Fetal growth
5- 18\10\2019fetal growth and birthweight are important determinants of immediate neonatal health and long-term adult health.
How to assess?
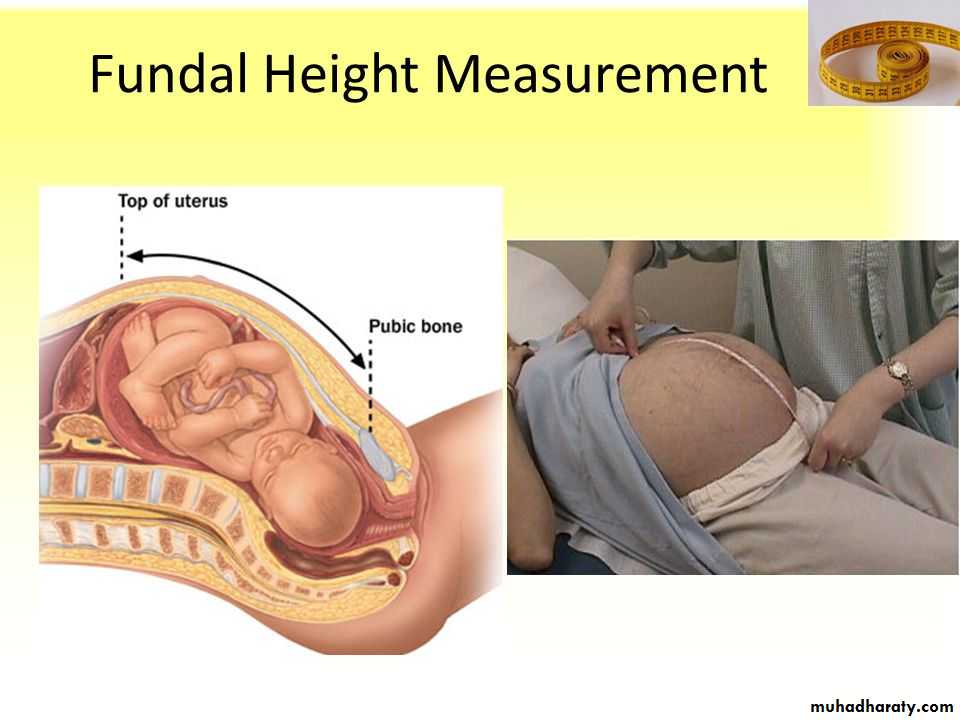
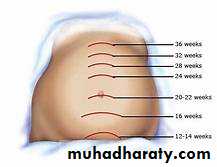
Fetal size can be assessed antenatally in two ways, either externally by using a tape measure to assess the uterine size from the superior edge of the pubic symphysis to the uterine fundus (symphysis–fundal height [SFH] measurement) orHow to assess?
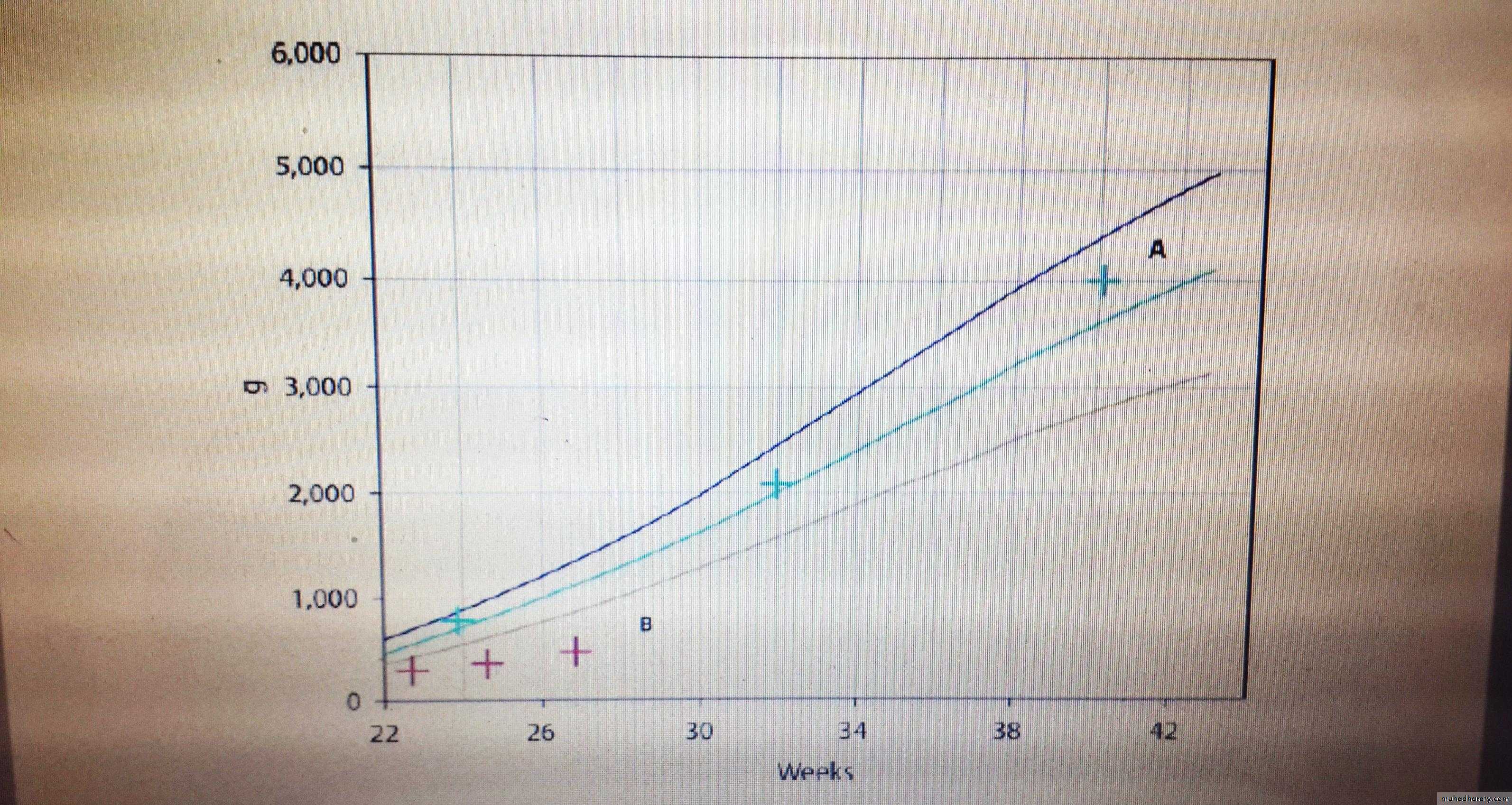
using ultrasound to measure specific parts of the fetus and then calculating the estimated fetal weight (EFW) using equations such as those described by HadlockThe fetal size is described in terms of its size for gestational age and is presented on centile charts. Centile charts can be designed for a population
A fetus that is less than the 10th centile is described as being small forgestational age (SGA)
An SGA fetus may be constitutionally small; in other words their growth potential was reached and they were destined to be that small
FGR
. Many fetuses that are SGA, have failed to reach their full growth potential, a condition called fetal growth restriction (FGR).
likely to suffer complications :-
hypoxia/asphyxia and, as a consequence, be stillborn or demonstrate signs and symptoms of
hypoxic-ischaemic encephalopathy (HIE), including
seizures and
multiorgan damage or failure in the neonatal period.
neonatal hypothermia,
hypoglycaemia,
infection and
necrotizing enterocolitis.
Fetal influences- Genetic
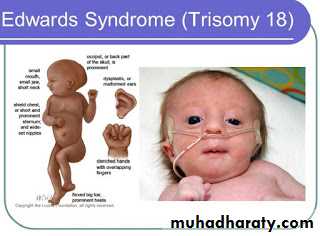
Obvious and sometimes severe FGR is seen in fetuses with chromosomal defects such as the trisomies, particularly of chromosomes 13 (Patau’s syndrome) and
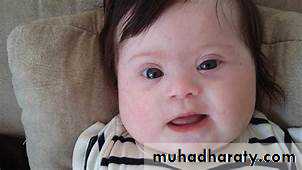
18 (Edward’s syndrome). Less severe FGR is common in trisomy 21 (Down’s syndrome).
The other genetic influence is fetal sex, with slightly greater birthweights in males.
- Infection
rubella, cytomegalovirus, Toxoplasma and syphilisMaternal influences1-Physiological influences
maternal height,prepregnancy weight,
age
certain ethnic groups lighter babies (e.g South Asian and Afro-Caribbean).
Parity is also an influence with increasing parity.
Age influences relate to the association with age and parity (i.e. older mothers are more likely to be parous).
In older women, the increased risk of chromosomal abnormalities and maternal disease, for example hypertension, lead to lower birthweights.
Teenage pregnancy is also associated with FGR.
2-Behavioural
Maternal behavioural influences are also important with smoking, alcohol and recreational drug use all associated with reduced fetal growth and birthweight.Babies born to mothers who smoke during pregnancy deliver babies up to 300 g lighter than non-smoking mothers
3-Chronic disease
Such diseases are largely those that affect placental function or result in maternal hypoxia.Conditions include hypertension (essential or secondary to renal disease) can lead to placental infarction that impairs its function
lung or cardiac conditions (cystic fibrosis, cyanotic heart disease)..
Maternal thrombophilia can also result in placental thrombosis and infarction.
Fetal developmentCardiovascular system and the fetal circulation
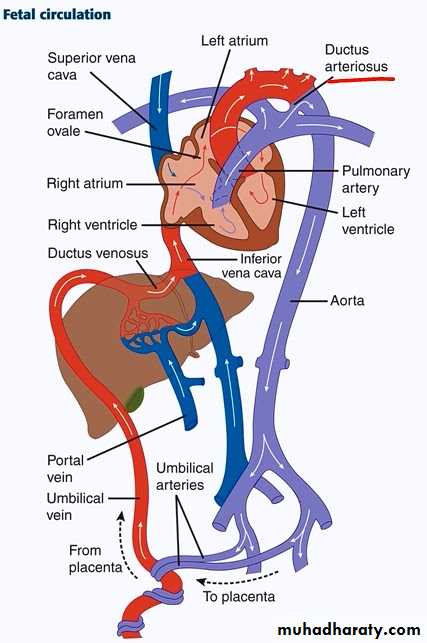
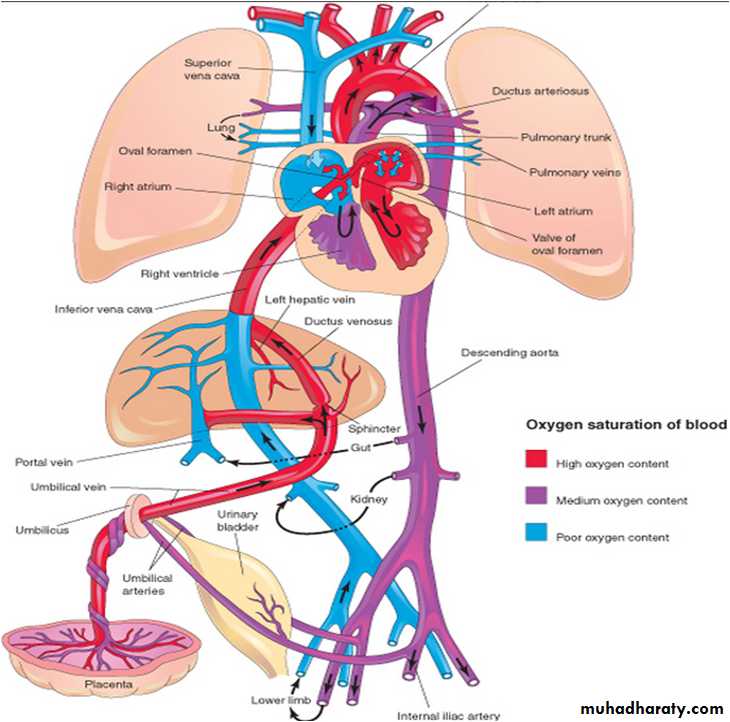
The fetal circulation is characterized by four shunts that ensure that the oxygenated bloodfrom the placenta is delivered to the fetal brain. These shunts are the:
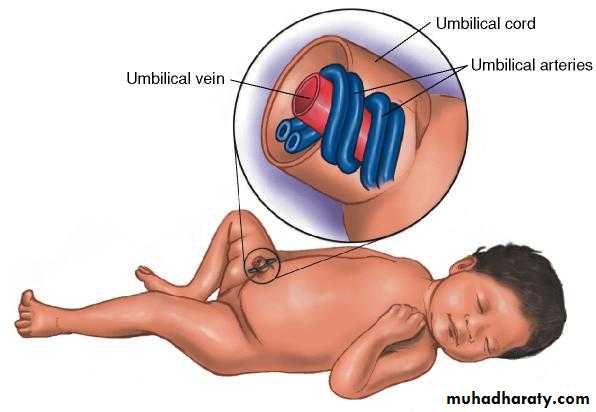
1-Umbilical circulation.
2-Ductus venosus.
3-Foramen ovale.
4-Ductus arteriosus
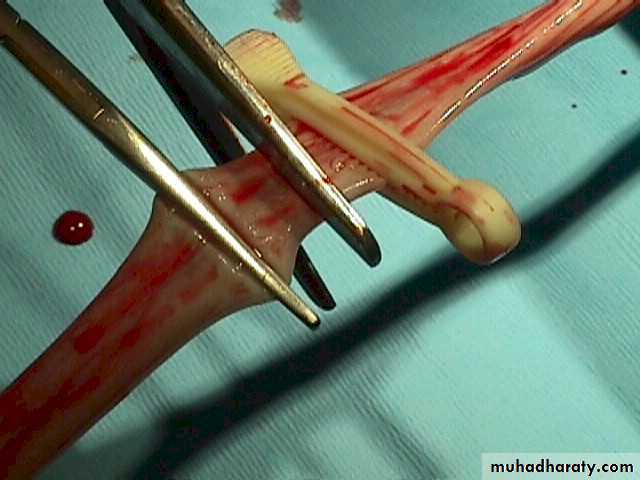
The umbilical circulation carries fetal blood to and from the placenta for gas and nutrient exchange. The umbilical arteries arise from the caudal end of the dorsal fetal aorta and carry deoxygenated blood from the fetus to the placenta.
Normally two umbilical arteries are present.
Oxygenated blood is returned to the fetus via the umbilical vein to the fetal liver.The umbilical cord
In the liver
A small proportion of blood oxygenates the liver but the bulk passes through the ductus venosusbypassing the liver and joins the inferior vena cava (IVC) as it enters the right atrium.
In the heart The ductus venosus is a narrow vessel and high blood velocities are generated within it. This streaming of the ductus venosus blood, together with a membranous valve in the right atrium (the crista dividens), prevents mixing of the
well-oxygenated blood from the ductus venosus with the desaturated blood of the IVC
foramen ovale
The ductus venosus stream passes across the right atrium through a physiological defect in the atrial septum called the foramen ovale, to the left atrium. From here, the blood passes through the mitral valve to the left ventricleand hence to the aorta.
About 50% of the blood goes to the head and upper
extremities, providing high levels of oxygen to supply the fetal heart, upper thorax and brain; the remainder passes down the aorta to mix with blood of reduced
oxygen saturation from the right ventricle.
Ductus arteriosus
Deoxygenated blood returning from the fetal head and lower body flows through the right atrium and ventricle and into the pulmonary artery, after which it bypasses the lungs to enter the descending aortavia the ductus arteriosus that connects the two vessels.
Only a small portion of blood from the right ventricle passes to the lungs, as they are not functional.
dose the fetus have breathing movement ?
Is there a high oxygen tension air entering the fetal lung ?
By this means, the desaturated blood from the right ventricle passes down the aorta to enter the umbilical arterial circulation and be returned to the placenta for reoxygenation.
Prior to birth
the ductus ateriosus remains patent due to the production of prostaglandin E2 and prostacyclin, which act as local vasodilators.Premature closure of the ductus arteriosus has been reported with the administration of cyclooxygenase inhibitors.
At birth
, the cessation of umbilical blood flow causes cessation of flow in the ductus venosus, a fall in pressure in the right atrium and closure of the foramen ovale.Ventilation of the lungs opens the pulmonary
circulation, with a rapid fall in pulmonary vascular resistance, which dramatically
increases the pulmonary circulation.
The ductus arteriosus closes functionally within a few days of birth.
The cord should be double clamped approximately 1-2minute after delivary
Central nervous system
Neural development is one of the earliest systems to begin and one of the last to be completed. The early central nervous system (CNS) begins as a simple neural plate thatfolds to form a groove then tube, open initially at each end.
Failure of these opening to close contributes a major class of neural abnormalities called neural tube defects (NTDs)
Which prophylaxis can be given ?
Respiratory system
The lung first appears as an outgrowth from the primitive foregut at about 3–4 weeks.By 26 weeks, with further development of the airway and vascular tree, type I and II epithelial cells are beginning to differentiate.
Pulmonary surfactant, a complex mixture of phospholipids and proteins that reduces surface tension at the air–liquid interface of the alveolus, is
produced by the type II cells starting from about 30 weeks
Pulmonary surfactant
prevents the collapse of small alveoli during expirationby lowering surface tension. The predominant phospholipid in surfactant (80% of the total) is phosphatidylcholine (lecithin), the production of which is enhanced by
cortisol, growth restriction and prolonged rupture of the membranes, and is
delayed in maternal diabetes mellitus. Inadequate amounts of surfactant result in poor lung expansion and poor gas exchange.
In infants delivering preterm, prior to the maturation of the surfactant system, this results in a condition known as respiratory distress syndrome (RDS).
Alimentary system
The primitive gut consists of three parts,the foregut,
midgut and
hindgut
Omphalocele (exomphalos)
Between 5 and 6 weeks, the midgut is extruded into the umbilical cord as a physiological hernia.then the gut undergoes rotation prior to reentering the abdominal cavity by 12 weeks of gestation.
The liver
By the sixth week, the fetal liver performs haematopoiesis. This peaks at 12–16 weeks and continues until 36 weeks.In utero, the normal metabolic functions of the liver are performed by the placenta.
The fetal liver has a reduced ability to conjugate bilirubin because of relative deficiencies in the necessary enzymes such as glucuronyl transferase.
physiological jaundice
After birth, the loss of the placental route of excretion of unconjugated bilirubin, in the presence of reduced conjugation, particularly in the premature infant, may result in transient unconjugated hyperbilirubinaemia or physiological jaundice of the newborn.Kidneys and urinary system
The kidneys developed from the mesonephric duct (willfian duct ) which extends towards the most caudal end of the embryo, ultimately attaching to the cloaca. During the fifth week of gestation the ureteric bud develops as an out-pouching from the Wolffian duct. This bud grows towards the head of the embryo and into the intermediate mesoderm and as it does so it branches to form the collecting duct system (ureter, pelvis, calyces and collecting ducts) of the kidneyAs fetal urine forms much of the amniotic fluid, renal agenesis will result in severe reduction (oligohydramnios) or absence of amniotic fluid (anhydramios).
Blood and immune system
by 20 weeks almost all of these cells are produced by the bone marrow.much of the immunoglobulin (Ig) G in the fetus originates from the maternal circulation and
crosses the placenta to provide passive immunity to the fetus and neonate.
The fetus normally produces only small amounts of IgM and IgA, which do not cross
the placenta. Detection of IgM/IgA in the newborn, without IgG, is indicative of fetal infection.
hemoglobin
Most haemoglobin in the fetus is fetal haemoglobin (HbF), (alpha-2, gamma-2). This differs from the adult haemoglobins HbA and HbA2, which have two beta-chains (alpha-2, beta-2) and two delta-chains (alpha-2, delta-2), respectively.Ninety percent of fetal haemoglobin is HbF
between 10 and 28 weeks gestation. From 28 to 34 weeks, a switch to HbA
occurs, and at term the ratio of HbF to HbA is 80:20; by 6 months of age, only 1%
of haemoglobin is HbF.
Skin and homeostasis
By the fourth week following conception, a single-cell layer of ectoderm surrounds the embryo.At about 6 weeks this ectodermal layer differentiates into an outer periderm and an inner basal layer.
The periderm eventually sloughs as the vernix, a creamy protective coat that covers the skin of the fetus.
The basal layer produces the epidermis and the glands, nails and hair follicles. Preterm babies have no vernix and thin skin; this
allows a proportionately large amount of insensible water loss.
thanks