LEISHMANIASIS
Dr. Ameer kadhim Hussein
M.B.Ch.B. FICMS (Community Medicine)
Leishmaniasis is one of the most important vector-borne diseases
of humans. This parasitic disease can be caused by many species of
Leishmania (over 20 Leishmania species), most of which are
zoonotic.
In humans, different species of the parasite are associated with
different forms of the disease.
Many Leishmania spp. cause skin ulcers and nodules. A few of
these organisms can also affect the mucous membranes, and may
cause disfiguring lesions of the nose.
Introduction

Other species damage the internal organs and
cause human visceral leishmaniasis which is a
life-threatening condition.
Among domesticated animals dogs are the
most important species in the epidemiology of
this disease.
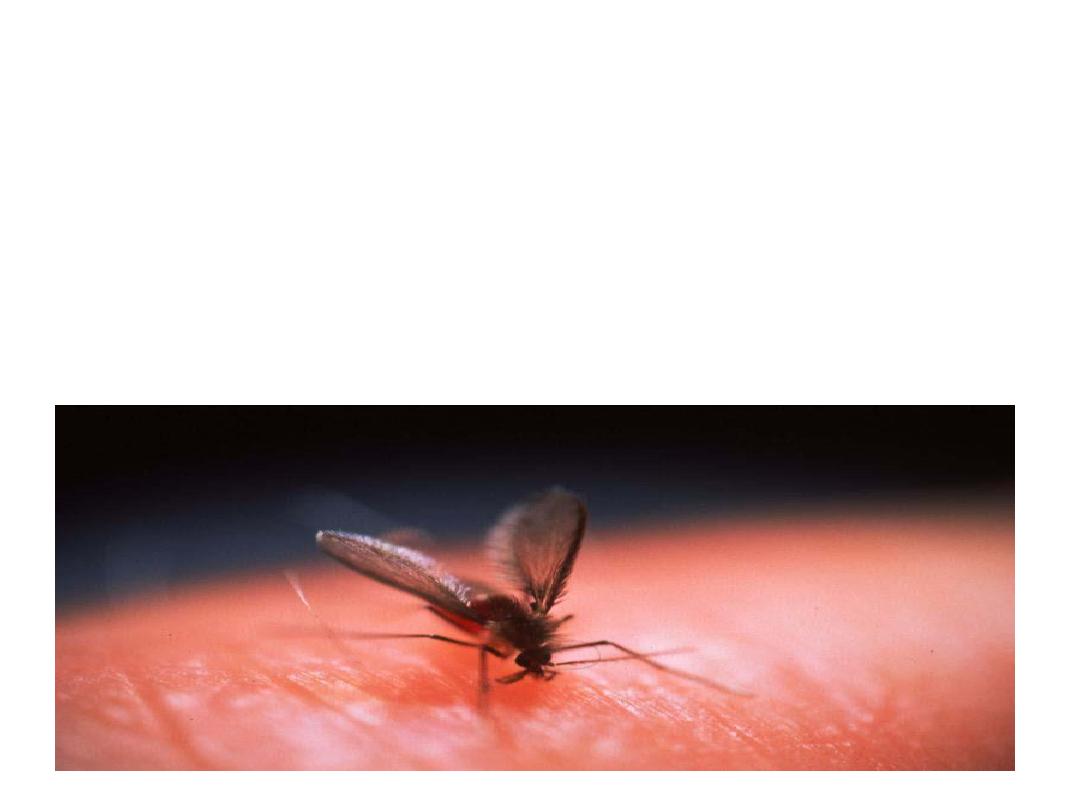
Leishmania transmitted to humans by the bite
of infected female phlebotomine sandflies.
Over 90 sandfly species are known to
transmit Leishmania parasites.
Types
There are 3 main forms of the
disease:
a. Cutaneous Leishmaniasis.
b. Mucocutaneous Leishmaniasis.
c. Visceral Leishmaniasis.
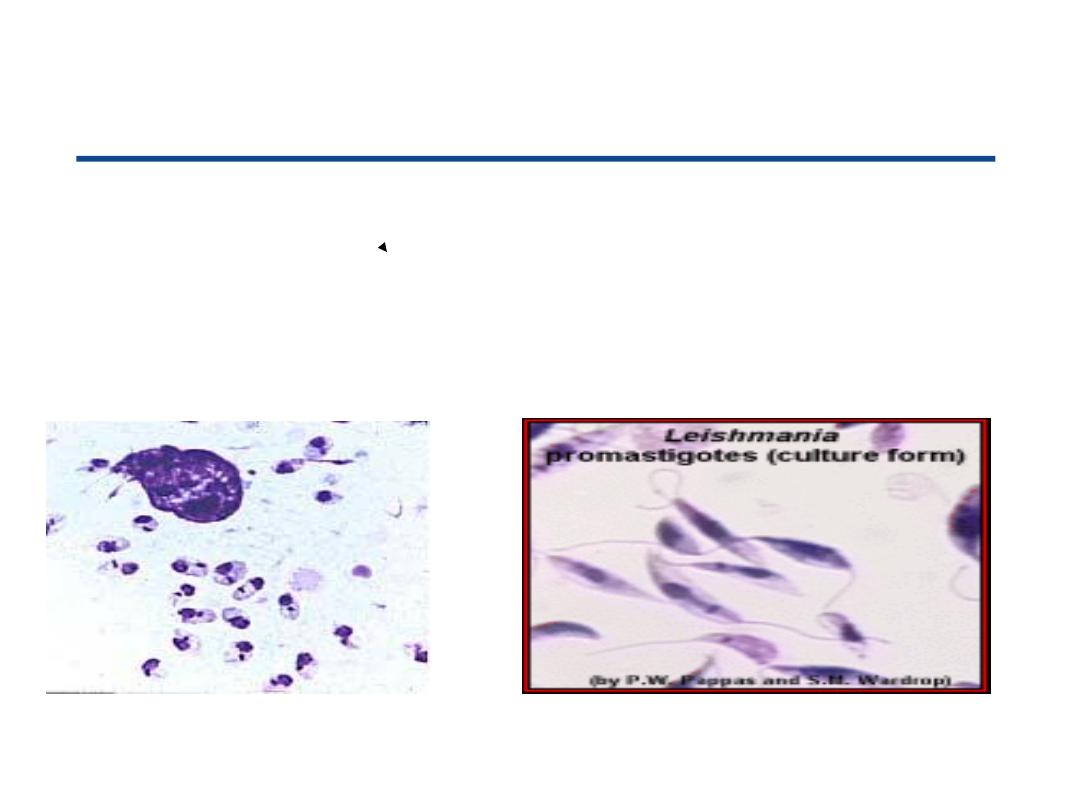
parasites
leishmania
Morphology of
in vertebrate hosts in sandfly vectors
Amastigote Promastigote
(Leishman body). (Leptomonad).

Sand fly
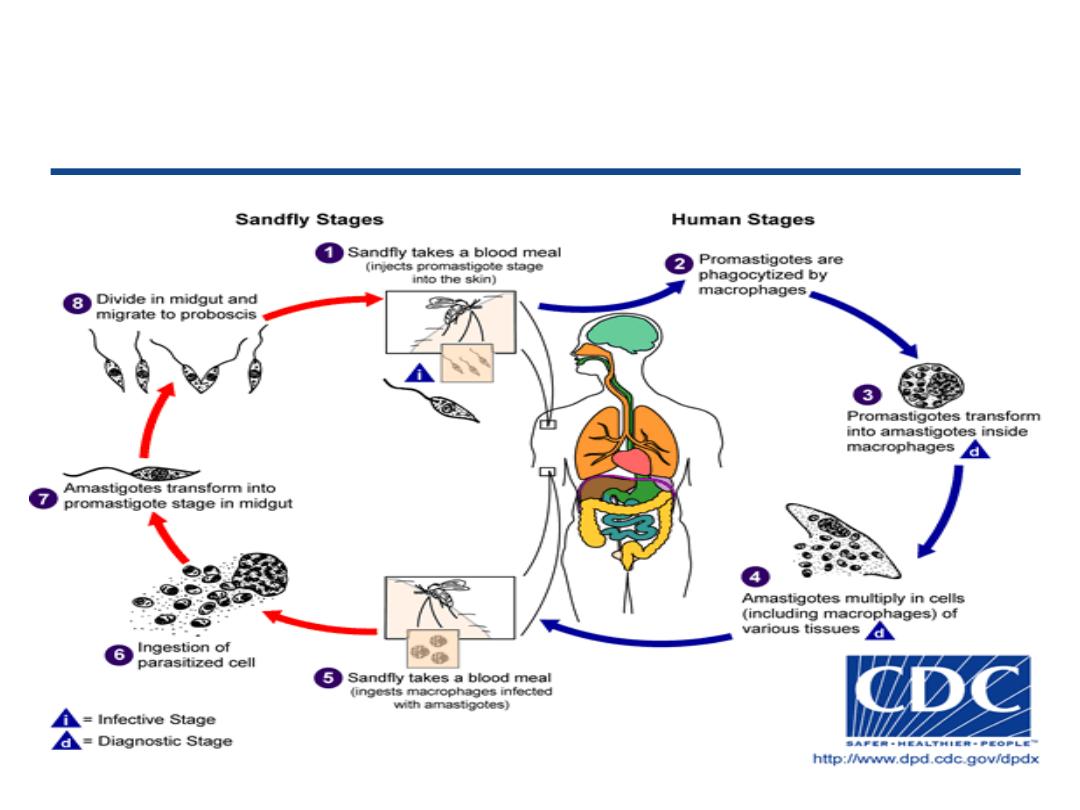
Leishmania
Life cycle of species of
Leishmaniasis
Visceral
Identification:
It is chronic systemic disease caused by intracellular protozoa of the
genus leishmania. The disease is characterized by fever, Hepato-
splenomegaly, lymphadenopathy, anemia, leukopenia,
thromboocytopenia and progrssive emaciation and weakness.
Untreated clinical disease is usually fatal.
Post kala-azar dermal leishmaniasis consist of macular, papular
and/or nodular skin lesions that occur weeks to years after
apparent cure of systemic disease. Post kala-azar dermal
leishmaniasis occur in about 50% of visceral L. in Sudan and in 10-
20% of cases in India.

Visceral Leishmaniasis
Girl suffering from visceral leishmaniasis – a potentially fatal condition, if
untreated - with markers showing signs of liver and spleen enlargement.
(Ethiopia).
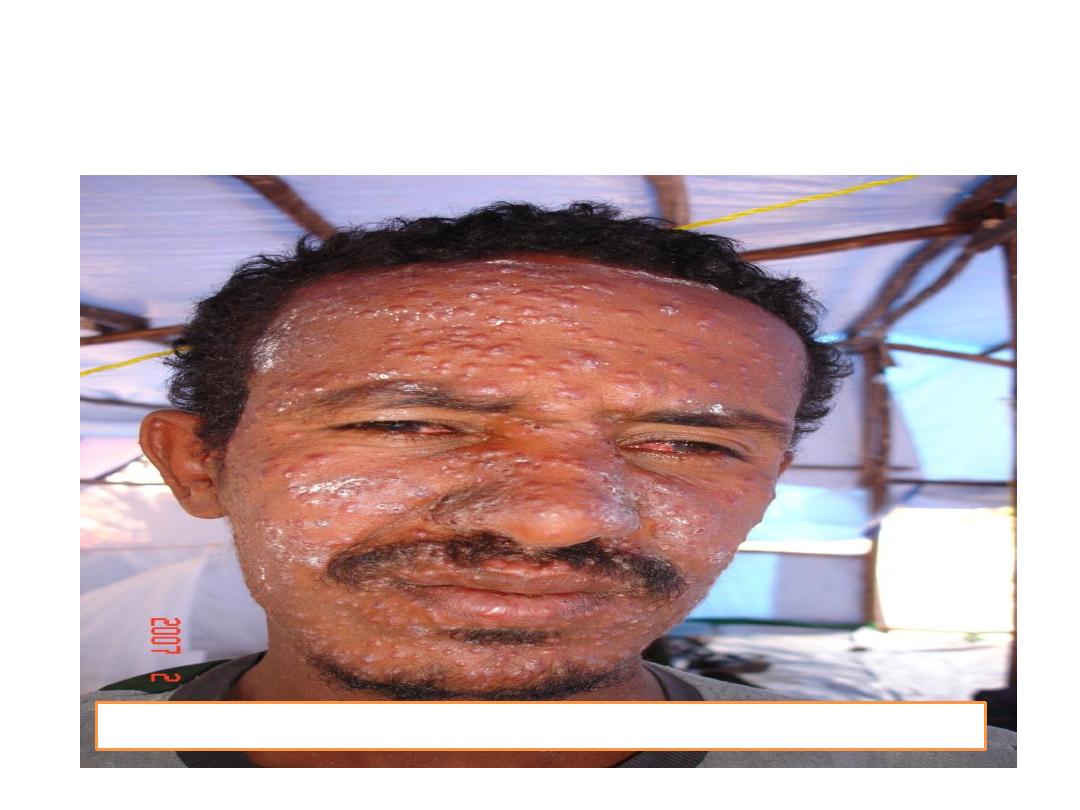
Post kala-azar dermal leishmaniasis
Patient with post-kala-azar-dermal leishmaniasis. (Ethiopia
)
Infectious agents:
Typically Leishmania donovani , L. infantum and L.infantum/
chagasi.
Reservoir:
Humans , wild Canidae (foxes and jackals) and domestic dogs.
Incubation period:
generally
2-6 months ranging from 10 days to years.
Period of communicability:
Not usually transmitted from person to person but infectious
to sandflies as long as parasites persist in the blood or skin
of reservoir.
Infectivity for phlebotomines may persist after clinical
recovery of human patients.
Susceptibility:
Susceptibility is general. Kala-azar induce lasting
homologous immunity.
Mode of transmission:
1.Bite of infected female phlebotomine sandflies
(P. argentipes).
2.Personto person transmission has been reported in
leishmania –HIV co-infected IV drug abuser through
exchange of syringes.
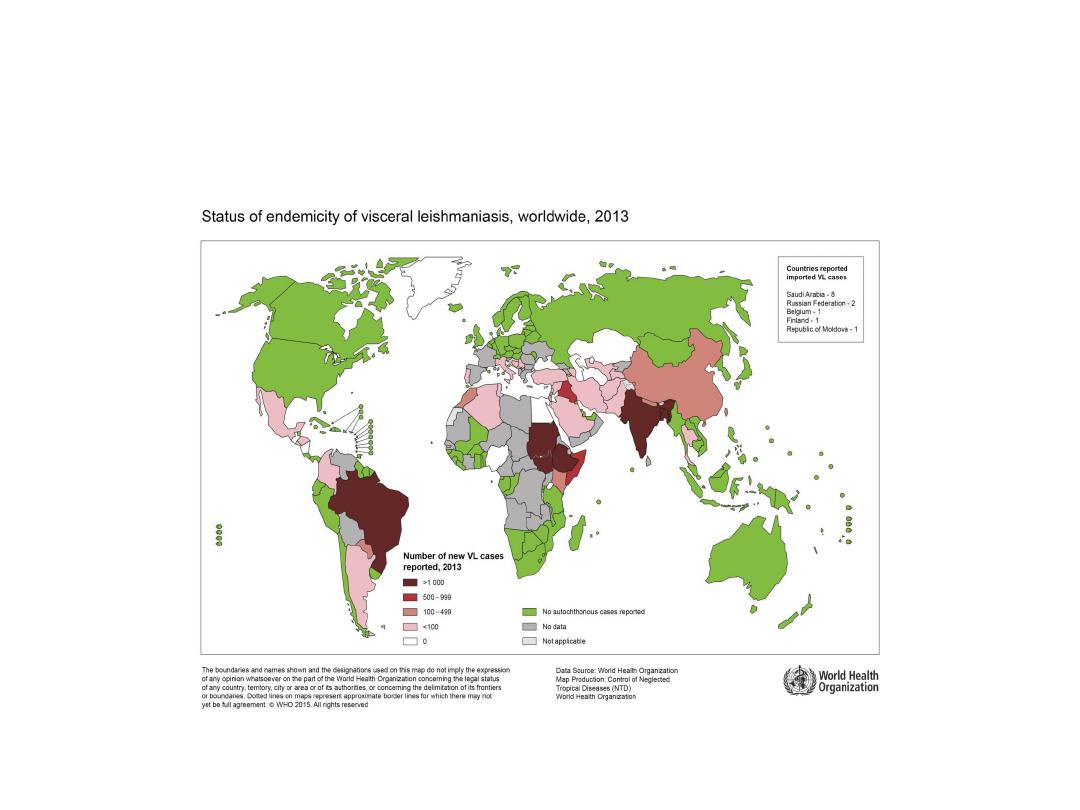
Occurrence:
Visceral leishmaniasis is a rural disease occur in 62
countries. It is highly endemic in the Indian
subcontinent and in East Africa.
An estimated 200 000 to 400 000 new cases of VL occur
worldwide each year.
Over 90% of new cases occur in 6 countries:
Bangladesh, Brazil, Ethiopia, India, South Sudan and
Sudan.
Diagnosis based on:
1. Culture of the organism from a biopsy specimen or
aspirated material.
2. Demonstration of intracellular amastigotes in stained
smears from bone marrow, spleen, liver, lymph nodes or
blood.
3. The PCR technique is the most sensitive, but remains
expensive.
4. Serological diagnosis was traditionally based
on IFA and ELISA tests.
5. An antigen detection test in urine is also under
evaluation.
Methods of control
A. Preventive measures :
No vaccine are currently available although candidate
vaccines are in development. Control measures are vary
according to the habits of mammalian hosts and habits of vectors
and include the following:
1. Case management : detect cases systematically and treat
rapidly this applied to all forms of leishmaniasis.
2. Vector control: apply residual insecticide periodically.
Phlebotomine are highly susceptible to control by systematic
spraying with residual insecticide. Spraying must include stone
walls, animal houses and rubbish heaps.

Insecticide –treated bed nets are also a good vector control
alternative which reduce the incidence of disease for example
in Syrian Arab Republic they reduce yearly incidence by 50-75%
.
3. Eliminate rubbish heaps and other breeding places.
4. Destroy gerbils implicated as reservoirs in local areas by
deep plowing and removal the plants they feed on.
5. Avoid sandfly infested forest area especially when
sundown and use insect repellents and protective clothes if
exposure is un avoidable.
6. Apply environmental management and forest clearance.
7. Control dogs which regard as animal reservoir of parasites.
A young gerbil
Control patients, contacts and immediate
environment
1. Report to local health authority.
2. Isolation with blood and body fluid precautions.
3. Concurrent disinfection, quarantine, immunization of
contacts and investigation of contacts and source of infection: not
applicable.
4. Specific treatment: Pentavalent antimonials regard as first line
treatement in most countries. Sodium stibogluconate and
meglumine antimonate are most effective. Cases that do not
respond to antimony may be treated with amphotericin B or
pentamidine. Recently developed alternative drugs include (Miltefosine,
Aminosidine (paromomycin) and Sitamaquine).

Epidemic measures:
Effective control must include understanding of the local
ecology and transmission cycle and application of
practical
measures to reduce mortality, stop transmission and
avoid
geographical extension of the epidemic.
The measures used:
1. Case detection and effective treatment.
2. Vector control by indoor residual spray and using
insecticide
treated bed nets.
3. Effective disease surveillance and program monitoring.
leishmaniasis
Cutaneous and mucosal
Other names
Baghdad boil , Delhi boil , oriental sore
.
In Americas
Espundia ,Uta and Chiclero ulcer.
It is polymorphic protozoan disease of skin and mucous membranes caused
by several species of the genus Leishmania. These protozoa exist as obligate
intracellular parasites in humans and other mammalian hosts. The disease
starts with a maculae, then a papule that enlarges and typically becomes an
indolent ulcer in the absence of bacterial infection.
Lesions may be
single or multiple
, occasionally non- ulcerative and diffuse.
Lesions may heal spontaneously within weeks to months, or last for a year or
more. In some individual certain strain (from Western Hemisphere) can
disseminate to cause mucosal lesions even years after healing of cutaneous
lesions.
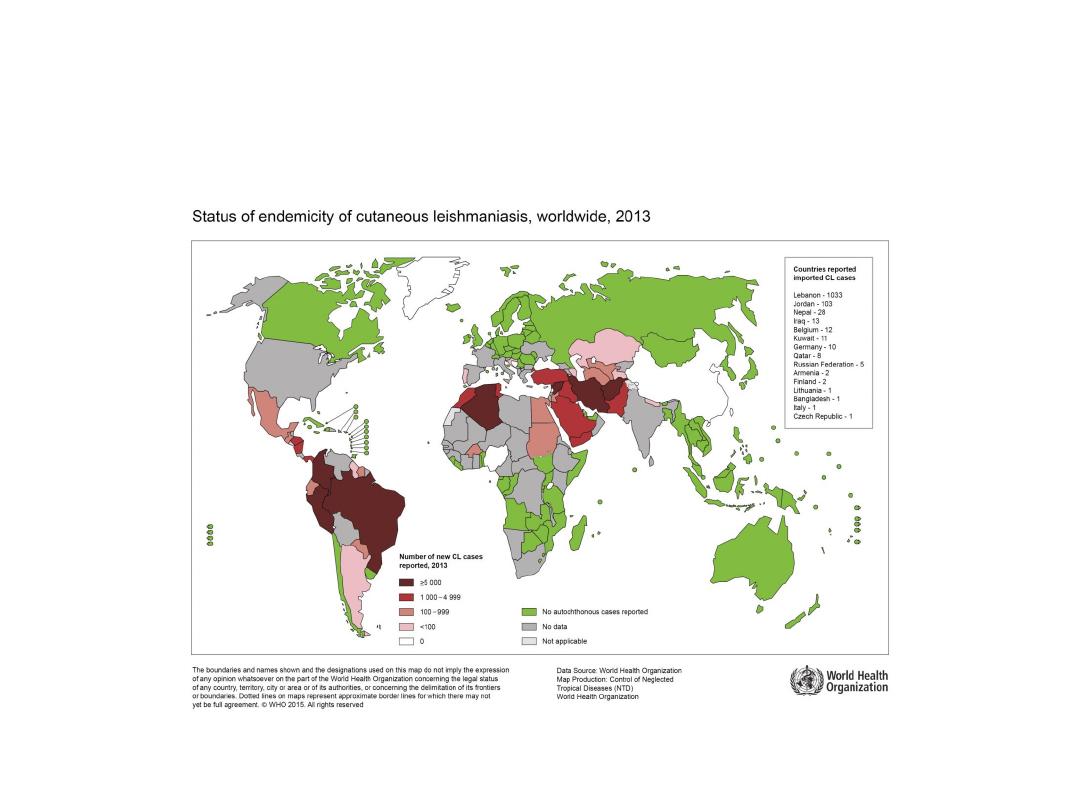
Occurrence
Cutaneous leishmaniasis (CL)
is the most common form of
leishmaniasis and causes skin lesions, mainly ulcers, on
exposed parts of the body, leaving life-long scars and
serious disability. About 95% of CL cases occur in the
Americas, the Mediterranean basin, the Middle East and
Central Asia. Over two thirds of new CL cases occur in 6
countries:
Afghanistan, Algeria, Brazil, Colombia, Iran and
the Syrian Arab Republic
. An estimated 0.7 million to 1.3
million new cases occur worldwide annually.
Mucocutaneous leishmaniasis
leads to partial or total
destruction of mucous membranes of the nose, mouth
and throat. Almost 90% of mucocutaneous leishmaniasis
cases occurs in the Bolivia, Brazil and Peru.
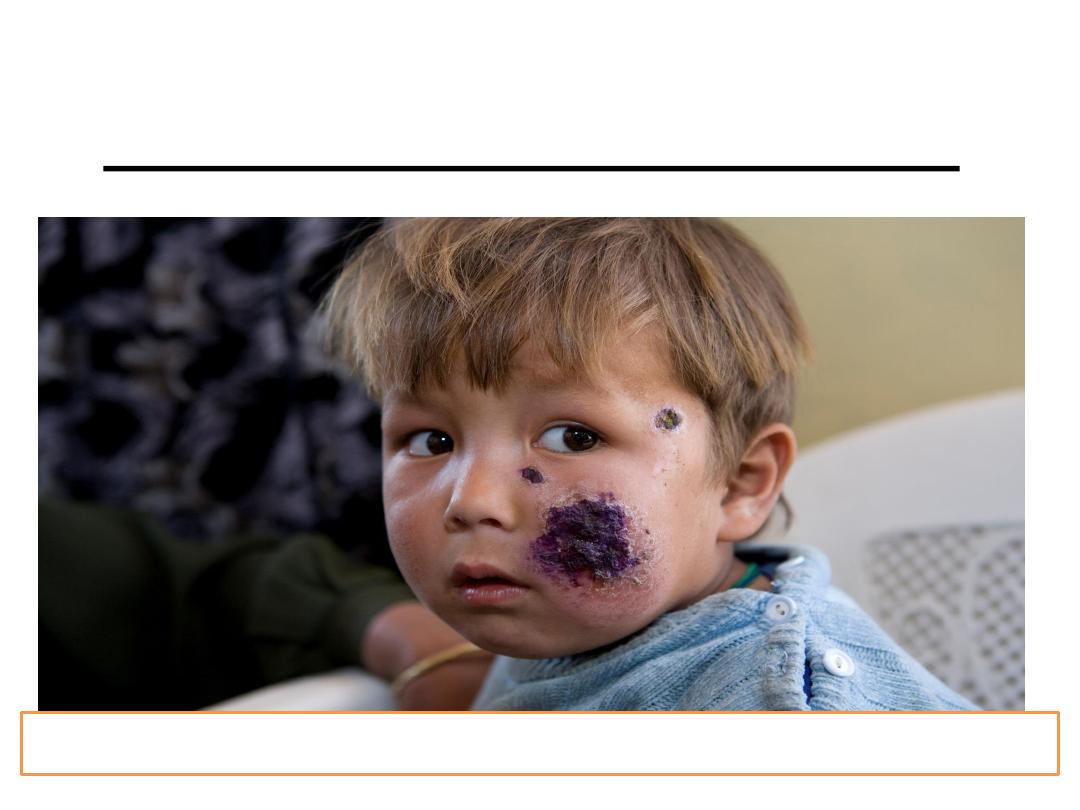
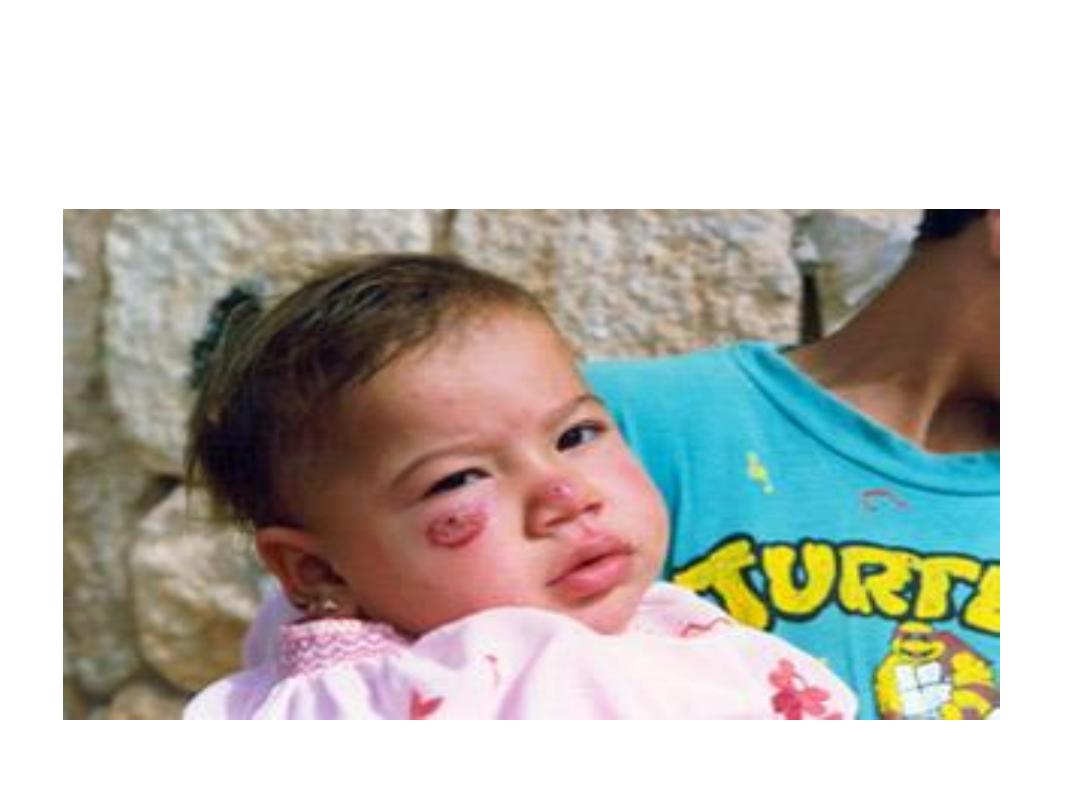
Cutaneous leishmaniasis
Child with cutaneous leishmaniasis in Kabul, Afghanistan
Diagnosis is based on:
1. Microscope identification of the non-motile,
intracellular form (amastigote) in stained specimens
from lesions.
2. An intra-dermal (Montenegro) test with leishmanin,
an antigen derived from promastigotes, is usually
positive in established disease but it is not helpful
with very early lesions and immuno-suppressed
patients.
3. Serological (IFA or ELISA) testing.
Infectious agents:
Eastern hemisphere:
Leishmania tropica , Leishmania major , Leishmania
aethiopica.
Western hemisphere:
Leishmania braziliensis and Leishmania mexicana.
Reservoir:
locally variable including humans, wild rodents, and
domestic
dogs.
Incubation period:
At least a week up to many
months.
Mode of transmission:
1.Bite of infective female phlebotomine sandfly. (P. papatasi
and
P. sergenti).
2. Rarely through blood transfusion.
Period of communicability:
Not directly transmitted from person to person but the patient
infectious for sand fly as long as parasites remain in the
lesions.
In untreated cases they can remain few months to 2 years.
Susceptibility: is general. Life long immunity may be present
after healing of lesions due to L.tropica and L.major but not
protect against other L. species.
Methods of control
A . Preventive measures:
As mentioned in visceral leishmaniasis.
B. Control patients , contacts and immediate
environment:
1. Report to local health authorities.
2. Isolation, concurrent disinfection, Quarantine and
immunization of contacts: Not applicable.
3. Investigation of contacts and source of infection:
Interrupt the local transmission cycle in the most
practical fashion.
4. Specific treatment:
Medicines called antimony-containing compounds are the
main drugs used to treatment.
These include:
Meglumine antimoniate.
Sodium stibogluconate.
Other drugs that may be used include:
Amphotericin B.
Ketoconazole.
Miltefosine.
Paromomycin.
Pentamidine.
Epidemic measures
Control the disease by:
1. Provision of adequate diagnostic and
treatment
facilities.
2. Provision of adequate measures against
sandflies and mammalian reservoirs.
Summary
• There are 3 main forms of leishmaniases – visceral (often known as
kala-azar and the most serious form of the disease), cutaneous (the
most common), and mucocutaneous.
• Leishmaniasis is caused by the protozoan Leishmania parasites
which are transmitted by the bite of infected sandflies.
• The disease affects some of the poorest people on the planet, and
is associated with malnutrition, population displacement, poor
housing, a weak immune system and lack of resources.
• Leishmaniasis is linked to environmental changes such as
deforestation, building of dams, irrigation schemes and
urbanization.
Summary
• An estimated 1.3 million new cases and 20
000 to 30 000 deaths occur annually.
• Only a small fraction of those infected
by
Leishmania
parasites will eventually
develop the disease.
Thank you
