
Classification of autoimmune diseases
1-classified as organ-specific or multisystem
2-mechanism responsible for tissue damage. The Gell and Coombs
classification of hypersensitivity
Gell and Coombs classification of hypersensitivity diseases
Type
Mechanism
Example of disease
in response to
exogenous agent
Example of
autoimmune disease
Type I
Immediate
hypersensitivity
IgE-mediated mast cell
degranulation
Allergic disease
None described
Type II
Antibody-
mediated
Binding of cytotoxic IgG or
IgM antibodies to antigens
on cell surface causes cell
killing
1-ABO blood
transfusion reaction
2-Hyperacute
transplant rejection
1-Autoimmune
haemolyticanaemia
2-Idiopathic
thrombocytopenic
purpura
3-Goodpasture's
disease
Type III
Immune
complex-
mediated
IgG or IgM antibodies bind
soluble antigen to form
immune complexes which
trigger classical complement
pathway activation
1-Serum sickness
2-Farmer's lung
e.gSLE
Type IV
Delayed type
Activated T cells,
phagocytes and NK cells
1-Acute cellular
transplant rejection
2-Nickel
hypersensitivity
1-Type 1 diabetes
2-Hashimoto's
thyroiditis
Type I hypersensitivity is relevant in allergy but is not associated with
autoimmune disease.
In type II hypersensitivity, injury is localised to a single tissue or organ.
Type III hypersensitivity is a generalised reaction resulting from immune
complex deposition in blood vessel walls, skin, joints and glomeruli,
where
they cause a chronic inflammatory response
. gives rise to systemic
diseases such as SLE.
In type IV hypersensitivity, activated T cells and macrophages mediate
phagocytosis and NK cell recruitment.

Investigations in autoimmunity
1-Autoantibodies
can be identified in the laboratory, and are useful in disease diagnosis and
monitoring.
-Rheumatoid factor
A rheumatoid factor is an antibody directed against the common (Fc) region of
human IgG. Rheumatoid factors may be of any immunoglobulin class but IgM
is most commonly tested
CONDITIONS ASSOCIATED WITH A POSITIVE RHEUMATOID
FACTOR
Disease Frequency (%)
Rheumatoid arthritis with extra-articular manifestations 100 %
Rheumatoid arthritis (overall) 75%
Sjögren's syndrome 90 %
Primary biliary cirrhosis 50 %
Subacute bacterial endocarditis 40 %
SLE 30 %
Tuberculosis 15%
Elderly (> 65 years) 20
. Only 50% of patients with rheumatoid arthritis are positive for rheumatoid
factor
at the time of diagnosis
; a further 25% will become seropositive
in the
first 2 years of disease
(. Thus this test is
insufficiently sensitive
to rule out
rheumatoid arthritis. In addition, rheumatoid factor
has low specificity
for
rheumatoid arthritis, being associated with a wide variety of autoimmune and
non-autoimmune conditions, and a common finding in the elderly (). The major
indication for rheumatoid factor testing is
to evaluate prognosis
in rheumatoid
arthritis, as it is associated with more severe erosive disease and extra-articular
disease manifestations such as nodules, vasculitis and Felty's syndrome.
Anti-CCP antibody
Antibodies to cyclic citrullinated peptide (anti-CCP antibodies) bind to
peptides in which the amino acid arginine has been converted to citrulline by
peptidylargininedeiminase, an enzyme abundant in the inflamed synovium.
It is
a more specific test for rheumatoid arthritis
than rheumatoid factor and a
better

predictor of an aggressive disease
course. In patients with undifferentiated
arthritis, anti-CCP antibodies may predict those who are likely to develop
rheumatoid arthritis.
Antinuclear antibodies
CONDITIONS ASSOCIATED WITH A POSITIVE ANTINUCLEAR
ANTIBODY
SLE
∼100%
Scleroderma 60-80%
Sjögren's syndrome 40-70%
Dermatomyositis or polymyositis 30-80%
Mixed connective tissue disease 100%
N.B. 5% of healthy individuals have an ANA titre> 1:80.
Antinuclear antibodies (ANA) are a group of antibodies which bind to
components of the nucleus.
The major indication for ANA testing is in the diagnosis of SLE, where it has a
very high sensitivity (almost 100%), and a negative ANA test virtually
excludes the diagnosis. However, the specificity is low (, and ANA may be
present in low titre in healthy individuals.
Anti-DNA antibodies
Anti-DNA antibodies bind to double-stranded DNA and are highly specific for
SLE (95%). They occur in up to 60% of SLE patients at some time in their
disease course.
Antiphospholipid antibodies
Antiphospholipid antibodies are associated with the development of
venous
and arterial thrombosis and recurrent fetal loss
. This may occur in isolation
(primary antiphospholipid syndrome), or as a complication of SLE (secondary
antiphospholipid syndrome).
, but the most commonly measured are anticardiolipin antibodies and lupus
anticoagulant.
2-Measures of complement activation
Measuring complement useful in the evaluation of immune complex-mediated
diseases(type III). Classical complement pathway activation leads to a decrease
in circulating C4, and decreased C3 levels. Serial measurement of C3 and C4
is a useful surrogate measure of immune complex formation.
3-C-reactive protein (CRP)
4-Erythrocyte sedimentation rate (ESR)
In allergies
, the immune system reacts to an outside substance that it normally
would ignore.
With autoimmune disorders
, the immune system reacts to normal body
tissues that it would normally ignore.
Symptoms of an autoimmune disease vary based
on the disease
and
location of
the abnormal immune response
.
ALLERGY
Mechanisms of allergic disease

Pathology of allergy
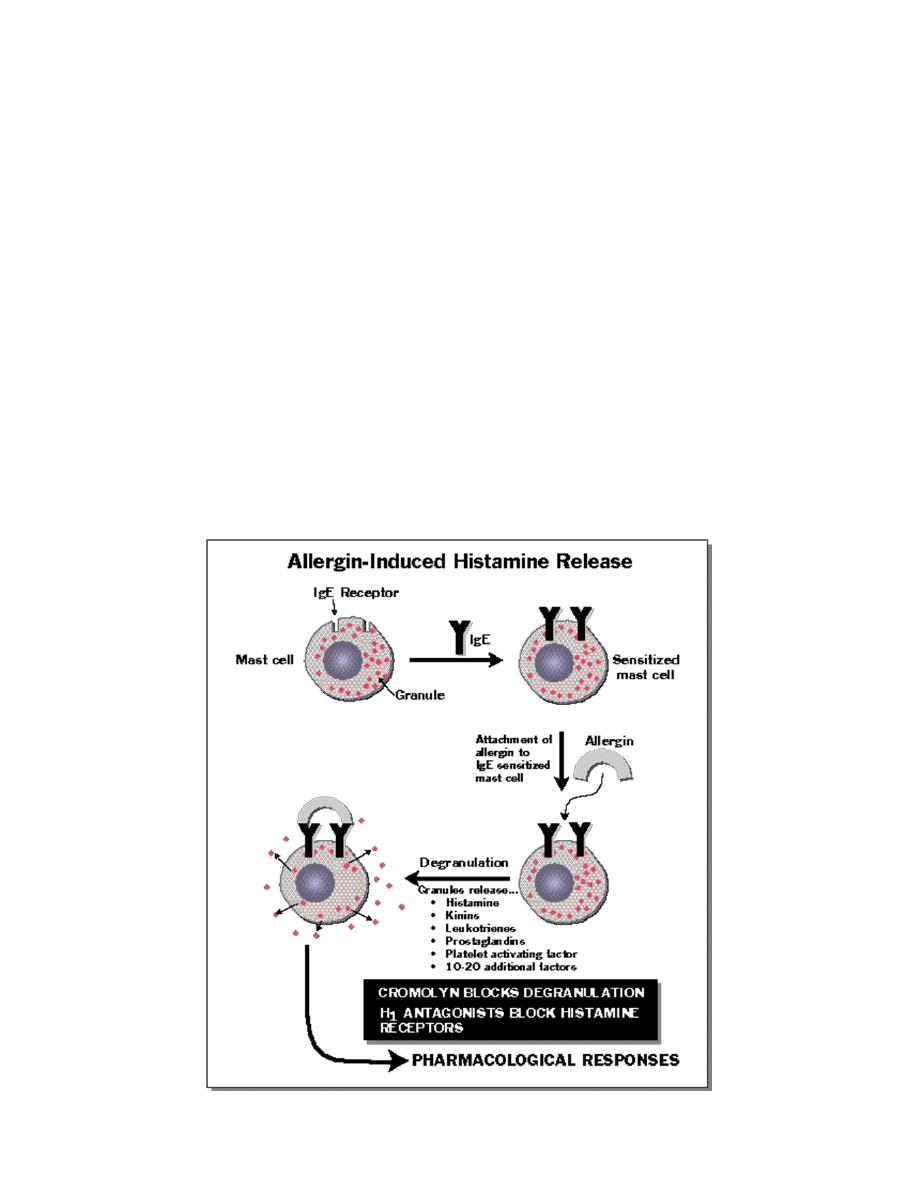
Normally, the immune system does not make detectable responses to the many
environmental substances to which it is exposed on a daily basis. However, in
an allergic reaction, initial exposure to an otherwise harmless exogenous
substance (known as an allergen)
triggers the production of specific IgE
antibodies by activated B cells
(). These IgE antibodies bind to the surface of
mast cells via high-affinity IgE receptors,
a step that is not immediately
associated with clinical sequelae
.
However, upon re-exposure
, the allergen
binds to membrane-bound IgE which activates the mast cells, releasing a
variety of vasoactive mediators (the early phase response) and causing a type I
hypersensitivity reaction and the symptoms of allergy. The latter range from
sneezing and rhinorrhoea to anaphylaxis
Allergic diseases
Atopy
is the tendency to produce an exaggerated(inappropriate)IgE immune
response to otherwise harmless environmental substances,
And an allergic diseaseis
clinical manifestation of this inappropriate
IgE immune response
Factors influencing susceptibility to allergic diseases
1- 'Hygiene hypothesis'. infections in early life bias the immune system against
the development of allergies, and that allergy is the penalty for the decreased
incidence of infection that has resulted from improvements in sanitation and
health care.
2-Family history., including genes controlling cytokine production,.
3-Environmental factors such as pollutants and cigarette smoke, and the
incidence of bacterial and viral infection.

Products of mast cell degranulation
Products of mast cell degranulation
Mediator
Biological effects
Histamine,Leukotrienes
Prostaglandins
Thromboxanes
Vasodilatation, bronchoconstriction and
mucus secretion. Increases capillary permeability
Eosinophil chemotactic factor
Eosinophil chemotaxis
Neutrophil chemotactic factor
Neutrophil chemotaxis
Platelet-activating factor
Bronchoconstriction, chemotaxis of
eosinophils and neutrophils
Common allergic diseases
• Urticaria
• Angioedema
• Atopic dermatitis
• Allergic conjunctivitis
• Allergic rhinitis (hayfever)
• Allergic asthma
• Food allergy
• Drug allergy
• Allergy to insect venom
• Anaphylaxis
Investigations
Skin prick tests
Skin prick testing is the 'gold standard' of allergy testing. A droplet of diluted standardised
allergen solution is placed on the forearm and the skin is superficially punctured through
the droplet with a sterile lancet. After 15 minutes, a positive response is indicated by a
local weal and flare response ≥ 2 mm larger than the negative control.
Specific IgE tests
An alternative to skin prick testing is the quantitation of IgE directed against the putative
allergen..
Non-specific markers of atopic disease: total serum IgE and eosinophilia
Peripheral blood eosinophilia is common in atopic individuals
Causes of increase IgE
Atopy is the most common cause

parasite and helminth infections (), lymphoma (), drug reactions and Churg-Strauss
vasculitis (
Management
•
Avoidance of the allergen
•
Antihistamines block histamine H1 tissue receptors, thereby inhibiting
the effects of histamine release..
•
Corticosteroids down-regulate pro-inflammatory cytokine production..
•
Sodium cromoglicatestabilises the mast cell membrane, inhibiting release
of vasoactive mediators. It is effective as a prophylactic agent in asthma and
allergic rhinitis, but has no role in management of acute attacks. It is poorly
absorbed and therefore ineffective in the management of food allergies.
•
Antigen-specific immunotherapy involves the sequential administration
of escalating amounts of dilute allergen over a prolonged period of time. Its
mechanism of action is unknown, but it is highly effective in the prevention of
insect venom, anaphylaxis, allergic asthma, and allergic rhinitis secondary to
grass pollen
•
Omalizumab, a monoclonal antibody against IgE, inhibits the binding of
IgE to mast cells and basophils. It is effective in moderate and severe allergic
asthma and rhinitis.
•
Preloaded self-injectable adrenaline (epinephrine) may be life-saving in
the acute management of anaphylaxis.
Anaphylaxis
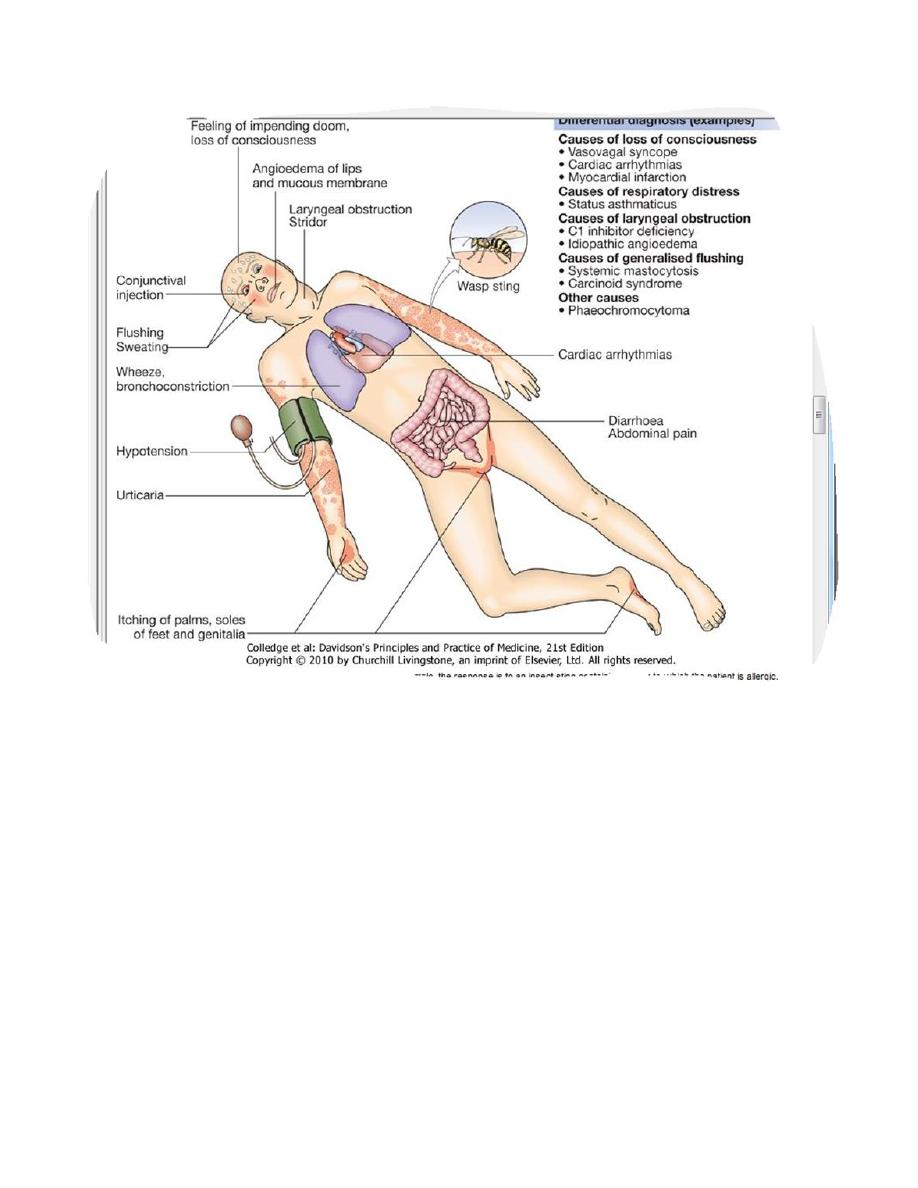
Anaphylaxis is a potentially life-threatening, systemic allergic reaction caused
by the release of histamine and other vasoactive mediators from mast cells.
The risk of death is increased in patients with pre-existing asthma, particularly
if this is poorly controlled, and in individuals in whom treatment with
adrenaline (epinephrine) is delayed.
Common causes of immediate generalised reactions
Anaphylaxis: IgE-mediated mast cell degranulation
Foods
•
Peanuts
•
Fish and shellfish

•
Milk
•
Eggs
•
Soy products
Insect stings
•
Bee venom
•
Wasp venom
Chemicals, drugs and other foreign proteins
•
Intravenous anaesthetic agents,
•
Penicillin and other antibiotics
•
Latex
Anaphylactoid: non-IgE-mediated mast cell degranulation Drugs
•
Aspirin and non-steroidal anti-inflammatory drugs (NSAIDs)
•
Opiates
•
Radiocontrast media
•
Physical Exercise
•
Cold
Idiopathic
•
No cause is identified in 20% of patients with anaphylaxis
Clinical feature of anaphylaxis
.
Management
Emergency manage ment of anaphylaxis
Prevent further contact with allergen
•
e.g. Removal of bee sting
Ensure airway patency
Administer intramuscular adrenaline (epinephrine) promptly
•
Adult dose: 0.3-1.0 mL 1:1000 solution
•
Acts within minutes
•
Repeat at 5-10 min intervals if initial response is inadequate
Administer antihistamines
•
e.g. Chlorphenamine 10 mg i.m. or slow i.v. injection
•
Directly opposes effects of mast cell activation
Administer corticosteroids
•
e.g. Hydrocortisone 200 mg i.v.
•
Prevents rebound symptoms in severely affected patients
Provide supportive treatments
•
e.g. Nebulised β2-agonists to decrease bronchoconstriction
•
I.v. fluids to restore or maintain blood pressure
•
Oxygen
Angioedema
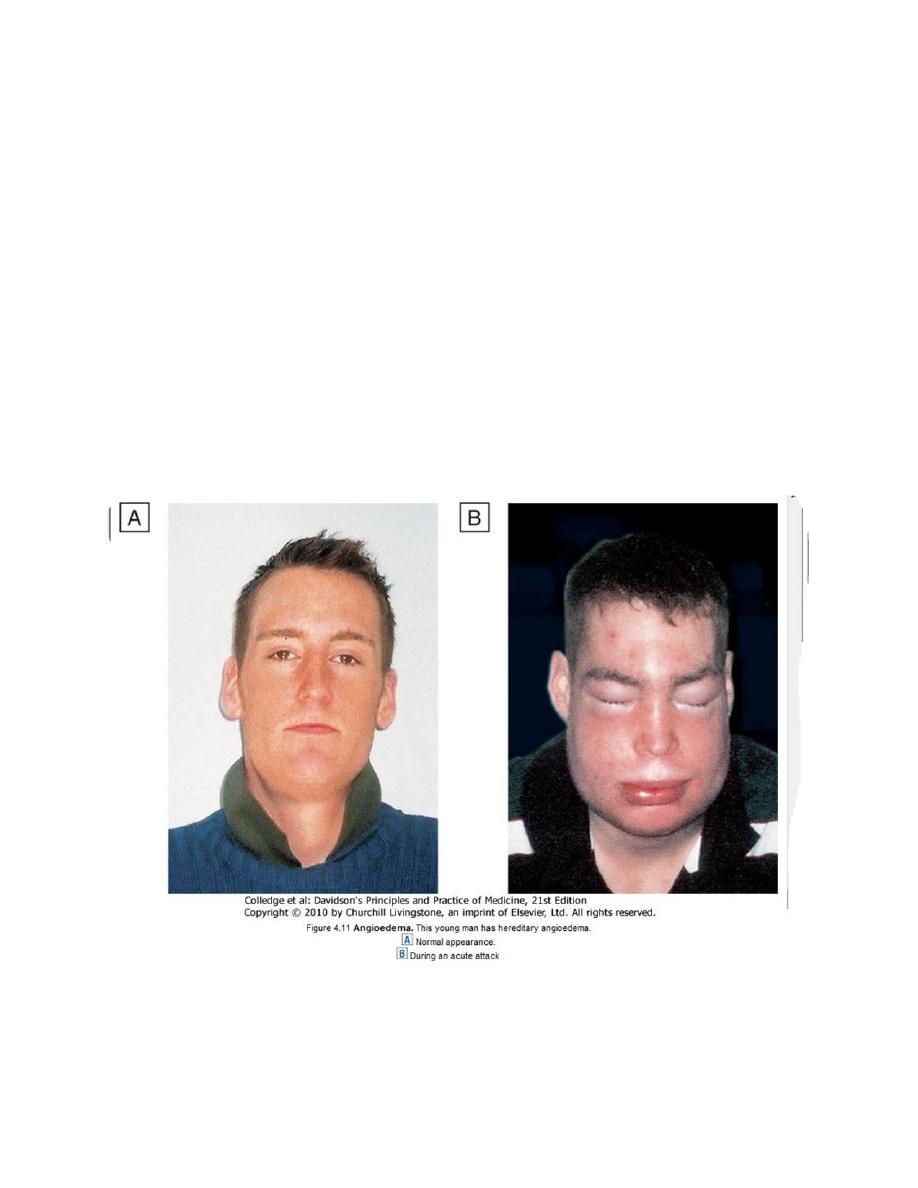
Angioedema is the episodic, localised, non-pitting swelling of submucous or
subcutaneous tissues. This most frequently affects the face ), extremities and
genitalia. Involvement of the larynx or tongue may cause life-threatening
respiratory tract obstruction, and oedema of the intestine may cause abdominal
pain and distension.
