Cholera
د
-
هديل فاضل
فرهود

1- identification: an acute bacterial eneric disease
characterized by (in its severe form) sudden onset,
profuse painless watery stool, nausea & vomiting early
in the course of illness & in untreated cases rapid
dehydration, acidosis, circulatory collapse,
hypoglycemia in children & renal failure.
In sever untreated cases death may occur within few
hours, & the case fatality rate may exceed 50% , with
proper treatment the rate is less 1%.

•
Cholera is essentially the only diarrheal
disease where patients can become severely
dehydrated in less than six hours. No one who
arrives at a treatment center and is still
breathing should die of cholera.

• Case classification
•
1- Suspected case: Any case complains of
acute watery diarrhea without pain, +/-
vomiting, regardless of patient age.
•
2- Probable case: Any suspected case with
severe dehydration, or death due to acute
watery diarrhea.
•
3-Confirmed case: A suspected case with
isolation of Vibrio cholera O1 or O139 from
stools.
•
4- Carrier: Asymptomatic person Vibrio
cholera isolated from his or her stool

Diagnosis: by isolation vibrio cholera of a sero group
O1 or O139 from feces.
2- infectious agent: vibrio cholerae sero group O1
includes 2 biotypes ( classical & EI Tor) . V. cholerae
O139 also cases typical cholera.
3-resorviour : human
4- mode of transmission: this occur through:
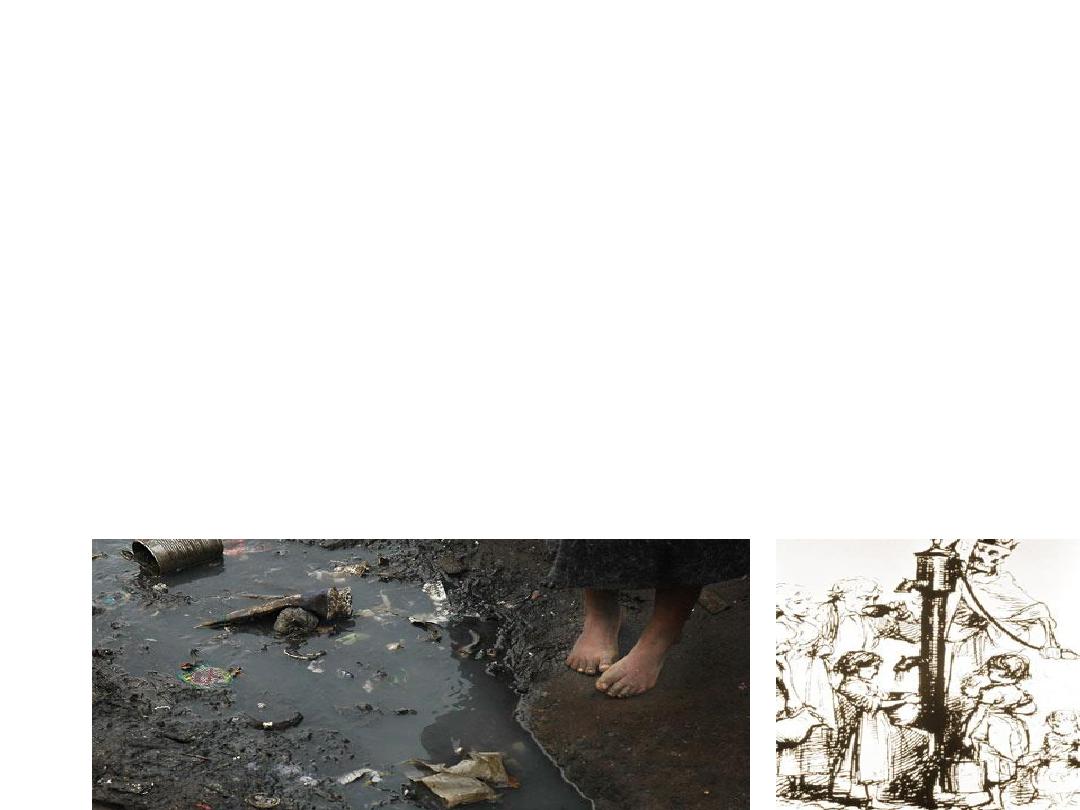
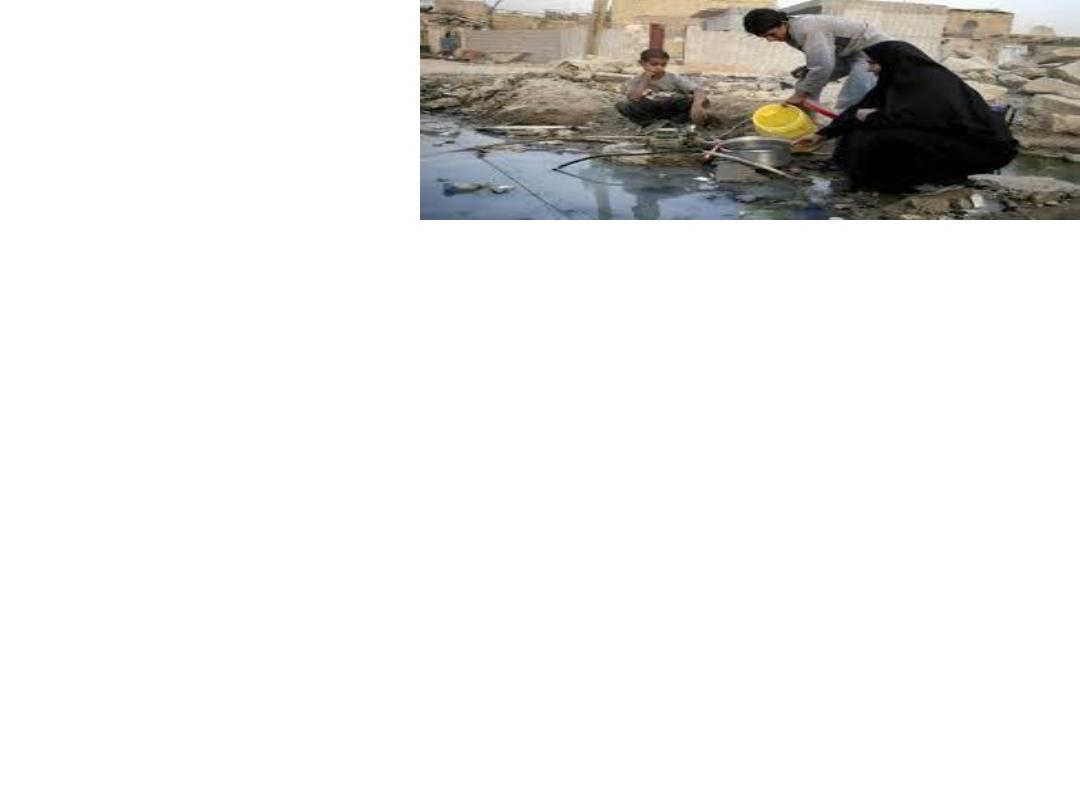
**ingestion of food or water contaminated directly or
indirectly with feces or vomitus of infected person..
EI Tor & O139 organisms can persist in water for long periods
*The cholera toxin is primarily responsible for fluid loss..
**contaminated surface water & unsafe domestic
water storage methods resulting in extensive water
borne transmission of cholera
**vegetable & fruits freshened with untreated sewage
water have also as a vehicle of transmission. Out
breaks or epidemics as well as sporadic cases are
often attributed to raw or under cocked sea foods.
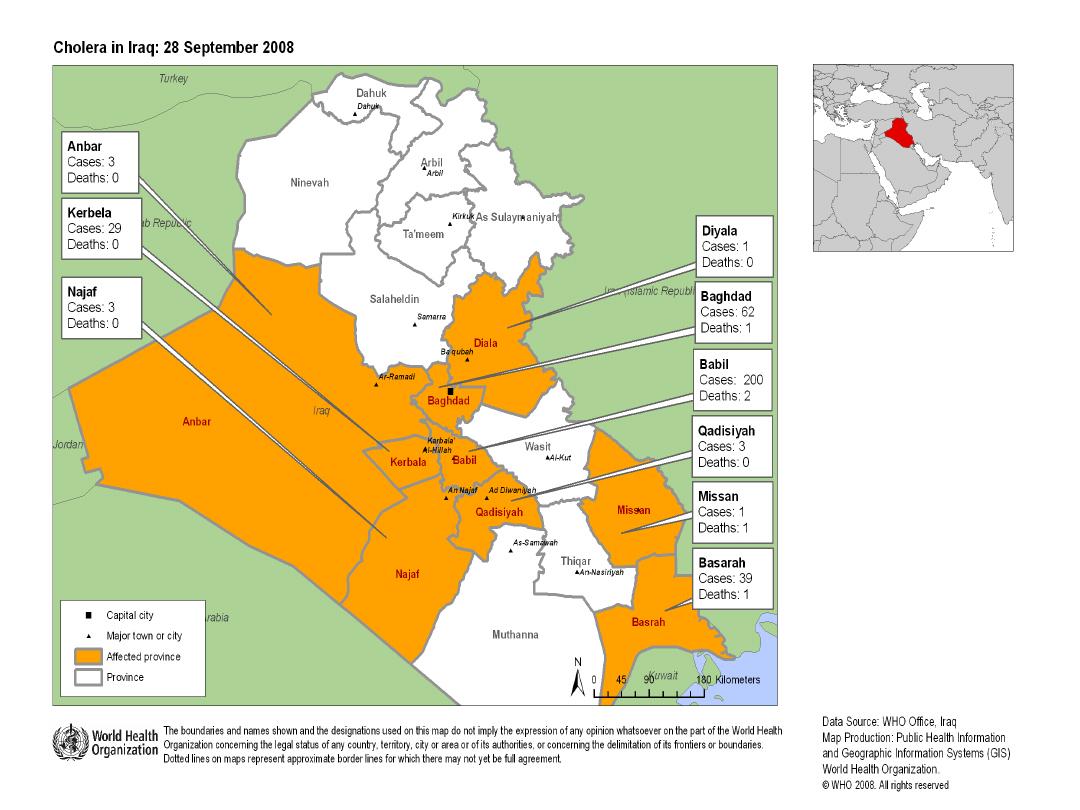
Occurrence
•
Cholera is one of the oldest and best-
understood epidemic diseases. Epidemics and
pandemics are strongly linked to the
consumption of unsafe water and food, poor
hygiene, poor sanitation and crowded living
conditions.
•
4- incubation period: from a few hours to 5 days,
usually 2-3 days.
•
5- period of communicability: as long as stools are
positive, usually only a few days after recovery.
Occasionally the carrier state may persist for several
months.

Susceptibility and resistance
• Variable; gastric achlorhydria increases the
risk of illness, and breastfed infants are
protected. Severe cholera occurs significantly
more often among persons with blood group
O. Infection with either V.cholera O1 or O139
results in a rise in agglutinating and antitoxic
antibodies, and increased resistance to
• re-infection.

7- methods of control:
A- preventive measures:
1- health education to public regarding the importance of hand
washing after defecation & before eating or serving & carrying
food for food handler & attendants.
2- dispose of human feces in a sanitary matter & maintain fly
proof latrines
3- protect, purify & chlorinate public water supply.

•
4- control flies by screening, spraying with
insecticide & use of insecticidal baits & traps
5- cleanliness in food preparation & handling,
refrigerate as appropriate. Particular attention
should be directed to the proper storage of
salads & other foods served cold.
6- pasteurize or boil all milk & diary products.
7- enforced suitable quality-control procedures
in industries that prepare food & drink for
human consumption
.

8- active immunization with current killed whole
cell vaccine given parentally is of little practical
value in endemic control or management of
contacts to cases. These vaccine shown to
provide partial protection (50%) of short
duration (3-6 months) in highly endemic areas &
do not prevent asymptomatic infection, they are
not recommended.

•
Two oral vaccine that provide significant protection
for several months against cholera caused by O1
strain
9- measures that inhibit or otherwise compromise
the movement of people, foods or other goods are
not justified.
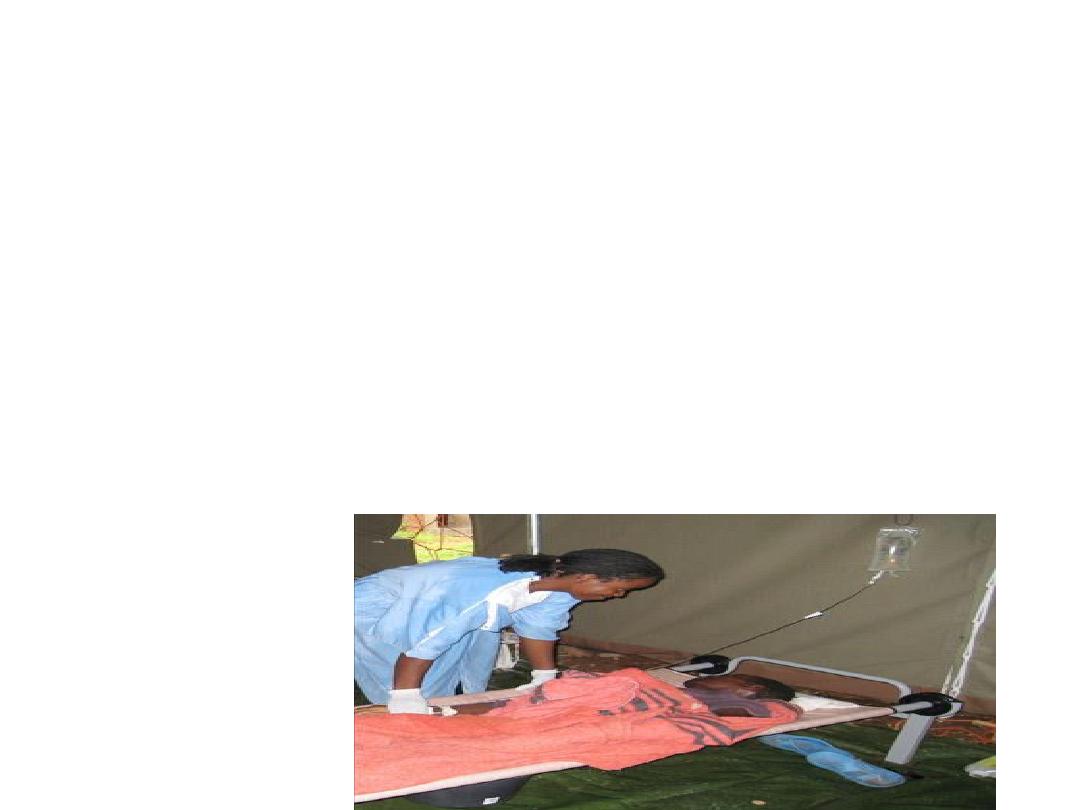
B- control of patients, contact & immediate environment:
1- report to local health authority: obligatory (within 24 hours)
(Immediate Notification Diseases)
2- isolation: hospitalization with enteric precaution for severely
ill patients. Fly control should be practiced
3- concurrent disinfection: of feces & vomitus & of linens &
articles use by patients , by heat or other disinfectant.
4- quarantine: none

5- management of contact: tetracycline(500 mg four times
daily) or doxycyclin (a single daily dose of 300 mg for 3 days).
6- investigation of contact & source of infection: investigate
possibilities of infection from polluted drinking water&
contaminated food. Meal history for the 5 days prior to onset
should be interviewed
7- a search by stool culture for unreported cases is
recommended only among household members or those
exposed to possible common source in a previously an infected
area.
8- specific treatment
a- aggressive rehydration therapy
b- give effective antibiotic
c- treatment of complication

• Data analysis: Routine weekly and monthly
reporting of aggregate data is recommended
from peripheral level to intermediate and
central levels. Immediate notification for every
case to local health authority is required. Zero
reporting is mandatory when there is no case.
C- epidemic measures:
1- educate the population at risk concerning the need to
seek appropriate treatment without delay
2- provide effective treatment facilities
3- adopt emergency measures to ensure a save water
supply. Chlorinate public water supply, even if the
source water appears to be uncontaminated. Chlorinate
or boil water used for drinking, cocking & washing
dishes & food container unless the water supply is
adequately chlorinated & subsequently protected from
contamination

•
4- ensure careful preparation & supervision of food & drink.
After cocking or boiling , protect against contamination by flies &
unsanitary handling
5- investigation designed to find the vehicle & circumstances
(time, place, person) of transmission, & plan control measure
accordingly
6- save facilities for sewage disposal
7- parenteral whole cell vaccine is not recommended.
•
Thank you
