neurology
DR. Abullah Shakir MahmoodWhat is neurology?
Neurology is the branch of medicine that deals with diseases of nervous system.nervous system consist of :
1. central nervous system (CNS)
2. peripheral nervous system (PNS)
The brain, spinal cord and peripheral nerves combine to allow us to perceive and react to the external world, while maintaining a stable internal environment.
skill is required to identify those neurological symptoms not associated with neurological disease, and to differentiate patients requiring investigation and treatment from those who need reassurance.
it is important to exclude conditions that constitute neurological emergencies If the presentation is not an emergency, more time can be taken to reach a diagnosis.
The history should provide a hypothesis for the site and nature of the potential pathology, which a focused examination may refine and inform what further investigation would be useful.
CNS consist of
Intracranial part:1. cerebrum
2. brain stem
3. cerebellum
Spinal part
FUNCTIONAL ANATOMY AND PHYSIOLOGY
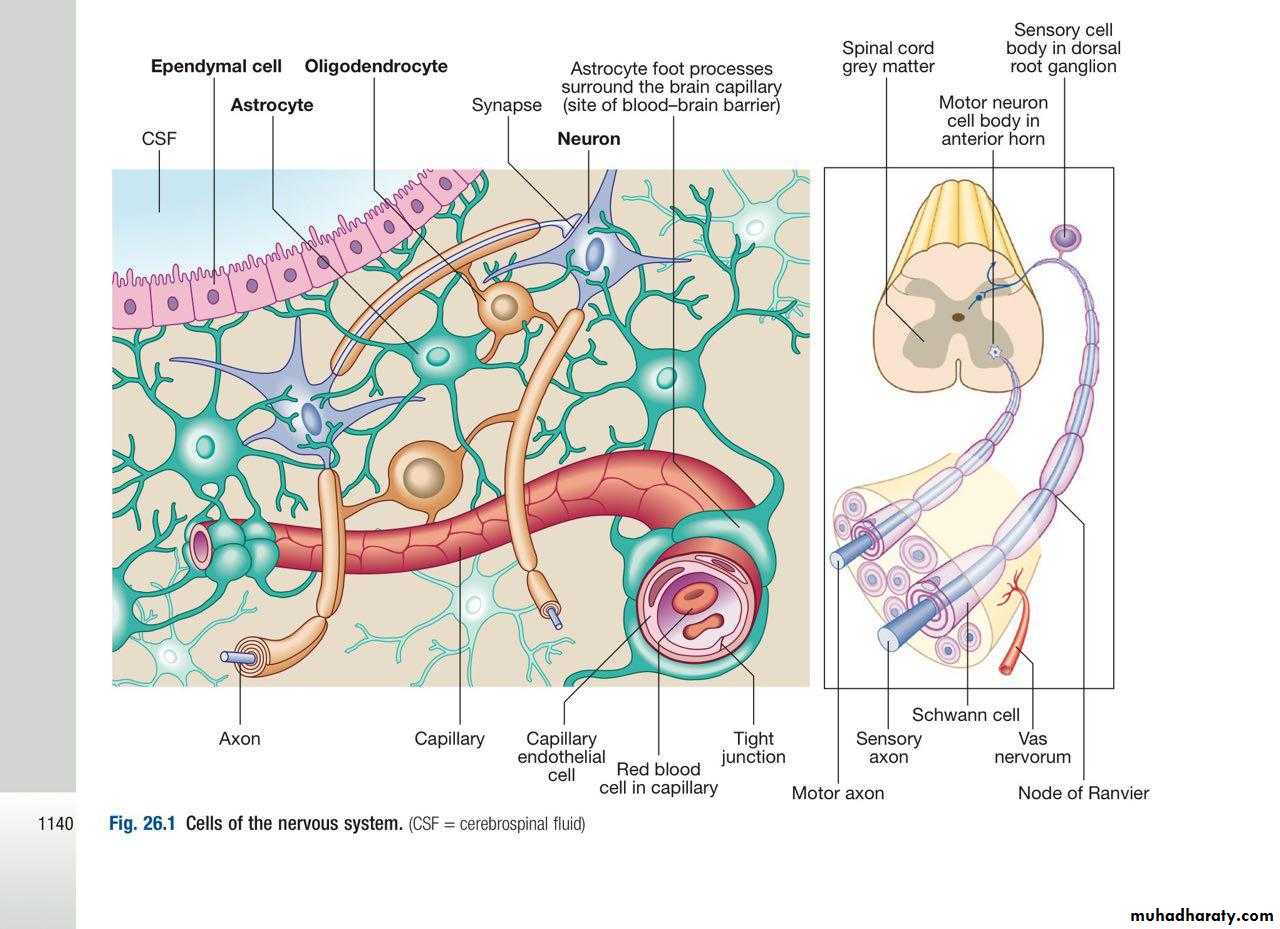
Cells of the nervous system:
The nervous system comprises billions of connections between billions of specialised cells, supplied by a complex network of specialised blood vessels.
In addition to neurons , which is the main cells of nervous systems; there are three types of glial cells:
Astrocytes form the structural framework for neurons and control their biochemical environment. Astrocyte foot processes are intimately associated with blood vessels, forming the blood–brain barrier
Oligodendrocytes are responsible for the formation and maintenance of the myelin sheath, which surrounds axons and is essential for the rapid transmission of action potentials by saltatory conduction.
Microglial cells derive from monocytes/ macrophages and play a role in fighting infection and removing damaged cells.
Peripheral neurons have axons invested in myelin made by Schwann cells.
Ependymal cells line the cerebral ventricles
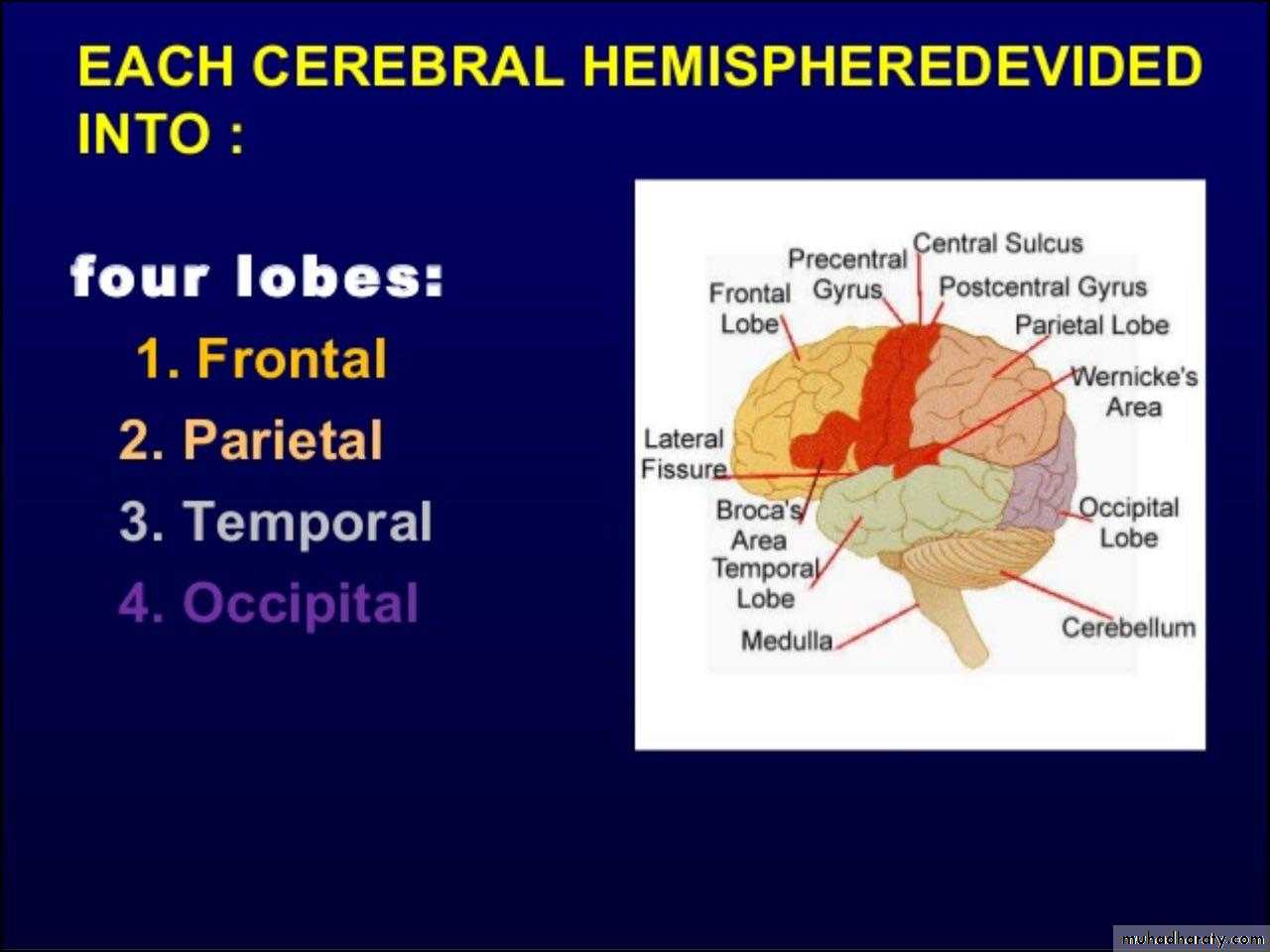
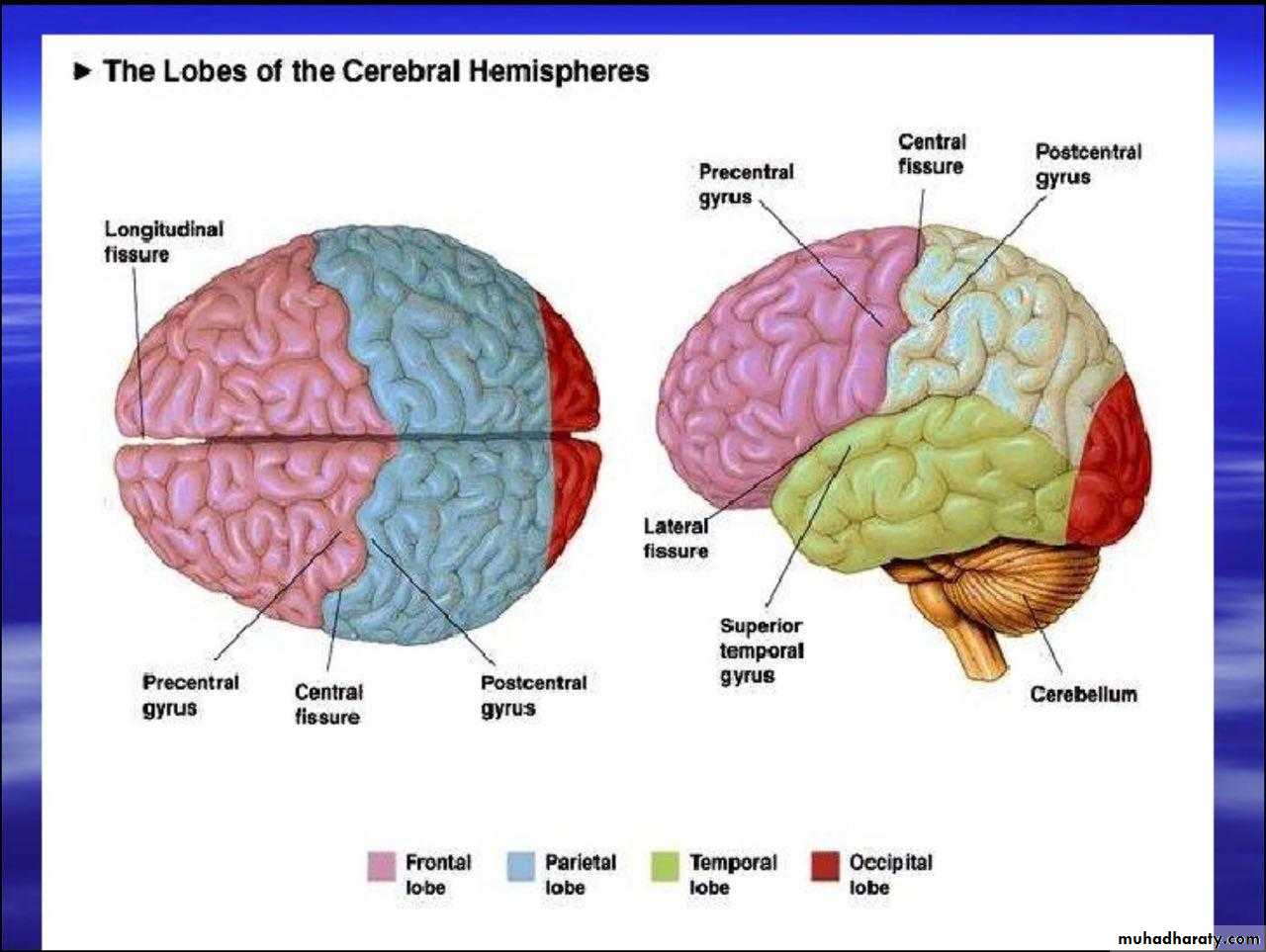
Cerebral hemispheres
The cerebral hemispheres coordinate the highest level of nervous function,the anterior half dealing with executive (‘doing’) functions and the posterior half constructing a perception of the environment
Each cerebral hemisphere has four functionally specialised lobes but some functions are lateralized, and this depends on cerebral dominance (i.e. the hemisphere in which language is represented).
in right-handed individuals the left hemisphere is almost always dominant, while around half of left handers have a dominant right hemisphere.
Frontal lobe
The frontal lobes are concerned with executive function, movement, behaviour and planning.In addition to the primary and supplementary motor cortex, there are specialised areas for the control of eye movements, speech (Broca’s area) and micturition
Parietal lobe
The parietal lobes integrate sensory perception.The primary sensory cortex lies in the post-central gyrus of the parietal lobe.
Much of the remainder is devoted to ‘association’ cortex, which processes and interprets input from the various sensory modalities.
The supra marginal and angular gyri of the dominant parietal lobe form part of the language area .
The non dominant parietal lobe is concerned with spatial awareness and orientation.
temporal lobe
The temporal lobes contain the primary auditory cortex and primary vestibular cortex.On the inner medial sides lie the olfactory cortex and the parahippocampal cortex, which is involved in memory function.
The temporal lobes also contain much of the limbic system, including the hippocampus and the amygdala, which are involved in memory and emotional processing.
The dominant temporal lobe also participates in language functions, particularly verbal comprehension (Wernicke’s area).
Occiptal lobe
The occipital lobes are responsible for visual interpretation.
The contralateral visual hemifield is represented in each primary visual cortex, with surrounding areas processing specific visual sub modalities such as colour, movement or depth, and the analysis of more complex visual patterns such as faces
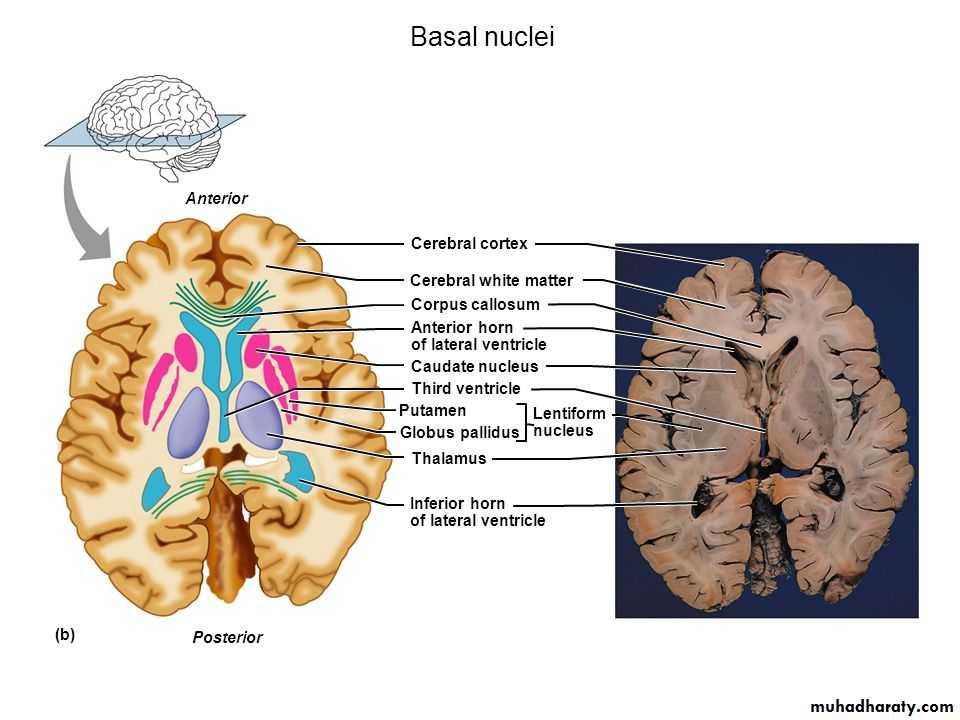
Other important structures
Deep to the grey matter in the cortices, and the white matter are collections of cells known as the basal ganglia that are concerned with motor control;the thalamus, which is responsible for the level of attention to sensory perception;
the limbic system, concerned with emotion and memory; and
the hypothalamus, responsible for homeostasis, such as temperature and appetite control.
The cerebral ventricles contain cerebrospinal fluid (CSF), which cushions the brain during cranial movement .
CSF is formed in the lateral ventricles and protects and nourishes the CNS.
The CSF flows from third to fourth ventricles and through foramina in the brainstem to dissipate over the surface of the CNS, eventually being reabsorbed into the cerebral venous system.
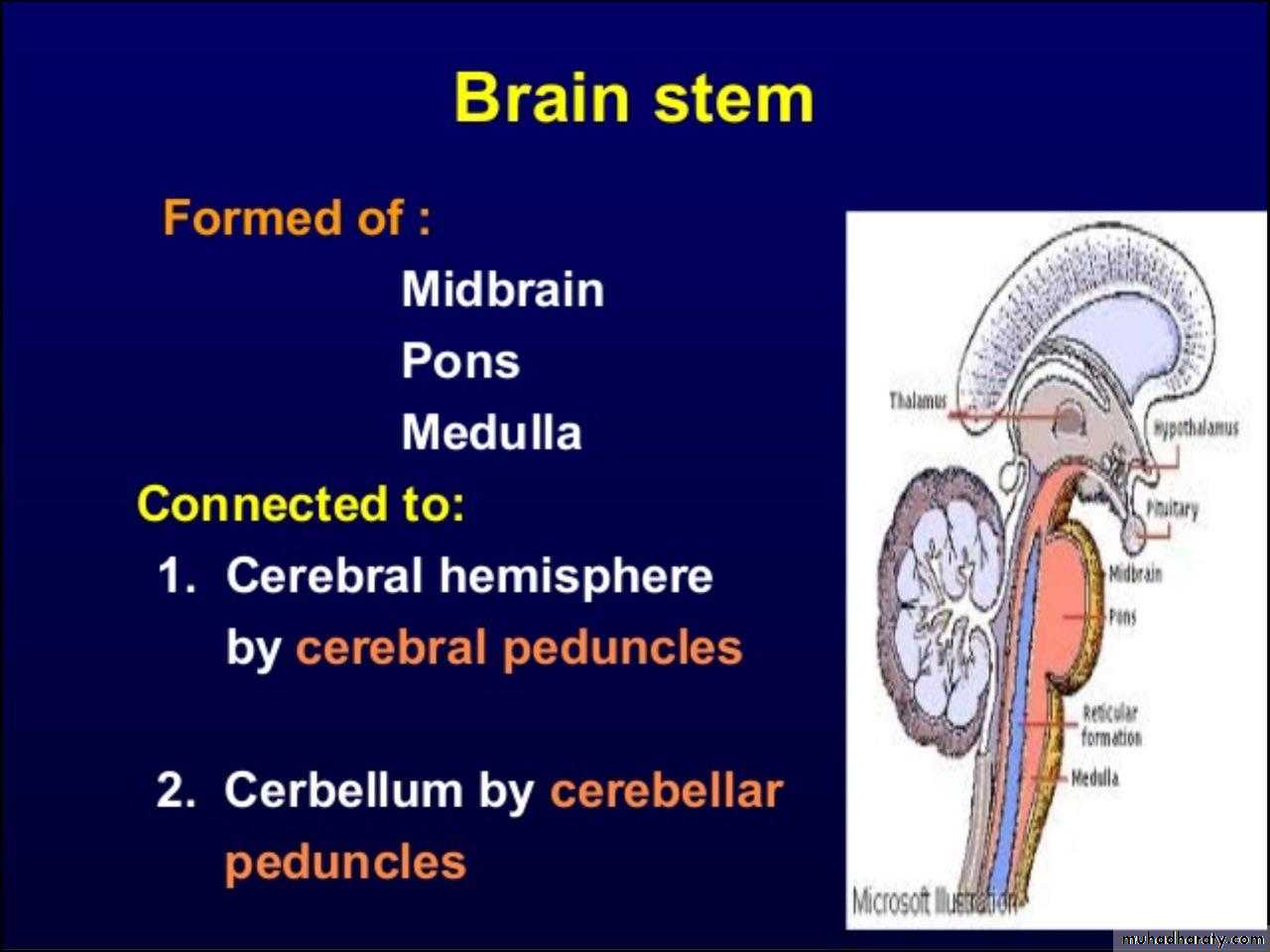
The brainstem
The brainstem containing all the sensory and motor pathways entering and leaving the hemispheres, it also contain the nuclei and projections of the cranial nerves, as well as other important collections of neurons in the reticular formation
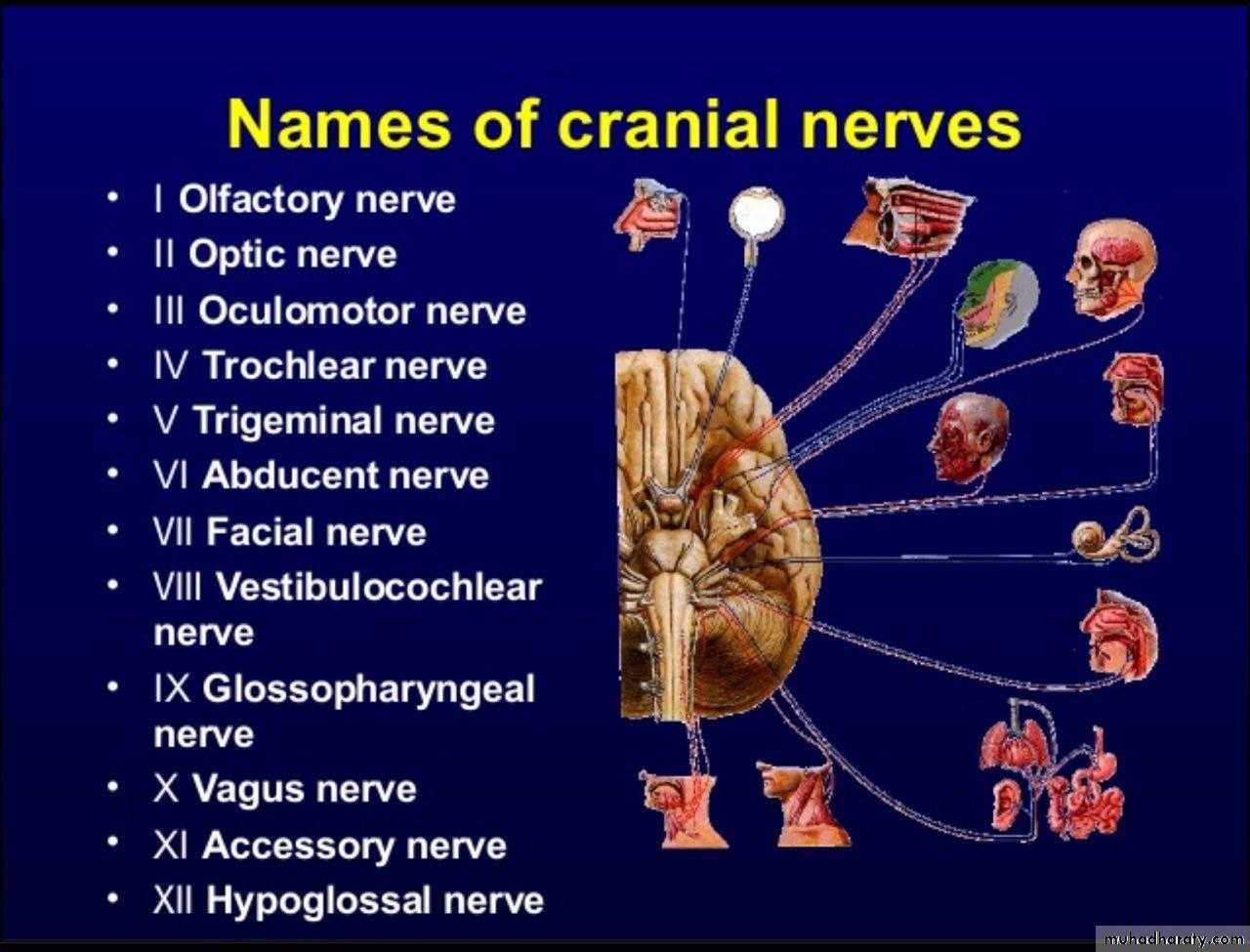
Cranial nerve nuclei provide motor control to muscles of the head (including the face and eyes) and coordinate sensory input from the special sense organs and the face, nose, mouth, larynx and pharynx.
They also relay autonomic messages, including pupillary, salivary and lacrimal functions
The reticular formation is predominantly involved in the control of conjugate eye movements, the maintenance of balance, cardiorespiratory control and the maintenance of arousal.
Cranial nerves emerging from brainstem
3-4 midbrain5- pons
6,7,8 junction of pons and medulla.
9,10,11,12 - medulla
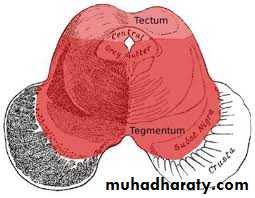
midbrain
It is the upper part of brainstem connect with cerebral hemisphere by cerebral peduncleIt contain cerebral aqueduct which connect between 3rd ventricle and 4th ventricle
It contain nuclei of 3rd and 4th cranial n.s
Pons
Pons lies between midbrain above and medulla below; infront of cerebellum.It contain neural pathways that conduct signals from brain down to cerebellum and medulla.
It contains nuclei that deals with respiration , swallowing , bladder control eye movement etc
Medulla oblongata
Located in the hind brain anterior to cerebellumContains cardiac , respiratory , vomiting and vasomotor centers and thus deals with breathing , heart rate , bl. preasure
It contain nuclei of the lower cranial n. (9-10-11-12)
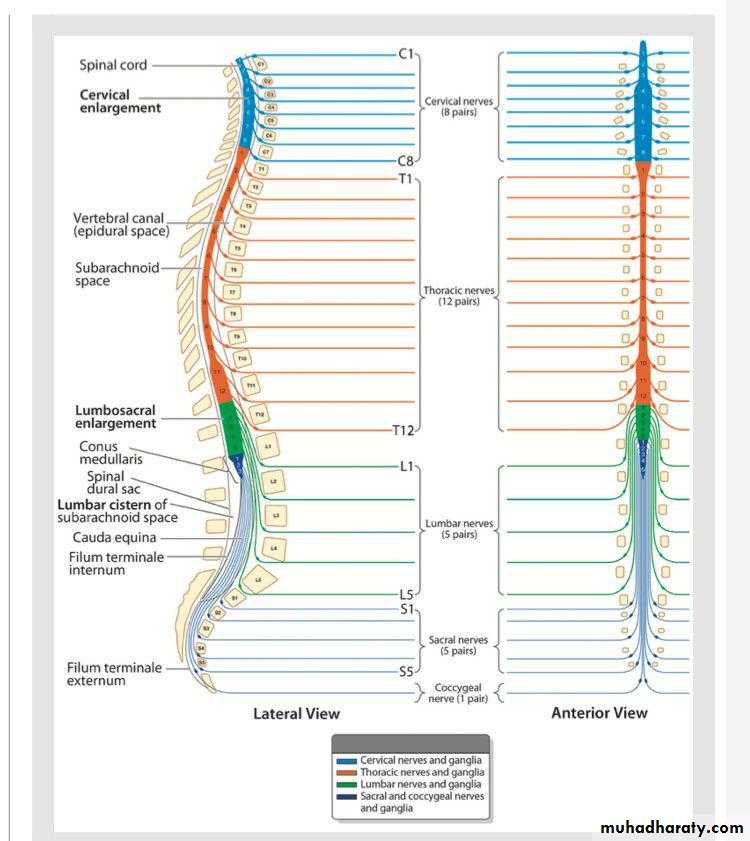
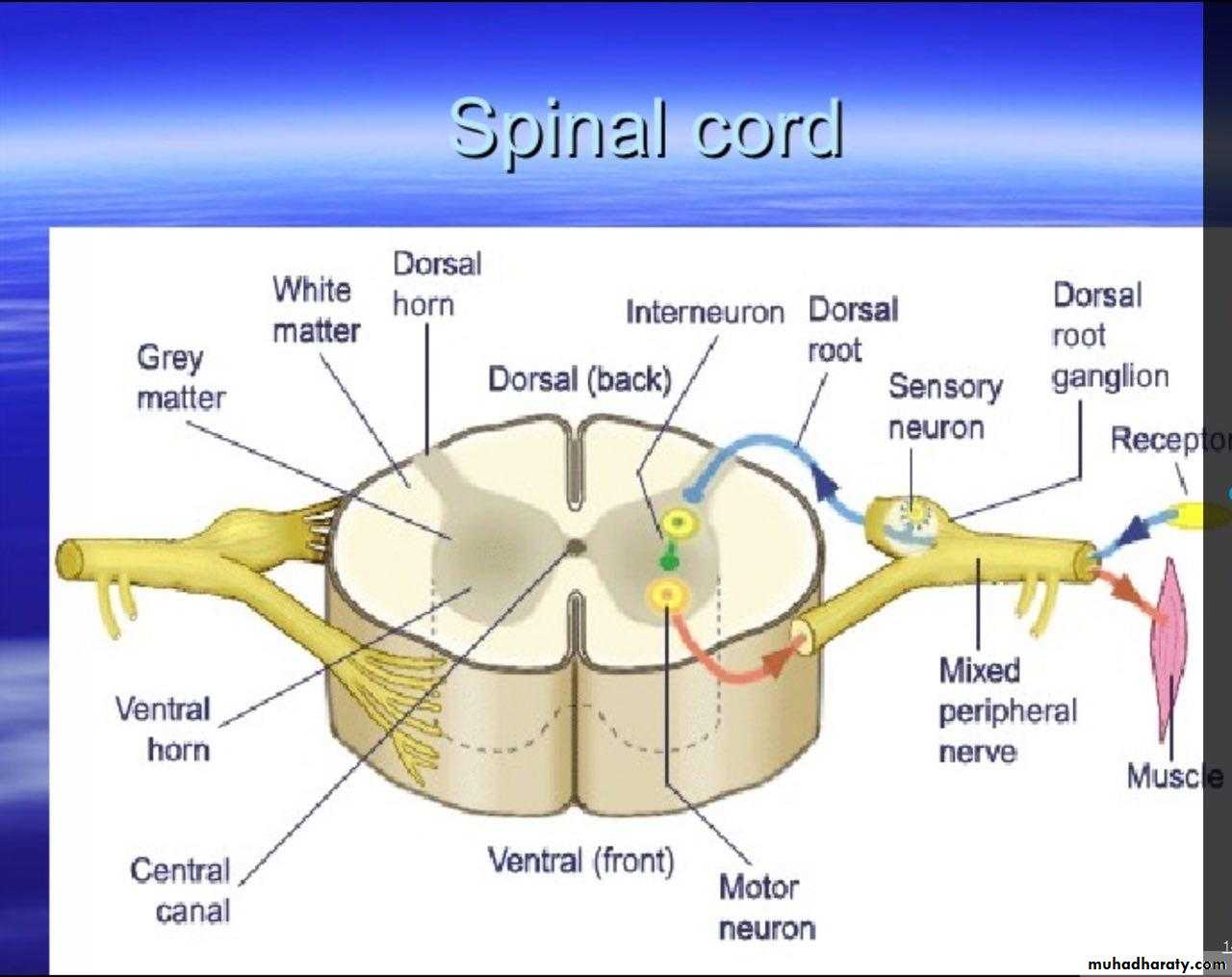
Spinal cord
There are 31 spinal cord segments (eight cervical, twelve thoracic, five lumbar, five sacral, and one coccygeal.each segment has a pair of dorsal (sensory) and ventral (motor) roots that join to form a mixed spinal nerve just as they enter the dural sleeve and neural foramina
Spinal nerves divided into dorsal and ventral roots near to the cord.
Dorsal roots carry afferent fibers
Ventral roots carry efferent fibers
Ascending tract:
Dorsal columns(vibration and position sensation)
Spinothalamic ( pain and tempresure)
Spinocerebellar
Descending tract:
Corticospinal
Sensory peripheral nervous system
The sensory cell bodies of peripheral nerves are situated just outside the spinal cord, in the dorsal root ganglia in the spinal exit foramina, whilst the distal ends of their neurons utilise various specialised endings for the conversion of external stimuli into action potentials.Sensory nerves consist of a combination of large, fast, myelinated axons (which carry information about joint position sense and commands to muscles) and smaller, slower, unmyelinated axons (which carry information about pain and temperature, as well as autonomic function).
Motor peripheral nervous system
The anterior horns of the spinal cord comprise lower motor cell bodies.To increase conduction speed, peripheral motor nerve axons are wrapped in myelin produced by Schwann cells.
Motor neurons release acetylcholine across the neuromuscular junction, which changes the muscle end-plate potential and initiates muscle contraction.
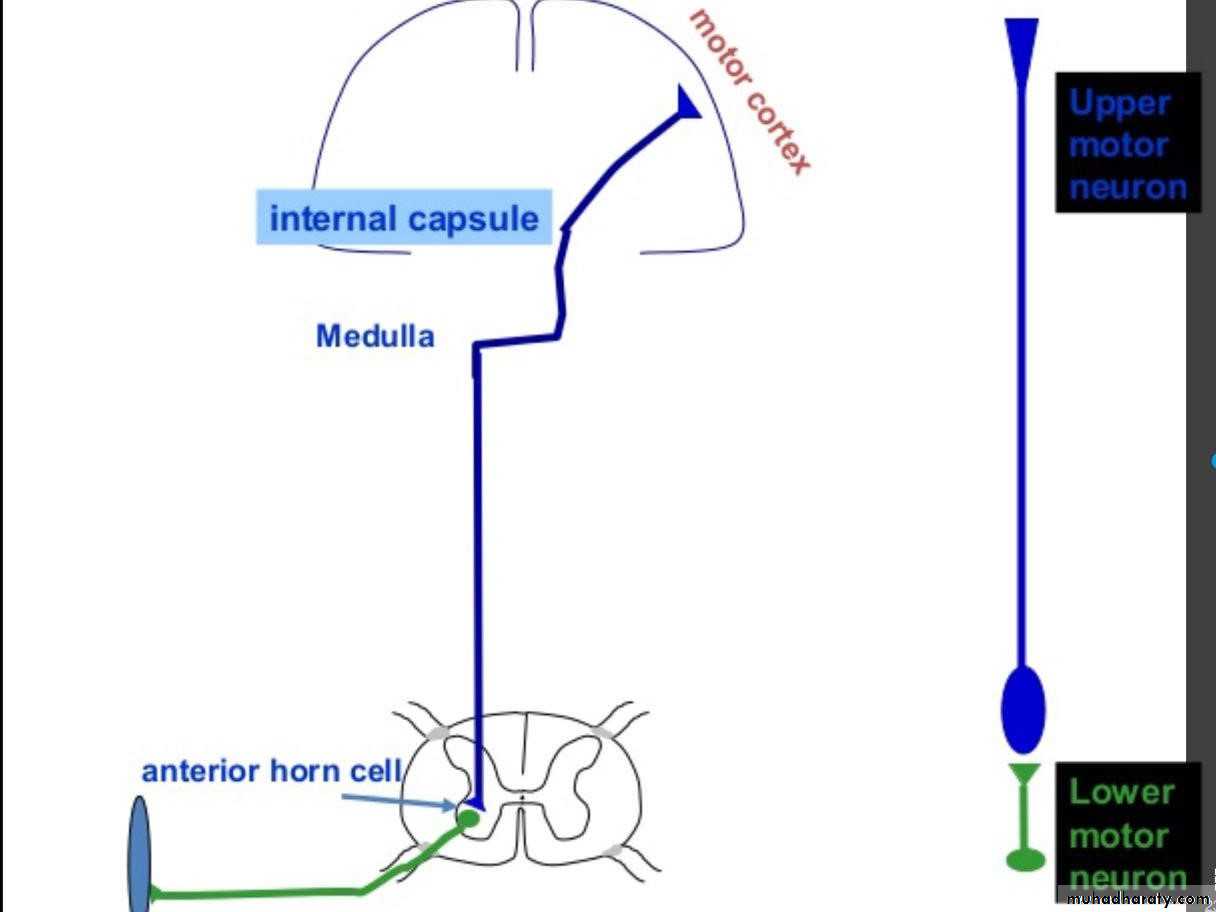
The motor system
A programme of movement formulated by the premotor cortex is converted into a series of signals in the motor cortex that are transmitted to the spinal cord in the pyramidal tract.This passes through the internal capsule and the ventral brainstem before decussating in the medulla to enter the lateral columns of the spinal cord.
The pyramidal tract ‘upper motor neurons’ synapse with the anterior horn cells of the spinal cord grey matter, which form the lower motor neurons.
Any movement necessitates changes in posture and muscle tone, sometimes in quite separate muscle groups to those involved in the actual movement.
Upper motor neurons
Upper motor neurons have both inhibitory and excitatory influence on the function of anterior horn motor neurons.Lesions affecting the upper motor neuron result in increased tone, most evident in the strongest muscle groups (i.e. the extensors of the lower limbs and the flexors of the upper limbs).
upper motor neuron lesion lead to Loss of inhibition which lead to brisk reflexes.
The increased tone is more apparent during rapid stretching (‘spastic catch’), but may suddenly give way with sustained tension (the ‘clasp-knife’ phenomenon).
More primitive reflexes are also released, manifest as extensor plantar responses.
Spasticity may not be present until some weeks after the onset of an upper motor neuron lesion.
Lower motor neurons
Lower motor neurons in the anterior horn of the spinal cord innervate a group of muscle fibres termed a ‘motor unit’.Loss of lower motor neurons causes loss of contraction within this unit, resulting in weakness and reduced muscle tone.
Subsequently, denervated muscle fibres atrophy, causing muscle wasting, and depolarise spontaneously, causing ‘ fasciculations .
The extrapyramidal system
Circuits between the basal ganglia and the motor cortex constitute the extrapyramidal system, which controls muscle tone, body posture and the initiation of movement.Lesions of the extrapyramidal system produce an increase in tone that is continuous throughout the range of movement at any speed of stretch (‘lead pipe’ rigidity).
Involuntary movements are also a feature of extrapyramidal lesions and tremor in combination with rigidity produces typical ‘cogwheel’ rigidity.
Extrapyramidal lesions also cause slowed and clumsy movements (bradykinesia), which characteristically reduce in size with repetition, as well as postural instability, which can precipitate falls.
The autonomic system
The autonomic system regulates the cardiovascular and respiratory systems, the smooth muscle of the gastrointestinal tract, and many exocrine and endocrine glands throughout the body.
The autonomic system is controlled centrally by diffuse modulatory systems in the brainstem, limbic system and hypothalamus.
Autonomic output divides functionally and pharmacologically into two divisions: the parasympathetic and sympathetic systems
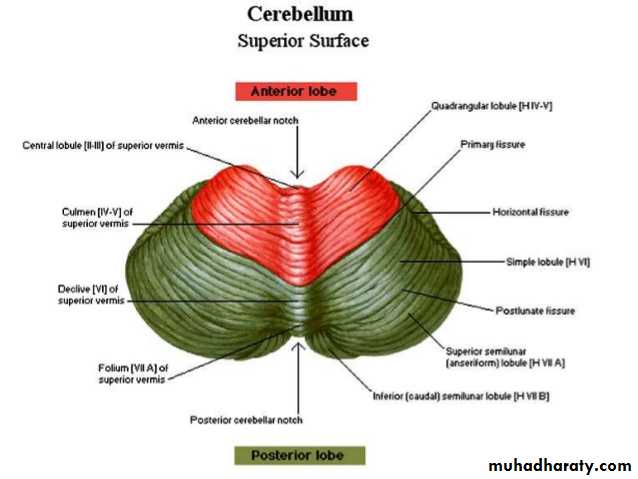
The cerebellum
The cerebellum fine-tunes and coordinates movements initiated by the motor cortex including speech.A lesion in a cerebellar hemisphere causes lack of coordination on the same side of the body.
Cerebellar dysfunction impairs the smoothness of eye movements, causing nystagmus and renders speech dysarthric.
In the limbs, the initial movement is normal, but as the target is approached, the accuracy of the movement deteriorates, producing an ‘intention tremor’.
The distances of targets are misjudged (dysmetria), resulting in ‘past-pointing’.
The ability to produce rapid, accurate, regularly alternating movements is also impaired (dysdiadochokinesis).
The central vermis of the cerebellum is concerned with the coordination of gait and posture; Disorders of this therefore produce a characteristic ataxic gait (see below).
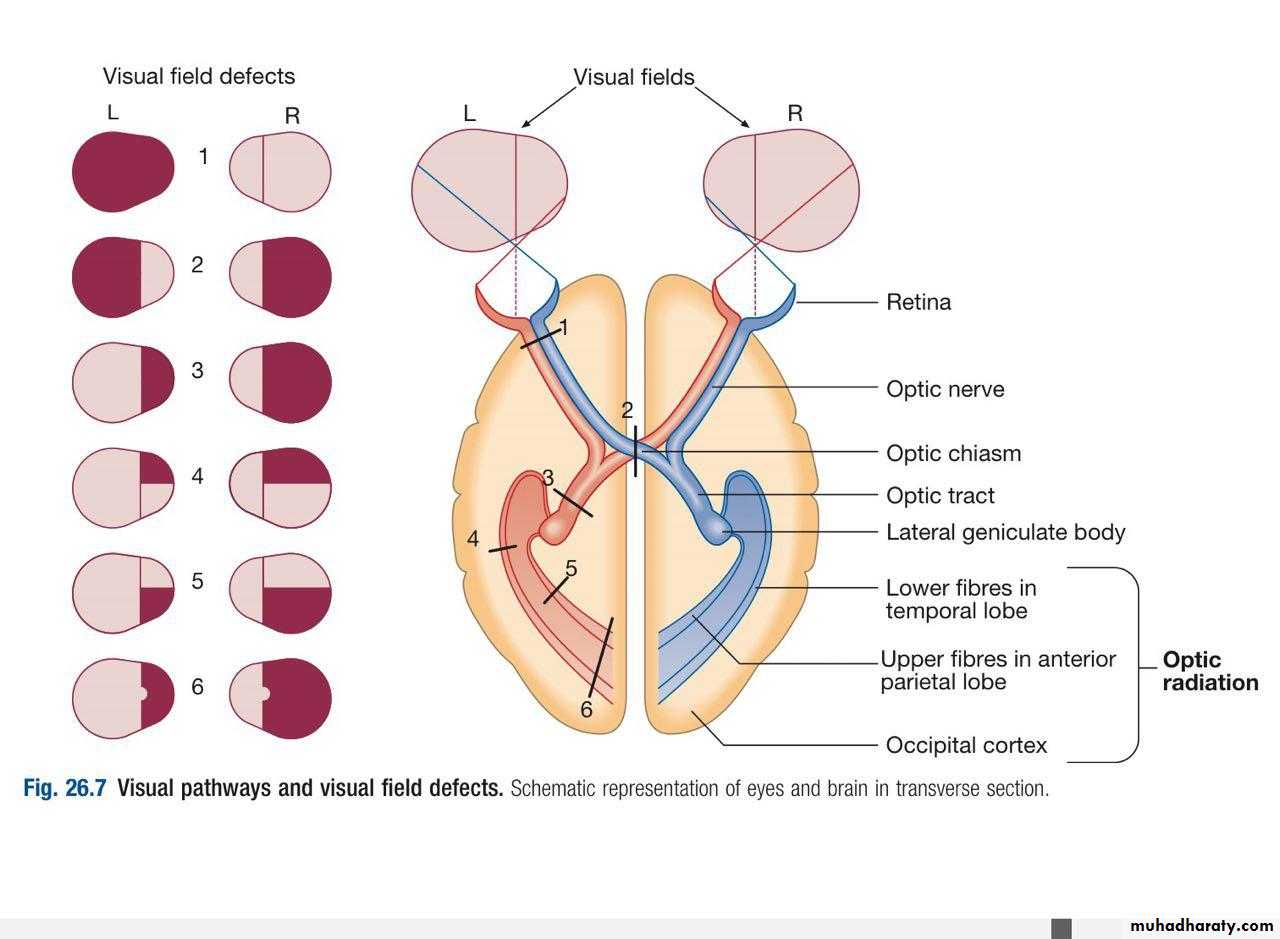
vision
visual pathways start by Fibers from ganglion cells in the retina pass to the optic disc and then backwards through to the optic nerve.Nasal optic nerve fibers (subserving the temporal visual field) cross at the chiasm, but temporal fibers do not. Hence, fibers in each optic tract and further posteriorly carry representation of contralateral visual space.
From the lateral geniculate nucleus, lower fibers pass through the temporal lobes on their way to the primary visual area in the occipital cortex,
while the upper fibers pass through the parietal lobe.
Normally, the eyes move conjugately (in unison), though horizontal convergence allows visual fusion of objects at different distances.
The control of eye movements begins in the cerebral hemispheres, particularly within the frontal eye fields, and the pathway then descends to the brainstem .
Horizontal and vertical gaze centres in the pons and mid-brain, respectively, coordinate output to the ocular motor nerve nuclei (3, 4 and 6), which are connected to each other by the medial longitudinal fasciculus (MLF).
The MLF is particularly important in coordinating horizontal movements of the eyes.
The extraocular muscles are then supplied by the oculomotor(3rd), trochlear (4th) and abducent (6th) cranial nerves.
Sphincter control
The sympathetic supply to the bladder leaves from T11–L2 to synapse in the inferior hypogastric plexus, while the parasympathetic supply leaves from S2–4.In addition, a somatic supply to the external (voluntary) sphincter arises from S2–4, travelling via the pudendal nerves.
Storage of urine is maintained by inhibiting parasympathetic activity and thus relaxing the detrusor muscle of the bladder wall.
Continence is maintained by simultaneous sympathetic and somatic (via the pudendal nerve) mediated tonic contraction of the urethral sphincters.
Voiding is usually under conscious control, and triggered by relaxation of tonic inhibition on the pontine micturition center from higher centers, leading to relaxation of the pelvic floor muscles and external and internal urethral sphincters, along with parasympathetic mediated detrusor contraction.
INVESTIGATION OF NEUROLOGICAL DISEASE
Experienced clinicians will make around 90% of neurological diagnoses on history alone, with a lesser contribution from examination and investigation.Investigation may include assessment of structure (imaging) and function (neurophysiology).
including X-rays (plain X-rays, computed tomography (CT), CT angiography, myelography and angiography),
magnetic resonance (MR imaging (MRI), MR angiography (MRA)) and ultrasound (Doppler imaging of blood vessels).
It is now possible to use imaging techniques to assess
CNS function. Single photon emission clinical tomography(SPECT)
Functional MRI (fMRI) can be used to assess blood flow during specific tasks
Plain skull X-rays are now largely restricted to the diagnosis of fractures and sinus disease.
CT will show bone and calcification well, and will easily image collections of blood.
It will also detect abnormalities of the brain and ventricles, such as atrophy, tumours, cysts, abscesses, vascular lesions and hydrocephalus.
MRI resolution is unaffected by bone and so is more useful in the investigation of posterior fossa disease.
Its sensitivity to cortical and white matter changes makes it effective in picking up inflammatory conditions such as multiple sclerosis, and in investigating epilepsy.
Myelography is an invasive technique involving injection of contrast into the lumbar theca.
Neurophysiological testing
Electroencephalography (EEG):it is used to detect electrical activity arising in the cerebral cortex
EEG is at its most useful when it captures activity during one of the events in question.
Up to 5% of some normal populations may demonstrate epileptiform discharges on EEG which prevent its use as a screening test for epilepsy.
Over 50% of patients with proven epilepsy will have a normal ‘routine’ EEG, and, conversely, the presence of epileptiform features does not of itself make a diagnosis (most notably in younger patients with a family history of epilepsy)
The EEG in epilepsy is predominantly used in its classification and prognosis, and in some patients to localize the seat of epileptiform discharges when surgery is being considered.
Nerve conduction studies
Electrical stimulation of a nerve causes an impulse to travel both efferently and afferently along the underlying axons.Nerve conduction studies (NCS) make use of this, recording action potentials as they pass along peripheral nerves
If the recorded potential is smaller than expected, this provides evidence of a reduction in the overall number of functioning axons. Significant slowing of conduction velocity, in contrast, suggests impaired saltatory conduction due to peripheral nerve demyelination.
It aid to diagnose peripheral neuropathy , compression neuropathy
Root lesion , guillian barre disease etc..
Electromyography (EMG) is usually performed with NCS, and involves needle recording of muscle electrical potential during rest and contraction.
It may aid in the diagnosis of nerve compression or injury
In myopathic disease
In motor neuron disease
In neuromuscular junction disease
Lumbar puncture
Lumbar puncture (LP) is the technique used to obtain a CSF sample and provides an indirect measure of intracranial pressure.CSF is normally clear and colour less.
Pressure 50–250 mm of water
Red cell count (× 106/L) 0–4
White cell Count (× 106/L) 0-4 mainly lymphocyte.
Glucose > 50–60% of blood level
Protein < 0.45 g/L
Microbiology Sterile
Oligoclonal bands Negative
Routine analysis will involve a cell count, as well as assay of glucoseand protein.
CSF assessment is important in investigating infections (meningitis or encephalitis), subarachnoid haemorrhage and inflammatory conditions (multiple sclerosis, sarcoidosis and cerebral lupus).
If there is a cranial space-occupying lesion causing raised intracranial pressure, LP presents a theoretical risk of downward shift of intracerebral contents, a potentially fatal process known as coning .
Consequently, LP is contraindicated if there is any clinical suggestion of raised intracranial pressure (papilledema), depressed level of consciousness, or focal neurological signs suggesting a cerebral lesion, until imaging (by CT or MRI) has excluded a space occupying lesion or hydrocephalus.
When there is a risk of local hemorrhage (thrombocytopenia, disseminated intravascular coagulation or anticoagulant treatment), then caution should be exercised or specific measures should be taken.
LP can be safely performed in patients on antiplatelet drugs or low-dose heparin, but may be unsafe in patients who are fully anticoagulated due to the increased risk of epidural haematoma
Evoked potentials
The cortical response to visual, auditory or electrical stimulation can be measured on an EEG as an evoked potential (EP
In practice, visual evoked potentials (VEPs) are most commonly used to help differentiate CNS demyelination from small-vessel white-matter changes
Biopsy
Biopsies of nervous tissue (peripheral nerve, muscle, meninges or brain) are occasionally required for diagnosis.Nerve biopsy can help in the investigation of peripheral neuropathy.
Histological examination can help identify underlying causes, such as vasculitides or infiltrative disorders like amyloid.
Muscle biopsy is performed more frequently and is indicated for the differentiation of myopathies types.
The quadriceps muscle is most commonly biopsied but other muscles may also be sampled if they are involved clinically.
Brain biopsy is required when imaging fails to clarify the nature of intracerebral lesions: for example, in unexplained degenerative diseases such as unusual cases of dementia and in patients with brain tumour.