Orthopedics
Principle of FracturesDr. Ali Khairaldeen
Definition: A fracture is a break in the structural continuity of a bone.
It can be classified depending on the basis of:Aetiology ( Traumatic, fragility, Stress and Pathological fractures)
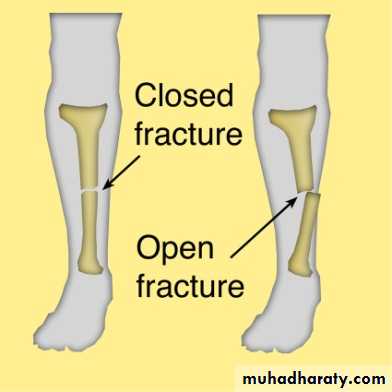
Relationship of the fracture with the external environment (closed, open fracture)
If the overlying skin remains intact it is closed (simple) fracture.
If the skin break it is an open (compound) fracture.
Pattern of the fracture ( complete fracture: transverse, spiral and oblique;……. incomplete : green stick fracture)
Fractures are variable in appearance but for practical reasons they are divided into two well-defined groups.
COMPLETE FRACTURES: the bone is split into two or more fragments.
INCOMPLETE FRACTURES: here the bone is incompletely divided and the periosteum remains in continuity. In children a greenstick fracture the bone is buckled or bent (like snapping a green twig).
How fracture happen? Aetiology of fractures
From single Traumatic incident.Direct trauma b. indirect trauma
Fragility fractures
Repetitive Stress (fatigue).
Abnormal weakening of the bone, (Pathological fracture).
1. Traumatic fracture
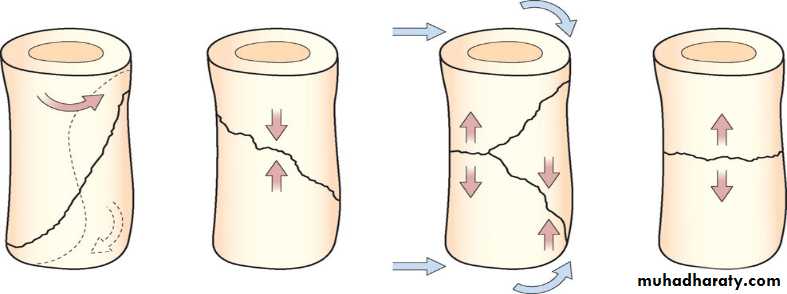
Most fractures are due to combination of forces (twisting, compression, bending or tension)
The x- ray pattern may suggest the dominant mechanism:
Twisting cause spiral fractureCompression cause short oblique fracture
Bending cause fracture with triangular butterfly fragment.
Tension cause transverse fracture
This description applies mainly to the long bones.
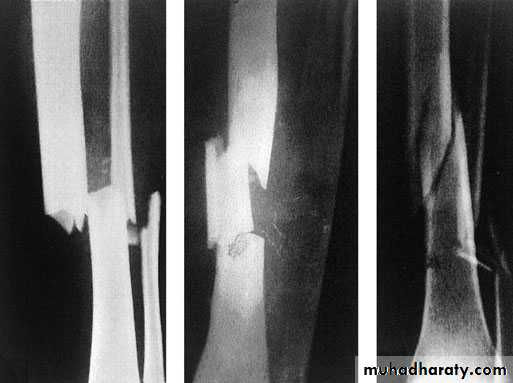
Transverse segmental spiral Greenstick fracture
A cancellous bone when subjected to sufficient force sustains a comminuted crush fracture.
Avulsion fracture my result when there is resisted muscle action may pull off the bony attachment of the muscle.
2. Fragility (low energy) fractures
Osteoporosis is a common disease in the elderly and is now recognised as the major factor to rising the number of so-called fragile fractures.The condition is characterized by loss of trabecular bone mass and connectivity as well as thinning of the cortical bone.
The commonest fragility fractures:
Colles fracture
Femoral neck fracture
Thoracic and lumbar vertebrae fractures
3. Stress fractures
Fatigue or stress fractures can occur in metal and other materials due to gradual rearrangement of molecular structure which weaken the metal and permit the crack to occur.
A similar mechanism of crack can occur in bone.
These fractures occur in Normal bone which is subject to repeated stress, typically seen in athletes or military personnel.
This is most seen in tibia, fibula and metatarsal.
The great difference between stress and traumatic fractures is that there is no single specific injury in case of fatigue fractures, the onset of pain is gradual and increase by activity and relieved by rest.
Examination reveals local tenderness over the affected bone. X-ray finding may be normal at first time and after 2-4 weeks the radiological changes appear as a faint hairline crack surrounded by callus, occasionally if a biopsy taken from the callus may be mistaken to diagnosed as a bone sarcoma!!!!). A mistake that should not occur if the feature of stress fracture are properly understood.
Treatment: rest + non-steroidal anti inflammatory drugs
4. Pathological fractures
Fractures may occur even with normal stresses if the bone has been weakened by a disease that cause changes in its structure.The underlying disease may be local (bone cyst). Or generalized disorder affecting several bones or whole skeleton e.g. osteogenesis imperfecta or Paget’s disease.
Osteomalacia
Metastasis non-ossifying fibroma
Causes of pathological fractures
Local disease of bone:
Infection ( osteomylitis)
Benign tumours like ( Chondroma, haemangioma)
Malignant bone tumours like (osteosarcoma, Ewing sarcoma, metastatic carcinoma)
Miscellaneous like ( simple bone cyst, monostotic fibrous dysplasia)
General affection of the skeleton:
Congenital disorder like ( osteogenesis imperfect)
Diffuse bone weakening ( osteoporosis, Cushing's syndrome, osteomalacia)
Tumours ( multiple myeloma)
Miscellaneous like ( Paget's disease, polyostotic fibrous dysplasia
How the fractures are displaced?
After a complete fracture the fragment usually displacedPartly by the force of injury
Partly by gravity
Partly by pull of muscles attached to them.
Displacement usually described in terms of:
Translation (shift).Alignment (angulations).
Rotation (twist).
Length.
How the fractures heal:
The process of fracture repair varies according to the type of bone involved and the amount of movement at the fracture site.
In a tubular bone and in the absence of rigid fixation healing proceeds in five stages (indirect healing):
Tissue destruction and haematoma formation.
Inflammation and cellular proliferation: start 8 hours after injury as acute inflammatory reaction and cellular proliferation.
Callus formation: the proliferating cells is potentially chondrogenic and osteogenic and start to form primitive bone (woven bone) which will splint the broken bone.
Consolidation: the woven bone replaced by lamellar bone by active osteoblastic and osteoclastic activity.
Remodeling: the bone restore its normal shape and the medullary canal opened through the process of resorption and formation. This occur over a period of months or years.
In healing of fractures under rigid fixation and compression the bone heal without callus the forming cell, cross directly from one fragment to other (direct healing or union).
Timetable for fracture healing:
How long does the fracture take to unite and consolidate?No precise answer is possible.
It depends on: Age, blood supply, type of fracture and other factors
Perkins’ can give us approximate time for healing:
Perkin’s timetable…………………………………………………………………………………………..
A spiral fracture in the upper limb unite within 3 weeks; for consolidation multiply by 2:
3 * 2 = 6 weeks for consolidation
Transverse fracture upper limb multiply by 2:
2 * 3 = 6 weeks need for union
For consolidation multiply by 2:
6 * 2 = 12 weeks
……………………………………………………………………………………………..
For lower limb multiply by 2 again.
Spiral fracture lower limb:
3 * 2 = 6 weeks for union
6 * 2 = 12 weeks for consolidation
For transverse fracture multiply by 2 again.
6 * 2 = 12 weeks for union12 * 2 = 24 weeks for consolidation
Factors affects fracture healing
Age of the patient: in children fractures usually healed faster than same fractures if happen in old age.Constitution of fracture: simple fractures with limited soft tissue damage healed faster than fractures with sever soft tissue damage.
Shape of the fractures: spiral fractures healed faster than transverse fracture this is due to bigger surface area in spiral fractures.
Site of the fracture: very important in healing of the fractures e.g intracapsular fracture neck femur heal slowly or it will end with nonunion, and this is due to the blood supply i.e more blood supply to the fracture mean quicker healing.
Apposition of the fracture: if the two ends of the fracture in contact and in good alignment so the fracture will heal faster than if the two segment in displaced and not contact
Immobilization: is necessary for fracture healing excessive movement at the fracture site can cause non union
General condition of the patients and disease like DM, renal failure, liver disease.
Patients on steroid therapy, immune suppressant drugs.
Diet
Clinical features for fracture
History:
General sign:
Local sign: look, feel, move
X-ray
Special imaging
History: Usually there is a history of injury (in traumatic fractures) followed by inability to use the injured limb.
BE WARE ……
The fracture is not always at the site of the injury, a blow to the knee may fracture the patella, femoral condyle, even the acetabulum.General signs
A broken bone is part of a patient, so look for:
Hemorrhage.
Associated damage to spinal cord, viscera.
Predisposing cause.( Bone disease).
Local signs
Look: swelling, brusing, deformity, state of the skin.Feel: tenderness, distal pulse, and sensation
Move: crepitus and abnormal movement, check for movement of the joint distal to the injury.
hX-Ray: X-ray examination is mandatory. Remember the ruleof twos:
Two views – A fracture or a dislocation may not beseen on a single x-ray film, and at least two views (anteroposterior and lateral) must be taken.
Two joints – In the forearm or leg, one bone may befractured and angulated. Angulation, however, is impossible unless the other bone is also broken, or a joint dislocated. The joints above and below the fracture must both be included on the x-ray films.
Two limbs – In children, the appearance of immature epiphyses may confuse the diagnosis of a fracture; x-rays of the uninjured limb are needed for comparison.
Two injuries – Severe force often causes injuries at more than one level. Thus, with fractures of the calcaneum or femur it is important to also x-ray the pelvis and spine
Two occasions – Some fractures are difficult to detect at time of injury, but another x-ray examination a week or two later may show the lesion. Common examples are scaphoid, femoral neck and lateral malleolus, and also stress fractures and physeal injuries wherever they occur.
Special imaging:
TOMOGRAPHY: In spine or tibial condyle injure.
CT / M.R.I.: In spine fracture which threatened the cord.
RADIO- ISOTOP scanning: In stress fracture or undisplaced fracture.
Treatment of close fractures
The objects of treatment of close fracture are
Reduce the fracture
Immobilize the fracture
Exercise
Treatment of closed fractures
Reduce
Close method
Should be done as early as possible, it is not indicated when the fracture is undisplaced or minimally displaced.
Close reduction: under GA and muscle relaxation
Pull the distal part of the limb in the line of bone
The fragment is disengaged and repositioned
Alignment is adjusted in each plain
After reduction the limb hold by splitage
Open reduction...indication of open reduction:
Failure of close reduction
Intra- articular fracture
Avulsion fracture
Hold ( immobilization)
Splintage
Traction
Internal fixation
External fixation
Functional brace
Exercise
It mean restore function, not only the injured part but the patient as whole.
The objectives are to reduce the oedema, preserve the joint movement, restore muscle power.
This can be done by elevation, active exercise assisted movement.
………………………………………………………………………………………………….
The problem is how to hold the limb adequately and yet use the limb sufficiently:
This conflict (hold versus move) which the surgeon seek to resolve as rapidly as possible by (internal fixation)
But we also want to avoid unnecessary risk here is a second conflict (speed versus safety)
Fracture quartet
Cast splintage:
Plaster of Paris is still widely used as a splint especially for children’s fractures
Advantages: safe, patient can go home sooner
Disadvantage “fracture disease” i.e. stiffness (move).
Complications:
Tight casting
Pressure sore
Skin abrasion
Loose cast
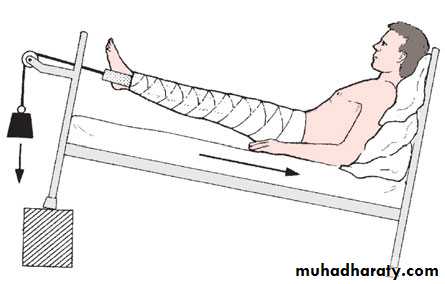
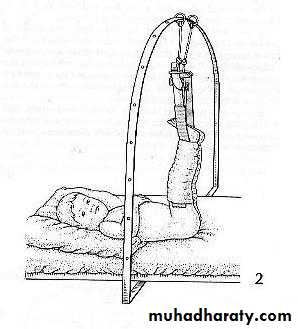
Continuous traction:
Traction is applied to the limb distal to the fracture.
Advantage: it is safe, patient can move the joint and exercise his or her muscles.
Disadvantage is the speed (traction keep the patient in the hospital.
Types of traction:
Traction by gravity
Skin traction
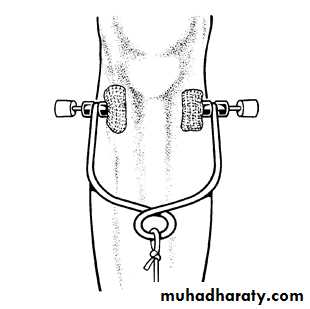
Skeletal traction
Fixed traction
Balanced traction
Combined traction
COMPLICATIONS of skin and skeletal
May constrict circulation (gallows traction).
Nerve injuries (peroneal).
Pin site infection (in skeletal traction).
Functional bracing:
Segments of cast are applied only over the shaft of the bone, leaving the joint free; the cast segments are connected by metal or plastic hinges which allow movements in on plane.Is one way of preventing joint stiffness while still permitting fracture splintage and loading.
E.g. (fracture femur, fracture tibia).
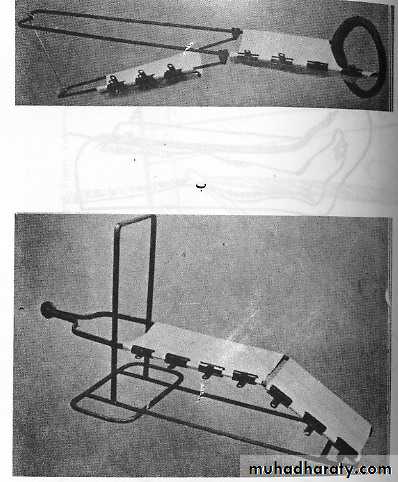
Skin traction not more than (4-5KG) e.g. Traction by gravity
Balanced traction
Fixed traction
Thomas splint. And Bohler splint
Skeletal traction
Gallose traction
Functional bracing
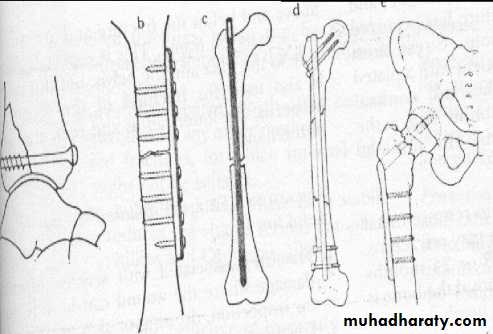
Internal fixation:Bone fragments can be fixed with:
Screws
transfixing pins
plate and screws
intramedullary nail ( with or without locking screws)
circumferential band
combination of these methods
Advantage of internal fixation:
Hold the fracture securely so movement can begin.
With early movement the fracture disease is abolished. The patient can leave the hospital early so the speed is concerned.
Indication for internal fixation:
Unreduced fractures
Unstable fractures
Fractures that unit poorly or slowly ( femoral neck)
Pathological fractures
Multiple fractures
Fractures in a who present nursing difficulties (paraplegic, multiple injuries, elderly)
Complications of internal fixation
Infection: Iatrogenic infection is now the most common cause of chronic osteomyelitis; the metal does not predispose to infection but the operation and quality of the patient’s tissues do.
Non-union: If the bones have been fixed rigidly with a gap between the ends, the fracture may fail to unite.
Implant failure: Metal is subject to fatigue and can fail unless some union of the fracture has occurred. Stress must therefore be avoided and a patient with a broken tibia internally fixed should walk with crutches and stay away from partial weight bearing for 6 weeks or longer, until callus or other radiological sign of fracture healing is seen on x-ray. Pain at the fracture site is a danger signal and must be investigated.
Too little Too much Too weak
Refracture: it is important not to remove metal implants too soon, or the bone may refracture. A year is the minimum and 18 or 24 months safer; for several weeks after removal the bone is weak, and care or protection is needed.
External fixation
It is a method of holding the fracture by transfixing screws or tensioned wires which pass through the bone above and below the fracture and attached to an external frameIndication of external fixation:
Fracture associated with sever soft tissue damage (compound fractures).
Fracture associated with nerve or vessels damage
Fracture pelvis
Infected fractures
Sever multiple injuries
Bone lengthening, shortening and carrying
Fractures around joints that are potentially suitable for internal fixation but the soft tissues are too swollen to allow safe surgery; here, a spanning external fixator provides stability until soft-tissue conditions improve.
Complications.
Pin tract infection.
Over distraction: if there is no contact between the fragments, union is unlikely.
3. Damage to soft –tissue structures (nerves or vessels)