Gestational trophoblastic diseases(GTD)
Dr. Bushra m majeedIt is a benign neoplasm of the chorionic villi
Incidence:1:2000 pregnancies in United States and Europe
1:200 in Asia10 times more in women over 45 years old.
The increasing use of ultrasound in early pregnancy has probably led to the earlier diagnosis of molar pregnancy1-Maternal age :
Young mothers (under age 20 years) have a slightly higher prevalence of GTD, although not nearly so great as those mothers over age 35 years.2-Women who have had a previous molar gestation
.
3- Women with blood type A may be more likely to develop choriocarcinoma (but not hydatidiform mole);
RISK FACTORS:
What Is A Hydatidiform Mole?
A hydatidiform mole is an abnormality of fertilization
It is the result of fertilisation of anucleated ovum ( has no chromosomes) with a sperm which will duplicate giving rise to 46 chromosomes of paternal origin only.
It is the result of fertilisation of an ovum by 2 sperms so the chromosomal number is 69 chromosomes
COMPLETE MOLE
PARTIAL MOLE
Comparative Pathologic Features of Complete and Partial Hydatidiform Mole
• Feature• Complete Mole
• Partial Mole
• Karyotype
• Usually diploid 46XX
• Usually triploidy 69XXX most common.
• Villi
• All villi hydropin; no normal adjacent villi
• Normal adjacent villi may be present
• vessels
• present they contain no fetal blood cells
• blood cells
• Fetal tissue
• None present
• Usually present
• Trophoblast
• Hyperplasia usually present to variable degrees
• Hyperplasia mild and focal
Three components make up the trophoblast:
cytotrophoblast,
syncytiotrophoblast
intermediate trophoblast
The cytotrophoblast is a stem cell with high mitotic activity but without hormonal synthesis.
The syncytiotrophoblast, which constitutes the villous trophoblast, has low mitotic activity. The syncytiotrophoblast is responsible for the synthesis of the (beta-hCG)
The intermediate trophoblast has features of the other two components and is responsible for endometrial invasion and implantation
There is trophoblastic proliferation, with mitotic activity affecting both syncytial and cytotrophoblastic layers. This causes excessive secretion of hCG,chorionic thyrotrophin and progesterone.
.
Pathology
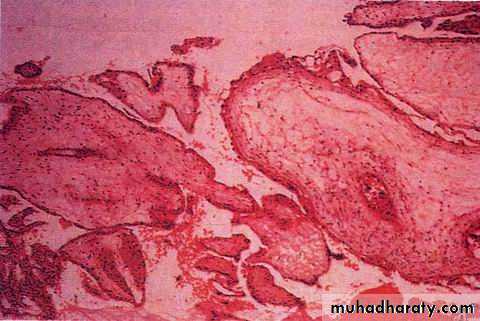
microscopic evaluation shows trophoblastic hyperplasia(hydropic) villi The uterus is distended by thin walled, translucent, grape-like vesicles of different sizes.
At histologic analysis,
Uniformly edematous (hydropic) villi with dissolution of central stroma (cavitation/cisternPathology
There is no vasculature in the chorionic villi leads to early death and absorption of the embryo.
At histologic analysis Occasionally, necrosis is seen
PathologyHigh hCG causes:
multiple theca lutein cysts in the ovaries in about 50% of cases.exaggeration of the normal early pregnancy symptoms and signs
Pathology
Uniformly edematous (hydropic) villi with dissolution of central stroma (cavitation/cistern)Villous vessels absent (usually)
Trophoblastic hyperplasia – circumferential, haphazard involves
Trophoblastic atypia
Pathology
Symptoms and Signs
Usually occur in first 20 24 weeks of gestation.
Bleeding.
pain.
toxemia (25% ).
hyperemesis (25%) .
absent fetus, LGA.
hyperthyroidism (7%).
passage of tissue with vesicles.
bilateral thecalutein cysts (30%).
GTD
MOST COMMON:
complete hydatidiform mole,
invasive mole,
choriocarcinoma.
Partial hydatidiform moles
placental site trophoblastic tumor
LESS COMMON:
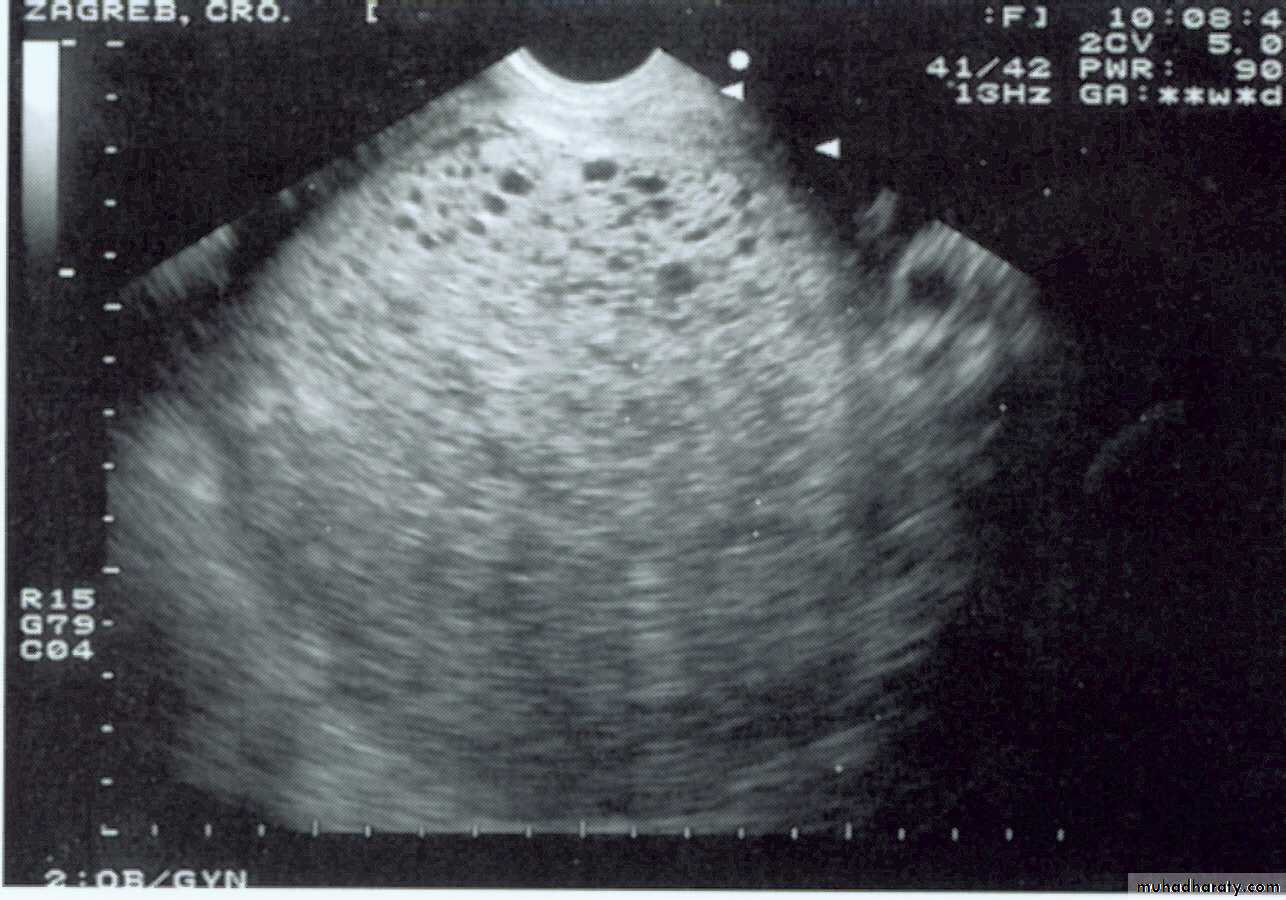
U/S evaluation.
Complete Hydatidiform Moleallows identification of numerous, discrete, anechoic (cystic) spaces within a central area of heterogeneous echotexture
Complete hydatidiform mole demonstrating enlarged villi of various size
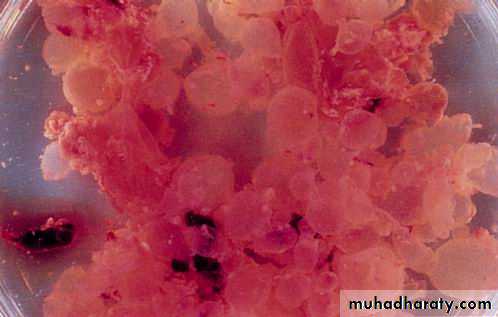
Hydatidiform mole: specimen from suction curettage
A large amount of villi in the uterus.The microscopic appearance of hydatidiform mole:
Hyperplasia of trophobasitc cellsHydropic swelling of all villi
Vessles are usually absent
Complete Hydatidiform Mole
Theca lutein cysts
multiloculated,
often bilateral
resolve after treatment of the intrauterine process
Occasionally seen in twin gestations, fetal hydrops, pharmacologic stimulation (especially with human maternal gonadotropin)
• U/S evaluation.
the ultrasound diagnosis of a complete mole is often reliable, the diagnosis of a partial molar pregnancy is more complex. The finding of multiple cystic spaces in the placenta is suggestive of a partial molar pregnancy. *When there is diagnostic doubt about the possibility of a combined molar pregnancy with a viable fetus then ultrasound examination should be repeated before intervention.
Partial Hydatidiform Mole
.Ultrasound has limited value in detecting partial molar pregnancies.
• U/S evaluation.Diagnosis of hydatidiform mole
Quantitative beta-HCGUltrasound is the criterion standard for identifying both complete and partial molar pregnancies. The classic image is of a “snowstorm” pattern
A sonographic findings of a molar pregnancy. The characteristic “snowstorm” pattern is evident.
Transvaginal sonogram demonstrating the “ snow storm” appearance.
Color Doppler image of a hydatidiform mole and surrounding vessels. The uterine artery is easily identified from its anatomical location.The clues for the sonographer in this diagnosis are the presence of a fetus (although usually with severe, but nonspecific, abnormalities) in combination with a formed placenta containing numerous cystic spaces
• U/S evaluation.
Partial Hydatidiform Mole
Partial hydartidiform mole
Microscopic image of partial molar pregnancy.
Here is a partial mole in a case of triploidy. Note the scattered grape-like masses with intervening normal-appearing placental tissue.Large bilateral theca lutein cysts resembling ovarian germ cell tumors. With resolution of the human chorionic gonadotropin(HCG) stimulation, they return to normal-appearing ovaries.
Treatment
Suction dilation and curettage :to remove benign hydatidiform molesWhen the diagnosis of hydatidiform mole is established, the molar pregnancy should be evacuated.
An oxytocic agent should be infused intravenously after the start of evacuation and continued for several hours to enhance uterine contractility
Evacuation of Molar Pregnancies
Suction curettage is the method of choice of evacuation for complete molar pregnancies.
Medical termination of complete molar pregnancies, including cervical preparation prior to suction evacuation should be avoided where possible. because of the potential to embolise and disseminate trophoblastic tissue through the venous system.
Evacuation of Molar Pregnancies
oxytocic infusions are only commenced once evacuation has been started. If the significant haemorrhage prior to evacuation and some degree of control is required then use of these agents will be necessary according to the clinical condition.Evacuation of Molar Pregnancies
Therapy:dilatation and suction curettage (at which time the diagnosis is confirmed).
15% of women with complete hydatidiform mole will develop recurrent disease in the form of invasive mole or choriocarcinoma.
all patients are followed up with successive serum beta-hCG measurements to allow early detection of persistent gestational trophoblastic neoplasia
SO
IF serial testing shows progressive decrease in the serum beta-hCG level
The clinical diagnosis of complete hydatidiform mole is reached.Avoid pregnancy
Because persistent trophoblastic disease may develop after any pregnancy it is recommended that all products of conception obtained after repeat evacuation, performed because of persisting symptoms, should undergo histological examination.
Evacuation of Molar Pregnancies
Removal of the uterus (hysterectomy) : used rarely to treat hydatidiform moles if future pregnancy is no longer desired.Treatment
Treatment
Remove the intrauterine contents promplyHysterectomy
in the older reproductive group who have no interest in further childbearing
Management of luteinizing cyst
Chemotherapy with a single-agent drug
Prophylactic (for prevention) chemotherapy at the time of or immediately following molar evacuation may be considered for the high-risk patients( to prevent spread of disease )Treatment
Preventive chemotherapyAge more than 40
Level of serum HCG increased significantaly(more than
100KIU/L)
Titer of HCG has not returned to normal after 12 weeks
postevacuation
Re-elevated HCG level
Uterus larger than expected
Diameter of luteinizing cyst more than 6cm
Trophoblast hyperproliferation still after second curettage
Has no condition to follow-up
Follow-up
Pelvic examination, ultrasound examination
Assessment of HCG
Serum quantitative HCG level every 1 week until normal
Every 1 week(three month)
Every 2 weeks(three month)
Every 1 month( half year)
Every half year(one year)
Contraception for 1-2 years
Choriocarcinoma
Hyper-malignant tumor50% of patients follow molar pregnancy
25% of patients follow abortion
25% of patients follow term pregnancy
few of patient follow ectopic pregnancy
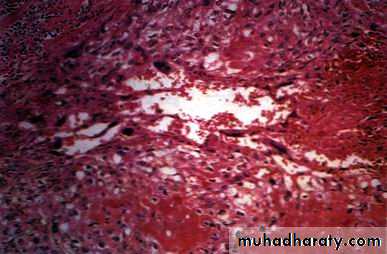
Gross specimen of choriocarcinoma
Microscopic image of choriocarcinoma
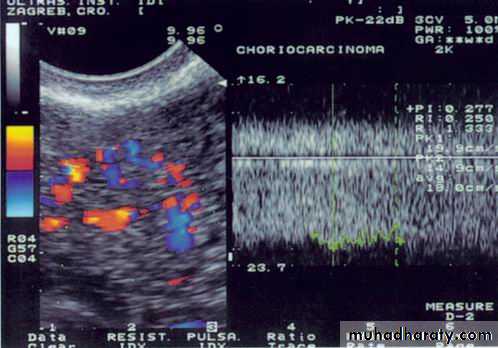
absence of chorionic villiDoppler image of choriocarcinoma
Doppler image of choriocarcinoma
Clinical presentationVaginal bleeding
Abdominal pain
Pelvic mass
Presentation of metastasis
Lung, vagina, brain, liver et al
Diagnosis
Clinical presentation
If the symptom and sign follow abortion, term birth and ectopic pregnancy companing HCG level increased, the diagnosis can be considered
Assessment of HCG titer
Ultrasound and doppler examination
Histology
WHO Prognostic Scoring System
• Score• Prognostic factor
• 0• 1
• 2
• 4
• Age(years)
• ≤39
• >39
• —
• —
• Pregnancy history
• Hydatidiform mole
• Abortion,
• ectopic
• Term pregnancy
• —
• Interval (months) of treatment
• <4
• 4-6
• 7-12
• >12
• Initial hCG(mIU/ml)
• <103
• 103-104
• 104-105
• >105
• Largest tumor(cm)
• <3
• 3-5
• >5
• —
• Sites of metastasis
• Lung
• Spleen,
• kidney
• GI tract, liver
• Brain
• No. of metastasis
• —
• 1-4
• 4-8
• 8
• Previous (treatment)
• —
• —
• Single drug
• 2 or more
0-4 low risk, 5-7 intermediate risk, >8 high risk for death
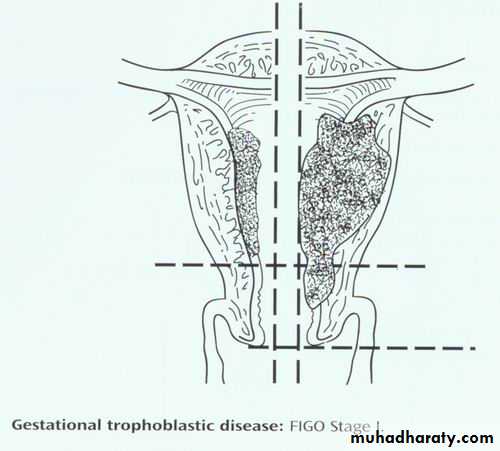
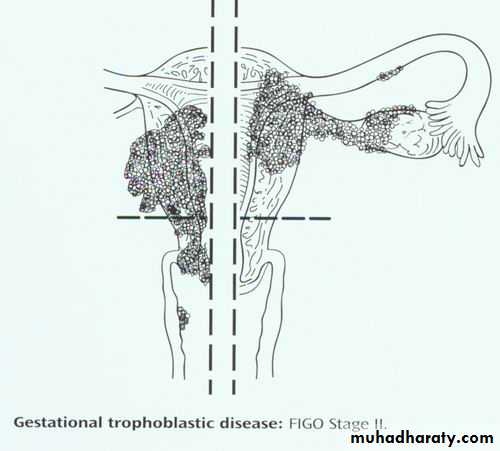
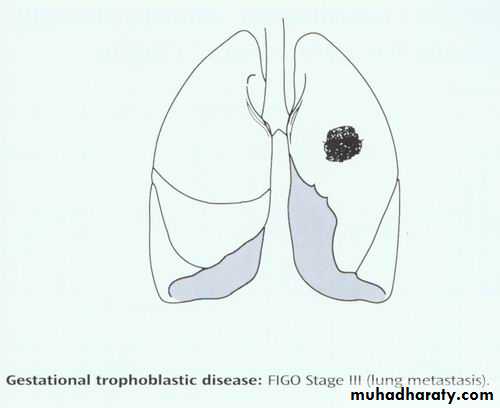
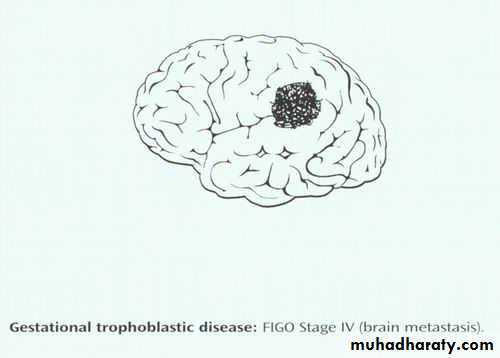
FIGO Staging System for Gestational Trophoblastic Tumors
• Stage
• Description
• Ⅰ
• Limited to uterine corpus
• Ⅱ
• Extends to the adnexae, outside the uterus, but limited to the genital structures
• Ⅲ
• Extends to the lungs with or without genital tract
• Ⅳ
• All other metastatic sites
IIb
IIa
IIIa<3cm or locate in half lung
IIIb disease beyond IIIaDiagnosis and evaluation
Gestational trophoblastic tumor is diagnosed by rising hCG following evacuation of a molar pregnancy or any pregnancy eventOnce the diagnosis established the further examinations should be done to determine the extent of disease ( X-ray, CT, MRI)
Treatment
Nonmetastatic GTDLow-Risk Metastatic GTD
High-Risk Metastatic GTD
Treatment of Nonmetastatic GTD
Hysterectomy is advisable as initial treatment in patients with nonmetastatic GTD who no longer wish to preserve fertilityThis choice can reduce the number of course and shorter duration of chemotherapy.
Adjusted single-agent chemotherapy at the time of operation is indicated to eradicate any occult metastases and reduce tumor dissemination.
Single-agent chemotherapy is the treatment of choice for patients wishing to preserve their fertility.
Methotrexate(MTX) and Actinomycin-D are generally chemotherapy agents
Treatment is continued until three consecutive normal hCG levels have been obtained and two courses have been given after the first normal hCG level.
Treatment of Nonmetastatic GTD
To prevent relapse or metastasis
Single-agent chemotherapy with MTX or actinomycin-D is the treatment for patients in this category
If resistance to sequential single-agent chemotherapy develops, combination chemotherapy would be taken
Approximately 10-15% of patients treated with single-agent chemotherapy will require combination chemotherapy with or without surgery to achieve remission
Treatment of Low-Risk Metastatic GTD
Multiagent chemotherapy with or without adjuvant radiotherapy or surgery should be the initial treatment for patients with high-risk metastatic GTD
EMA-CO regimen formula is good choice for high-risk metastatic GTD
Treatment of High-Risk Metastatic GTD
EMA-CO Chemotherapy for poor Prognostic Disease• Etoposide(VP-16)
• 100mg/M2
• IV daily×2 days (over 30-45 minutes)
• Methotrexate
• 100mg/M2
• IV losding dose, then 200mg/M2 over 12 hours day 1
• Actinomycin D
• 0.5mg
• IV daily×2 days
• Folinic acid
• 15mg IM or p.o. q 12 hours×4 starting 24 hours after starting methotrexate
• Cyclophosphamide
• 600mg/M2
• IV on day8
• Oncovin (vincristine)
• 1mg/M2
• IV on day8
• (Repeat every 15 days as toxicity permits)
Prognosis
Cure rates should approach 100% in nonmetastatic and low-risk metastatic GTDIntensive multimodality therapy has resulted in cure rates of 80-90% in patients with high-risk metastatic GTD
Follow-up After Successful Treatment
Quantitative serum hCG levels should be obtained monthly for 6 months, every two months for remainder of the first year, every 3 months during the second yearContraception should be maintained for at least 1 year after the completion of chemotherapy. Condom is the choice.
Treatment
ChemotherapyOperation
Follow-up
Every 1 month first year
Every 3 months 2 years
Every 1 year 2 years
Then every 2 yeas ……
THANK YOU