Pediatrics
NEUROLOGY
1
L.1 Dr. Roua Al yaseen
Central nervous system (CNS) congenital malformations
Neural tube defects
Neural tube defects (NTDs) are commonest congenital anomalies of the
CNS and result from failure of the neural tube to close spontaneously
between the 3rd and 4th wk. of in utero development
Etiology
o Unknown,
o Hyperthermia
o Drugs (valproic acid)
o Malnutrition
o Low red cell folate levels
o Maternal obesity or diabetes
o Genetic determinants (mutations in Folate-responsive or folate-
dependent enzyme pathways)
o Exposure to radiation before conception.
Prenatal screening
Prenatal screening of maternal serum for AFP in the 16th-18th wk of
gestation is an effective method for identifying pregnancies at risk for fetuses
with NTDs in utero.
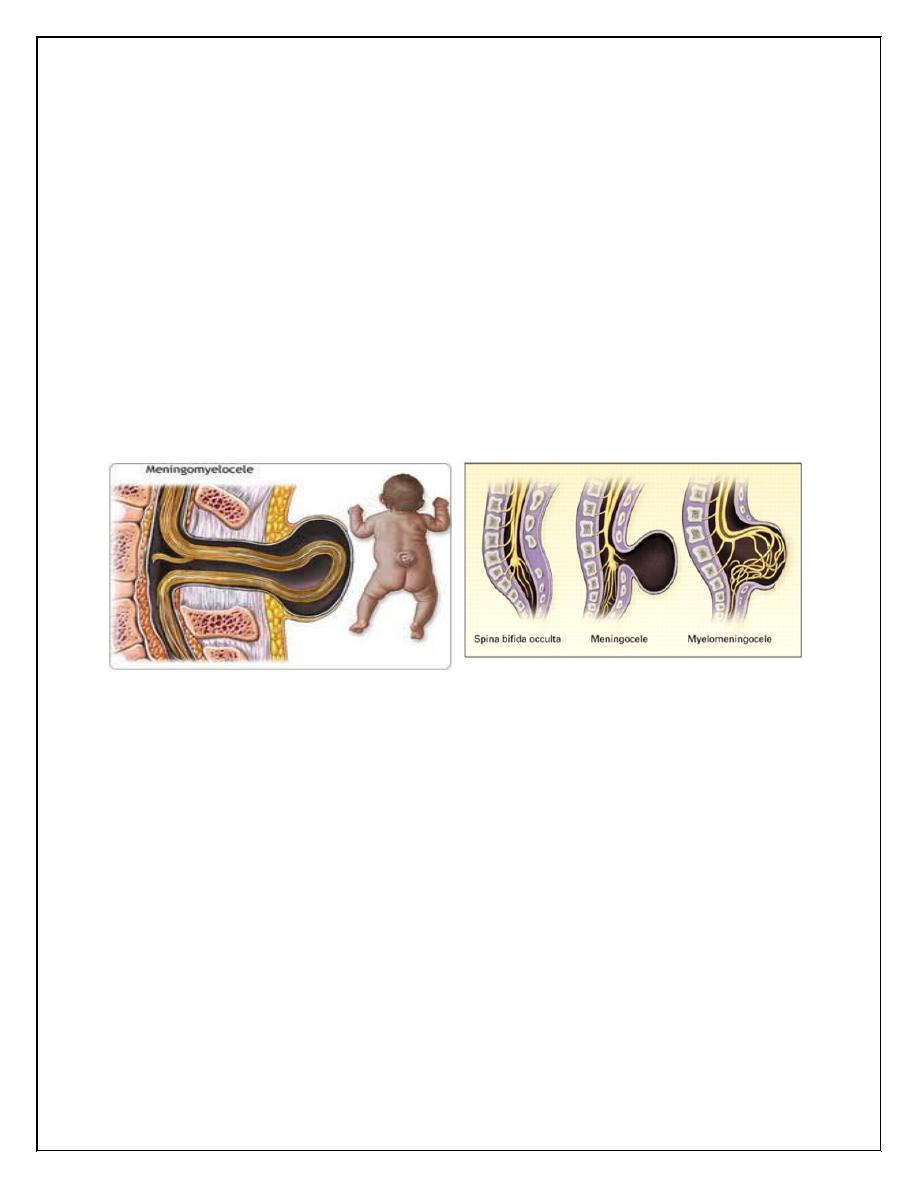
1. Spina bifida occulta
is a common anomaly consisting of a midline defect of the vertebral bodies
without protrusion of the spinal cord or meninges. Most patients are
asymptomatic and lack neurologic signs, This simple defect does not have an
associated spinal cord malformation but there are cutaneous manifestations
such as a hemangioma, discoloration of the skin, lump ,dermal sinus, or hairy
patch. All cases are best investigated with MRI.
Pediatrics
NEUROLOGY
2
2.Meningocele
A meningocele is formed when the meninges herniate through a defect in the
posterior vertebral arches or the anterior sacrum. Most meningoceles are well
covered with skin Careful neurologic examination is mandatory.
Orthopedic and urologic examination should also be considered. In
asymptomatic children with normal neurologic findings and full-thickness
skin covering the meningocele, surgery may be delayed or sometimes not
performed.
3. Myelomeningocele
Myelomeningocele represents the most severe form of dysraphism , so called
open form , involving the vertebral column and spinal cord.
CLINICAL MANIFESTATIONS
Myelomeningocele
produces
dysfunction
of
skeleton,
skin,
and
gastrointestinal and genitourinary tracts, peripheral nervous system and the
CNS.
A myelomeningocele located in lumbosacral region accounts for at least 75%
of the cases. A lesion in the low sacral region causes bowel and bladder
incontinence.
Examination
of the infant shows a flaccid paralysis of the lower
extremities, an absence of deep tendon reflexes, a lack of response to touch
and pain, and a high incidence of lower-extremity deformities (clubfeet,
ankle and /or knee contractures , and subluxation of the hips)
Patients with a myelomeningocele in the upper thoracic or the cervical region
usually have a very minimal neurologic deficit and, in most cases .
Pediatrics
NEUROLOGY
3
TREATMENT
Management and supervision of a child and family with a myelomeningocele
require team approach, including surgeons, other physicians, and therapists,
with a pediatrician
1-Surgery : repair of a myelomeningocele is often done within a day of birth
but can be delayed for several days (except when there is a CSF leak).
2- Shunting procedure for hydrocephalus if present.
3- Clubfeet may require casting.
4-Careful evaluation of the genitourinary system, & regularly catheterize a
neurogenic bladder to prevents urinary tract infections and reflux leading to
pyelonephritis , hydro nephrosis , and bladder damage.
PROGNOSIS
For a child who is born with a myelomeningocele and who is treated
aggressively, the mortality rate is 10-15%, and most deaths occur before age
4 yr. At least 70% of survivors have normal intelligence, but learning
problems and seizure disorders are more common than in the general
population. Renal dysfunction is one of the most important determinants of
mortality.
Prevention
All women of childbearing age take 0.4 mg of folic acid daily. If high-risk
women (previously affected child), supplementation should be started with
4 mg of folic acid daily, beginning 1 mo before pregnancy. Certain drugs,
including drugs that antagonize folic acid such as trimethoprim and the
anticonvulsants (carbamazepine, phenytoin & phenobarbital) increase the risk
of myelomeningocele if administered during pregnancy.
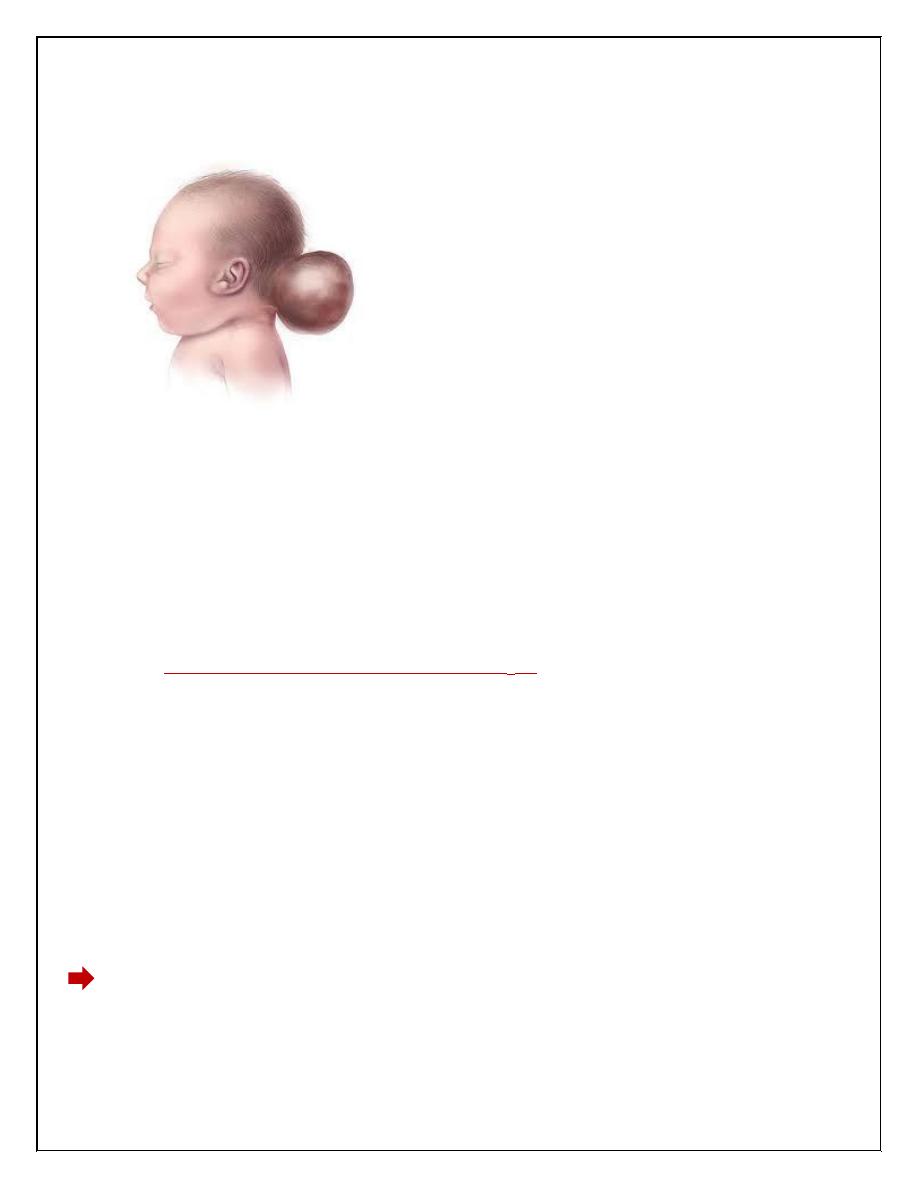
4.Encephalocele
Protrusion of tissue through a bony midline defect (commonly in the occipital
region ).a cranial encephalocele contains the sac plus cerebral cortex,
Pediatrics
NEUROLOGY
4
cerebellum, or portions of the brainstem. Infants with a cranial encephalocele
are at increased risk for developing hydrocephalus .
5.Hydrocephalus
Hydrocephalus is not a specific disease; it represents a diverse group of
conditions that result from impaired circulation and absorption of CSF .
Physiology:
The CSF is formed primarily in the ventricular system by the choroid plexus,
which is situated in the lateral, 3rd, and 4th ventricles.
The total volume of CSF approximates 50 mL in an infant and 150 mL in an
adult.
Intraventricular pressure is 180 mm H
2
O.
Hydrocephalus resulting from obstruction within the ventricular system is
called obstructive or noncommunicating hydrocephalus. The CSF then
circulates from the basal cisterns over the convexities of the cerebral
hemispheres & absorbed by the arachnoid villi.
If it is resulting from obliteration of the subarachnoid cisterns or malfunction
of the arachnoid villi is called nonobstructive or communicating
hydrocephalus.
Etiology
Obstructive hydrocephalus( noncommunicating) :
1-Aqueductal stenosis
- Infectious(meningitis)
-neurofibromatosis
Pediatrics
NEUROLOGY
5
2-Lesions or malformation of posterior fossa like tumor, Chiari
malformation, Dandy-Walker malformation.
3-Mass lesions ( Abscess, Hematoma, Tumors and neurocutaneous disorders.
Communicating hydrocephalus:
1-Meningitis (Pneumococcal and tuberculous meningitis) due to produce a
thick, exudate that obstructs the basal cisterns.
2-Subarachnoid hemorrhage because blood in the subarachnoid spaces cause
obliteration of the cisterns or arachnoid villi and obstruction of CSF flow.
3- Leukemic infiltrates.
4- Choroid plexus papilloma.
5- Achondroplasia.
Clinical manifestations
It is variable and depends on many factors, including the age at onset, the
nature of the lesion causing obstruction, and the duration and rate of increase
of the intracranial pressure (ICP).
In infants:
Accelerated rate of enlargement of the head is the most prominent sign.
The anterior fontanel is wide open and bulging, and the scalp veins are
dilated.
The forehead is broad, and the eyes deviate downward, producing the
setting-sun sign.
Long-tract signs including brisk tendon reflexes, spasticity, clonus
(particularly in the lower extremities), and Babinski sign are common.
In older child
The cranial sutures are partially closed so that the signs of hydrocephalus
may be subtler.
headache is a prominent symptom in older patients.
Irritability, lethargy, poor appetite, and vomiting are common .
A gradual change in personality and a deterioration in academic
productivity suggest a slowly progressive form of hydrocephalus.
Pediatrics
NEUROLOGY
6
By examination:
1-Serial measurements of the head circumference(OFC) indicate an increased
velocity of growth.
2-Percussion of the skull may produce a cracked pot sound or Macewen sign,
indicating separation of the sutures.
3-Papilledema, abducens nerve palsy, and pyramidal tract signs mainly in the
lower extremities, are apparent in most cases.
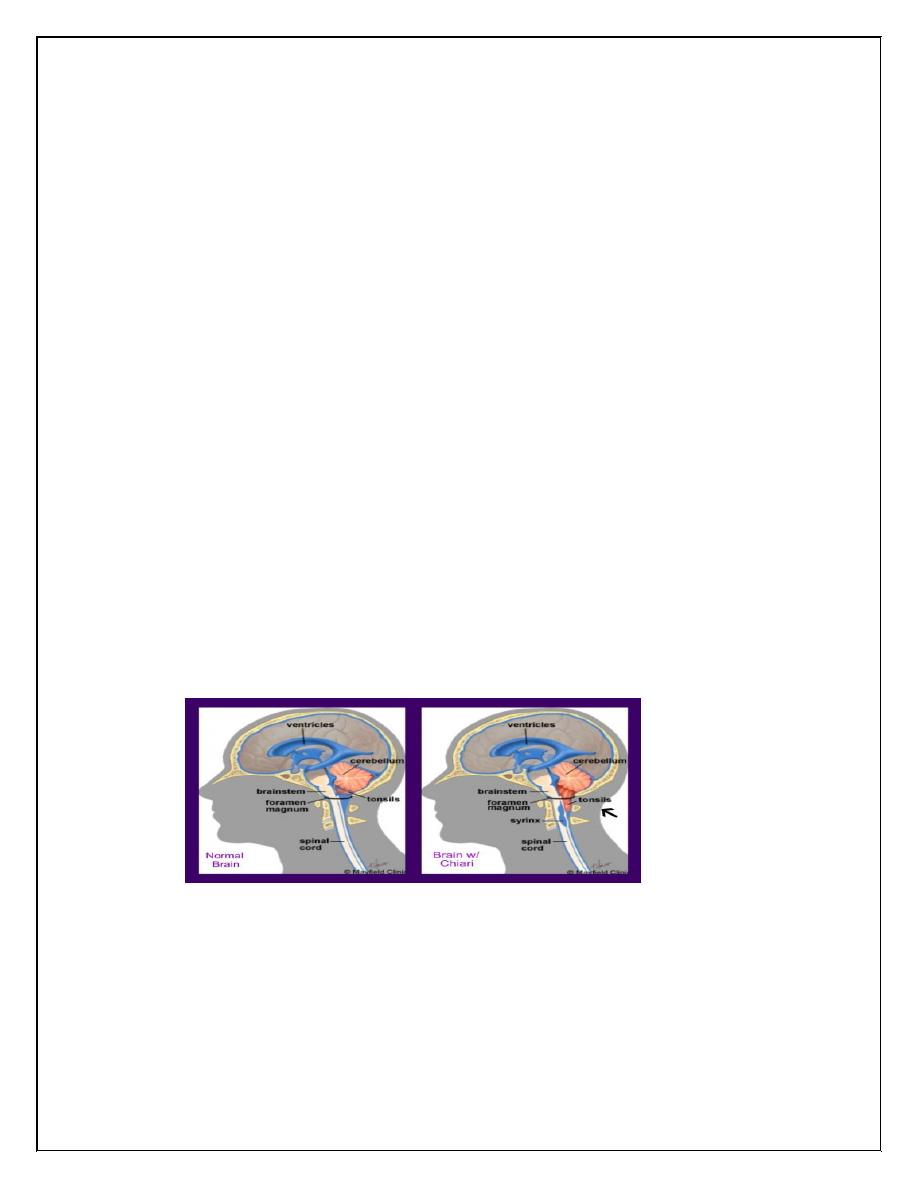
Chiari malformation: consists of two major subgroups.
Type I typically produces symptoms during adolescence or adult life and is
usually not associated with hydrocephalus. Patients complain of recurrent
headache, neck pain, urinary frequency, and progressive lower extremity
spasticity. The deformity consists of displacement of the cerebellar tonsils
into the cervical canal.
Type II Chiari malformation is characterized by progressive hydrocephalus
with a myelomeningocele. This lesion represents an elongation of the 4th
ventricle and kinking of the brainstem, with displacement of the inferior
vermis, pons, and medulla into the cervical canal. Symptoms during infancy
consisting of stridor, weak cry, and apnea.
Dandy-Walker malformation consists of a cystic expansion of the 4th
ventricle in the posterior fossa. 90% of patients have hydrocephalus.
Pediatrics
NEUROLOGY
7
6.Anencephaly
Large defect of the calvarium, meninges, and scalp associated with a
rudimentary brain.The cerebral hemispheres and cerebellum are usually
absent, and only a residue of the brainstem can be identified.
The pituitary gland is hypoplastic, folding of the ears, cleft palate, and
congenital heart defects in 10-20% of cases. Most anencephalic infants die
within several days of birth.
