
Common Medical
Emergencies
BY:
Adel Mohammed
Maath.Hameed Al-ani
Omer Rakan Yehya

Pulmonary
Embolism (PE)
BY:
Adel Mohammed
Pulmonary Embolism
(PE)
• The majority (80%) of pulmonary emboli arise
from the propagation of lower limb DVT. Rare
causes include septic emboli (from endocarditis
affecting the tricuspid or pulmonary valves),
tumour (especially choriocarcinoma), fat, air,
amniotic fluid and placenta.
• it occurs in approximately 1% of all patients
admitted to hospital and accounts for around 5%
of in-hospital deaths.
• Clinical presentation varies, depending on
number, size and distribution of emboli and on
underlying cardiorespiratory reserve . A
recognised risk factor is present in 80
–90% .
The presence of one or more risk factors
increases the risk further still.
PE may be difficult to diagnose. It is helpful
to consider:
• Is the clinical presentation consistent with
PE?
• Does the patient have risk factors for PE?
• Are there any alternative diagnoses that
can explain the patient’s presentation?
Clinical presentation of acute
massive PE
• A big thrombus obstructing major
pulmonary artery causing low cardiac
output and acute right side heart failure
• The patient presents with sudden collapse
(fainting), crushing central chest pain, and
severe dyspnoea.
• The examination may reveals major
circulatory collapse: tachycardia,
hypotension, ↑JVP, severe cyanosis.
Risk factors
Surgery
• Major abdominal/pelvic surgery
• Hip/knee surgery
• Post-operative intensive care
Lower limb problems
• Fracture
• Varicose veins
• Stroke/spinal cord injury
Obstetrics
• Pregnancy/puerperium
Cardiorespiratory disease
• COPD
• Congestive cardiac failure
• Other disabling disease
Malignant disease
• Abdominal/pelvic
• Advanced/metastatic
• Concurrent chemotherapy
Miscellaneous
• Increasing age
• Previous proven VTE
• Immobility
• Thrombotic disorders
• Trauma
Differential Diagnosis
• Myocardial infarction
• pericardial tamponade
• aortic dissection
Investigations
• chest X-ray
is most useful in excluding key
differential diagnoses, e.g. pneumothorax.
Normal appearances in an acutely
breathless and hypoxaemic patient should
raise the suspicion of PE.
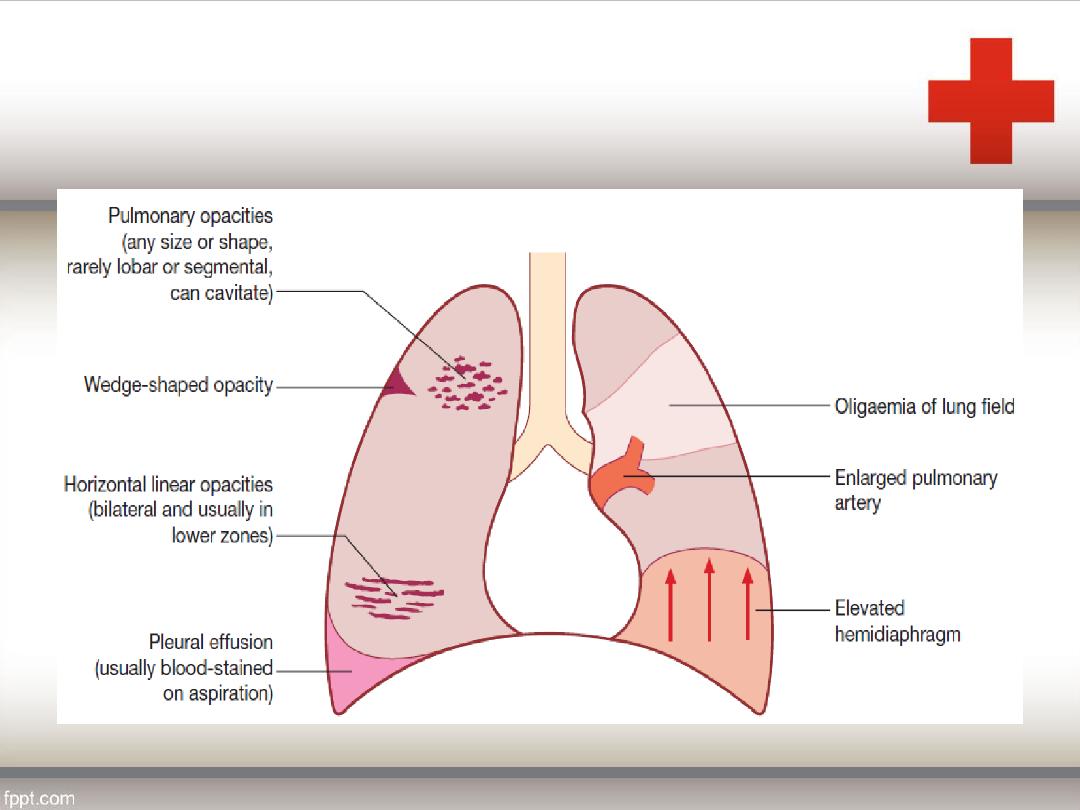
CXR features
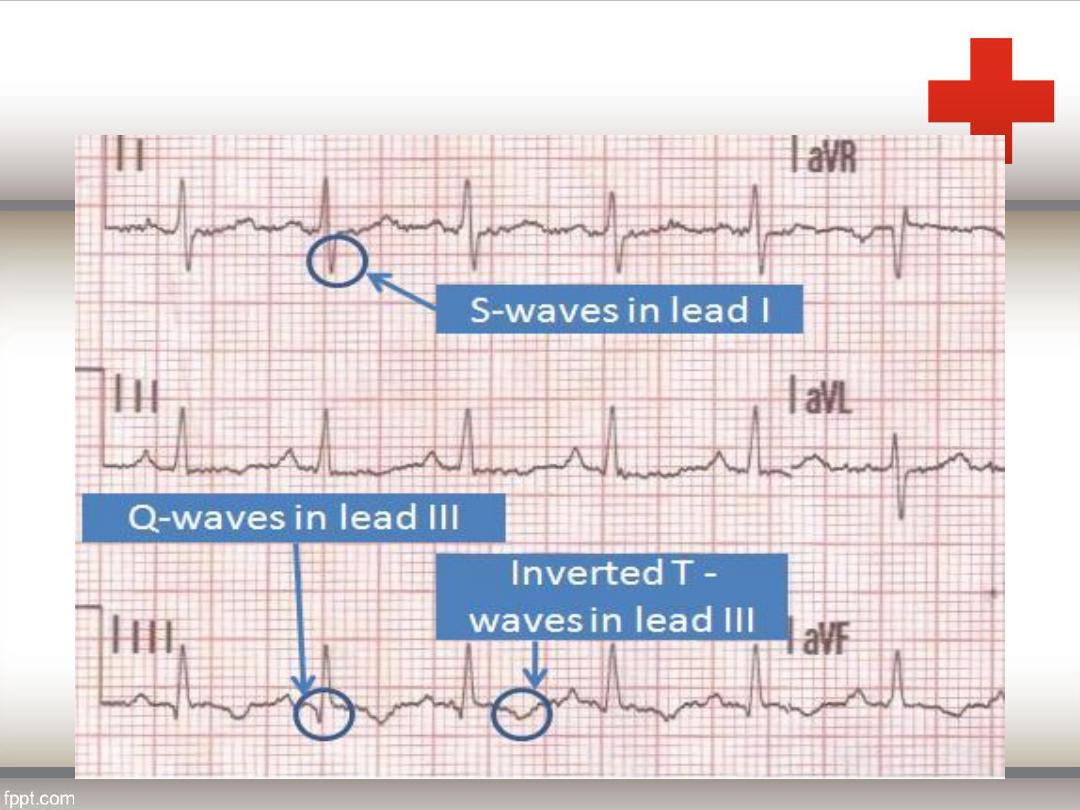
• ECG
is often normal but is useful in excluding
other important differential diagnoses, such
as acute myocardial infarction and
pericarditis. The most common findings in PE
include sinus tachycardia and anterior T-
wave inversion but these are non-specific;
larger emboli may cause right heart strain
revealed by an S1Q3T3 pattern, ST-segment
and T-wave changes, or the appearance of
right bundle branch block.
• Arterial blood gases
typically show a
reduced
PaO2
and a normal or low
PaCO2
. A metabolic acidosis may be seen
in acute massive PE with cardiovascular
collapse.
• D-dimer
an elevated D-dimer is of limited
value, as it may be raised in a variety of
conditions including PE, myocardial
infarction, pneumonia and sepsis.The D-
dimer result should be disregarded in high-
risk patients, as further investigation is
mandatory even if it is normal.
• Other circulating markers that reflect right
ventricular micro-infarction, such as
troponin I
and
brain natriuretic peptide.
CT pulmonary angiography
(CTPA) is the
first-line diagnostic test. It has the
advantages of visualising the distribution
and extent of the emboli, or highlighting an
alternative diagnosis, such as
consolidation, pneumothorax or aortic
dissection.
• Ventilation–perfusion scanning
is seldom used
nowadays, although a limited role remains in those
without significant cardiopulmonary disease.
• Colour Doppler ultrasound
of the leg veins
remains the investigation of choice in patients with
suspected DVT.
• Bedside echocardiography
is extremely helpful in
the differential diagnosis and assessment of acute
circulatory collapse. Acute dilatation of the right
heart is usually present in massive PE, and
thrombus (embolism in transit) may be visible.
• Conventional pulmonary angiography
has
been largely superseded by CTPA but is
still useful in selected settings or to deliver
catheter-based therapies.
Management
General Measures
• Sufficient oxygen should be given to hypoxaemic
patients to maintain arterial oxygen saturation above
90%.
• Circulatory shock should be treated with intravenous
fluids or plasma expander.
• Opiates may be necessary to relieve pain and
distress but should be used with caution in the
hypotensive patient.
• Diuretics and vasodilators should also be avoided, as
they will reduce cardiac output.
Anticoagulation
• Anticoagulation should be commenced
immediately in patients with a high or
intermediate probability of PE, but may be
safely withheld in those with low clinical
probability, pending investigation. Heparin
reduces further propagation of clot and the
risk of further emboli, and lowers mortality.
• It is most easily administered as
subcutaneous low molecular weight
heparin (LMWH). The dose is based on
the patient’s weight (enoxaparin 1 mg/kg
twice daily SC) and there is usually no
requirement to monitor tests of
coagulation. Treatment with LMWH should
continue for at least 5 days during which
an oral anticoagulant is commenced.
• Warfarin – a vitamin K antagonist – remains
the most commonly used oral anticoagulant.
Therapy is initiated with a high loading
dose, followed by a maintenance dose
based on the international normalised ratio
(INR). LMWH should not be discontinued
until the INR is 2 or more for at least 24
hours.
Thrombolytic therapy
• Thrombolysis is indicated in any patient presenting with
acute massive PE accompanied by cardiogenic shock. In
the absence of shock, the benefits are less clear but
thrombolysis may be considered in those presenting with
right ventricular dilatation and hypokinesis or severe
hypoxaemia.
• Patients must be screened carefully for haemorrhagic
risk.
• Major contraindication to thrombolytic therapy include
intracranial disease, uncontrolled hypertention and
recent surgery or trauma (less then 3 weeks).
surgical therapy
• Surgical pulmonary embolectomy may be
considered in selected patients but carries
a high mortality.
Caval filters
• A patient in whom anticoagulation is
contraindicated, who has suffered massive
haemorrhage on anticoagulation, or
recurrent VTE despite anticoagulation,
should be considered for an inferior vena
caval filter

Asthma
BY:
Maath.Hameed Al-ani
• Definition
• Chronic inflammation of lung airway result
in episodic attack of airway obstruction
(bronchospasm) due to the air way hyper
responsiveness due to the various
immunological & non-immunological
exposure triggers(exercise, air pollution,
Occupational allergen , drugs : Aspirine
beta blocker)
Asthma
Asthma
• Pathology
Inhaled allergen rapidly interacts with
mucosal mast cells ,This will results in
histamine and leukotrienes release leading
to bronchoconstriction.
Airway edema, increased volume and size
of sub mucosal glands.
desquamation of airway epithelial cells
Asthma
• Presentation
SOB (Breathlessness)
Cough (Dry , intermittent cough)
Chest tightness
+ve family history of atopy (Atopic
dermatitis ,renitis )
These symptoms exacerbated by exercise
and usually at night due to exposure to
antigens at bed
Asthma
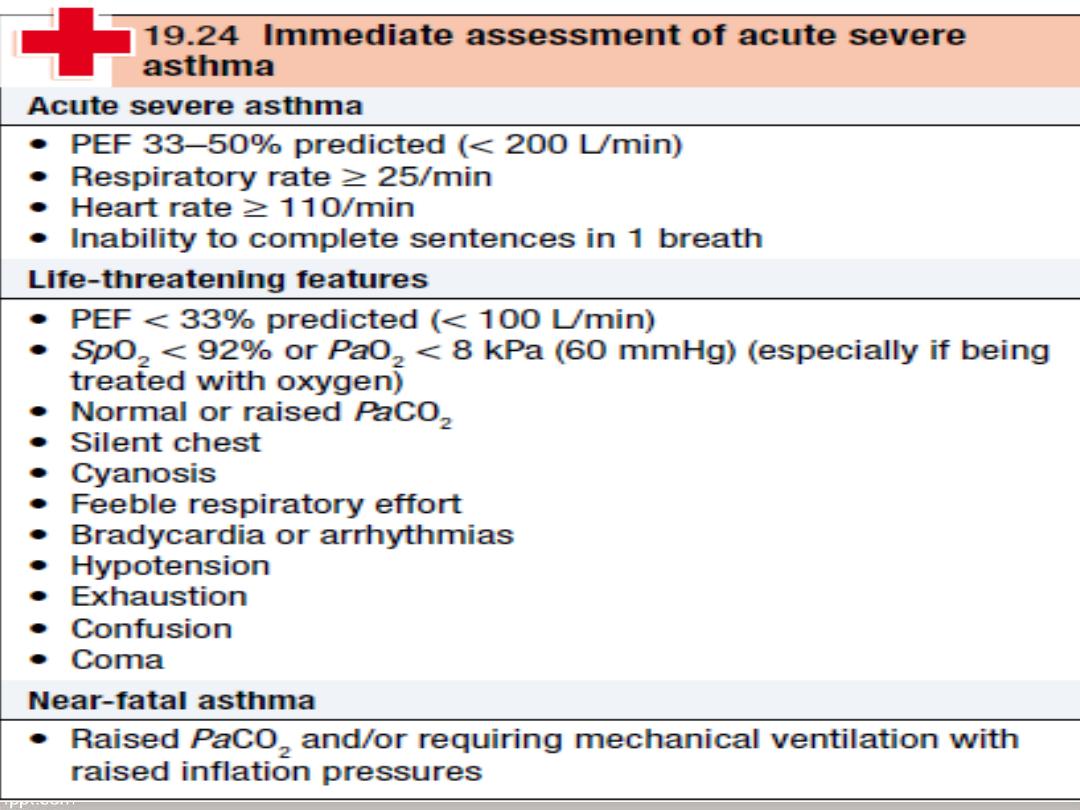
Acute sever asthma
Patient usually extremely distressed, using
accessory muscles of respiration, the
chest is inflated and the patient is
tachypnoea.
Pulsus paradoxus (loss of pulse pressure
on inspiration due to reduce cardiac return
due to sever hyperinflation) and sweating.
Central cyanosis in sever cases with silent
chest and bradycardia
Asthma
• Physical finding
Wheeze (Expiratory)
Rhonchi ,crepitation.
Diminished breath sound
In sever cases inspiratory and expiratory
wheeze and silent chest
Asthma
•
Immediate treatment
Oxygen should be given at the highest
concentration.
To maintain oxygen saturation above 92%.
High dose of inhaled ß2-adrenoceptor agonist
nebulised using oxygen (salbutamol 2.5-5mgor
terbutaline5-10mg) repeated within 30 minutes if
necessary. Inhaled ß2-adrenoceptor agonist can
be given out side hospital by large volume
spacers.
Asthma
Systemic steroids; 30-60mg prednisolone
orally or intravenous 200mg
hydrocortisone.
Intravenous fluid there are no controlled
trials to support the use of IV fluid but
many patient are dehydrated due to high
insensible water loss and properly benefit
from these . potassium supplement maybe
necessary because repeated dose of
salbutamol can lower serum potassium
Asthma
•
If the features of severity of asthma persistent:
Ipratropium bromide 0.5mg should be added
to nebulised 2-adrenoceptor agonist.
Continue nebulised 2-adrenoceptor agonist
every 15-30 minutes as necessary.
Magnesium sulphate (25mg/kg i.v, maximum
2gm)
Mechanical ventilation

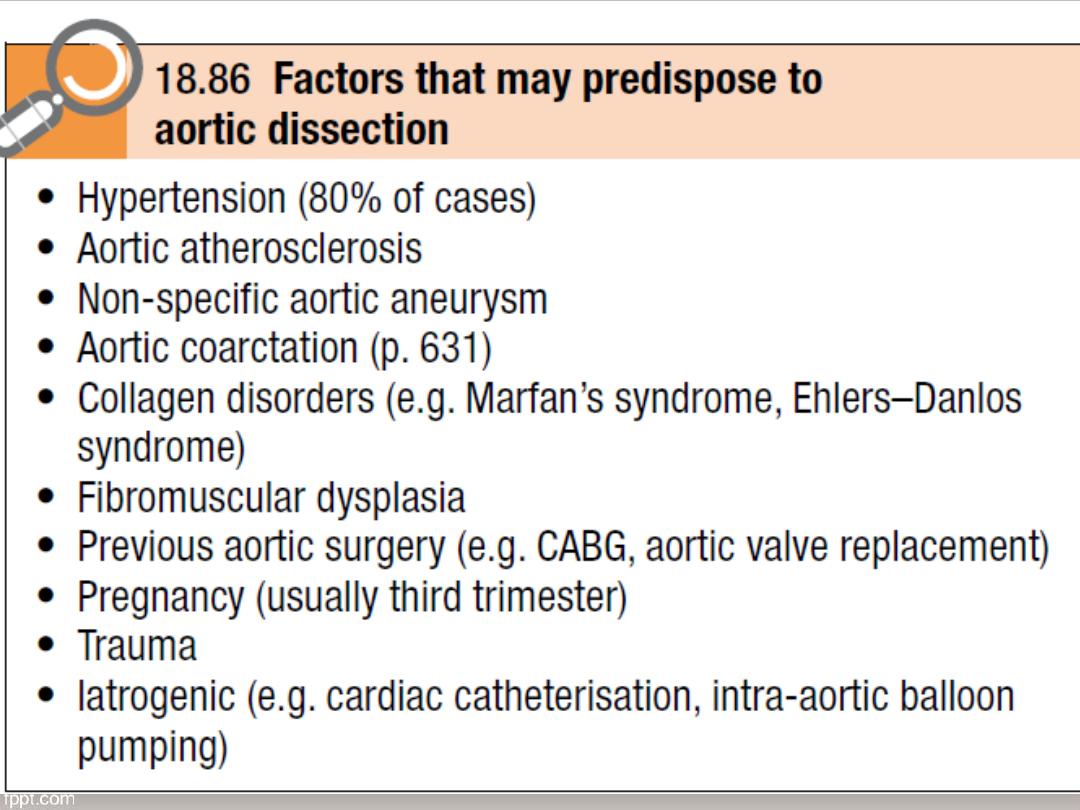
Aortic dissection
BY:
Omar Yehya
Aortic dissection
• Definition
A breach in the integrity of the aortic wall
allows atrial blood to inter the media which
is then split into two layers creating a false
lumen alongside he exiting of the true
lumen
Aortic valve maybe damaged and the
branch of the aorta maybe compromised
Aortic dissection
Typically the false lumen eventually re-
enters the true lumen creating a double
barreled aorta but it maybe also rapture
into the left pleura space or pericardium
with fetal consequences .
The primary event often a spontaneous or
iatrogenic tear in the intima of the aorta ,
multiple tears or entry points are common
Aortic dissection
Other dissections appear to be trigged by
primary hemorrhage in the media of the
aorta that then raptures through the intima
into the true lumen this form of
spontaneous bleeding from the vasa
vasorum is sometimes confined to the
aortic wall when it may present as a
painful intermural hematoma .
Aortic dissection
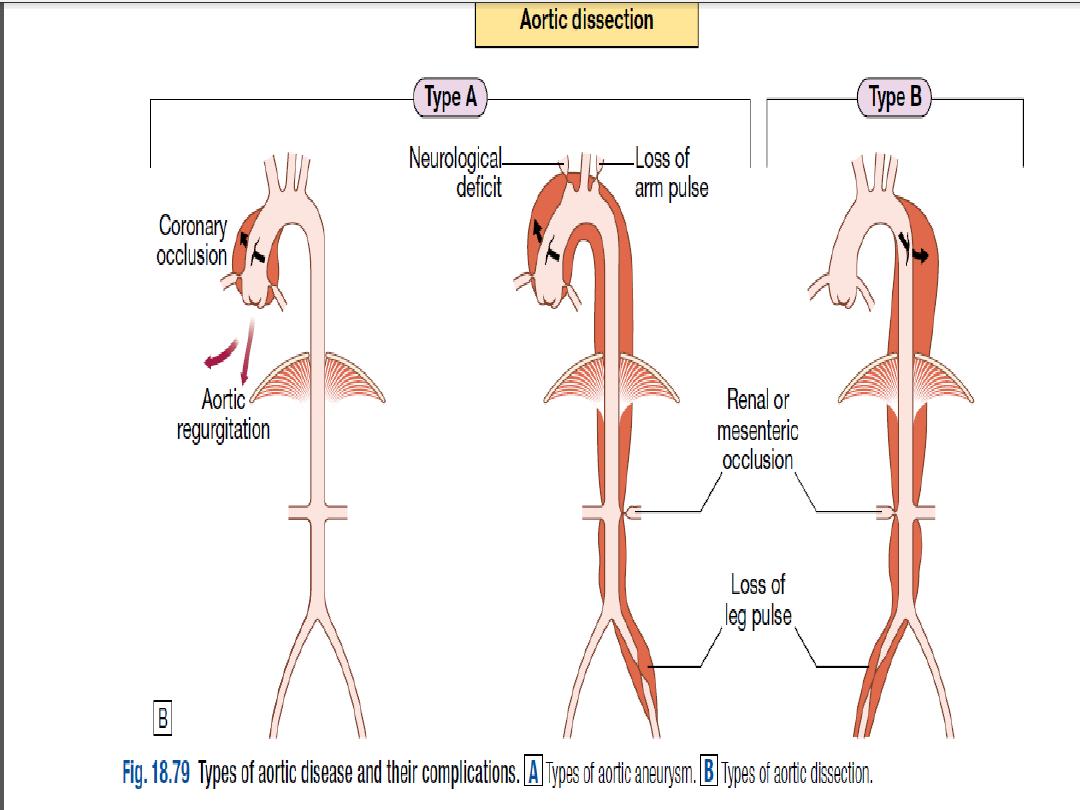
• Clinical feature
• Involvement of the ascending aorta
typically gives rise to anterior chest pain,
and involvement of the descending aorta
to intrascapular pain.
• The pain is typically described as ‘tearing’
and very abrupt in onset; collapse is
common. Unless there is major
haemorrhage .
Aortic dissection
• the patient is invariably hypertensive.
There may be asymmetryof the brachial,
carotid or femoral pulses and signs of
aortic regurgitation.
• Occlusion of aortic branches maycause MI
(coronary), stroke (carotid) paraplegia
(spinal),mesenteric infarction with an acute
abdomen (coeliacand superior
mesenteric), renal failure (renal) and
acutelimb (usually leg) ischaemia .
Aortic dissection
•
Investigations
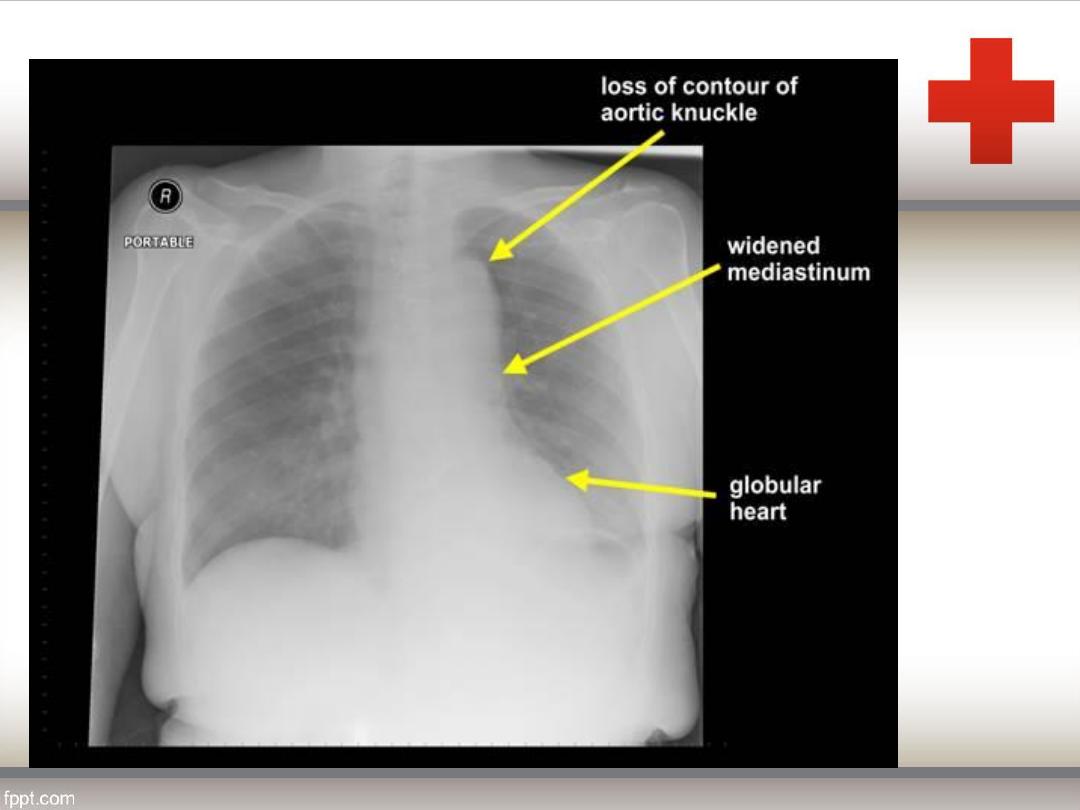
• The chest X-ray characteristically shows
broadening of the upper mediastinum and
distortion of the aortic ‘knuckle’, but these
findings are variable and are absent in
10% of cases. A left-sided pleural effusion
is common.
• The ECG may show left ventricular
hypertrophy in patients with hypertension,
or rarely changes of acute MI(usually
inferior).
Aortic dissection
• Doppler echocardiography may show
aortic regurgitation, a dilated aortic root
and, occasionally, the flap of the
dissection.
• Transoesophageal echocardiography is
particularly helpful because transthoracic
echocardiography can only image the first
3
–4 cm of the ascending aorta .
• CT and MRI angiography are both highly
specific and sensitive.
Aortic dissection
• Treatment
Pain control (morphine + plasil )
• Anti hypertensive drugs (β-blockers , Rate-limiting calcium
channel blockers, such as verapamil or diltiazem, are used
if β-blockers are contraindicated)
• Sodium nitroprusside may be considered if these fail to
control BP adequately.
• The aim of medical management is to maintain a mean
arterial pressure(MAP) of 60
–75 mmHg to reduce the
force of the ejection of blood from the LV.
Aortic dissection
• The aim of medical management is to
maintain a mean arterial pressure(MAP) of
60
–75 mmHg to reduce the force of the
ejection of blood from the LV.
Aortic dissection
• Type A dissections require emergency
surgery to replace the ascending aorta.
Type B aneurysms are treated medically
unless there is actual or impending
external rupture, or vital organ (gut,
kidneys) or limb ischaemia, as the
morbidity and mortality associated with
surgery is very high.
