain on the T1-
weighted images and higher in signal intensity on the T2-weighted images.
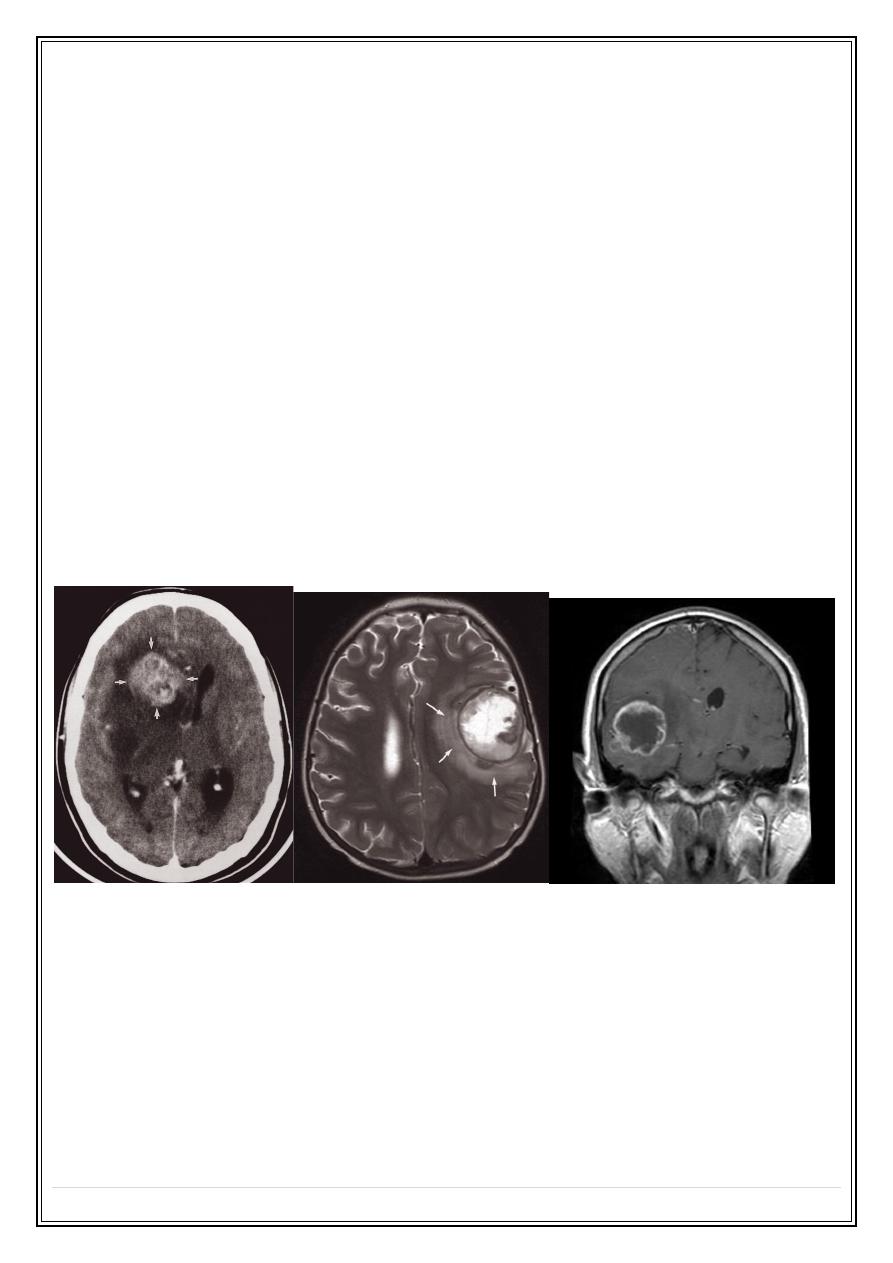
Brain metastasis
Metastases in the brain may be of high, iso, or low density
• They usually show contrast enhancement (ring enhancement(
• They are often surrounded by significant oedema
• Metastases are typically multiple.
• A solitary metastasis is indistinguishable from a primary intracerebral brain
tumour.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 6
P a g e
2
Meningioma:
•
Arise from the meninges of the vault, falx, or tentorium (extra-axial)
•
Characteristic sites, the commonest being the parasagittal region, over the
cerebral convexities, and the sphenoid ridges
•
Unenhanced CT scan, a meningioma is slightly denser than the brain
•
The tumour shows marked enhancement post contrast injection
•
Sclerosis and thickening of the adjacent bone.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 6
P a g e
3
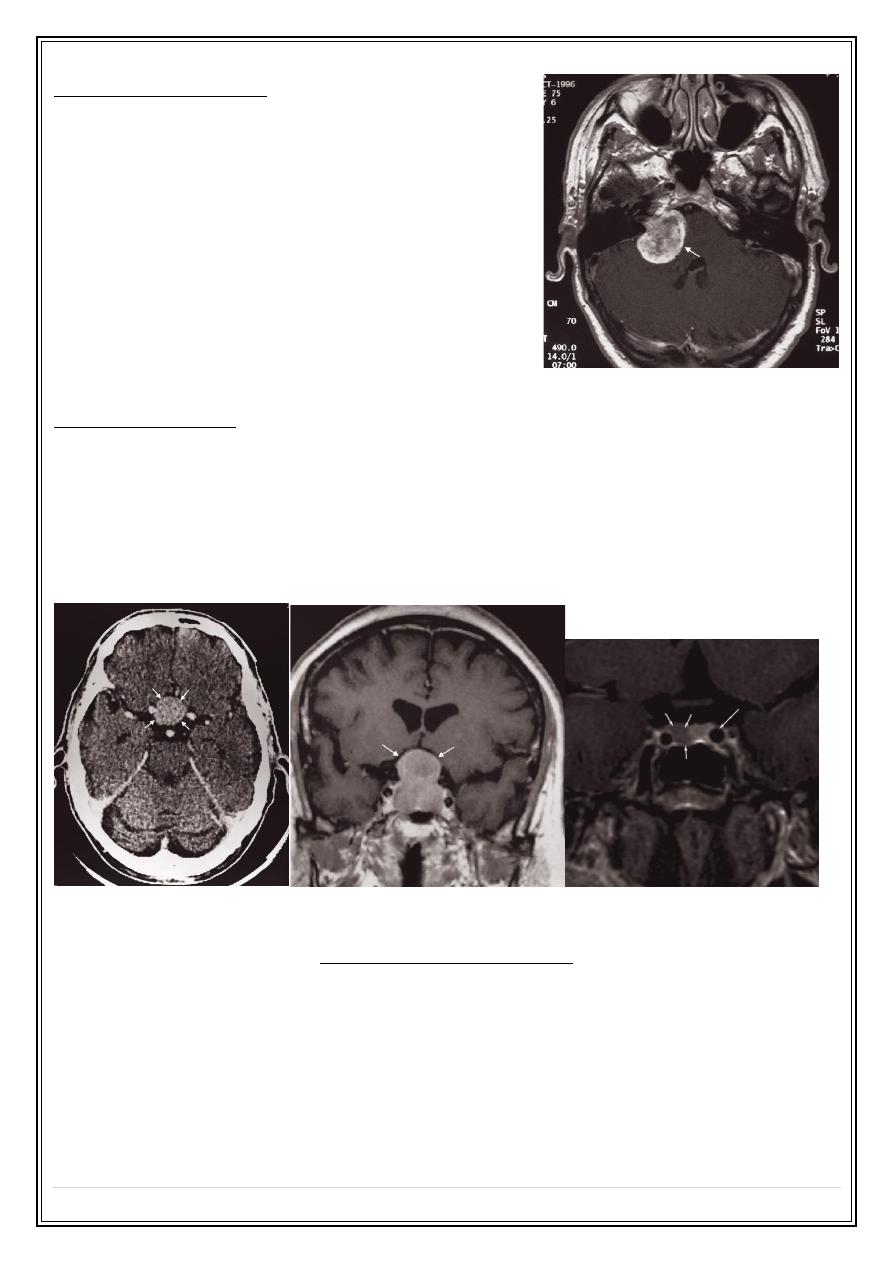
Acoustic neuroma:
•
Neurofibromas of the acoustic nerve arise in
the internal auditory canal or immediately
adjacent to the internal auditory meatus in the
cerebellopontine angle.
•
When large, they can be recognized at CT or
MRI. When small, they may only be identifiable
with MRI.
•
Contrast enhancement improves their visibility
with either technique
Pituitary tumours:
•
Divided into macroadenomas (>1 cm), and microadenomas (<1 cm).
•
Large tumours may cause enlargement of the pituitary fossa.
•
Computed tomography can show a pituitary tumour , but MRI is the investigation
of choice and can readily demonstrate its relationship to the optic chiasm and
optic nerves and can show very small tumours
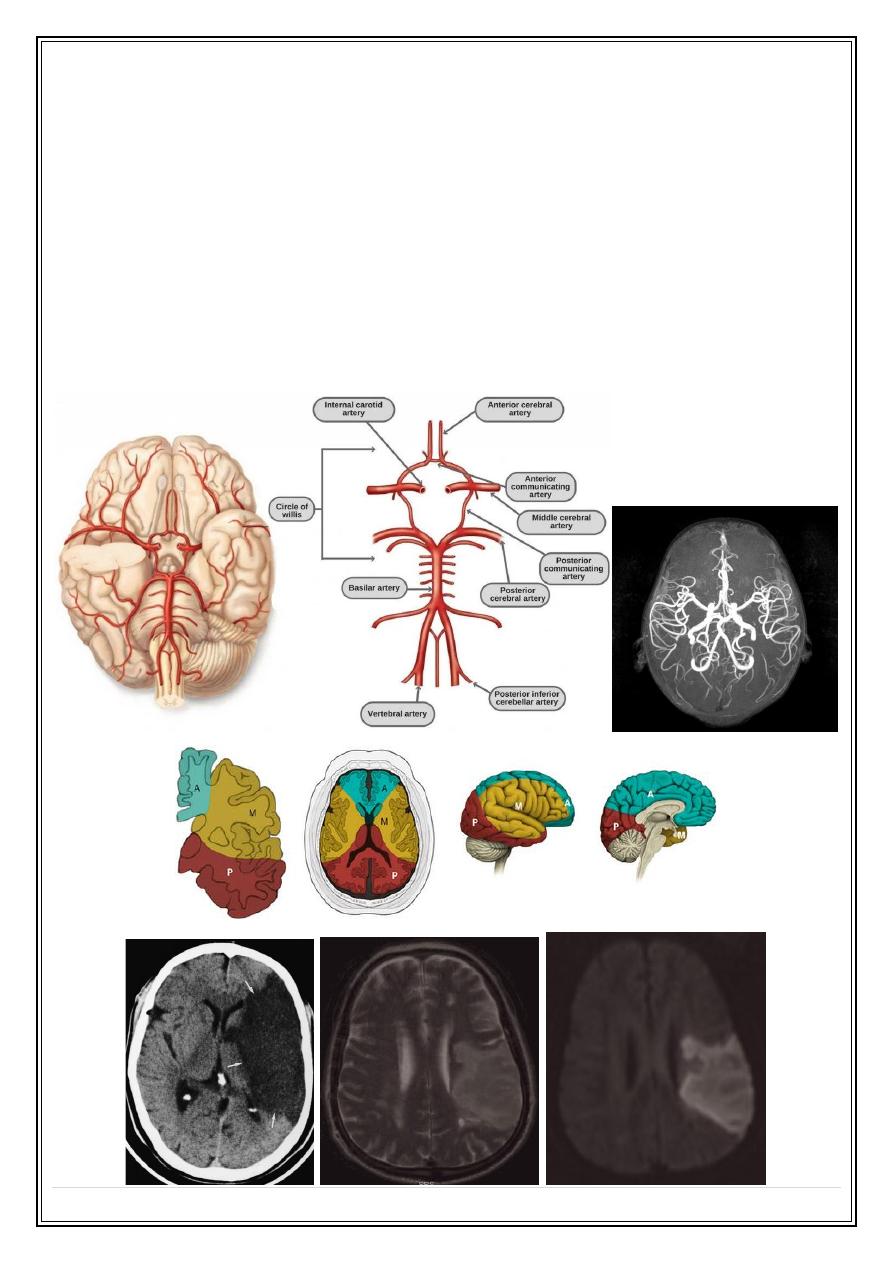
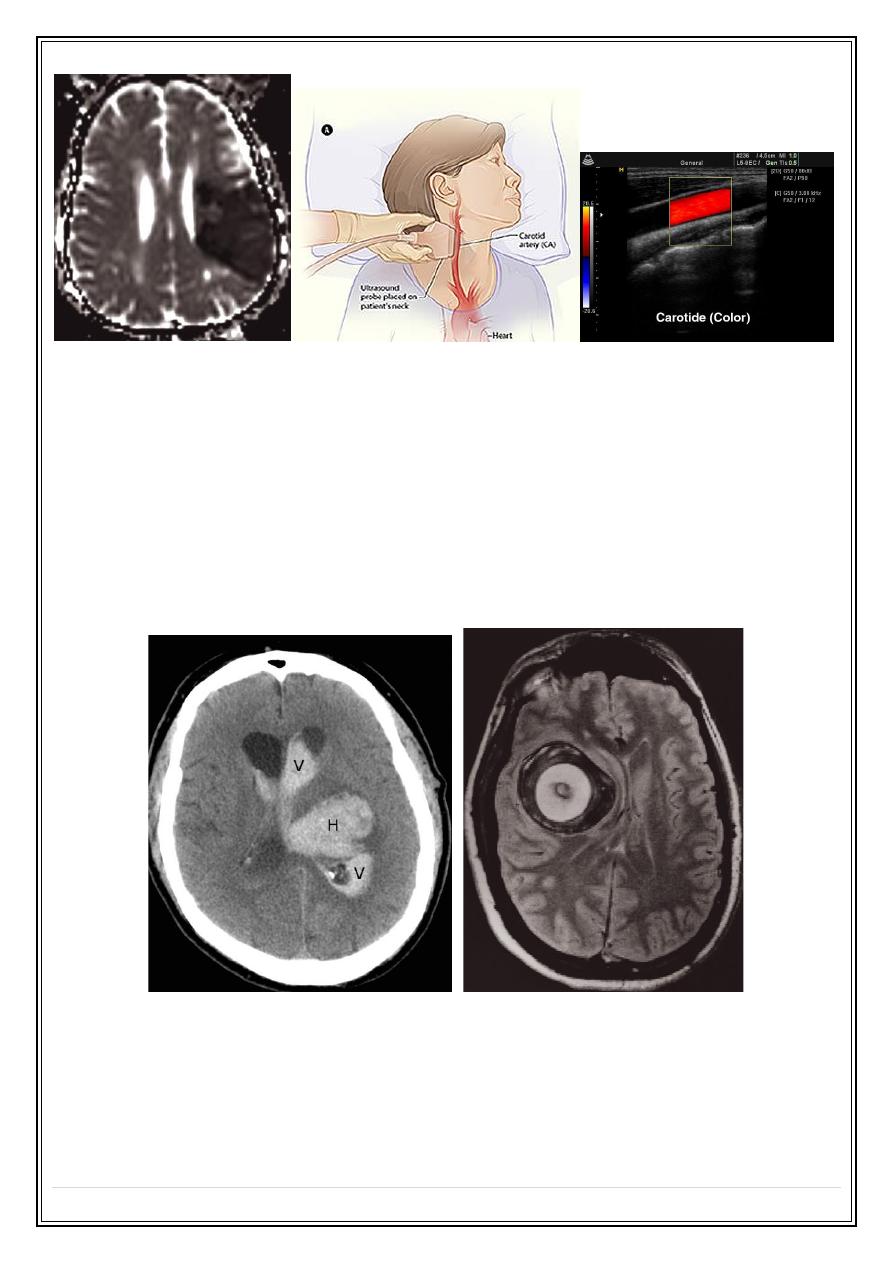
Cerebral infarction:
Changes of acute infarction are not usually recognized on CT before 6 hours
•
Over the next few days the infarct evolves into a low attenuation area conforming
to the shape of a recognizable arterial distribution
•
The infarct may gradually resolve, leaving an atrophic area and/or a persistent
scar
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 6
P a g e
4
•
MRI scanning : hyperintense areas on a T2-weighted scan, within 8 hours of the
onset of symptoms. Special fast scanning techniques such as perfusion / diffusion
scans show changes within minutes of the onset of symptoms.
•
Patients whose symptoms resolve within 24 hours are referred to as having a
transient ischaemic attack (TIA). A common cause for a TIA is embolus from an
atheromatous stenosis of the internal carotid artery. The presence of
atheromatous plaque and degree of stenosis can be assessed with Doppler
ultrasound of the neck. Ultrasound can also demonstrate a dissection of the
carotid artery in the neck.
•
The cerebral vessels may be imaged non-invasively with MR angiography (MRA).
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 6
P a g e
5
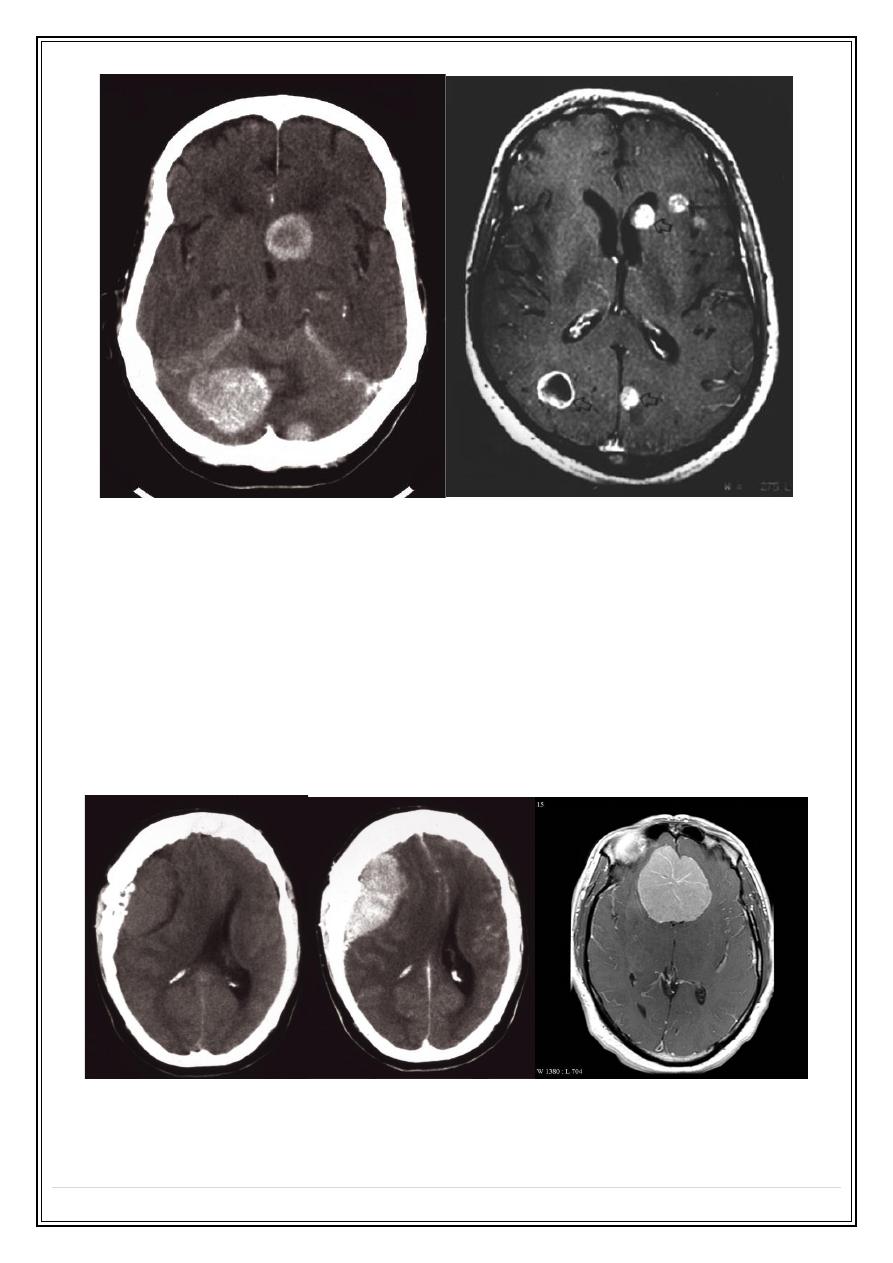
Cerebral haemorrhage:
•
Haemorrhage is demonstrable on CT immediately after the event as a region of
high attenuation
•
Frequently causing mass effect.
•
The initial high density of haemorrhage lessens over the following week or two
leaving a low- density area indistinguishable from an infarct.
•
May be associated with intraventricular or subarachnoid bleeding
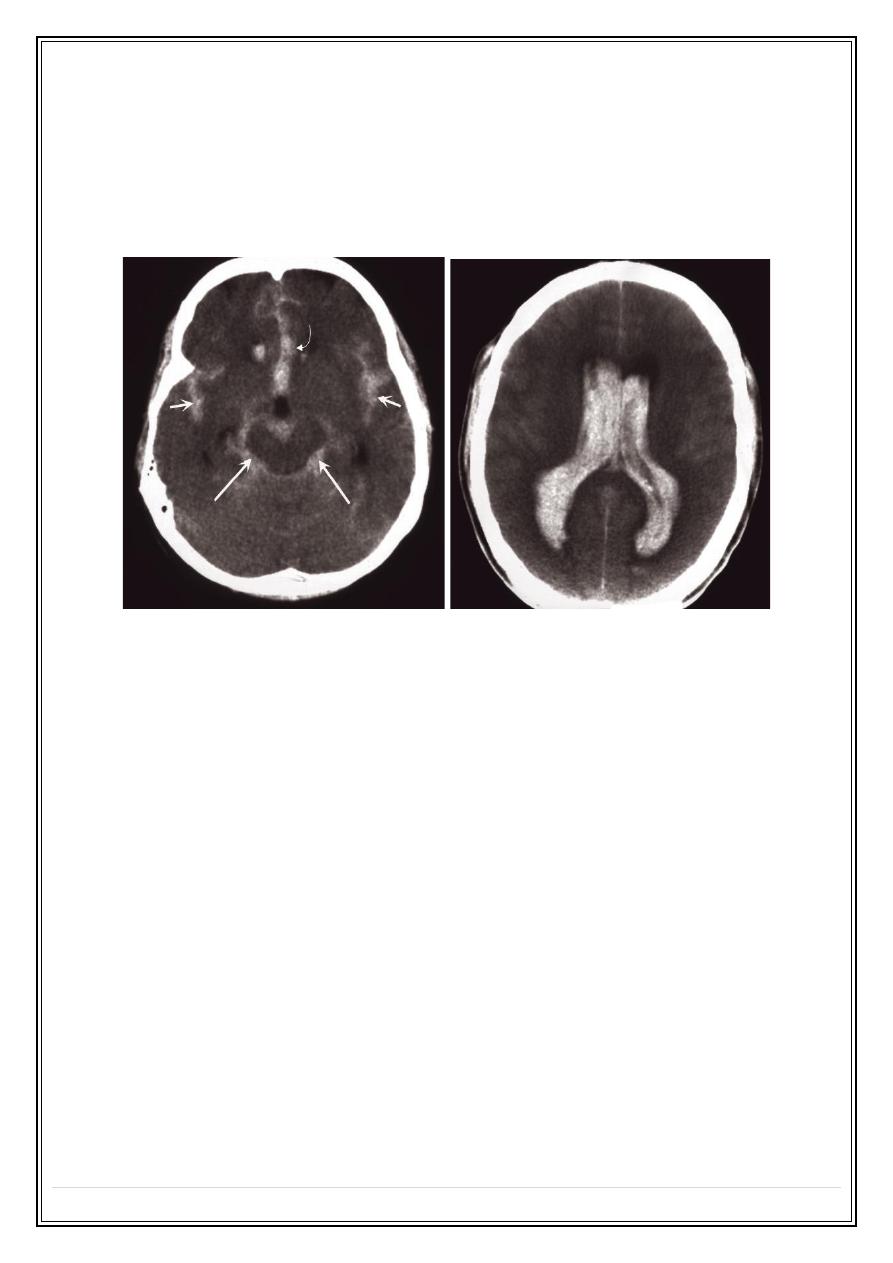
Subarachnoid haemorrhage
•
Usually due to a ruptured intracranial aneurysm or less commonly an
arteriovenous malformation.
•
CT is the best initial investigation to diagnose.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 6
P a g e
6
•
A subarachnoid haemorrhage is recognized by high density blood in the cortical
sulci, Sylvian fissures and basal cisterns.
•
CT will also show any intracerebral haemorrhage or blood in the ventricles
•
An unenhanced routine head CT is followed by CT angiography as a single
investigation to diagnose subarachnoid haemorrhage, localize the bleeding and
demonstrate the aneurysm.
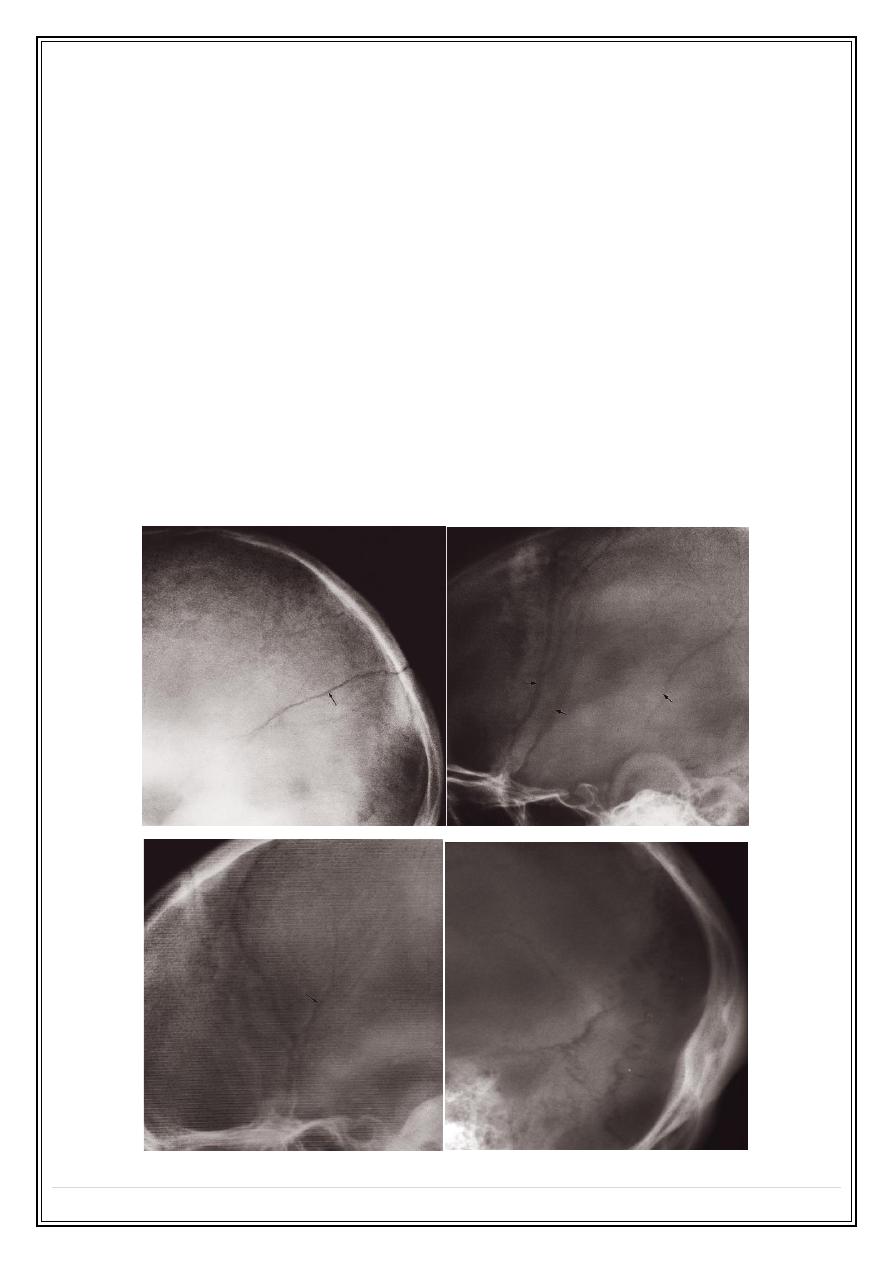
Head injury
•
Computed tomography is performed without intravenous contrast administration
•
brain and bone window.
•
Computed tomography can distinguish between extracerebral and intracerebral
lesions
•
CT can also demonstrate fluid levels in the sinuses and mastoid air cells
suggesting a facial or skull base fracture, air in the orbits and in severe head
injury, air in the cranial cavity.
•
Examination on bone windows can demonstrate fractures of the skull vault, face
or skull base.
•
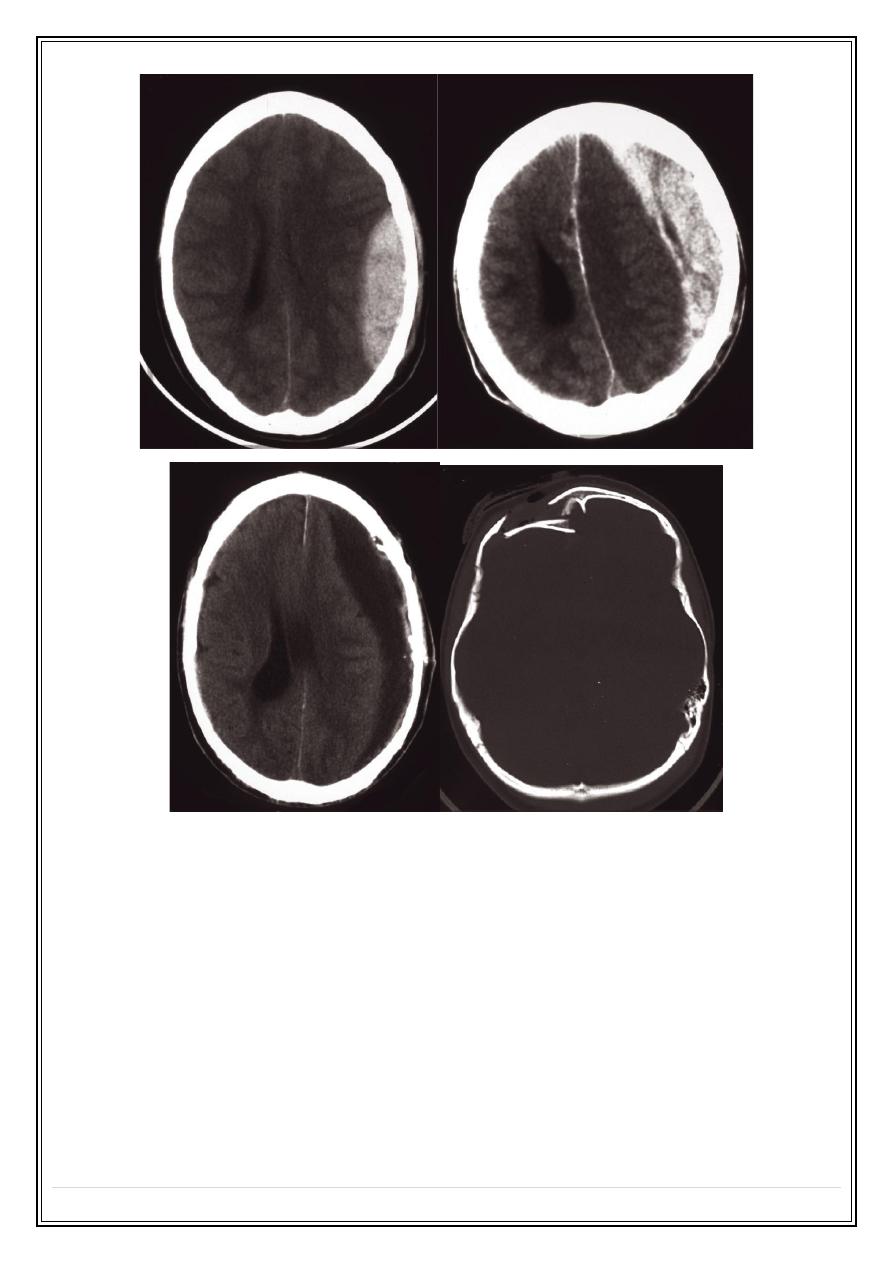
Extracerebral haematomas show a high density for about 1–2 weeks following the
injury, but after 3–4 weeks the density decreases to become lower than that of the
brain. In the intervening period, haematomas pass through a phase of being
isodense with the brain
•
Causes Midline or ventricular displacement.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 6
P a g e
7
•
Extradural haematoma is seen as a lens-shaped, smoothly demarcated, high-
density area situated over the surface of the hemisphere associated with a skull
fracture
•
Subdural haematoma conforms to the shape of the underlying brain (lenticular
shape) and occurs most commonly over the convexity of the brain, but can also
arise along the falx and tentorium
•
Contusions are bruises of the brain which appear as areas of low attenuation and
may be associated with high-density areas due to haemorrhage.
•
Intracerebral haematomas are seen as areas of high density, which may be
multifocal. There may be mass effect causing displacement of the ventricles and
accompanying brain oedema.
•
Fractures of the skull base or vault should be looked for on bone window settings.
•
Assessment of fracture type: linear or depressed . Also assessment of Paranasal
sinuses, sphenoid, petrous and occipital bones
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 6
P a g e
8
Infection
•
In acute meningitis CT and MRI are usually normal.
•
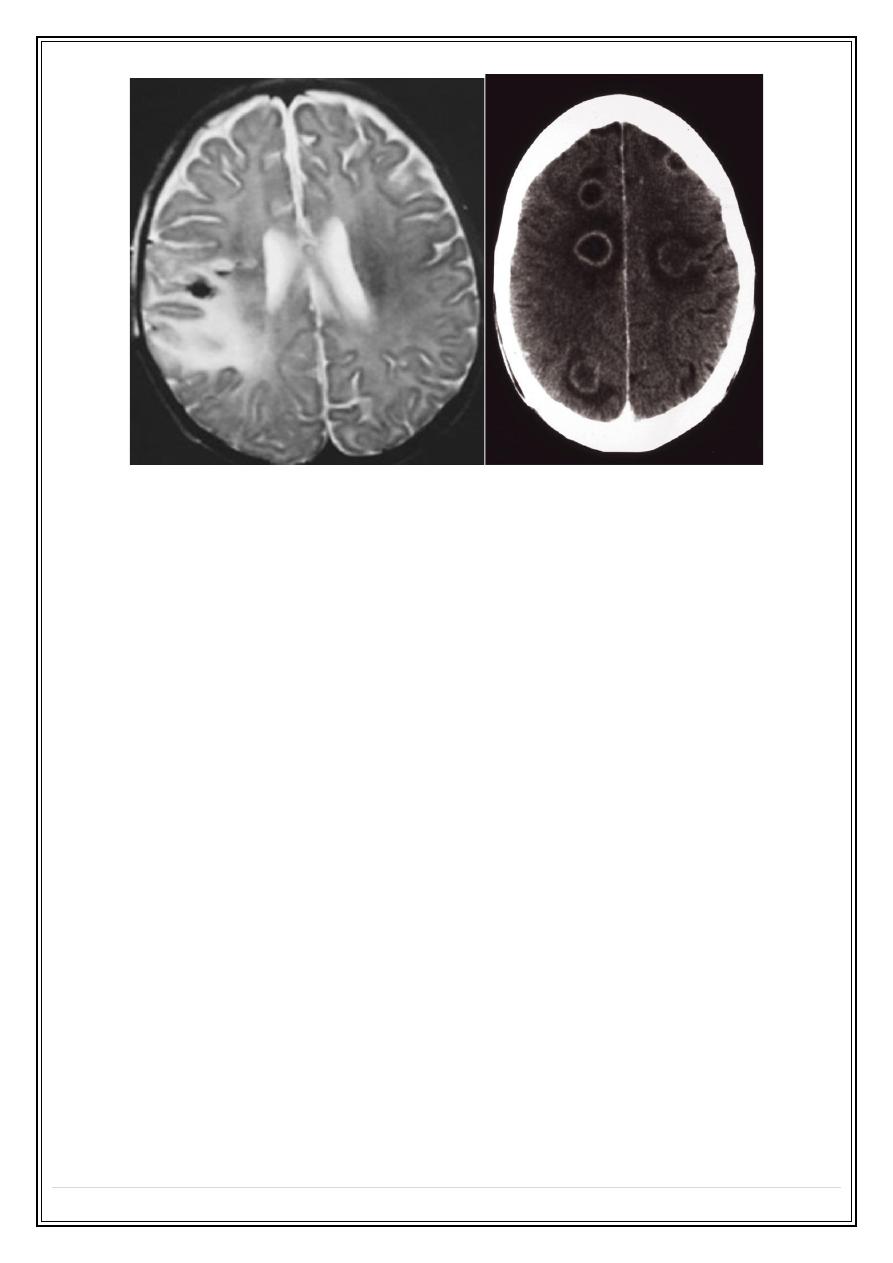
Encephalitis is caused by infection, usually viral or by an immune reaction to
infection. CT and MRI show unilateral or bilateral focal abnormal areas, often in a
characteristic distribution appearing as low attenuation on CT and high signal on a
T2-weighted MRI scan
•
An abscess can be caused by pyogenic, tuberculous, fungal or parasitic
organisms. Necrosis and pus formation occur in the center of the abscess, which
appears as low density on CT. The wall of the abscess enhances with intravenous
contrast and may be surrounded by oedema giving an appearance known as ring
enhancement
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 6
P a g e
9
Enecephalitis
abscess
Tha nk
y ou, , ,
