Rheumatology and bone disease
Introductionlecture 1
Musculoskeletal diseases may arise from processes affecting bones, joints, muscles, or connective tissues such as skin and tendon.
The exact etiology of most of these disorders is not known.
The principal manifestations are pain and impairment of locomotor function.
Diseases of the musculoskeletal system tend to be more common in women and most increase in frequency with increasing age.
TYPES OF JOINT
Fibrousfibrocartilaginous
and synovial
Fibrous and fibrocartilaginous joints joining two bones together where there is little requirement for movement e.g. Skull sutures , Costochondral junctions
The intervertebral disc is a special type of fibro cartilaginous.
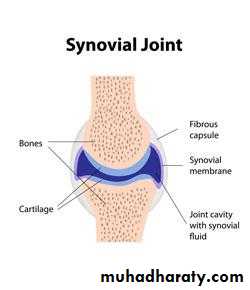
Anatomy of synovial joints
consist of:1. Opposing bony surfaces.
2. Hyaline cartilage covering the articulating surfaces of bones, It is firmly attached to the underlying bone, It is aneural & avascular. It gets the nourishment from synovial fluid, s. membrane &underlying bone. The cartilage is a shock absorber.
3. Capsule which is surrounding the articular tissue.
4. Synovial membrane which lines the capsule, it has a macrophages like a cells that removes the wear-and-tear debris from the synovial fluid with a phagocytic function & B cells are fibroblast like cells produce hyaluronate part of synovial fluid.
5. Joint cavity.
6. Synovial fluid: Is a viscous, pale yellow & clear fluid, present in small amount ranging from (0.1- 4 ml). The hyaluronic acid makes the fluid viscous to lubricate the joint.
History in rheumatology
AgeThe age of the patient is the first step in considering a differential diagnosis. For example, arthritis is a major manifestation of hemophilia with onset during childhood.
The term juvenile RA refers to three different forms of arthritis with onset before the age of 16 years.
In young adults, inflammatory and septic arthritic conditions may be seen, but OA is exceptional.
The onset of RA is often in the middle years, whereas the elderly are more prone to OA.
Arthritis in the elderly is often assumed to be degenerative, when in fact the patient may have an inflammatory process such as polymyalgia rheumatica, RA, or systemic lupus erythematosus (SLE).
Gender:
RA and other autoimmune diseases are more common in women, whereas ankylosing spondylitis and the other spondyloarthropathies associated with the human leukocyte antigen HLA-B27 are more common in men.Gouty arthritis is more common in men and rarely attacks women before menopause.
Occupation and Recreation
The clinician should inquire about the patient's job to determine how demanding itis.Occupational factors such as repetitive joint trauma may contribute to the development of OA in susceptible individuals.
Musculoskeletal symptoms may also be associated with jogging or with trauma from sports activities.
Family History
It is important to obtain a complete family history, because autoimmune diseases and gout occur with an increased incidence in families.
Onset and Evolution of Symptoms
Knowledge of the pattern of onset, location, and evolution of musculoskeletal symptoms is essential for accurate diagnosis.
The development of symptoms over hours to days is characteristic of acute arthritis and usually represents an inflammatory or traumatic process.
The persistence of symptoms for more than 6 weeks is considered chronic arthritis,
whereas an intermediate duration of days to weeks is referred to as subacute arthritis.
Pattern of Joint Involvement
The distribution of joint involvement is one of the most essential aspects of diagnosis of musculoskeletal diseases.Monoarthritis describes symptoms in a single joint;
oligoarthritis (or pauciarthritis), symptoms in two to four joints; and
polyarthritis, involvement of five or more joints.
Arthritis in an extremity is called peripheral joint disease, whereas spinal involvement is termed axial disease.
It is important to elicit a history of symmetrical versus asymmetrical peripheral joint disease.
The predominant involvement of the small joints of the hands and feet or of large joints such as the shoulder, hip, and knee also has diagnostic importance.
A critical feature in clinical diagnosis is the distinction between arthralgia (subjective joint pain) and arthritis (objective joint swelling, deformity, or impaired function).
Objective findings on physical examination must be found for a diagnosis of “arthritis” to be made.
Inflammatory versus non inflammatory Conditions
An important initial step in the evaluation of musculoskeletal symptoms is the differentiation of inflammatory versus non inflammatory disease.A history of warmth and erythema over a joint suggests inflammatory disease.
Morning stiffness lasting longer than 60 minutes, a “gel” phenomenon (stiffness after rest that is more than transient), and improvement in pain and stiffness with activity all suggest the presence of inflammatory disease.
In contrast, minimal morning stiffness and worsening pain with activity suggest non inflammatory joint disease
Extra-articular and Systemic Features
A careful history may reveal important systemic and extra-articular manifestations, including fever, fatigue, weakness, dry eyes, ocular inflammation, pulmonary symptoms, or Raynaud's phenomenon.
The finding of musculoskeletal complaints in the setting of systemic symptoms and multiorgan involvement strongly suggests the possibility of a diffuse connective tissue disease such as SLE.
INVESTIGATION OF MUSCULOSKELETAL DISEASE
SYNOVIAL FLUID ANALYSISThis is important investigation in patients suspected of having septic arthritis, crystal-associated arthritis and intra-articular bleeding, and it should be performed in all patients with acute monoarthritis, especially with overlying erythema.
Synovial fluid (SF) can readily be obtained from most peripheral joints and for diagnostic purposes only a small volume is required.
Normal SF is present in small volume, contains very few cells, is clear and either colourless or pale yellow, and has high viscosity.
With increasing joint inflammation the volume increases, the total cell count and proportion of neutrophils rise (causing turbidity), and the viscosity lowers (due to enzymatic degradation of hyaluronan and aggrecan).
PLAIN RADIOGRAPHY
X-rays can show anatomical changes that reflect important pathological processes, including:soft tissue swelling-seen as altered skin contours, displaced fat planes and intracapsular fat pads (fat appears dark on X-ray) ,
decreased bone density (osteopenia) or increased bone density (osteosclerosis) which may be localised or generalised bone enlargement and deformity .
joint erosion(non-proliferative or proliferative marginal erosion, central erosion)
joint-space narrowing (focal-osteoarthritis; generalised-inflammatory arthritis)
new bone formation (osteophyte, enthesophyte) and periosteal reaction
calcification (cartilage-chondrocalcinosis; synovium, capsule, ligament, tendon, muscle, blood vessels, skin) and intra-articular osteochondral bodies.
A hallmark of major inflammatory arthropathies is cartilage and bone erosion.
Intracapsular bone erosion first occurs at the 'bare areas' of the joint margin ('marginal erosion') where bone is exposed directly to inflammatory synovium without the protection of overlying cartilage.
X-ray of hip showing changes of osteoarthritis
Erosive arthritis in chronic gout.
Computerised tomography (CT) and magnetic resonance imaging (MRI)These modalities allow detailed three-dimensional visualization of anatomically complex structures, such as the spinal canal and facet joints, which may be inadequately assessed by plain X-rays.
limitation of CT include limited soft tissue resolution and a high radiation dose, and for many situations MRI is now preferred.
Contrast agents, such as gadolinium, can be administered to increase sensitivity in detecting erosions and synovitis
Ultrasound of joint & soft tissues.
- Radioisotope bone scan: (tumors, infection& trauma).
BLOOD TESTS IN RHEUMATIC DISEASES
C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR)Infections, inflammation and neoplasia all induce an acute phase response which is associated with changes in the full blood count, ESR and CRP.
Of the many acute phase proteins that react to inflammation and infection, CRP is the single most useful measure because it is the most sensitive and the quickest to respond.
A notable exception is in connective tissue diseases such as lupus, systemic sclerosis and dermatomyositis where there is little elevation of CRP despite clear evidence of inflammation and tissue damage.
CRP values can change within 24 hours while ESR takes a few days. This difference allows judicious use of these tests.
Their serial estimation helps to monitor disease activity and therapeutic response.
Bone mineral density
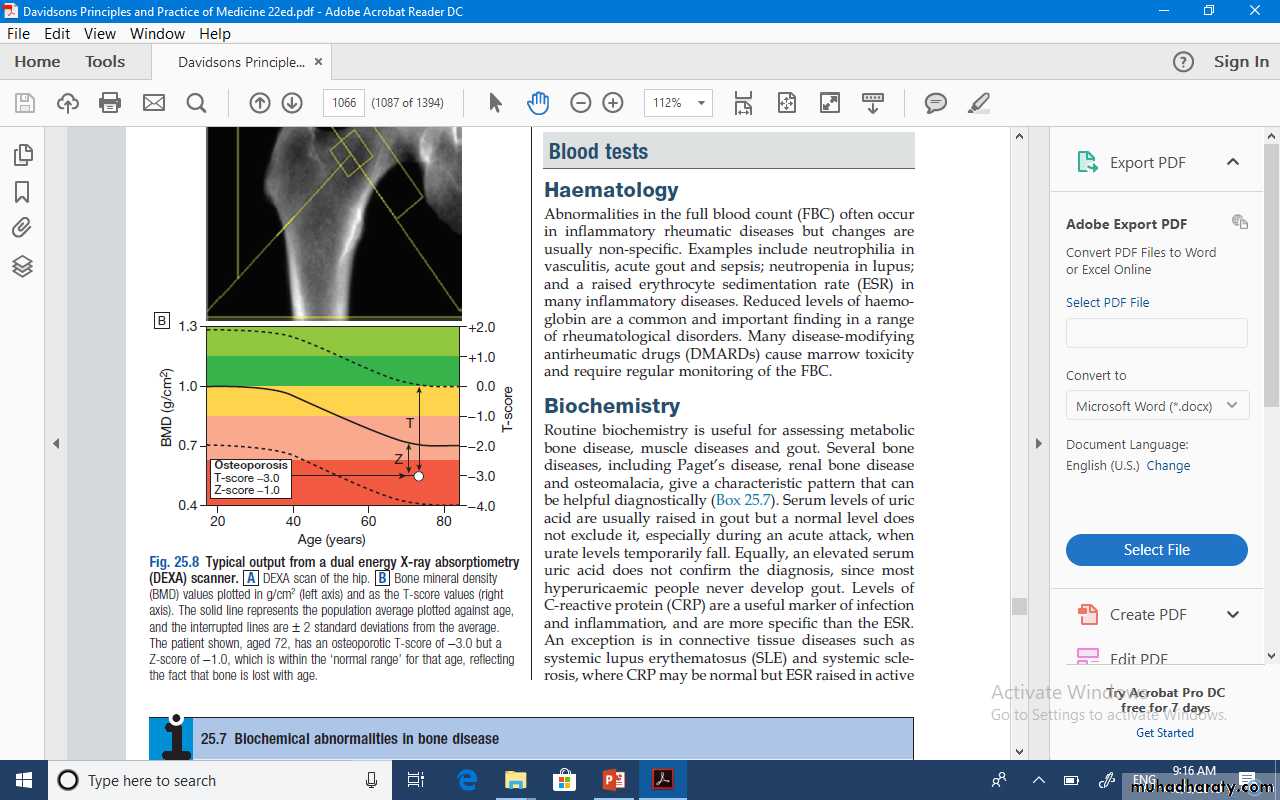
Bone mineral density (BMD) measurements play a key role in the diagnosis and management of osteoporosis.The technique of choice is dual energy X-ray absorptiometry (DEXA), which is usually performed at the lumbar spine and hip.
Most DEXA scanners give a BMD as a T-score and Z-score value.
The T-score is a measure of the number of standard deviations by which the patient’s BMD value differs from that in a young healthy control, whereas the BMD Z-score is a measure of the number of standard deviations by which the BMD deviates from that of age-matched controls
Osteoporosis is defined by a T-score value of -2.5 or below whereas osteopenia is diagnosed when the T-score lies between −1.0 and −2.5
Many healthy people, especially above the age of 50, have BMD values in the osteopenic range.
Values of BMD above −1.0 and below +2.5 are considered normal, whereas values above +2.5 can be found in osteosclerotic diseases and OA
Full blood count (FBC)
patients with inflammation frequently have a leukocytosis or thrombocytosis, most likely reflecting the action of cytokines and other mediators, including glucocorticoids, during this process.With chronic inflammation, anemia of chronic disease can also occur, with the hematocrit in conjunction with the white blood cell and platelet counts pointing to the presence of an inflammatory process.
In systemic lupus erythematosus (SLE), lymphopenia, thrombocytopenia, and low CRP values often characterize active disease, with the discordance between laboratory and clinical findings a clue to diagnosis.
Furthermore, many slow-acting anti rheumatic drugs have bone marrow toxicity requiring regular monitoring of the FBC.
Autoantibodies
Rheumatoid factor (RF) A rheumatoid factor is an antibody, directed against a specific region of the Fc fragment of human IgG.RF was first identified in patients with rheumatoid arthritis
but also occurs in a wide variety of other conditions and in some normal adults .
Importantly, RF is not a 'test for rheumatoid arthritis'. Its principal use is as a prognostic marker; a high titre at presentation associates with a poorer prognosis
Autoantibodies
Antinuclear antibodiesAn antinuclear antibody (ANA) is any autoantibody directed against one or more components of the nucleus . As with RF, the higher the titre of ANA, the greater its significance, although a high titre does not necessarily imply more severe disease.
The many causes of a positive ANA. The most common reason to test for ANA is if lupus is suspected. For lupus, ANA has high sensitivity (virtually 100%) so a negative ANA virtually excludes the diagnosis.
Anti-topoisomerase 1 (also termed Scl-70) is specific for diffuse systemic sclerosis and anti-centromere antibodies are reasonably specific for limited systemic sclerosis.
Antiphospholipid antibodies
These are part of the antiphospholipid syndrome (APS) which is characterised by arterial and venous thromboses, recurrent fetal losses and thrombocytopenia ,This condition may occur in lupus and other autoimmune diseases (secondary APS) or in isolation (primary APS).
Biochemical tests
Serum levels of uric acid are usually raised in patients with acute gout, but a normal level does not exclude the diagnosis. Moreover, a raised uric acid is not sufficient to make a diagnosis of gout since about 95% of subjects with hyperuricaemia never develop the condition.
Serum creatine kinase (CK) levels are an important investigation in patients suspected of having myopathy or myositis.
The skeletal muscle isoform (CK-MM) is much more abundant in health than the cardiac muscle (CK-MB) or brain (CKBB) isoforms.