Cardiac Chest pain
: اعداد وتقديم الطلبة
زينة بشار ذنون
مروة عبد الكريم
عمر عبد المحسن
Supervised by
: Dr. jasim Mohamad Taib

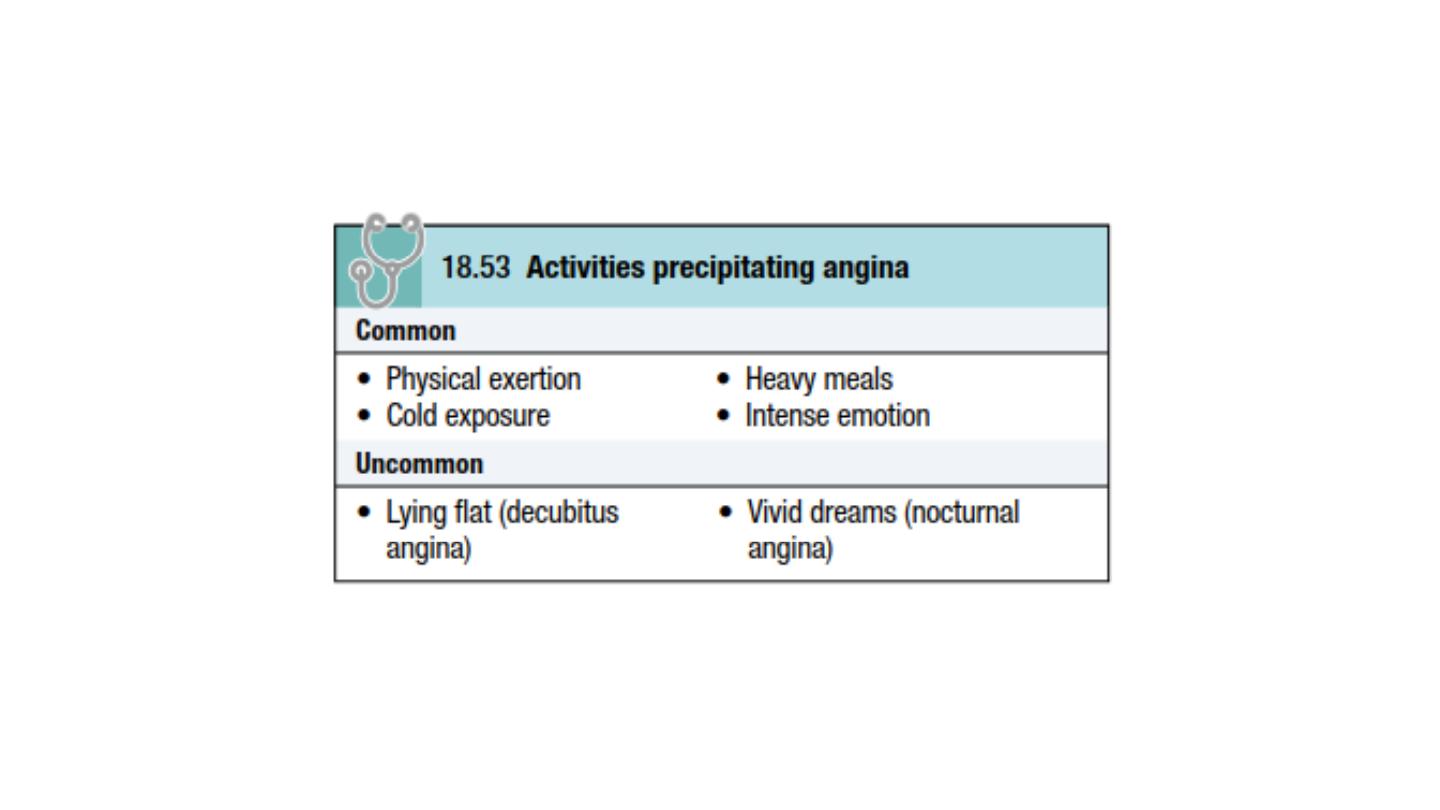
stable angina
Is transient myocardial ischaemia occur whenever there is an
imbalance between myocardial oxygen supply and demand .Coronary
atheroma is by far the most common cause of angina.
Clinical features
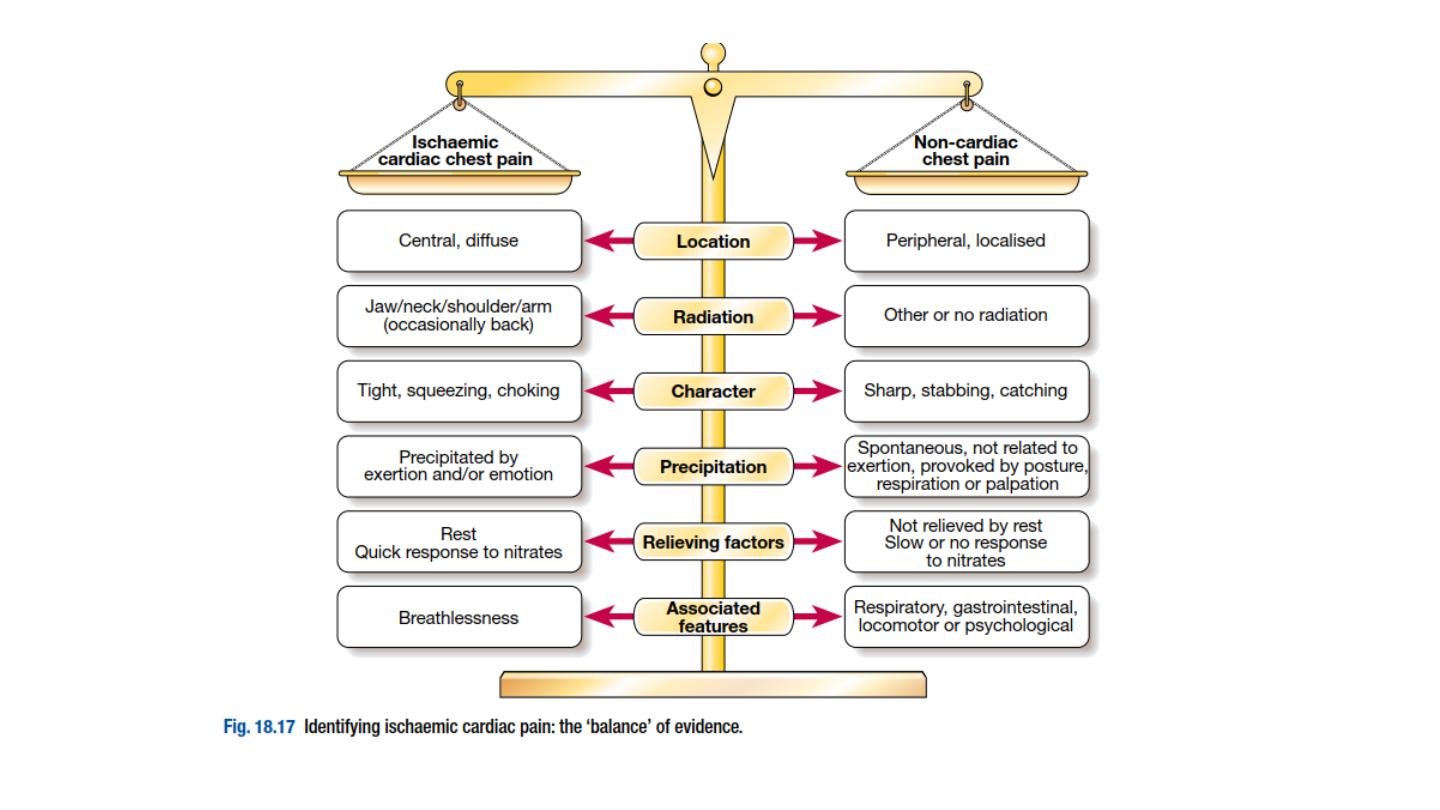
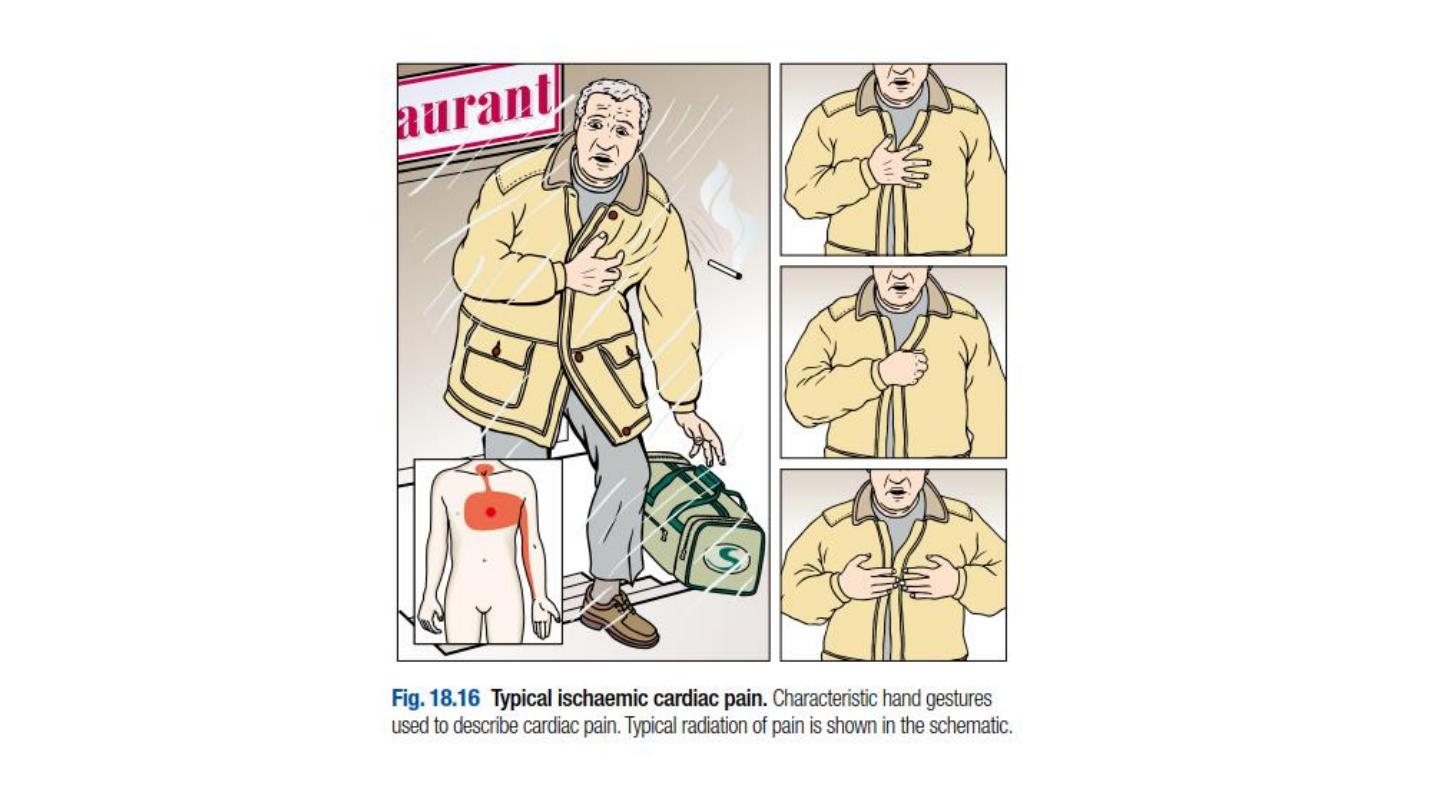
The history is by far the most important factor in making the diagnosis
.Stable angina is characterised by central chest pain, discomfort or
breathlessness that is precipitated by exertion or other forms of stress
important risk factors (e.g. hypertension, diabetes mellitus), left
ventricular dysfunction (cardiomegaly, gallop rhythm), other
manifestations of arterial disease (carotid bruits, peripheral vascular
disease) and unrelated conditions that may exacerbate angina
(anaemia, thyrotoxicosis).

Investigations
Resting ECG
The ECG may show evidence of previous MI but is often normal. Occasionally, there
is T-wave flattening or inversion in some leads, providing non-specific evidence of
myocardial ischaemia or damage. The most convincing ECG evidence of myocardial
ischaemia is the demonstration of reversible ST segment depression or elevation,
with or without T-wave inversion, at the time the patient is experiencing symptoms
(whether spontaneous or induced by exercise testing).
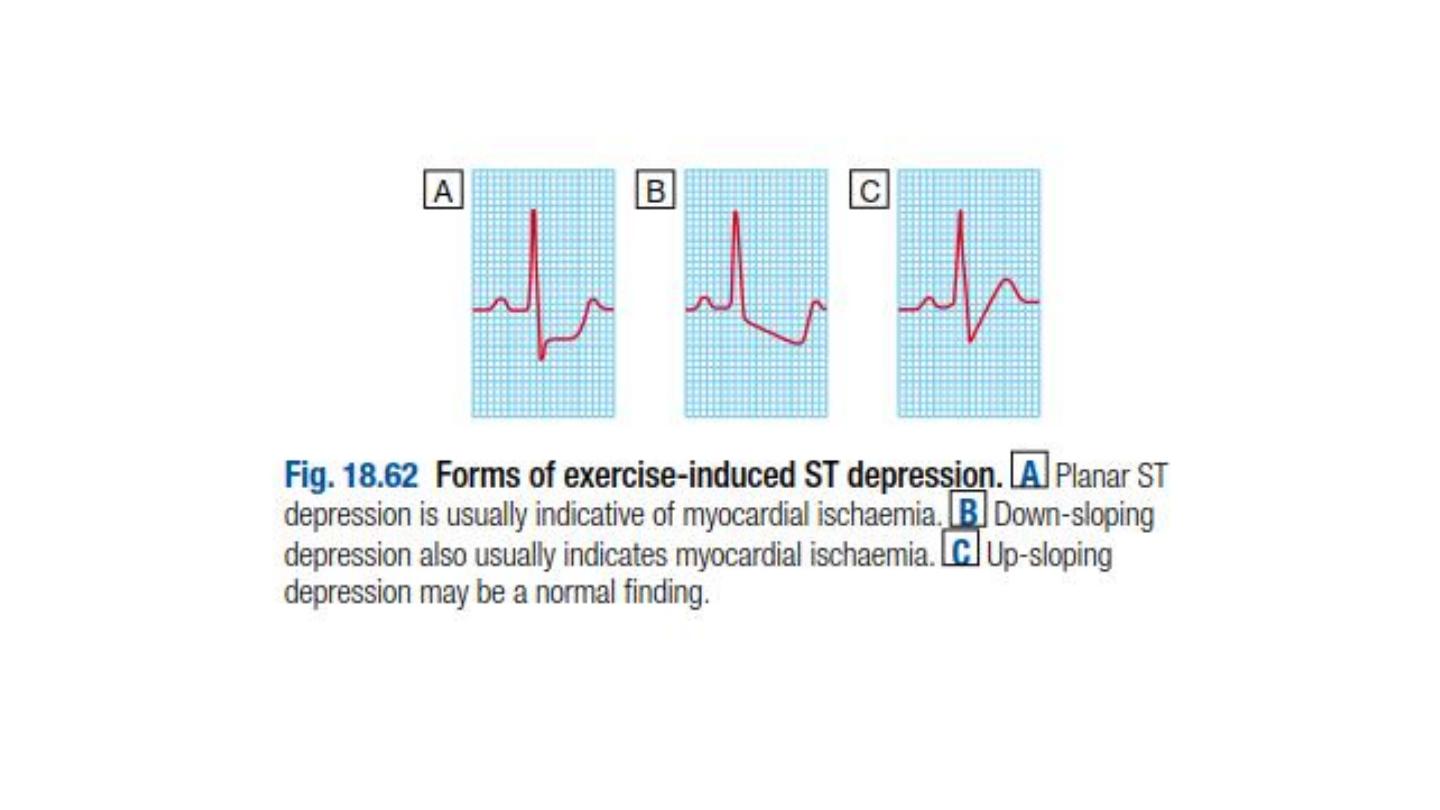
Exercise ECG
An exercise tolerance test (ETT) is usually performed using a standard treadmill or
bicycle ergometer protocol while monitoring the patient’s ECG, BP and general
condition. Planar or down-sloping ST segment depression of ≥ 1 mm is indicative of
ischaemia . Up-sloping ST depression is less specific and often occurs in normal
individuals.
Exercise testing is also a useful means of assessing the severity of coronary disease
and identifying highrisk individuals. For example, the amount of exercise that can
be tolerated and the extent and degree of any ST segment change provide a useful
guide to the likely extent of coronary disease.

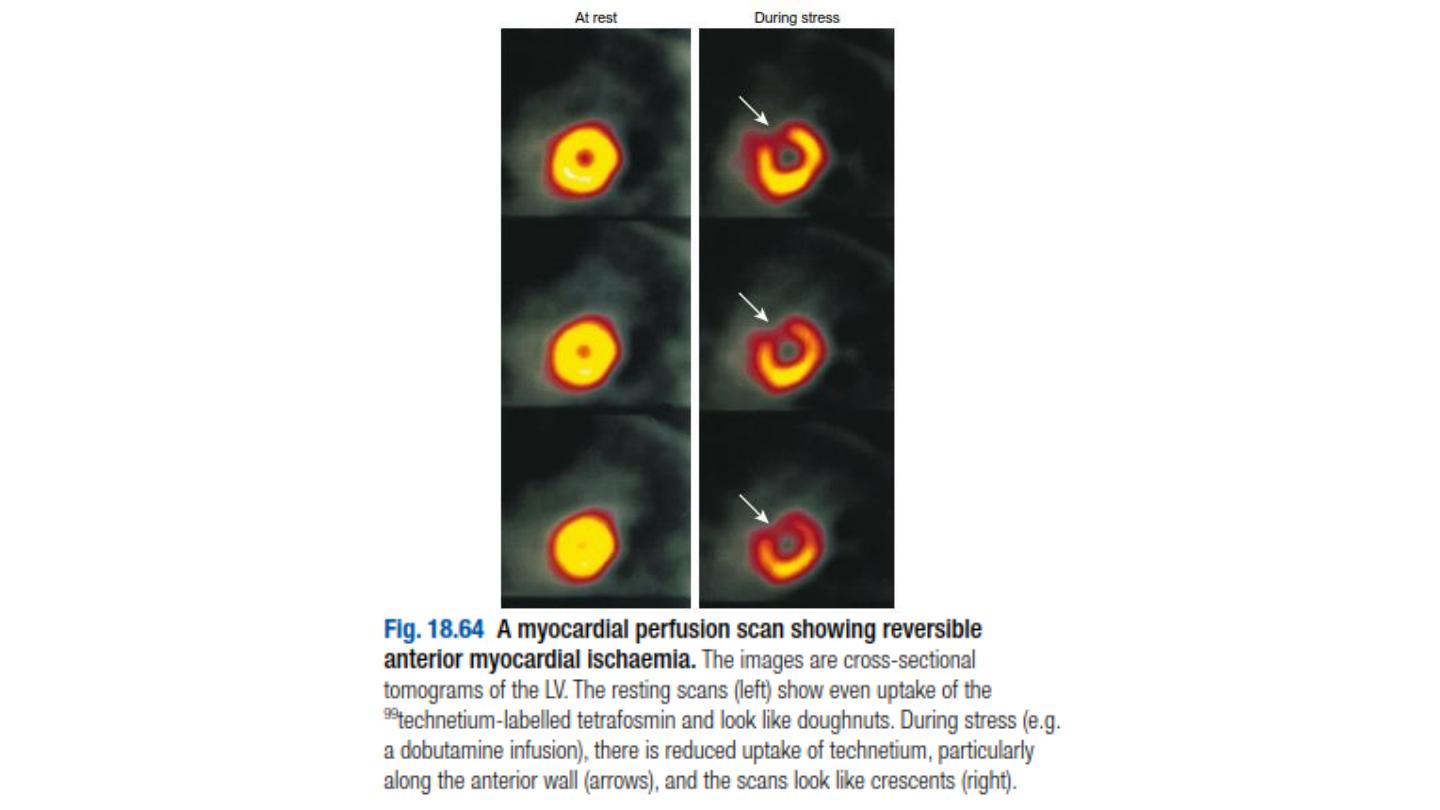
Other forms of stress testing
•
Myocardial perfusion scanning
. This may be helpful in the
evaluation of patients with an equivocal or uninterpretable exercise
test and those who are unable to exercise. It entails obtaining
scintiscans of the myocardium at rest and during stress (either
exercise testing or pharmacological stress, such as a controlled
infusion of dobutamine) after the administration of an intravenous
radioactive isotope, such as
99
technetium tetrofosmin. tetrofosmin
are taken up by viable perfused myocardium. A perfusion defect
present during stress but not at rest provides evidence of reversible
myocardial ischaemia,whereas a persistent perfusion defect seen
during both phases of the study is usually indicative of previous MI.
•
Stress echocardiography
.
This is an alternative to myocardial
perfusion scanning and can achieve similar predictive accuracy. It uses
transthoracic echocardiography to identify ischaemic segments of
myocardium and areas of infarction

Coronary arteriography
This provides detailed anatomical information about the extent and
nature of coronary artery disease ,and is usually performed with a view
to coronary artery bypass graft (CABG) surgery or percutaneous
coronary intervention .In some patients, diagnostic coronary
angiography may be indicated when non-invasive tests have failed to
establish the cause of atypical chest pain. The procedure is performed
under local anesthesia and requires specialized radiological equipment,
cardiac monitoring and an experienced operating team.

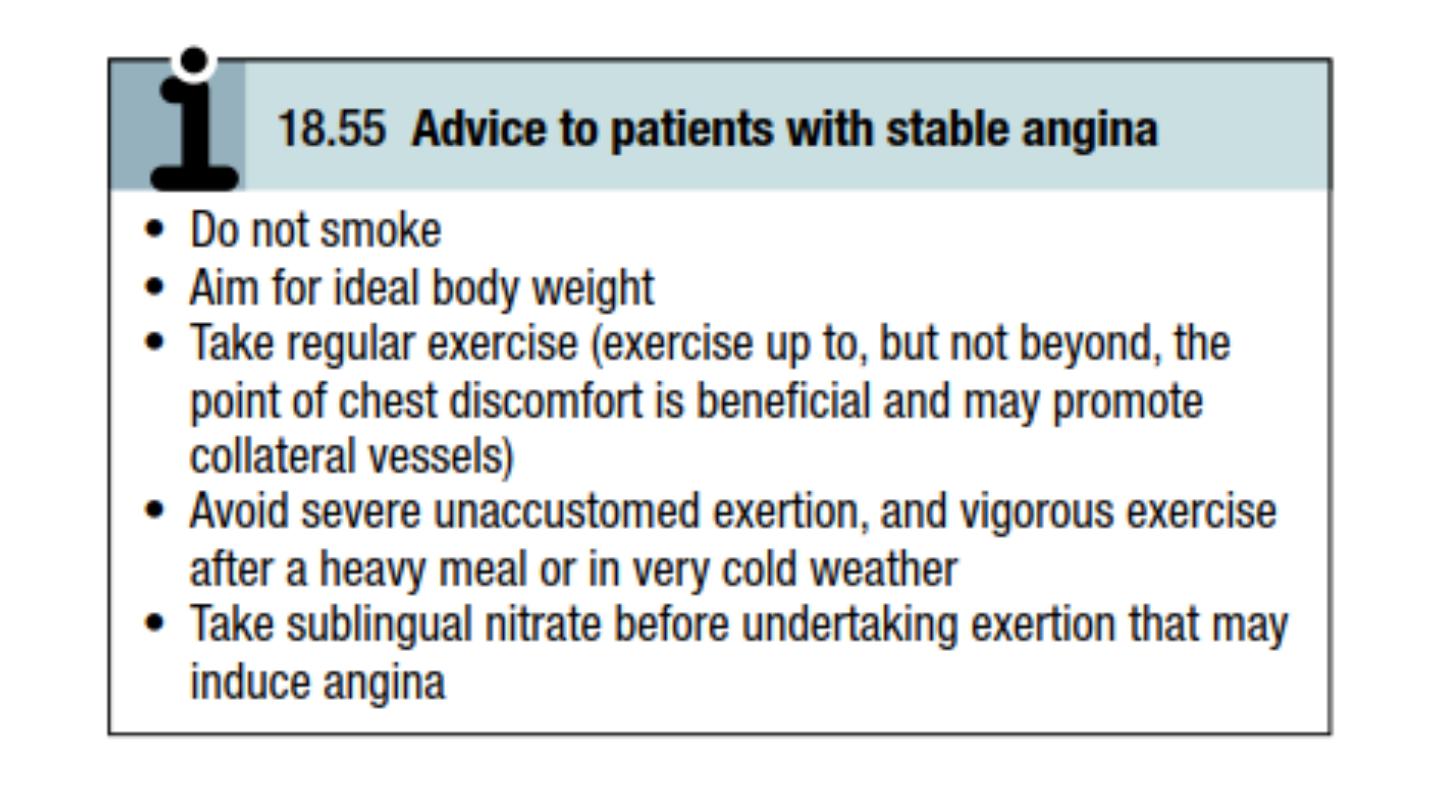
Management: general measures
The management of angina pectoris involves:
• a careful assessment of the likely extent and severity of arterial
disease
• the identification and control of risk factors such as smoking,
hypertension and hyperlipidemia
• the use of measures to control symptoms
• the identification of high-risk patients for treatment to improve life
expectancy.
Management should start with a careful explanation of the problem and
a discussion of the potential lifestyle and medical interventions that may
relieve symptoms and improve prognosis .

Antiplatelet therapy
Low-dose (75 mg) aspirin reduces the risk of adverse events such as MI and should be
prescribed for all patients with coronary artery disease indefinitely . Clopidogrel (75 mg
daily) is an equally effective antiplatelet agent that can be prescribed if aspirin causes
troublesome dyspepsia or other side-effects.
Anti-anginal drug treatment
Five groups of drug are used to help relieve or prevent the symptoms of angina: nitrates, β-
blockers, calcium antagonists, potassium channel activators and an I
f
channel antagonist.
1-
Nitrates
These drugs act directly on vascular smooth muscle to produce venous and arteriolar
dilatation. Their beneficial effects are due to a reduction in myocardial oxygen demand
(lower preload and afterload) and an increase in myocardial oxygen supply (coronary
vasodilatation). Sublingual glyceryl trinitrate (GTN) administered from a metered-dose
aerosol (400 μg per spray) or as a tablet (300 or 500 μg) will relieve an attack of angina in
2–3 minutes.
Side-effects include headache, symptomatic hypotension and, rarely, syncope.
GTN undergoes extensive first-pass metabolism in the liver and is ineffective when
swallowed.
2- Beta-blockers
reducing heart rate, BP and myocardial contractility, but they may provoke
bronchospasm in patients with asthma .slow-release metoprolol 50– 200 mg
daily, bisoprolol 5–15 mg daily. Beta-blockers should not be withdrawn
abruptly because this may have a rebound effect and precipitate dangerous
arrhythmias, worsening angina or MI.
3-
Calcium channel antagonists
reducing BP and myocardial contractility.
Amlodipin 2.5-10mg daily wich is ultra long acting
4-
Potassiu- channel activators
These have arterial and venous dilating properties. Nicorandil (10–30 mg 12-
hourly orally)
5-
I
f
channel antagonist
Ivabradine is the first of this class of drug. It induces bradycardia by
modulating ion channels in the sinus node. In contrast to β-blockers and
rate-limiting calcium antagonists, it does not have other cardiovascular
effects. It appears to be safe to use in patients with heart failure.

• then add a calcium channel antagonist or a long-acting nitrate later if
needed. The goal is the control of angina with minimum side-effects
and the simplest possible drug regimen. There is little evidence that
prescribing multiple anti-anginal drugs is of benefit, and
revascularisation should be considered if an appropriate combination
of two or more drugs fails to achieve an acceptable symptomatic
response.

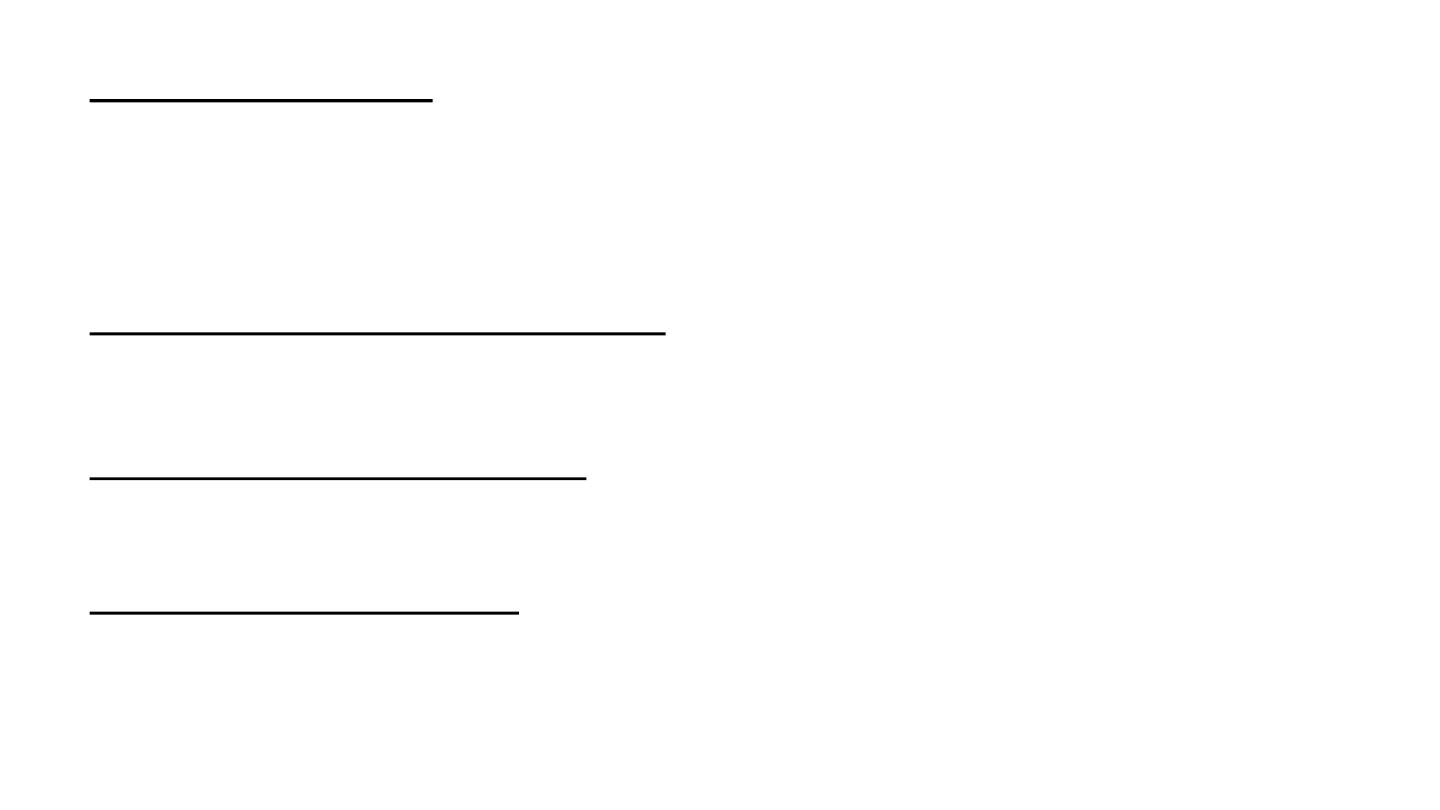
Invasive treatment
•
Coronary artery bypass grafting (CABG)
•
Percutaneous coronary intervention (PCI)

Prognosis
• Symptoms are a poor guide to prognosis; nevertheless, the 5-year
mortality of patients with severe angina is nearly double that of
patients with mild symptoms. Exercise testing and other forms of
stress testing are much more powerful predictors of mortality
• In general, the prognosis of coronary artery disease is related to the
number of diseased vessels and the degree of left ventricular
dysfunction,Spontaneous symptomatic improvement due to the
development of collateral vessels is common.

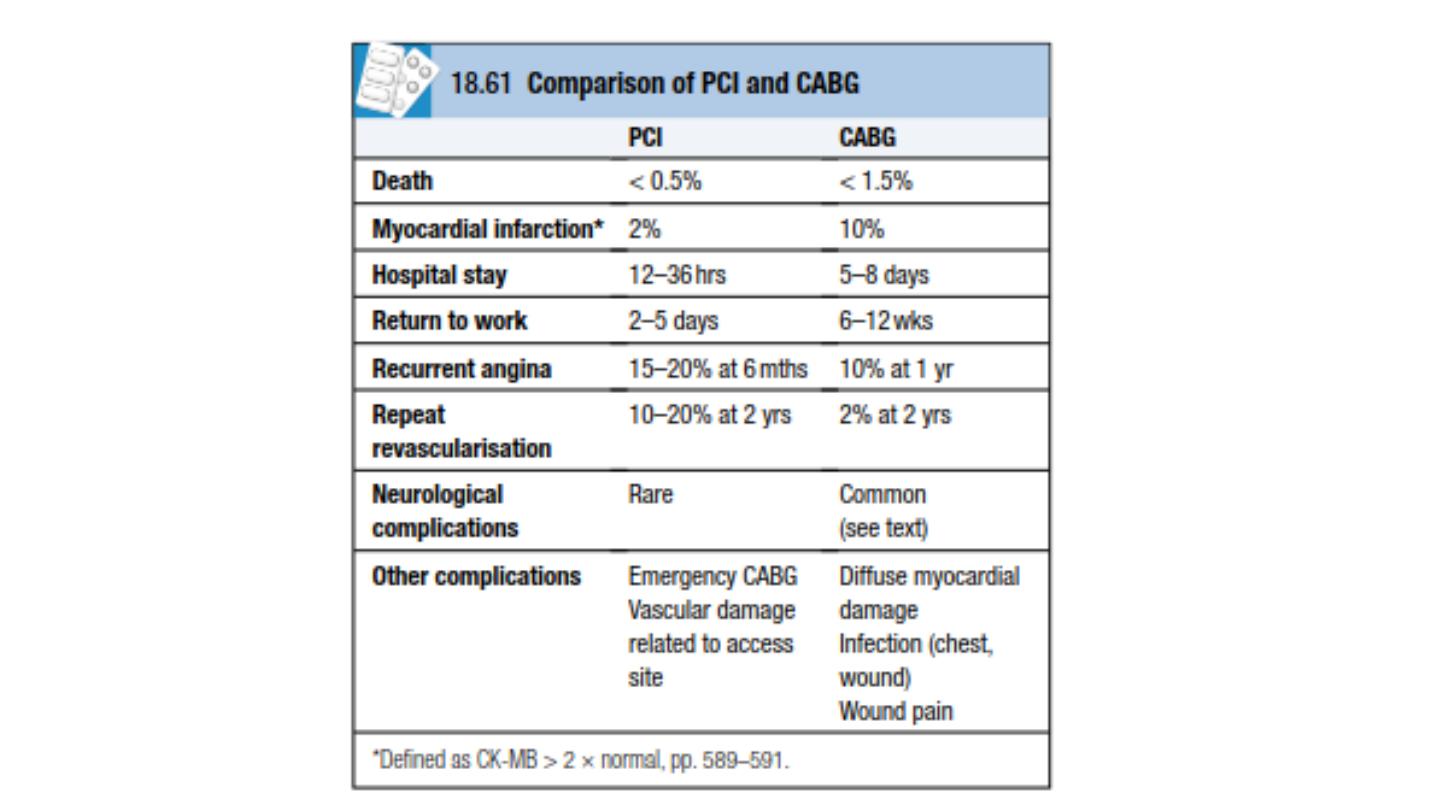
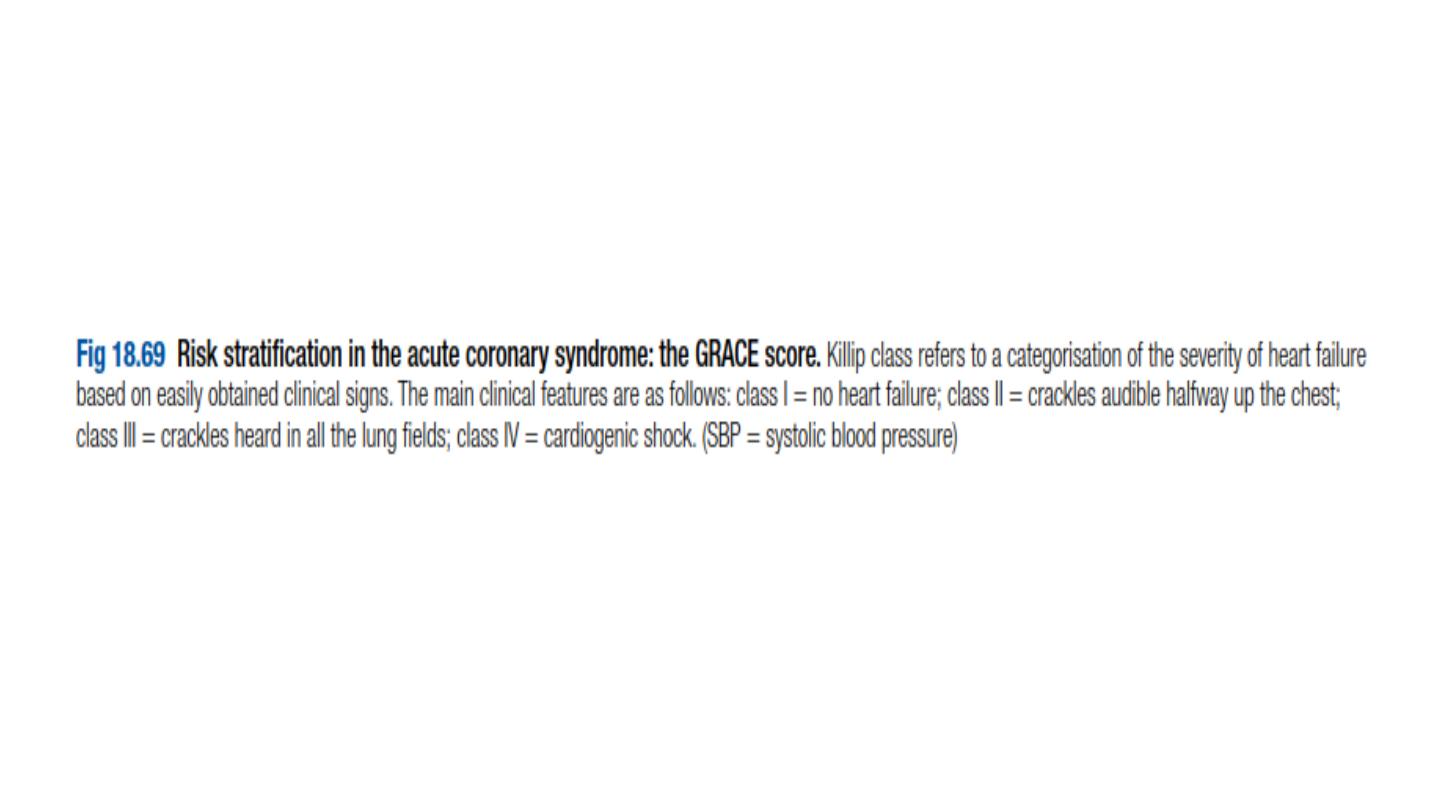
acute coronary syndrome
Acute coronary syndrome is a term that encompasses both unstable angina and MI.
Unstable angina is characterised by new-onset or rapidly worsening angina
(crescendo angina), angina on minimal exertion or angina at rest in the absence of
myocardial damage. In contrast, MI occurs when symptoms occur at rest and there
is evidence of myocardial necrosis, as demonstrated by an elevation in cardiac
troponin or creatine kinase-MB isoenzyme.
An acute coronary syndrome may present as a new phenomenon or against a
background of chronic stable angina. The culprit lesion is usually a complex
ulcerated or fissured atheromatous plaque with adherent plateletrich thrombus
and local coronary artery spasm .This is a dynamic process whereby the degree of
obstruction may either increase, leading to complete vessel occlusion, or regress
due to the effects of platelet disaggregation and endogenous fibrinolysis. In acute
MI, occlusive thrombus is almost alwayspresent at the site of rupture or erosion of
an atheromatous plaque. The thrombus may undergo spontaneous lysis over the
course of the next few days, although by this time irreversible myocardial damage
has occurred. Without treatment, the infarct-related artery remains permanently
occluded in 20–30% of patients. The process of infarction progresses over several
hours and most patients present when it is still possible to salvage myocardium and
improve outcome.

Investigations
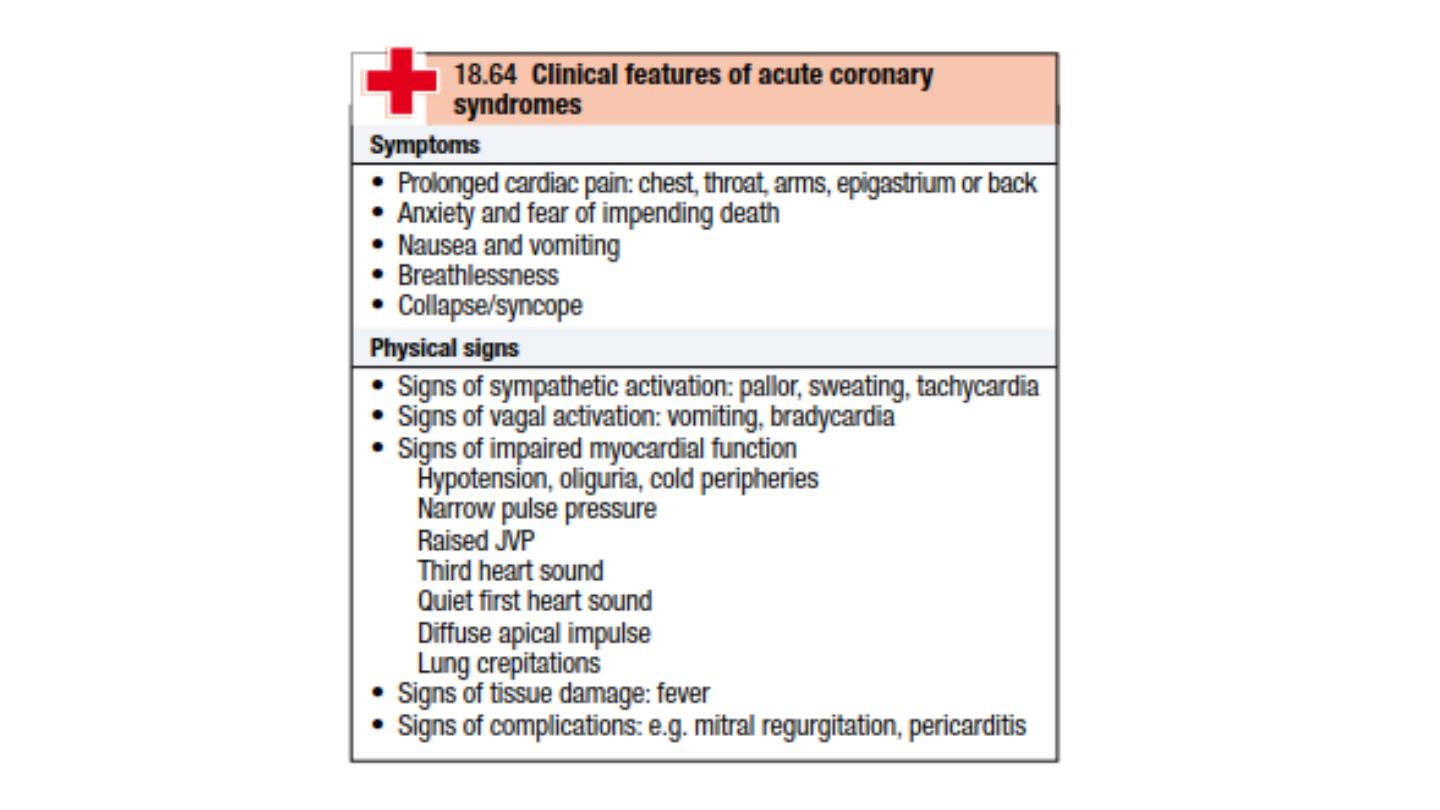
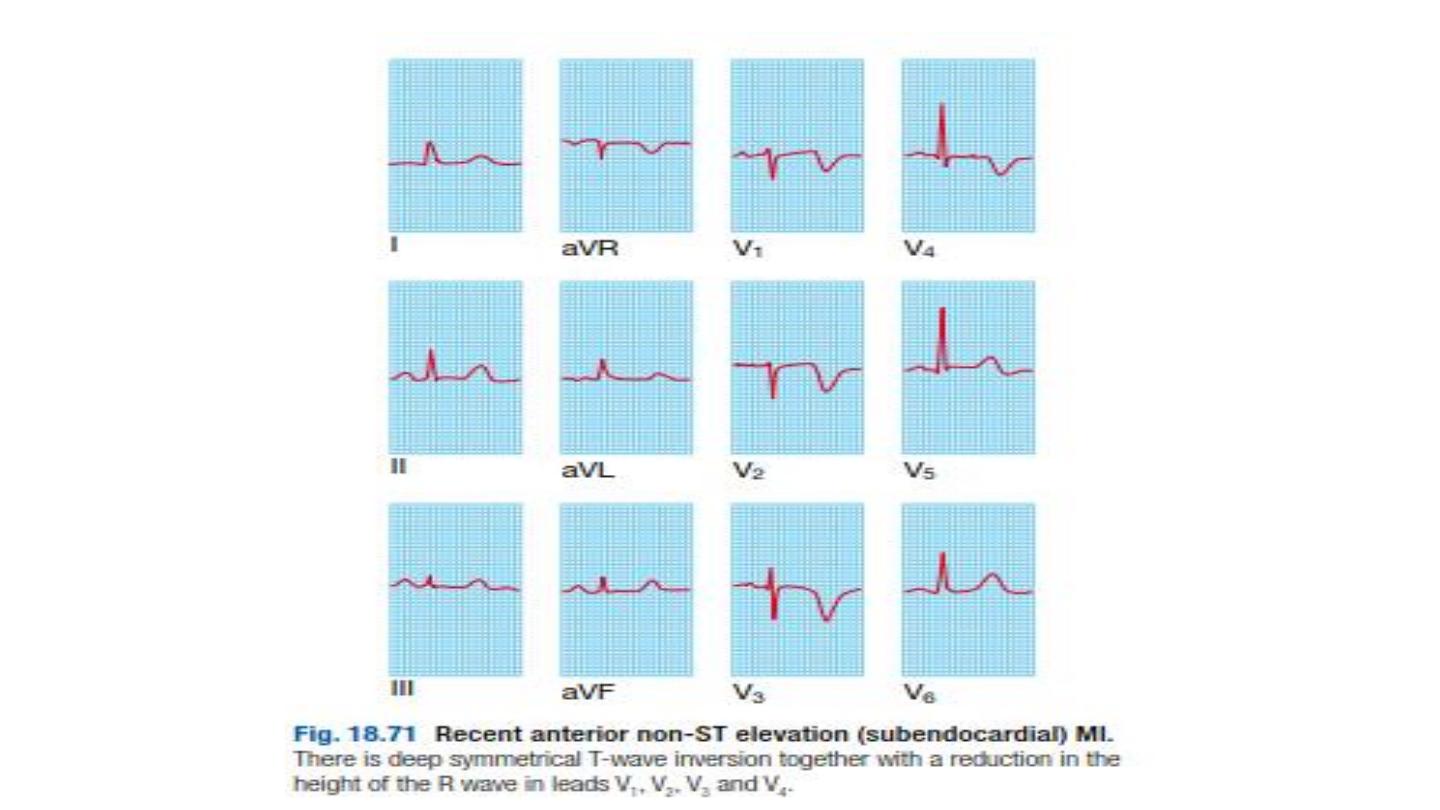
Electrocardiography
ST-segment elevation (or new bundle branch block) is seen initially with
later diminution in the size of the R wave, and in transmural (full
thickness) infarction, development of a Q wave.
Subsequently, the T wave becomes inverted because of a change in
ventricular repolarisation; this change persists after the ST segment has
returned to normal. These sequential features are sufficiently reliable
for the approximate age of the infarct to be deduced.

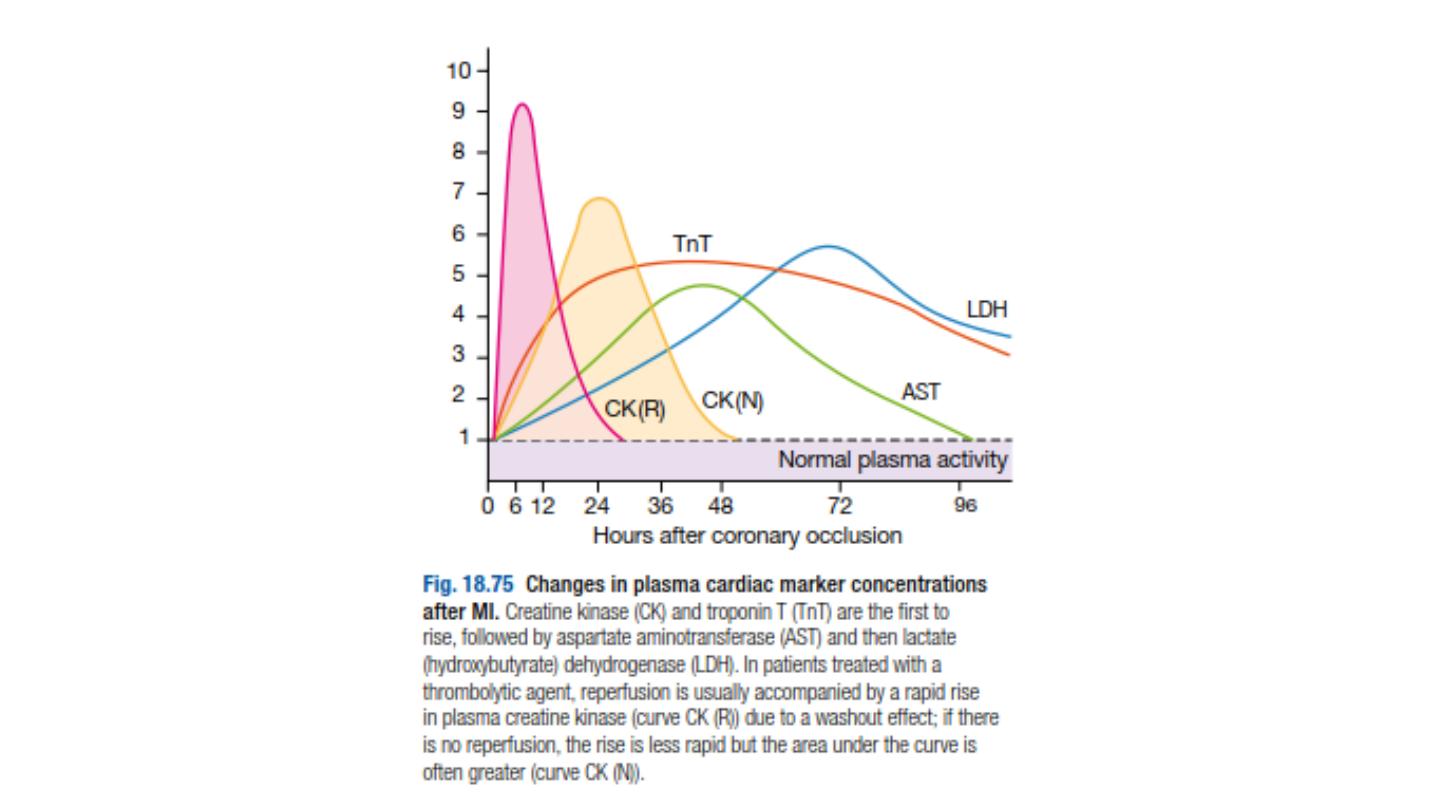
Plasma cardiac markers
These biochemical markers are creatine kinase (CK), a more sensitive
and cardiospecific isoform of this enzyme (CK-MB), and the
cardiospecific proteins, troponins T and I. CK starts to rise at 4–6 hours,
peaks at about 12 hours and falls to normal within 48–72 hours. CK is
also present in skeletal muscle, and a modest rise in CK (but not CK-
MB) may sometimes be due to an intramuscular injection, vigorous
physical exercise or, particularly in older people, a fall. Defibrillation
causes significant release of CK but not CK-MB or troponins. The most
sensitive markers of myocardial cell damage are the cardiac troponins T
and I, which are released within 4–6 hours and remain elevated for up
to 2 weeks.

Other blood tests
A leucocytosis is usual, reaching a peak on the first day. The erythrocyte
sedimentation rate (ESR) and C-reactive protein (CRP) are also elevated.
Chest X-ray
This may demonstrate pulmonary oedema that is not evident on
clinical examination .The heart size is often normal.
This is useful for assessing left and right ventricular function and for
detecting important complications such as mural thrombus, cardiac
rupture, ventricular septal defect, mitral regurgitation and pericardial
effusion.

Management
immediate management: the first 12 hours
Patients should be admitted urgently to hospital because there is a
significant risk of death or recurrent myocardial ischaemia during the
early unstable phase, and appropriate medical therapy can reduce the
incidence of these by at least 60%.
•
Analgesia
Adequate analgesia is essential not only to relieve distress, but also to
lower adrenergic drive and thereby reduce vascular resistance, BP,
infarct size and susceptibility to ventricular arrhythmias. Intravenous
opiates (initially morphine sulphate 5–10 mg or diamorphine 2.5–5 mg)
and antiemetics (initially metoclopramide 10 mg) should be
administered

•
Antithrombotic therapy
•
Antiplatelet therapy
In patients with acute coronary syndrome, oral administration of 75–300 mg
aspirin daily improves survival, with a 25% relative risk reduction in
mortality. The first tablet (300 mg) should be given orally within the first 12
hours and therapy should be continued indefinitely if there are no side-
effects. In combination with aspirin, the early (within 12 hours) use of
clopidogrel 600 mg, followed by 150 mg daily for 1 week and 75 mg daily
thereafter, ticagrelor (180 mg followed by 90 mg 12-hourly) is more effective
than clopidogrel in reducing vascular death, MI or stroke, and all-cause death
without affecting overall major bleeding risk.
•
Anticoagulants
Anticoagulation can be achieved using unfractionated heparin, fractioned
(low molecular weight) heparin. with low molecular weight heparin
(subcutaneous enoxaparin 1 mg/kg 12-hourly) being a reasonable
alternative. Anticoagulation should be continued for 8 days or until discharge
from hospital or coronary revascularisation.

•
Anti-anginal therapy
Sublingual glyceryl trinitrate (300–500 μg) is a valuable first-aid
measure in unstable angina or threatened infarction, and intravenous
nitrates (GTN 0.6–1.2 mg/ hour or isosorbide dinitrate 1–2 mg/hour)
are useful for the treatment of left ventricular failure and the relief of
recurrent or persistent ischaemic pain.
Intravenous β-blockers (e.g. atenolol 5–10 mg or metoprolol 5–15 mg
given over 5 mins) relieve pain, reduce arrhythmias and improve short-
term mortality in patients who present within 12 hours of the onset of
symptoms
A dihydropyridine calcium channel antagonist (e.g. nifedipine or
amlodipine) can be added to the β-blocker

•
Reperfusion therapy
Non-ST segment elevation acute coronary syndrome
Immediate emergency reperfusion therapy has no demonstrable benefit in
patients with non-ST segment elevation MI and thrombolytic therapy may be
harmful.
ST segment elevation acute coronary syndrome
Immediate reperfusion therapy restores coronary artery patency, preserves
left ventricular function and improves survival. Successful therapy is
associated with pain relief, resolution of acute ST elevation and sometimes
transient arrhythmias (e.g. idioventricular rhythm).
Primary percutaneous coronary intervention (PCI).
This is the treatment of
choice for ST segment elevation. Outcomes are best when it is used in
combination with glycoprotein IIb/IIIa receptor antagonists and
intracoronary stent implantation. When primary PCI cannot be achieved
within 2 hours of diagnosis, thrombolytic therapy should be administered.
Thrombolysis.
Alteplase (human tissue plasminogen activator or tPA) is given
over 90 minutes (bolus dose of 15 mg, followed by 50 mg, over 30 mins and
then 35 mg, over 60 mins). Its use is associated with better survival rates
than other thrombolytic agents, such as strepto-kinase, but carries a slightly
higher risk of intracerebralbleeding
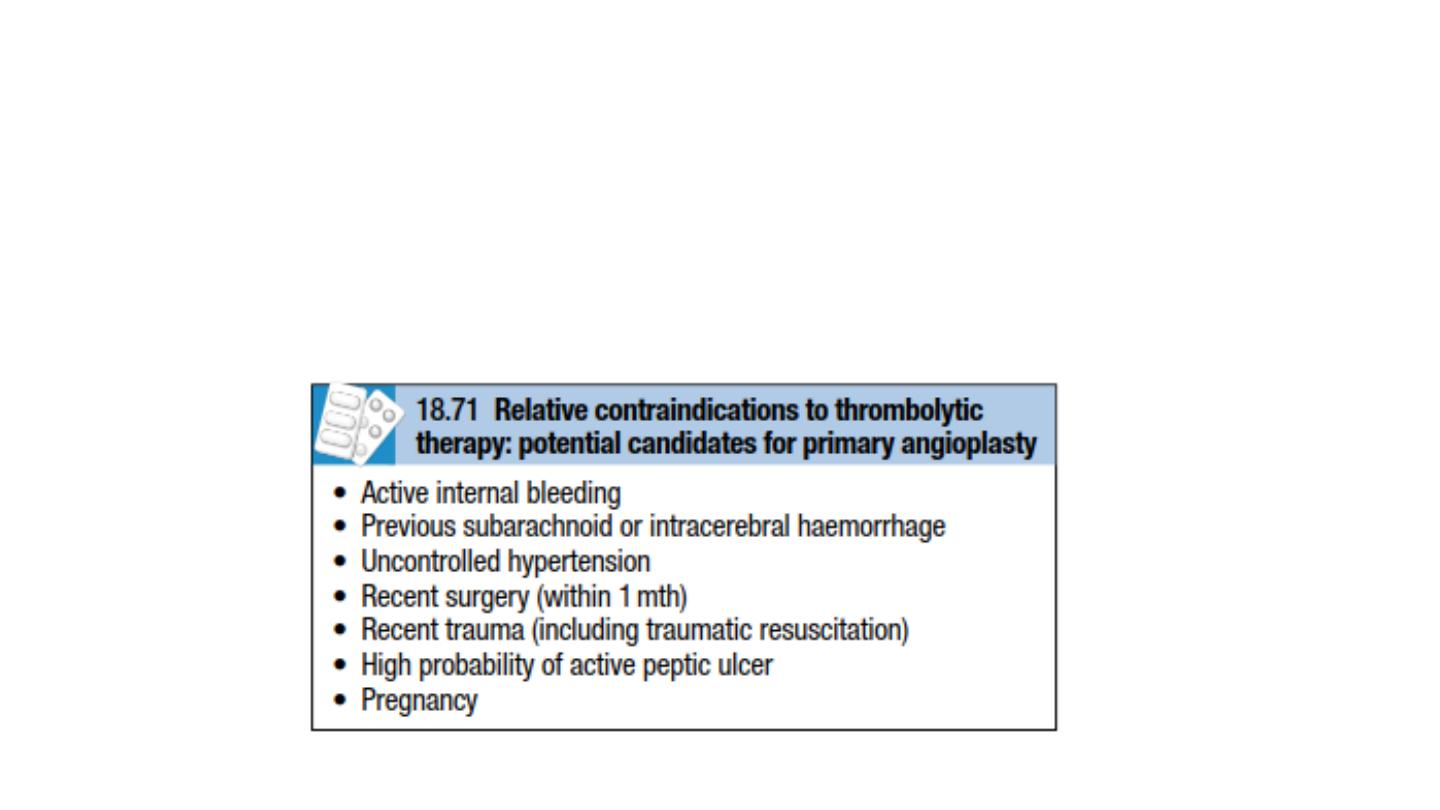
• The major hazard of thrombolytic therapy is bleeding. Cerebral
haemorrhage ,the treatment should be withheld if there is a
significant risk of serious bleeding.
• For some patients, thrombolytic therapy is contra-indicated or fails to
achieve coronary arterial reperfu-sion .Early emergency PCI may then
be considered, particularly where there is evidence of cardiogenic
shock.

Complications of acute coronary syndrome
•
Arrhythmias
•
Ventricular fibrillation
•
Atrial fibrillation
•
Acute circulatory failure
•
Pericarditis
•
Bradycardia
•
Ischaemia
•
Embolism
•
Impaired ventricular function, remodelling and ventricular
aneurysm

•
Mechanical complications
Part of the necrotic muscle in a fresh infarct may tear or rupture, with
devastating consequences:
Rupture of the papillary muscle
can cause acute pulmonary oedema and
shock due to the sudden onset of severe mitral regurgitation, which presents
with a pansystolic murmur and third heart sound.
In the presence of severe valvular regurgitation, the murmur may be quiet or
absent. The diagnosis is confirmed by echocardiography and emergency
mitral valve replacement may be necessary. Lesser degrees of mitral
regurgitation due to papillary muscle dysfunction are common and may be
transient.
Rupture of the interventricular septum
causes left-to-right shunting through
a ventricular septal defect. This usually presents with sudden haemodynamic
deterioration accompanied by a new loud pansystolic murmur radiating to
the right sternal border
Rupture of the ventricle
may lead to cardiac tamponade and is usually
Later in-hospital management

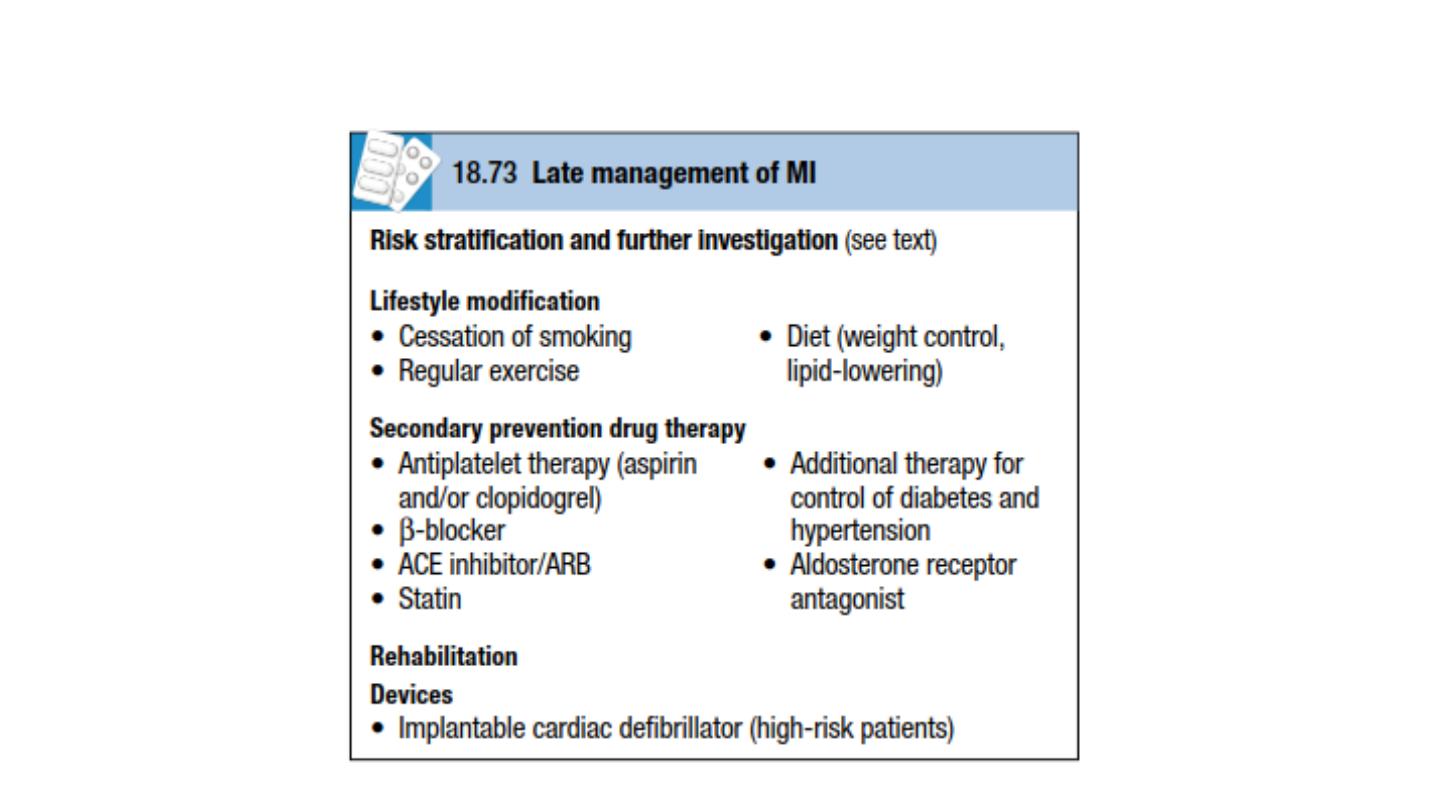
Secondary prevention drug therapy
*Aspirin and clopidogrel
*Beta-blockers
*Continuous treatment with an oral β-blocker
*ACE inhibitors
• patients with asymptomatic left ventricular dysfunction and those with
preserved left ventricular function. They should therefore be considered in all
patients with acute coronary syndrome. Caution must be exercised in
hypovolaemic or hypotensive patients because the introduction of an ACE
inhibitor may exacerbate hypotension and impair coronary perfusion. In patients
intolerant of ACE inhibitor therapy, angiotensin receptor blockers (e.g. valsartan
40–160 mg 12-hourly or candesartan 4–16 mg daily) are suitable alternatives and
are better tolerated.
• Patients with acute MI and left ventricular dysfunction (ejection fraction < 35%)
and either pulmonary oedema or diabetes mellitus further benefit from
additional aldosterone receptor antagonism (e.g. eplerenone 25–50 mg daily).

•
Device therapy
Implantable cardiac defibrillators are of benefit in preventing sudden
cardiac death in patients who have severe left ventricular impairment
(ejection fraction ≤ 30%) after MI.

Prognosis
In almost one-quarter of all cases of MI, death occurs within a few minutes
without medical care. Half the deaths occur within 24 hours of the onset of
symptoms and about 40% of all affected patients die within the first month.
The prognosis of those who survive to reach hospital is much better, with a
28-day survival of more than 85%. Patients with unstable angina have a
mortality approximately half those with MI.
Early death is usually due to an arrhythmia and is independent of the extent
of MI. However, late outcomes are determined by the extent of myocardial
damage and unfavourable features include poor left ventricular function, AV
block and persistent ventricular arrhythmias. The prognosis is worse for
anterior than for inferior infarcts. Bundle branch block and high cardiac
marker levels both indicate extensive myocardial damage. Old age,
depression and social isolation are also associated with a higher mortality.
Of those who survive an acute attack, more than 80% live for a further year,
about 75% for 5 years, 50% for 10 years and 25% for 20 years.

Mitral valve prolapse
This is also known as ‘floppy’ mitral valve and is one of the more
common causes of mild mitral regurgitation .It is caused by congenital
anomalies or degenerative myxomatous changes, and is sometimes a
feature of connective tissue disorders such as Marfan’s syndrome.
In its mildest forms, the valve remains competent but bulges back into
the atrium during systole, causing a midsystolic click but no murmur. A
click is not always audible and the physical signs may vary with both
posture and respiration.
Progressive elongation of the chordae tendineae leads to increasing
mitral regurgitation, and if chordal rupture occurs, regurgitation
suddenly becomes severe. This is rare before the fifth or sixth decade
of life.

Clinical features
• Mitral valve prolapse is associated with arrhythmias, atypical chest
pain and a very small risk of embolic stroke or TIA, the overall long-
term prognosis is good.
• Progressive elongation of the chordae tendineae leads to symtoms of
mitral regurgitation and then the clinical features of mitral
regurgitation will appear.
Prevention
• You can't prevent mitral valve prolapse. However, you can lower your
chances of developing the complications associated with it by making
sure you take your medications

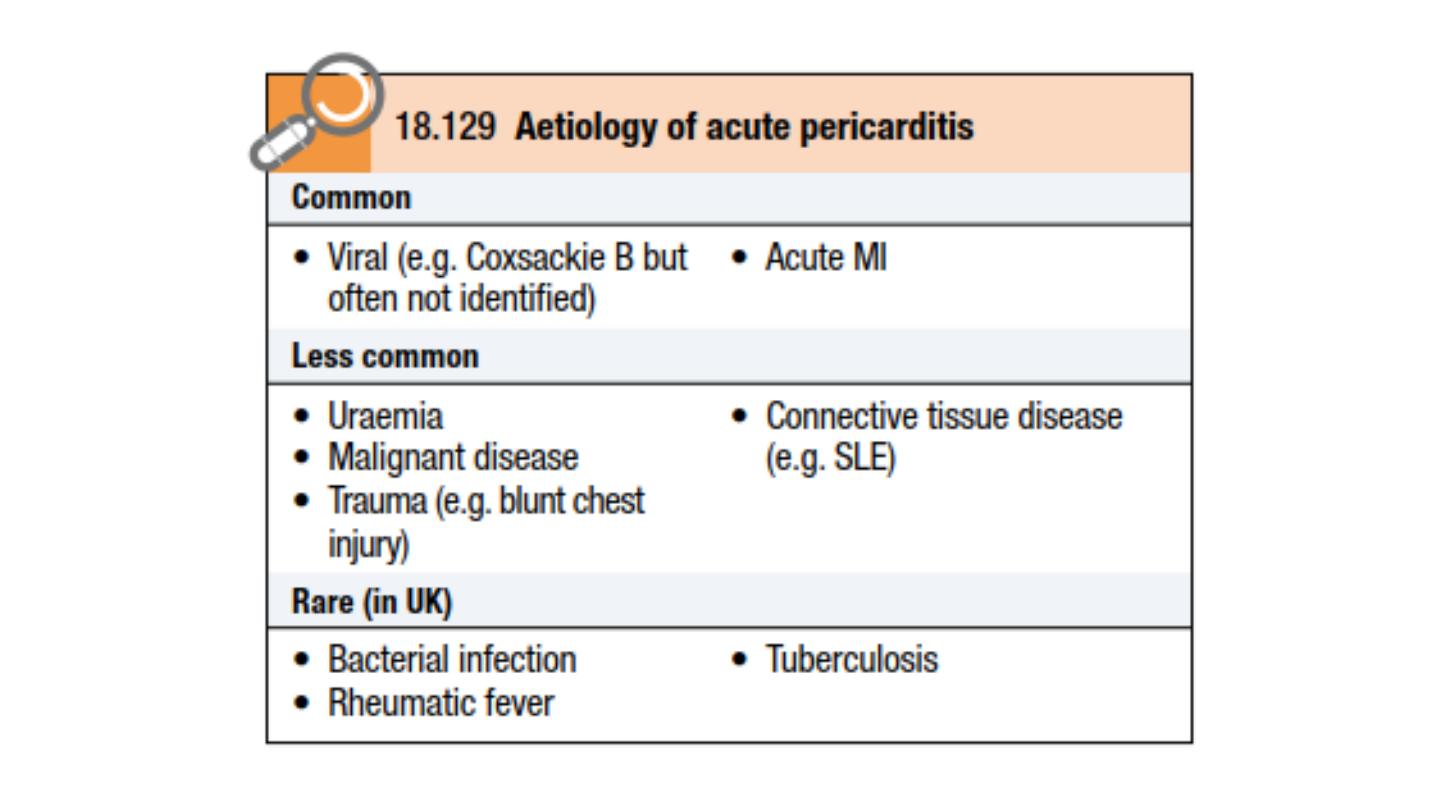
Acute pericarditis
Aetiology
• Pericarditis and myocarditis often coexist, and all forms of pericarditis may
produce a pericardial effusion that, depending on the aetiology, may be
fibrinous, serous, haemorrhagic or purulent.
• A fibrinous exudate may eventually lead to varying degrees of adhesion
formation
• Serous pericarditis often produces a large effusion of turbid, strawcoloured
fluid with a high protein content.
• A haemorrhagic effusion is often due to malignant disease, particularly
carcinoma of the breast or bronchus, and lymphoma.
• Purulent pericarditis is rare and may occur as a complication of
septicaemia, by direct spread from an intra-thoracic infection, or from a
penetrating injury.

Clinical features
• The characteristic pain of pericarditis is retrosternal, radiates to the shoulders and neck,
and is typically aggravated by deep breathing, movement, a change of position, exercise
and swallowing. A low-grade fever is common.
• A pericardial friction rub is a high-pitched superficial scratching or crunching noise
produced by movement of the inflamed pericardium and is diagnostic of pericarditis
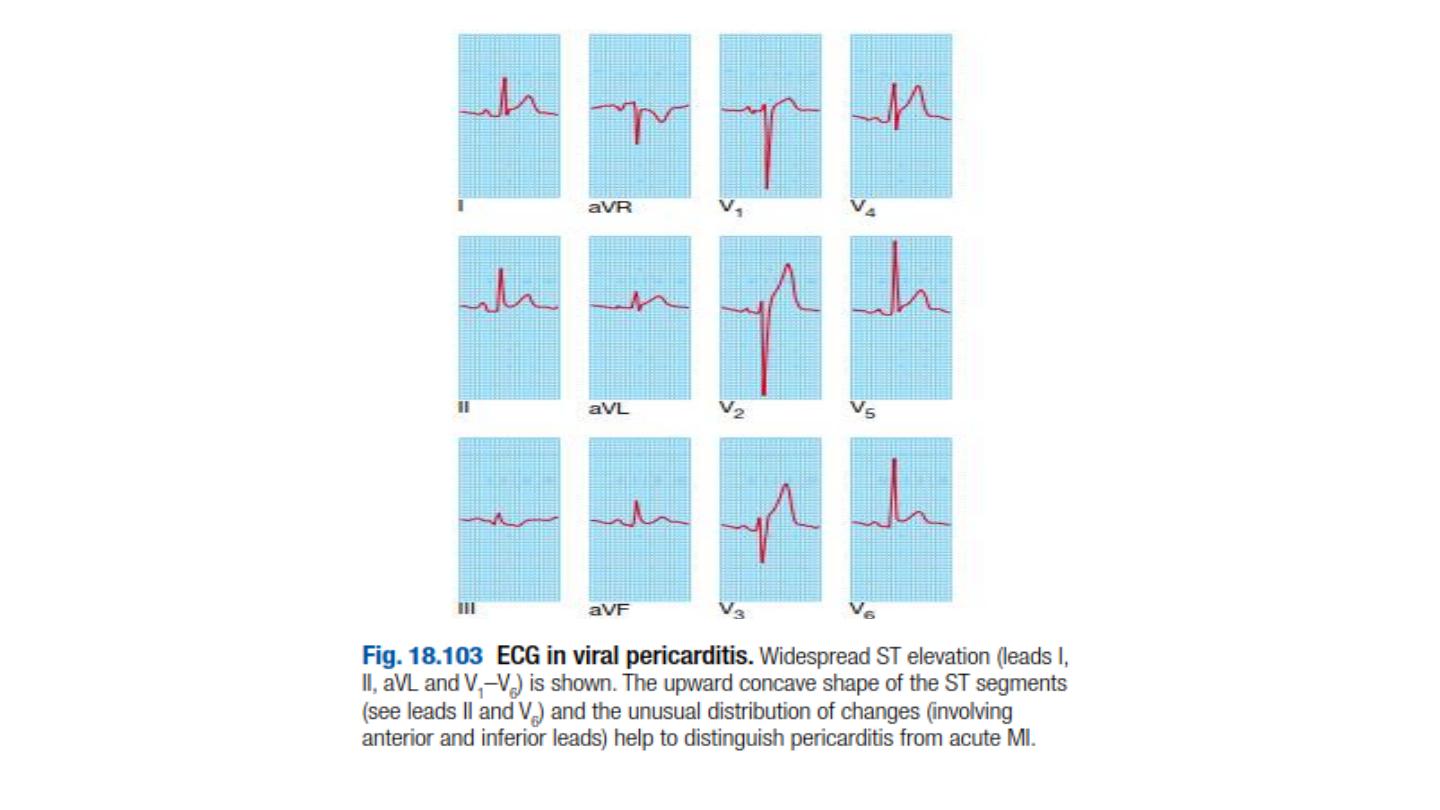
Investigations and management
• The ECG shows ST elevation with upward concavity over the affected area, which may be
widespread. PR interval depression is a very specific indicator of acute pericarditis. Later,
there may be T-wave inversion, particularly if there is a degree of myocarditis.
• The pain is usually relieved by aspirin (600 mg 4-hourly) but a more potent anti-
inflammatory agent such as indometacin (25 mg 8-hourly) may be required.
Corticosteroids may suppress symptoms but there is no evidence that they accelerate
cure.
• In viral pericarditis, recovery usually occurs within a few days or weeks but there may be
recurrences (chronic relapsing pericarditis). Purulent pericarditis requires treatment with
antimicrobial therapy, pericardiocentesis and, if necessary, surgical drainage.

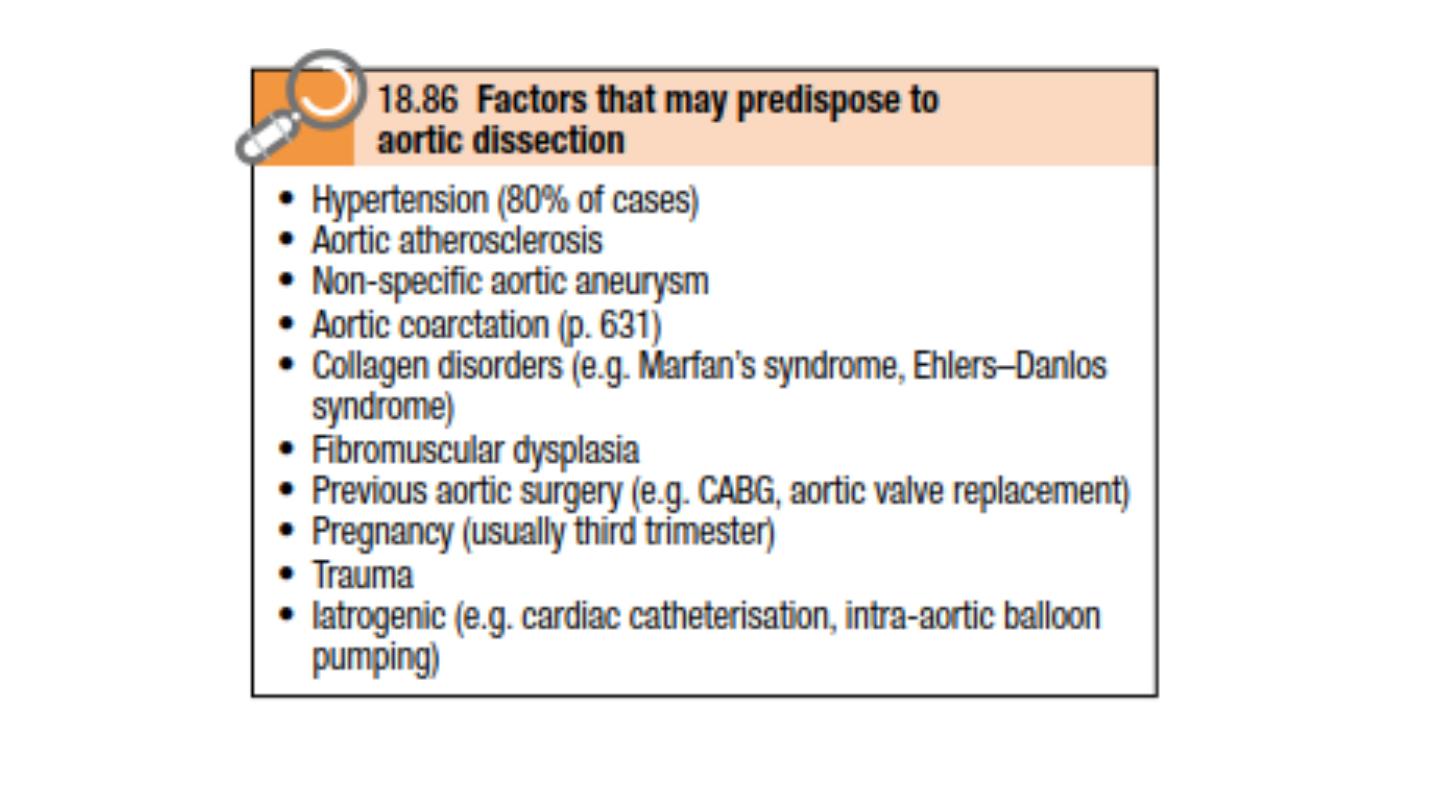
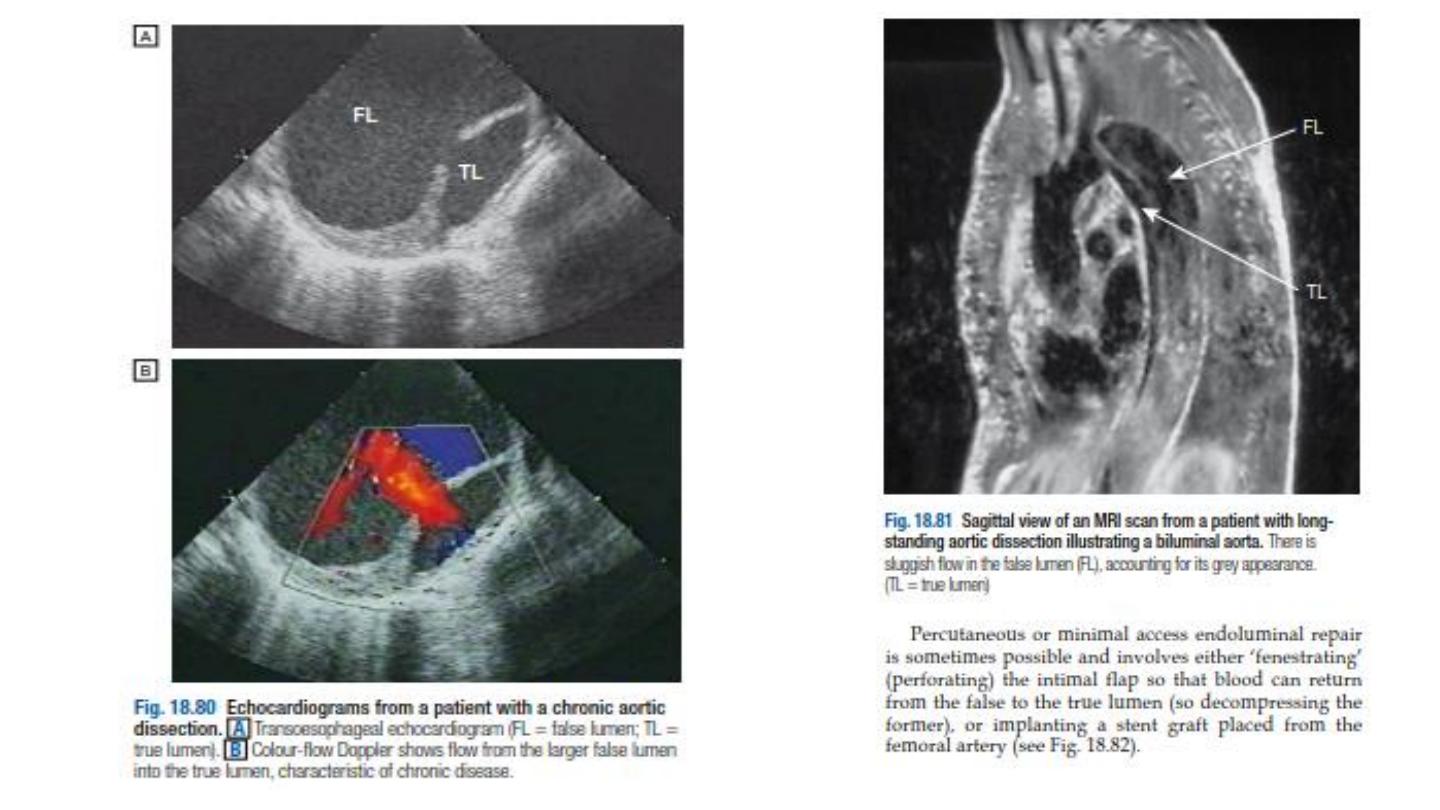
Aortic dissection
• A breach in the integrity of the aortic wall allows arterial blood to
enter the media, which is then split into two layers, creating a ‘false
lumen’ alongside the existing or ‘true lumen’ .The aortic valve may be
damaged and the branches of the aorta may be compromised.
Typically, the false lumen eventually re-enters the true lumen,
creating a double-barrelled aorta, but it may also rupture into the left
pleural space or pericardium with fatal consequences.

• Disease of the aorta and hypertension are the most important
aetiological factors but a variety of other conditions may be
implicated .Chronic dissections may lead to aneurysmal dilatation of
the aorta, and thoracic aneurysms may be complicated by dissection.
It is therefore sometimes difficult to identify the primary pathology.
• The peak incidence is in the sixth and seventh decades of life but
dissection can occur in younger patients, most commonly in
association with Marfan’s syndrome, pregnancy or trauma; men are
twice as frequently affected as women.
• Aortic dissection is classified anatomically and for management
purposes into type A and type B ,involving or sparing the ascending
aorta respectively. Type A dissections account for two-thirds of cases
and frequently also extend into the descending aorta.

•
Clinical features
• Involvement of the ascending aorta typically gives rise to
• anterior chest pain, and involvement of the descending aorta to
intrascapular pain. The pain is typically described as ‘tearing’ and very
abrupt in onset.
• collapse is common. Unless there is major haemorrhage, the patient
is invariably hypertensive.
• There may be asymmetry of the brachial, carotid or femoral pulses
and signs of aortic regurgitation.
• Occlusion of aortic branches may cause MI (coronary), stroke (carotid)
paraplegia (spinal), mesenteric infarction with an acute abdomen
(coeliac and superior mesenteric), renal failure (renal) and acute limb
(usually leg) ischaemia.

Investigations
• The chest X-ray characteristically shows broadening of the upper
mediastinum and distortion of the aortic, A left-sided pleural effusion is
common.
• The ECG may show left ventricular hypertrophy in patients with
hypertension, or rarely changes of acute MI (usually inferior).
• Doppler echocardiography may show aortic regurgitation, a dilated aortic
root and, occasionally, the flap of the dissection.
• Transoesophageal echocardiography is particularly helpful because
transthoracic echocardiography can only image the first 3–4 cm of the
ascending aorta .CT and MRI angiogra-phy are both highly specific and
sensitive.
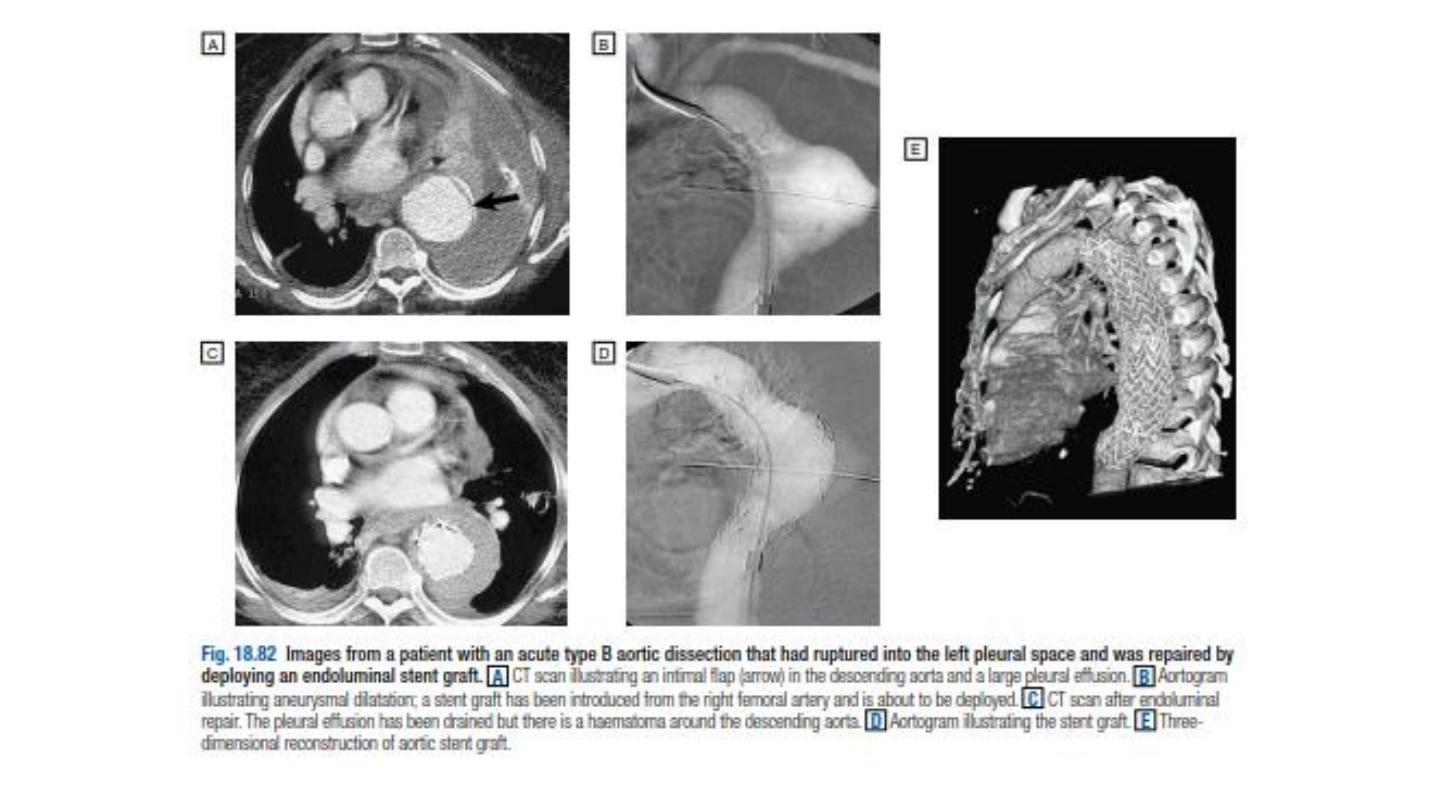

Management
• Initial management comprises pain control and antihypertensive
treatment.
• Type A dissections require emergency surgery to replace the ascending
aorta. Type B aneurysms are treated medically unless there is actual or
impending external rupture, or vital organ (gut, kidneys) or limb ischaemia,
as the morbidity and mortality associated with surgery is very high. The
aim of medical management is to maintain a mean arterial pressure (MAP)
of 60–75 mmHg to reduce the force of the ejection of blood from the LV.
• First-line therapy is with β-blockers; the additional α-blocking properties of
labetalol make it especially useful.
• Rate-limiting calcium channel blockers, such as verapamil or diltiazem, are
used if β-blockers are contraindicated. Sodium nitroprusside
• may be considered if these fail to control BP adequately.
