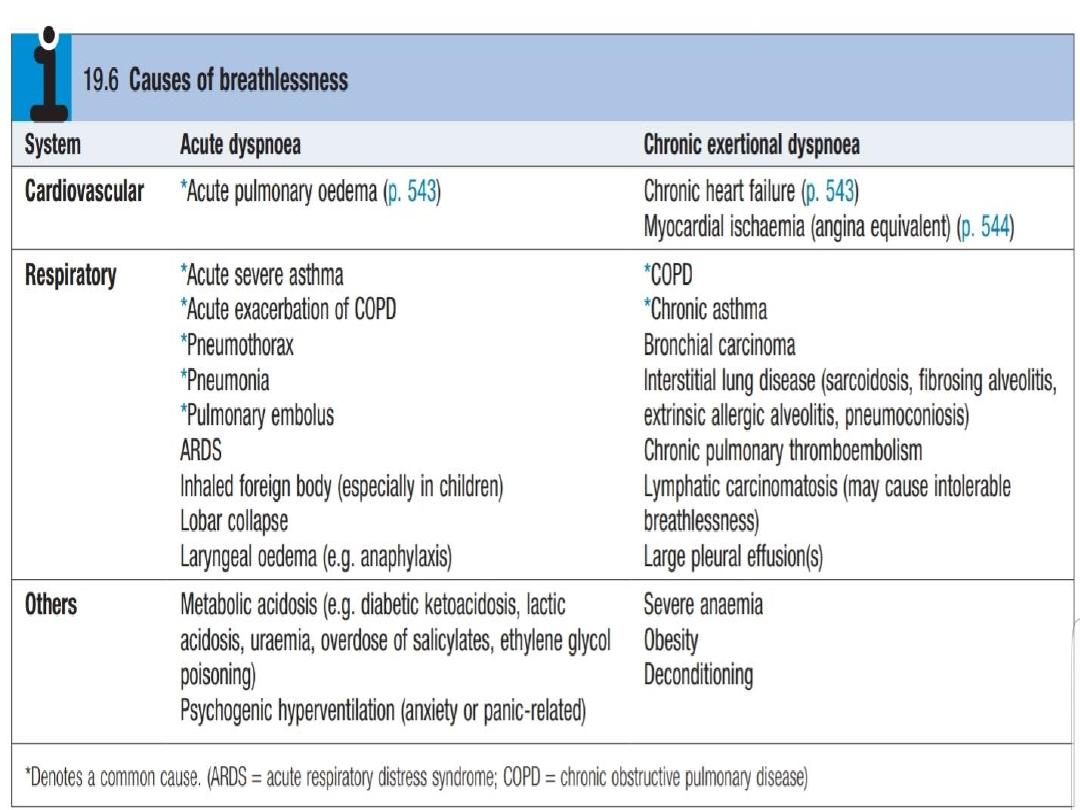
Acute dyspnea
(breathlessness)

jassim adnan

• Breathlessness
or
dyspnoea
can be defined
as the feeling of an uncomfortable need to
breathe. It is unusual among sensations in
having no defined receptors, no localised
representation in the brain, and multiple
causes both in health (e.g. exercise) and in
diseases of the lungs, heart or muscles.

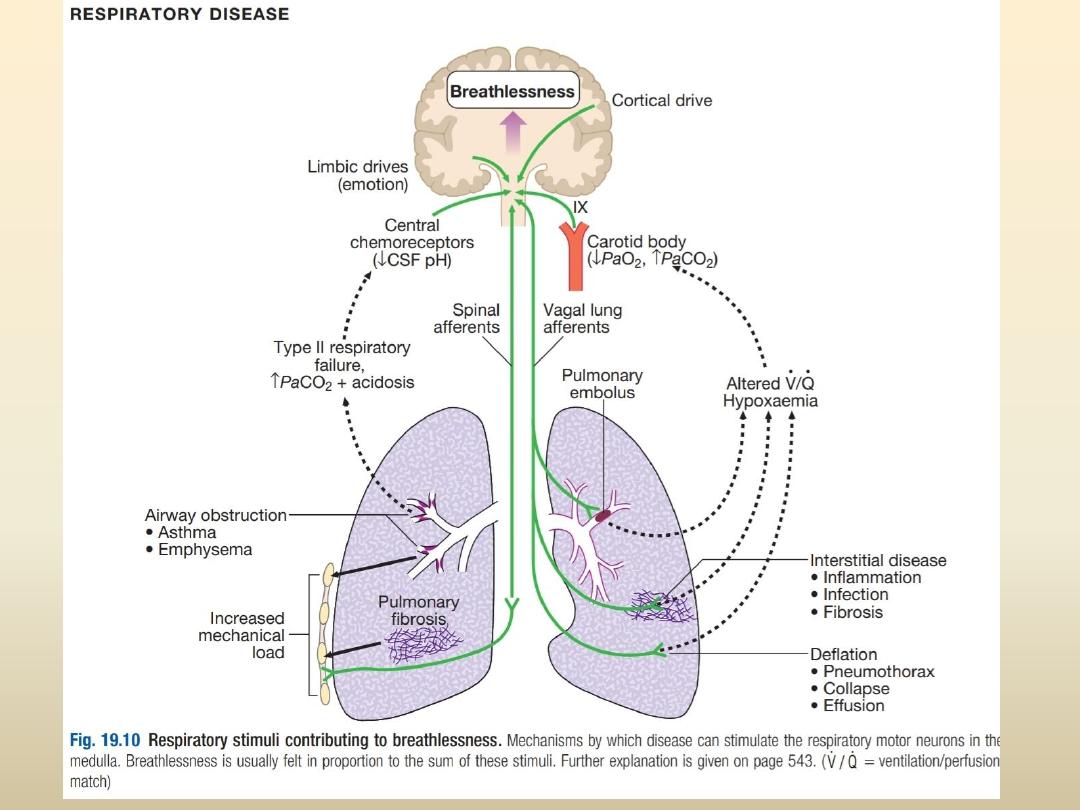
Pathophysiology
Respiratory diseases can stimulate breathing and
dyspnoea by
• stimulating intrapulmonary sensory nerves (e.g.
pneumothorax, interstitial inflammation and
pulmonary embolus),
• by increasing the mechanical load on the
respiratory muscles (e.g. airflow obstruction or
pulmonary fibrosis)
• by causing hypoxia, hypercapnia or acidosis,

• In cardiac failure, pulmonary congestion
reduces lung compliance and can also obstruct
the small airways
• Reduced cardiac output also limits oxygen
supply to the skeletal muscles during exercise,
causing early lactic acidaemia and further
stimulating breathing via the central
chemoreceptors.

presentation
History
• It is important to establish the rate of onset and
severity of the breathlessnes .Acute severe
breathlessness occur over minutes or hours
• Present of cardiovascular symptoms (chest pain,
palpitations, sweating and nausea) or respiratory
symptoms (cough, wheeze, haemoptysis, stridor).
• A previous history of repeated episodes of left
ventricular failure, asthma or exacerbations of COPD is
valuable.
• In children, the possibility of inhalation of a foreign
body or acute epiglottitis should always be considered

The following should be assessed and documented:
• level of consciousness
• degree of central cyanosis
• work of breathing (rate, depth, pattern, use of accessory muscles)
• adequacy of oxygenation (
SpO2)
• evidence of anaphylaxis (urticaria or angioedema)
• patency of the upper airway
• ability to speak (in single words or sentences)
• cardiovascular status (heart rate and rhythm, blood pressure and
degree of peripheral perfusion).
Airway obstruction, anaphylaxis and tension pneumothorax require
immediate identification and treatment.
Clinical assessment

Associated features
• pink, frothy sputum ,bi-basal crackles suggest
pulmonary edema
• Wheezes and prolonged expiration suggest
asthma and COPD
• silent resonant hemithorax suggest pneumothorax
• Severe breathlessness with normal breath sound
suggest pulmonary embolism
• Leg swelling suggest heart failure , or if
asymmetrical suggest vien thrombosis

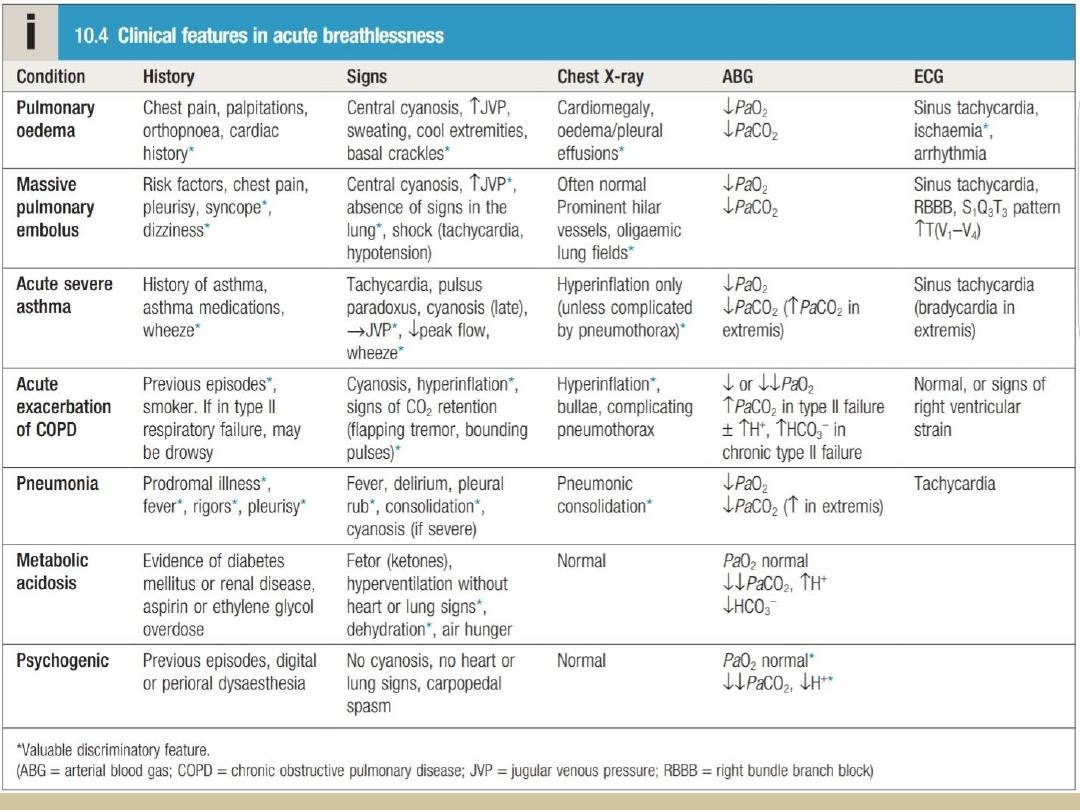
Initial investigation
• Chest X-ray
• ECG
• Arterial blood gases
• Peak expiratory flow to assess severity
whenever possible
First three with proper history and clinical assessment
can reach the primary cause of breathlessness

mudar hazim

Acute left heart failure
• This is characterized by a reduction in left ventricular
output , increase In left ventricular diastolic pressure and
an increase in left atrial and pulmonary venous pressure.
• When the hydrostatic pressure of the pulmonary
capillaries exceeds the oncotic pressure of plasma (about
25–30 mmHg), fluid moves from the capillaries into alveoli
that lead to pulmonary edema. This stimulates respiration
through a series of autonomic reflexes, producing rapid
shallow respiration. Congestion of the bronchial mucosa
may cause wheeze (cardiac asthma).
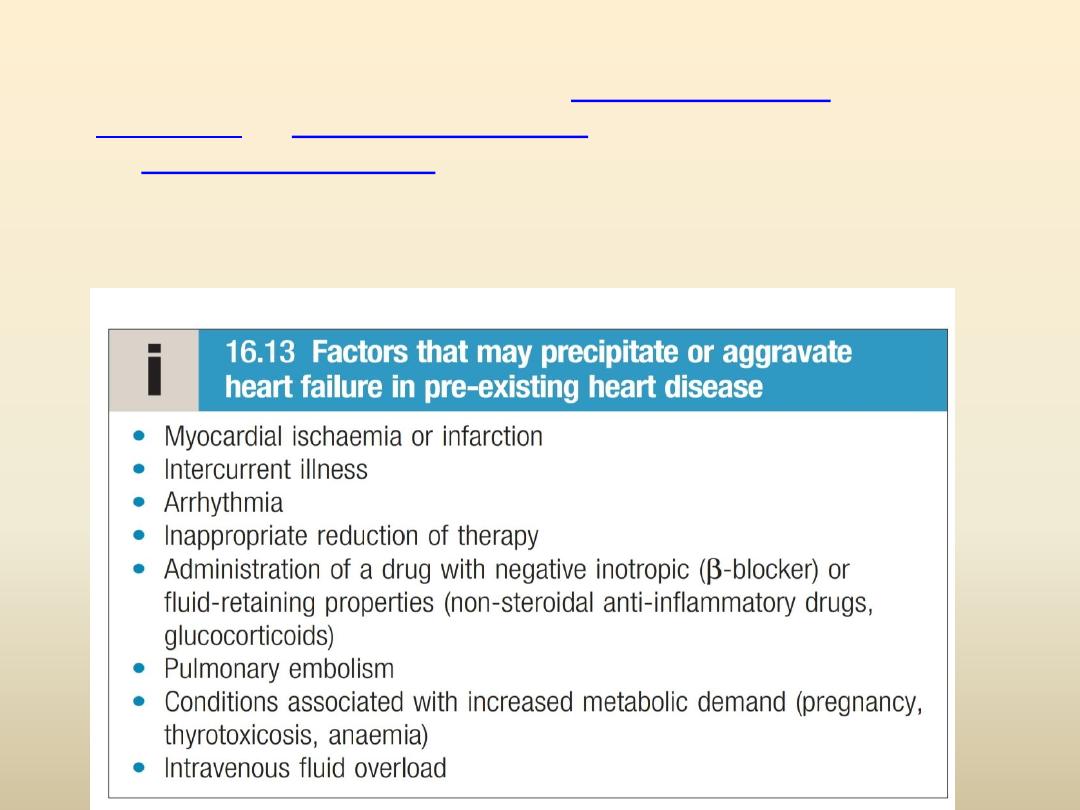
• It is most often precipitated by
or
, but can be caused
, and other causes .it can occur in
previously healthy heart as well as diseased heart with
preciptiating illness
• Acute on chronic heart failure

presentation
• a
sudden onset of dyspnoea
at rest that rapidly
progresses to acute respiratory distress
• orthopnoea
and
prostration.
• Often with precipitating factors like acute MI
• The patient appears
agitated
,
pale
and
clammy
• Cold extremities
and
rapid pulse
, but some times
bradycardia
that may contribute in this acute episode of
HF
• Pink frothy
or
blood stained sputum
• Blood pressure is
elevated
due to activation of SNS ,or
normal
or
low
in cardiogenic shoke
• The
JVP
is usually elevated, particularly with associated
fluid overload or right heart failure.

• A ‘
gallop
’ rhythm, with a
third heart sound
, is
heard
• A
new systolic murmur
may signify acute mitral
regurgitation or ventricular septal rupture
• Fine Basal crepitations ,
or throughout lungs if
severe case
• Expiratory wheezes
• Additional feature of chronic heart failure (in
acute on
chronic HF
)

Investigations
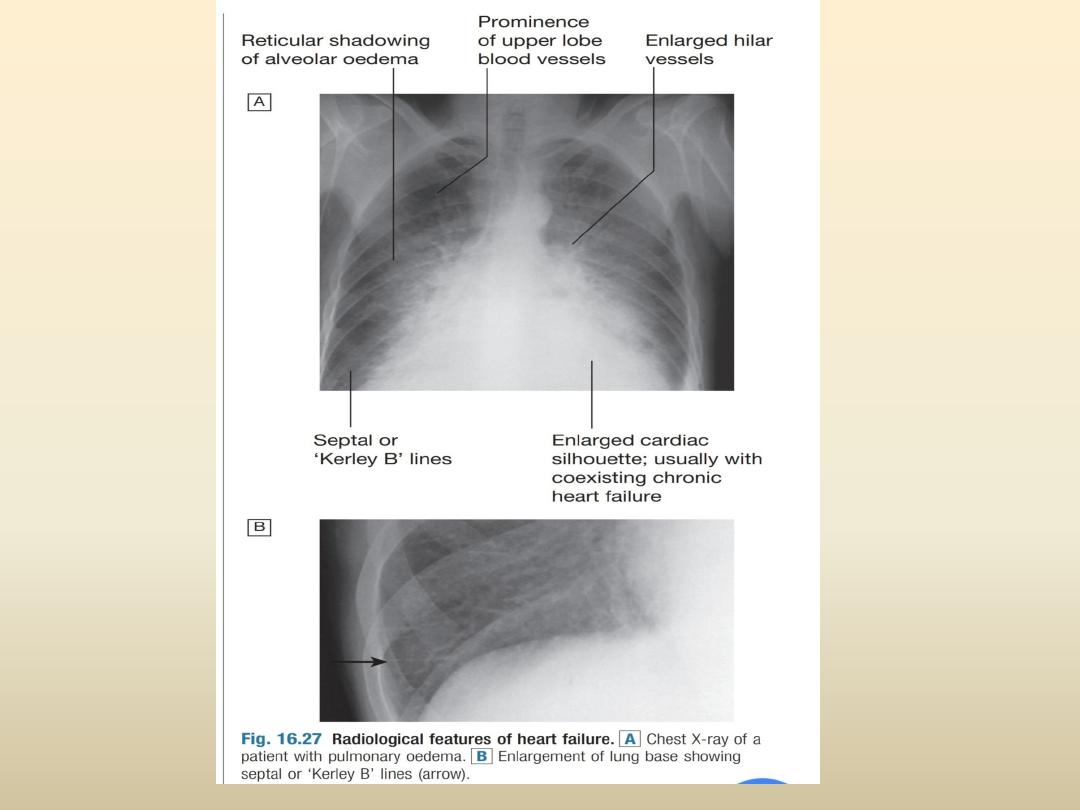
• Chest X-ray : increase vascularity, cardiomegaly,
thickened interlobular septa and dilated
lymphatics ( kerly B lines) , bilateral reticular
shadowing and pleural effusion
• Echocardiography to determine etiology
• ECG ,detect etiology (eg:-acute MI)
• Serum urea, creatinine and electrolytes,
haemoglobin and thyroid function determine
nature and severety of underlying disease and
complications

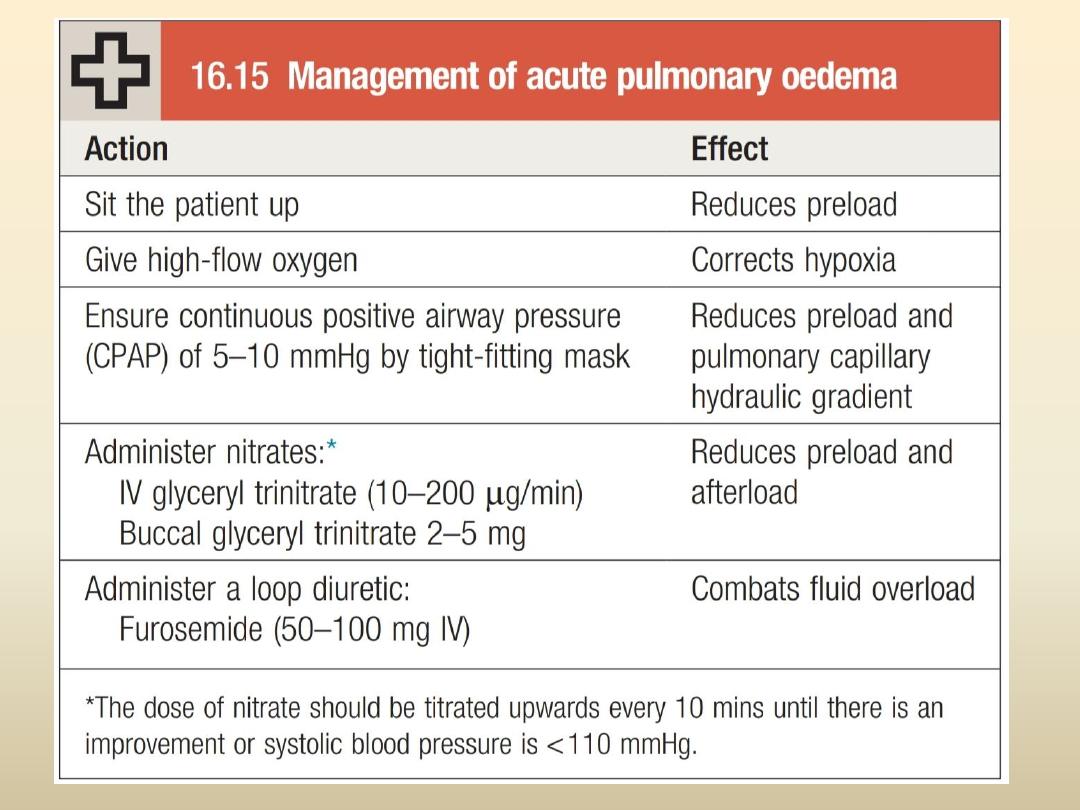
management
• Hospitalization
, rest
and
upright position
with continuous
heart monitoring , BP ad pulse oximetry
• IV opiate
( but give with caution )
• Oxygen high flow
• Diuretics
, (furosemide IV 50-100 mg)
• Inotropics
like dopamine or doputamine to augment
cardiac function especially in hypotensive patient
• IV nitrate infusion
or sublingual glyceryle trinitrate
• intra-aortic balloon pump
may be beneficial in patients
with acute cardiogenic pulmonary oedema and shock.
`
Other elements of management are summerized in
box 16.15

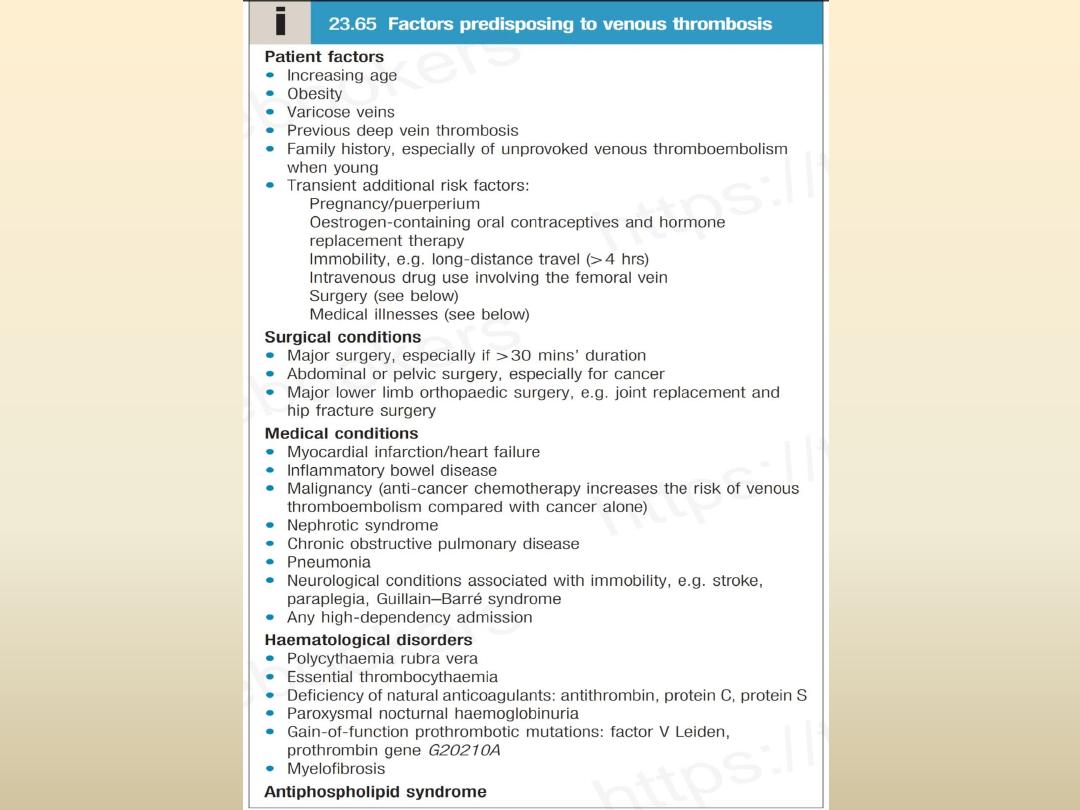
Pulmonary embolism
• The majority of pulmonary emboli arise from
the propagation of lower limb deep vein
thrombosis . other rare causes like septic
emboli , choriocarcinoma, fat following
fracture of long bones such as the femur, air,
and amniotic fluid, which may enter the
mother’s circulation following delivery.

presentation
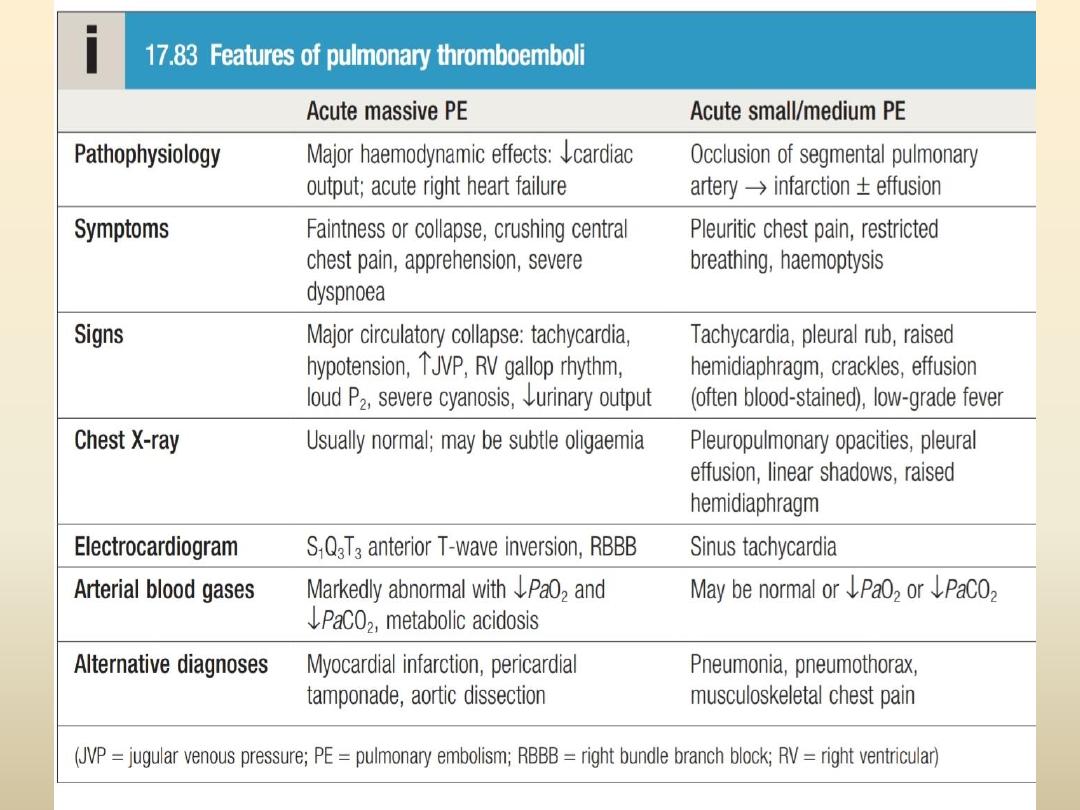

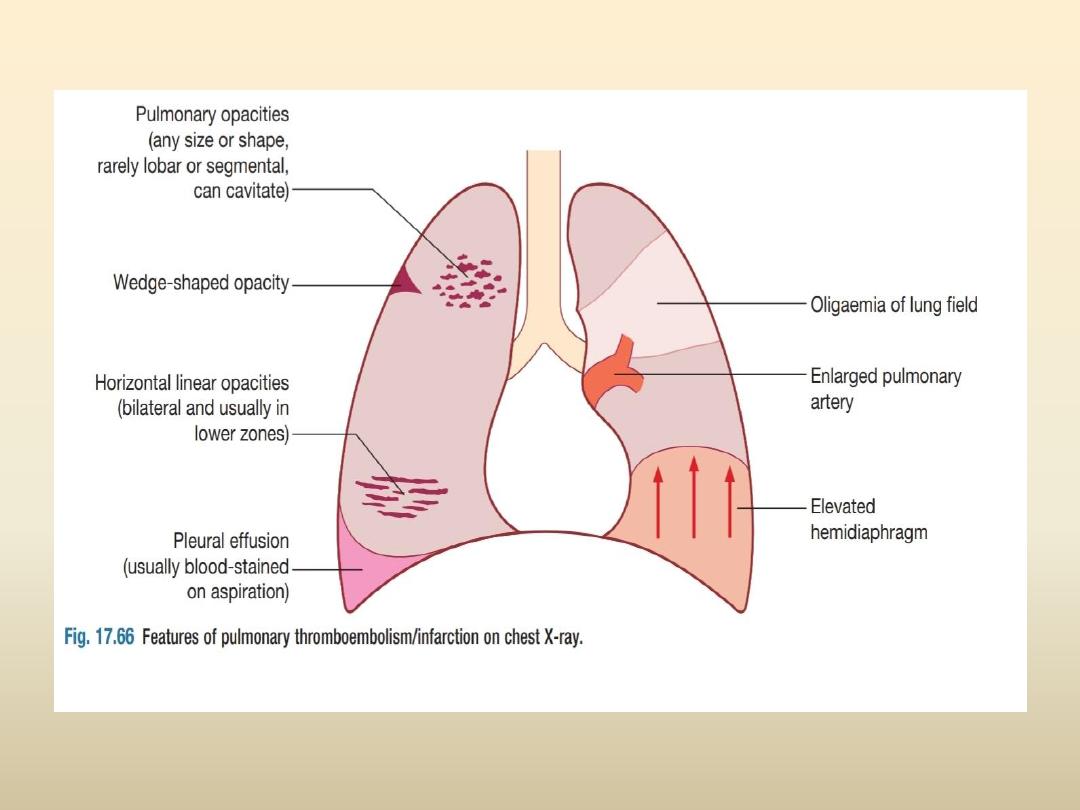
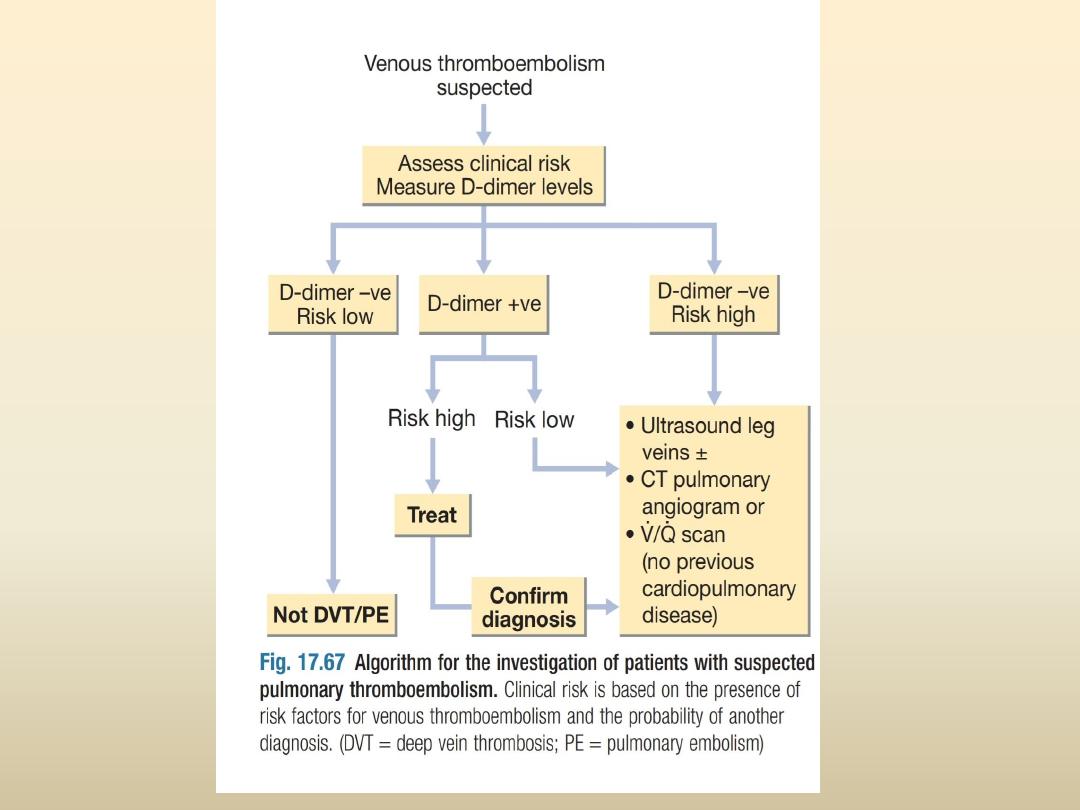
investigations
• Chest X-ray
• Electrocardiogram
• Arterial blood gases
•
D-dimer test,low value
high negative predictive value
• CT pulmonary angiography is the first-line diagnostic
test
• Colour Doppler ultrasound of the leg veins in
suspected case

management
General measures
;
recuscitation
• oxygen should be given to maintain oxygen saturation
above 90%
• Intravenous fluids or plasma expander, in hypotensive
and shock patients
• Opiate to relieve pain (with caution)
Anticoagulants
(eg:-LMWH and warfarin)
Thrombolytic and surgical therapy
in case of cardiogenic
shock
Prophylaxis and long term management

saad mahmood

Acute exacerbation of asthma
• increased symptoms, deterioration in lung
function, and an increase in airway inflammation.
Exacerbations are most commonly precipitated
by viral infections but moulds ,
pollens
(particularly following thunderstorms) and
air
pollution are also implicated
• Most attacks are characterised by a gradual
deterioration over several hours to days but some
appear to occur with little or no warning: so-
called brittle asthma.

presentation

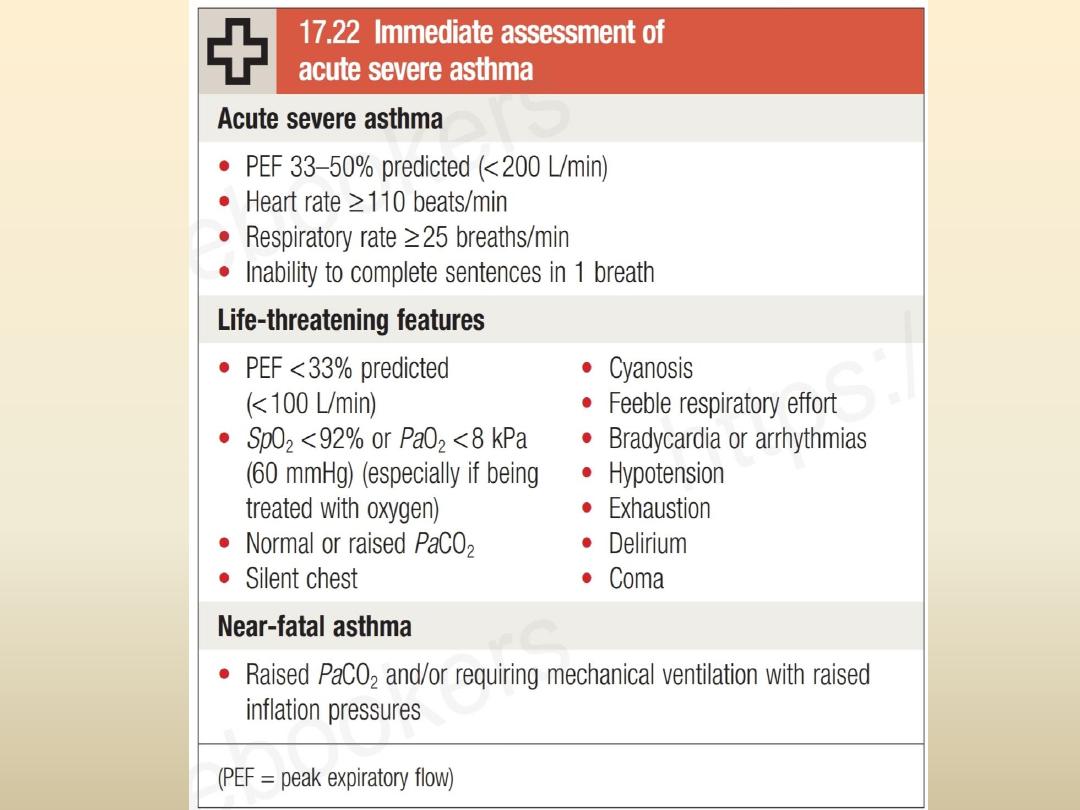
Acute severe asthma
• severe dyspnoea,
• tachypnoea (RR > 25/min),
• tachycardia (PR > 110/min),
• unable to complete a sentence in one breath
• PEF is 33%-50% of predicted (less than 200
L/min).
• PaO
2
(and SpO
2
) is usually normal
• PaCO
2
is low (hyperventilation)

Life threatening asthma
• The patient is unable to speak
• cyanosed, exhausted, and confused
• Bradycardia
• Silent chest and coma may follow.
• PEF is less than 33% predicted (less than 100
L/min)
• SpO
2:
<92% (PaO
2
<60 mmHg).
• PaCO
2
: normal or raised

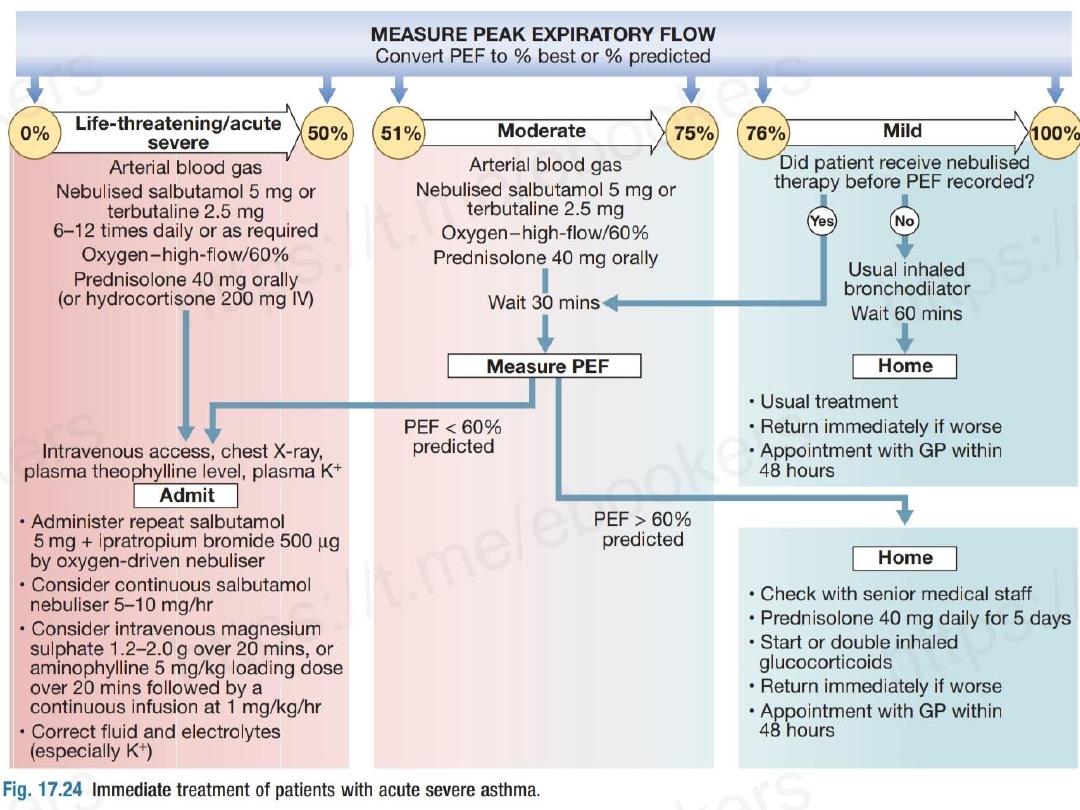
Management
Of acute severe and life threatening asthma

•
Oxygen
. High concentrations (humidified if possible)
to
maintain the oxygen saturation above 92% in adults.
• High dose nebulized bronchodilators
:
2
agonist
(salbutamol 2.5 – 5 mg) repeated within 30 minutes, +/-
nebulized ipratropium bromide
• IV hydrocortisone
200 mg or
oral prednisolone
40 -60
mg.
• Consider IV Magnesium sulphate ,
or
aminophylline
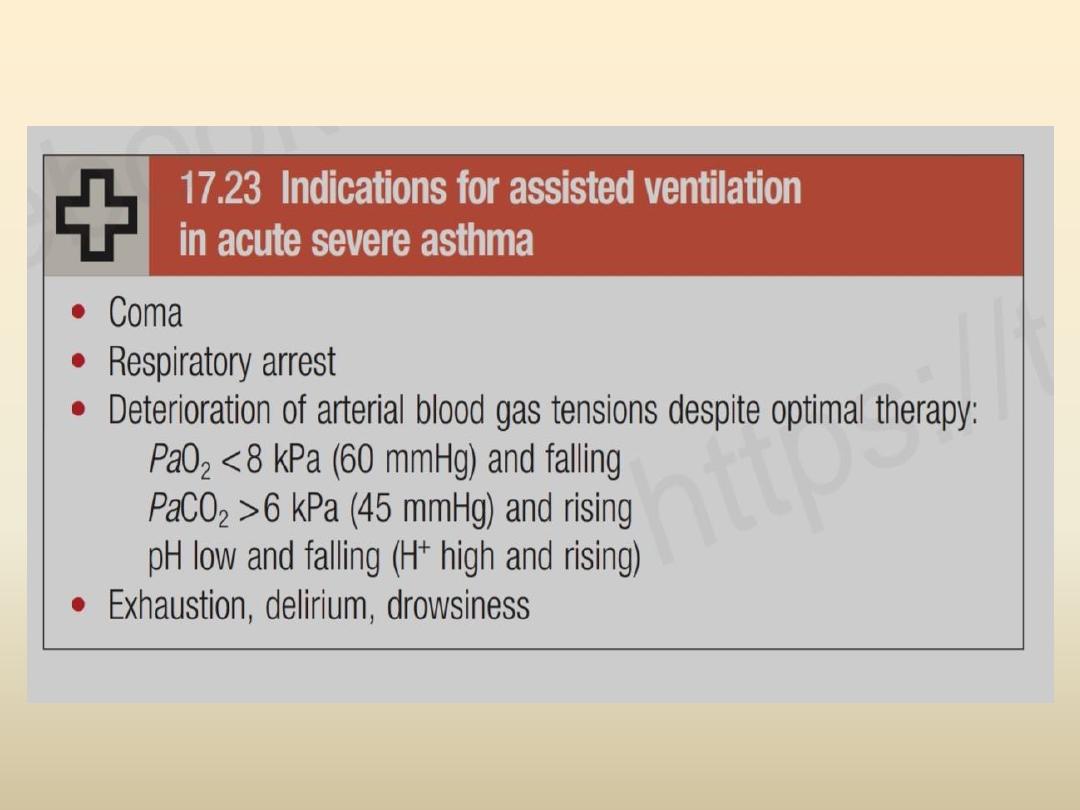
• Ventilatory support
(endotracheal intubation and
mechanical ventilation)
• Short course of oral corticosteroids
should be prescribed
with optimization of his medication and managing any
possible trigger factors after discharge.

Acute exacerbation of COPD

• Exacerbations are a prominent feature of the
natural history of COPD. Exacerbations are
episodes of
increasing
dyspnoea and cough and
change in
the amount
and
character
of sputum.
The frequency of exacerbations increases as the
airway obstruction increases. Exacerbations are
usually triggered by bacterial or
viral
respiratory
infections or
air pollution
. Commonly
encountered bacteria during exacerbations
include
H. influenza
,
Streptococcus
pneumonia
e
and
Moraxella catarrhalis
.

• The presence of
cyanosis
,
oedema
and
altered
level of consciousness
are indications for
hospital admission.

management
In hospital include:-
• Oxygen therapy: Controlled oxygen at 24% or 28%
should be used with the aim of maintaining a
PaO2 of
more than (60 mmHg) (or an
SaO2 of more than 90%).
• Bronchodilators: SABA (salbutamol) combined with
ipratropium bromide are nebulized with oxygen (or by
mechanical nebulizer).
• Corticosteroids: Oral prednisolone 30mg for 10 days.
• Antibiotics: are indicated in the treatment of
exacerbation in most cases. The choice usually include
penicillins or macrolides
• Consider:
• Non-invasive ventilation (NIV): if the patient failed to
respond to the above measures
• Mechanical ventilation is indicated if NIV failed, or if
the patient's consciousness is disturbed or he cannot
clear his secretions
• Additional therapies:
• Peripheral oedema may require diuretic therapy
• Respiratory stimulants like doxapram has been largely
replaced by the use of NIV, but may be useful for
selected patients with low respiratory rate

mustafa hussein

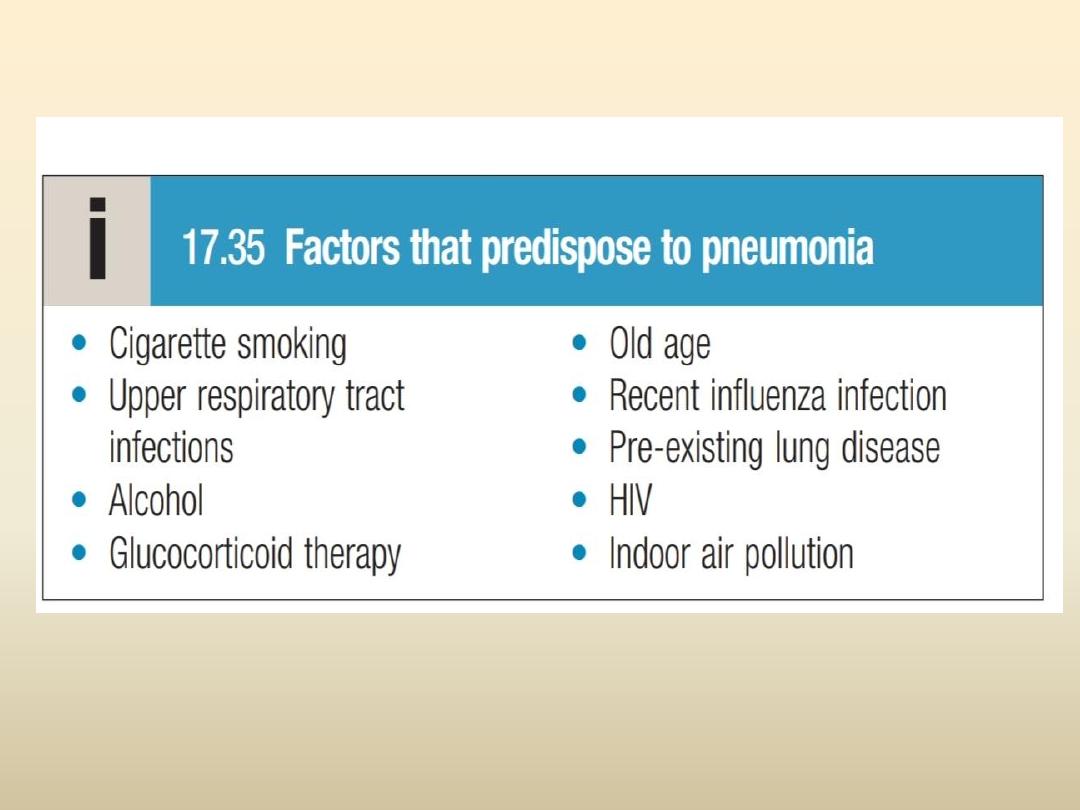
Pneumonia

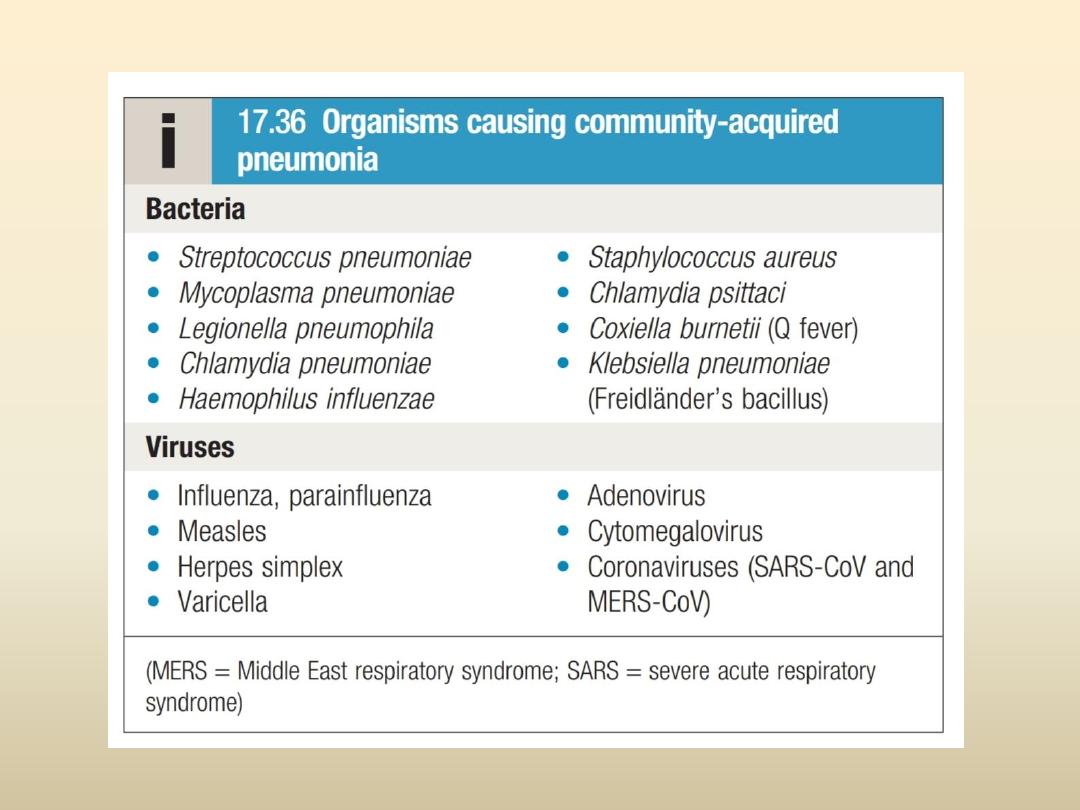
• Pneumonia is as an acute respiratory illness caused by
infection of lung parenchyma associated with recently
developed radiological pulmonary shadowing that may
be
segmental
,
lobar
or
multilobar
. pneumonias are
usually classified as
community-
or
hospital-acquired
,
or those occurring in
immunocompromised
hosts.
‘
Lobar pneumonia
’ is a radiological and pathological
term referring to homogeneous consolidation of one or
more lung lobes, often with associated pleural
inflammation;
bronchopneumonia
refers to more
patchy alveolar consolidation associated with bronchial
and bronchiolar inflammation, often affecting both
lower lobes.

presentation

Systemic features
• , such as fever, rigors, shivering and malaise,
predominate and delirium may be present.
• Loss of appetite and headache
Pulmonary symptoms
• Cough (painful dry then with mucopurulent sputum)
,rust coloured in strep.pneumoniae
• Acute dyspnea
• Occassionally haemoptysis
• Pleuritic chest pain(may be referred to the shoulder or
anterior abdominal wall.
Atypical presentation in young and old patients

• Clinically
;
patient is
febrile ,with tachycardia ,
tachypnea with use of accessory muscles
• Cyanosis in severe cases
• Chest examination
:Dullness on percussion on
affected side or stony dull if pleural effusion present
• Auscultation : bronchial breathing , whispering
pectoriloquy ,Crackles ,vocal resonance ,friction rub
• In Elderly ,confusion
• In severely ill patient septic shock or organ failure
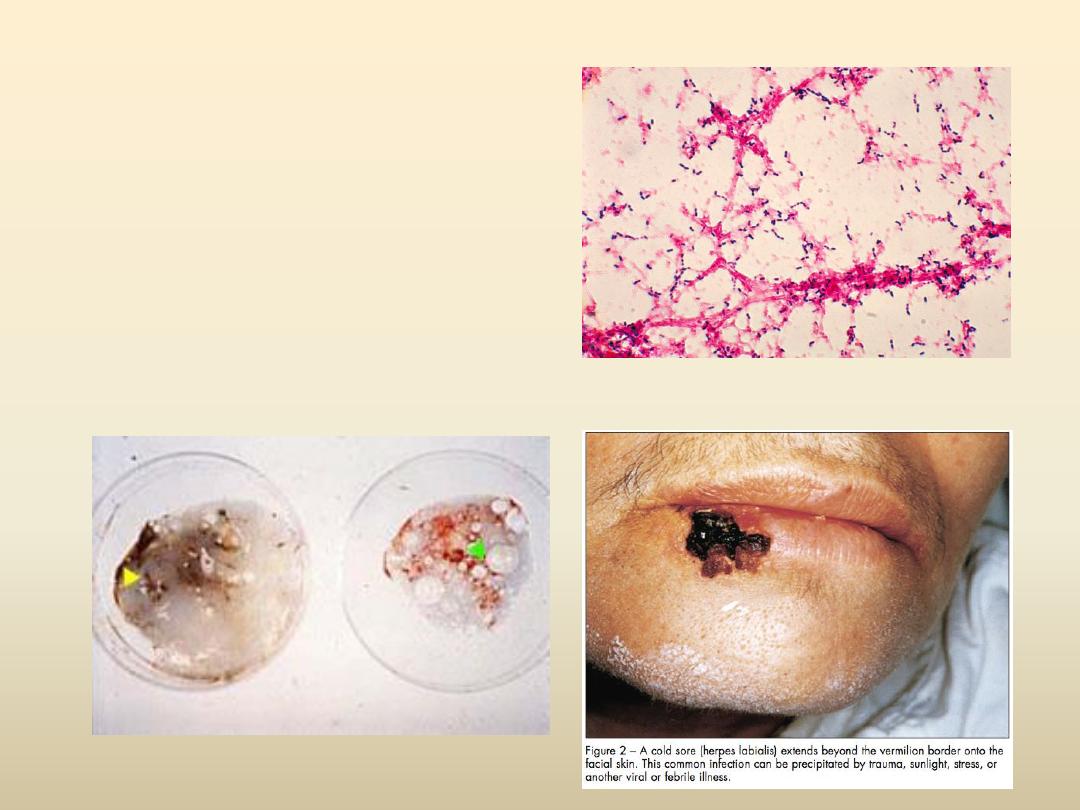
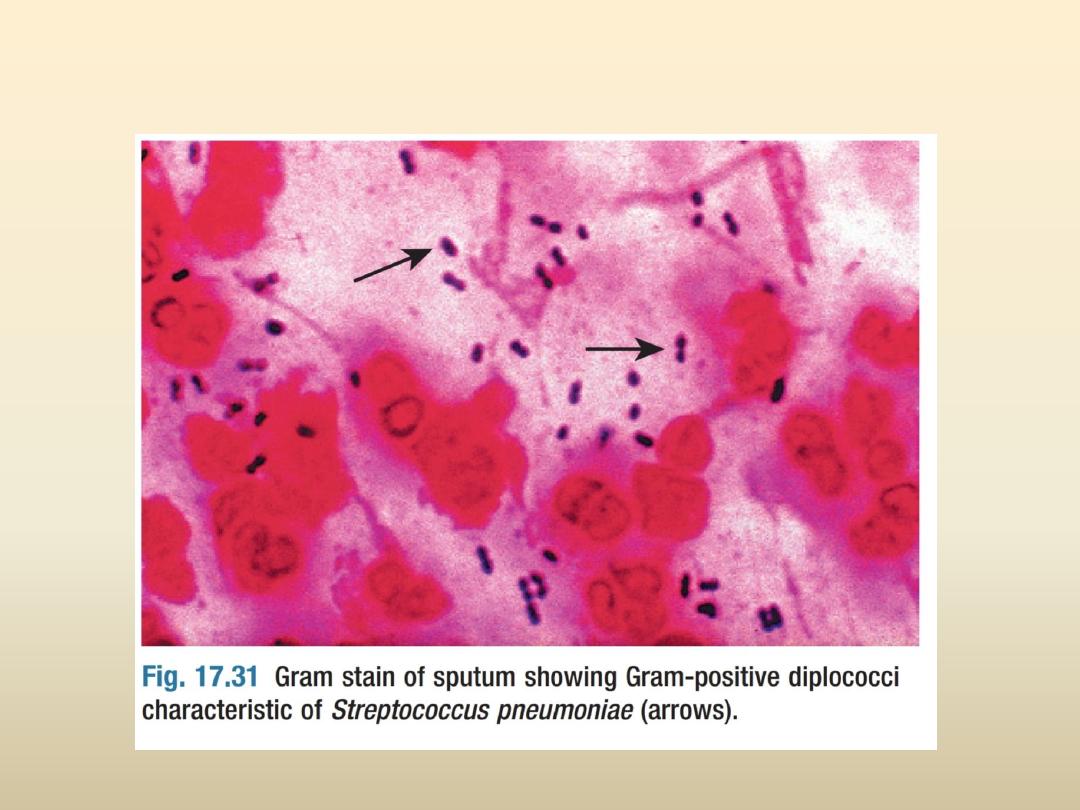
• Strep.pneumoniae
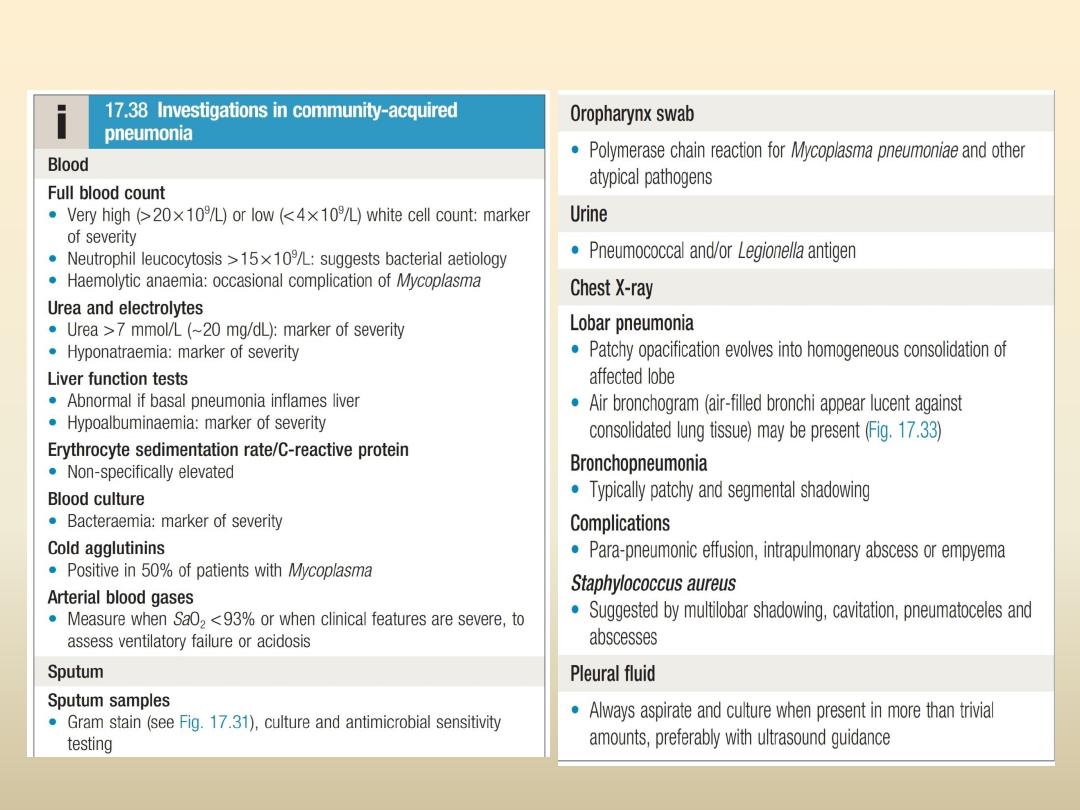
investigations
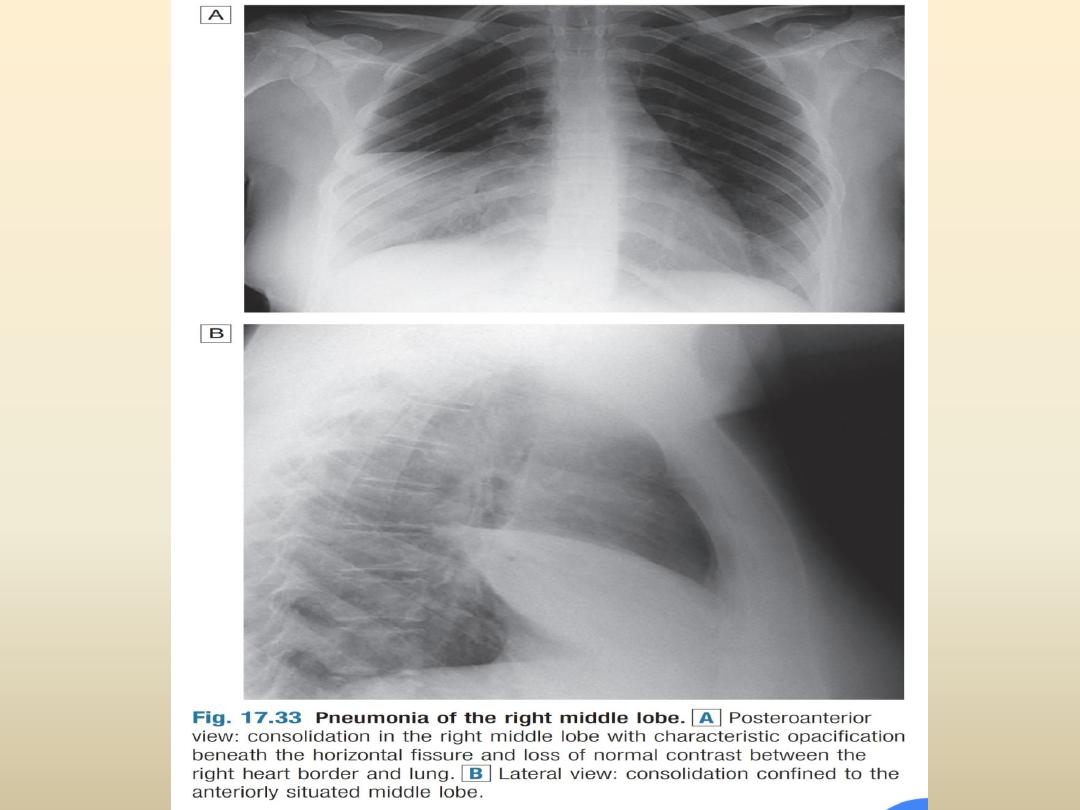

• Lobar pneumonia:
homogenous
consolidation of
one or more lung
lobes, often with
associated pleural
effusion

• Bronchopneumonia:
patchy alveolar
consolidation
associated with
bronchial
inflammation, often
affecting lower
lobes.
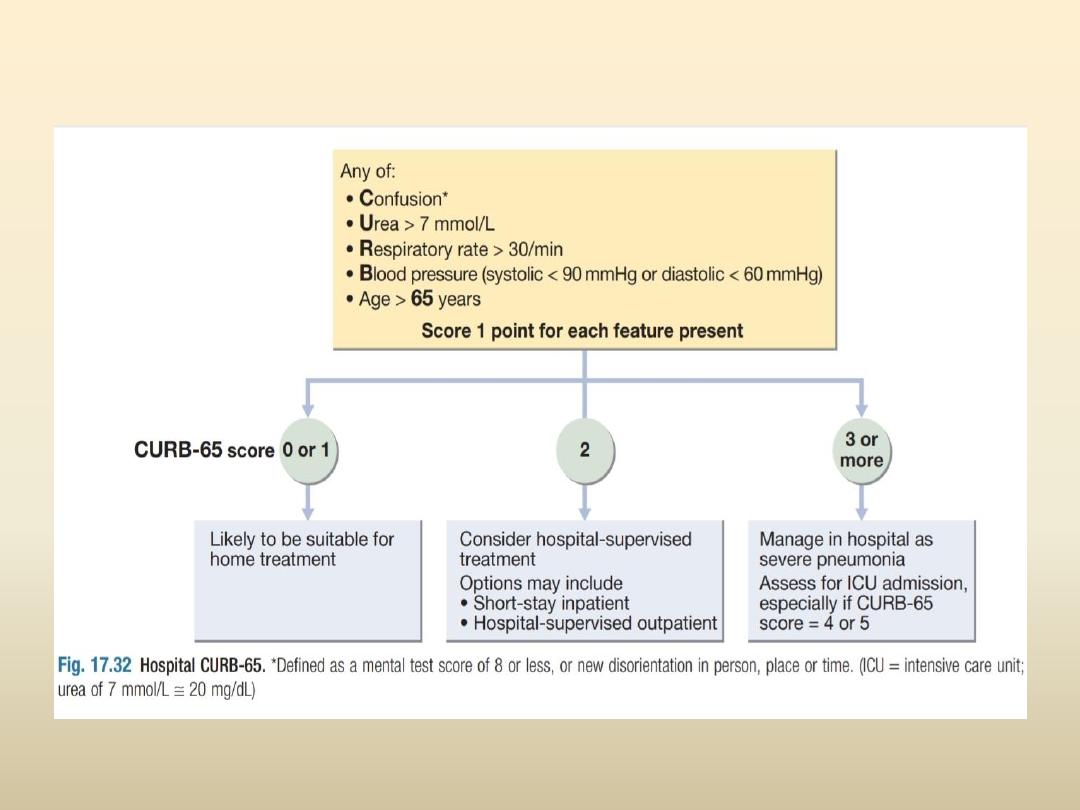
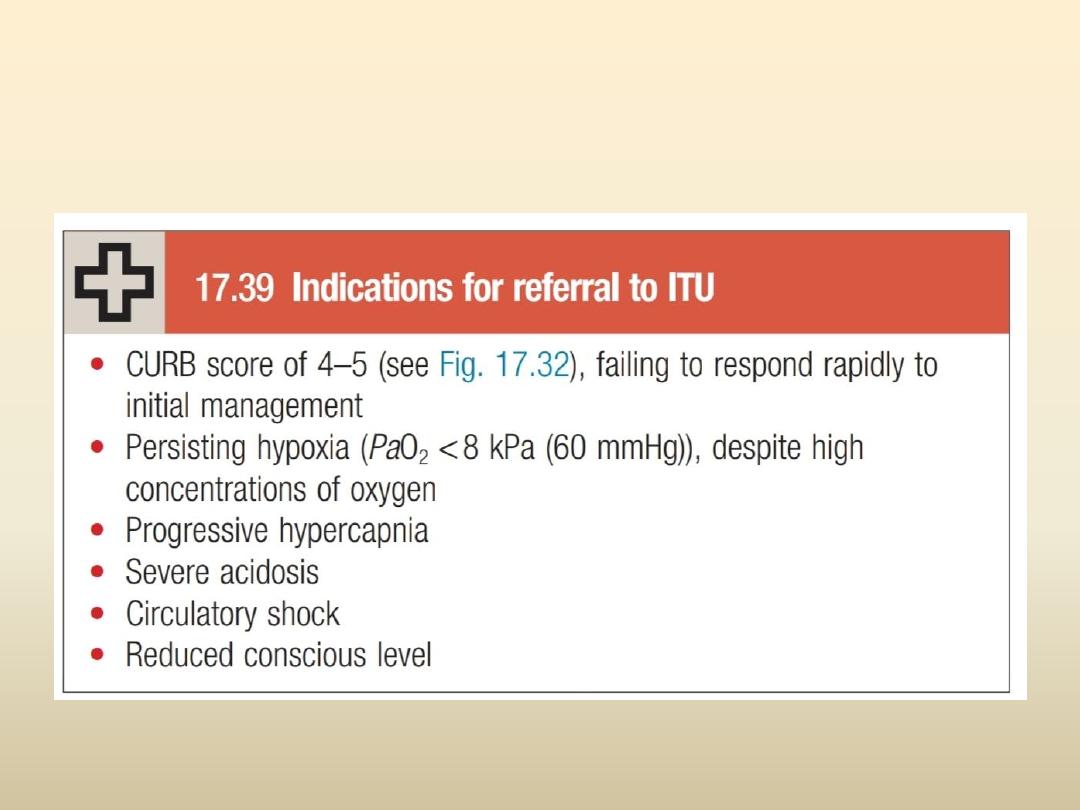

management
• Oxygen therapy ; high flow , maintain PaO2
around 60 mmHg (or SpO2 at 92%)
• Mechanical ventilation if remain hypoxic despite
oxygen therapy
• Fluid balance ; oral fluid ,or IV fluid in case of
vomiting or severely ill patient, vasopressors if
septic shock
• Antibiotic therapy ;
Inpatients:
• A respiratory quinolone (oral or IV) (OR)
• A β-lactam (co-amoxiclav 1-2 gm three time daily
IV or cefotaxime 1-2gm IV three time daily or
ceftriaxone 1-2 gm IV daily) PLUS, a macrolide
(oral or IV)
(If
Staphylococcus aureus
is suspected, add
vancomycin or linezolid).

• Pleuritic pain is treated with paracetamol or
NSAID.
• Physiotherapy to assisst expectoration.

russel mikdad

Pneumothorax

• Pneumothorax is the presence of air in the
pleural space, which can either occur
spontaneously, or result from iatrogenic injury
or trauma to the lung or chest wall
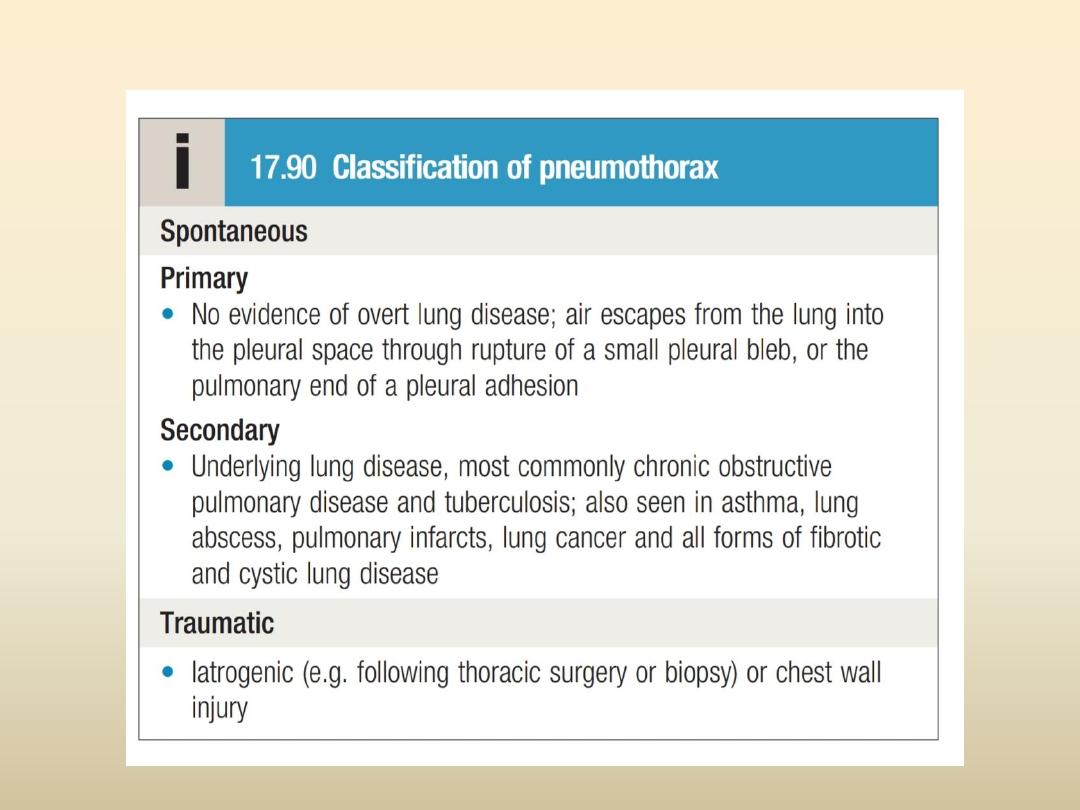
classification
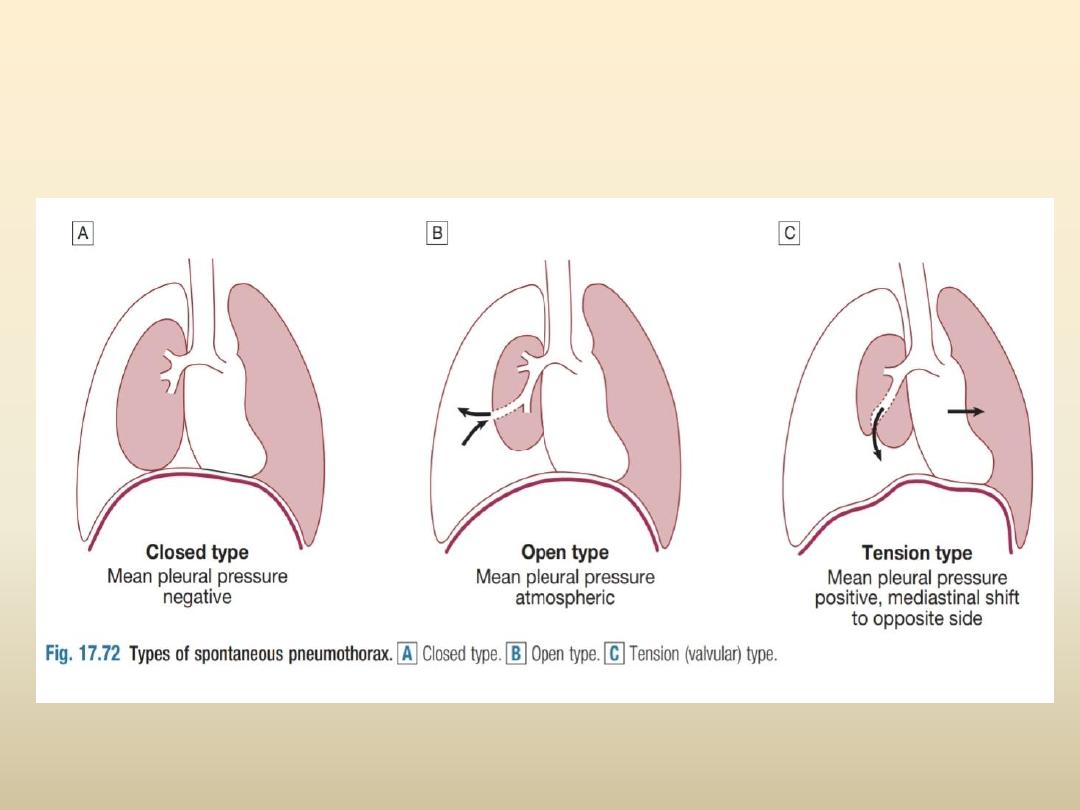
Types of spontaneous pneumothorax

presentation

• sudden-onset unilateral pleuritic chest pain or
breathlessness.
• In patient with unlderlying lung disease
breathlessness are severe
• Small pneumotharax : normal physical findings
• Larger one (> 15% of the hemithorax) decreased
or absent breath sounds
• The combination of absent breath sounds and a
resonant percussion note is diagnostic of
pneumothorax.

• in
tension pneumothorax
there is rapidly
progressive breathlessness associated with a
marked tachycardia, hypotension, cyanosis
and tracheal displacement away from the side
of the silent hemithorax.

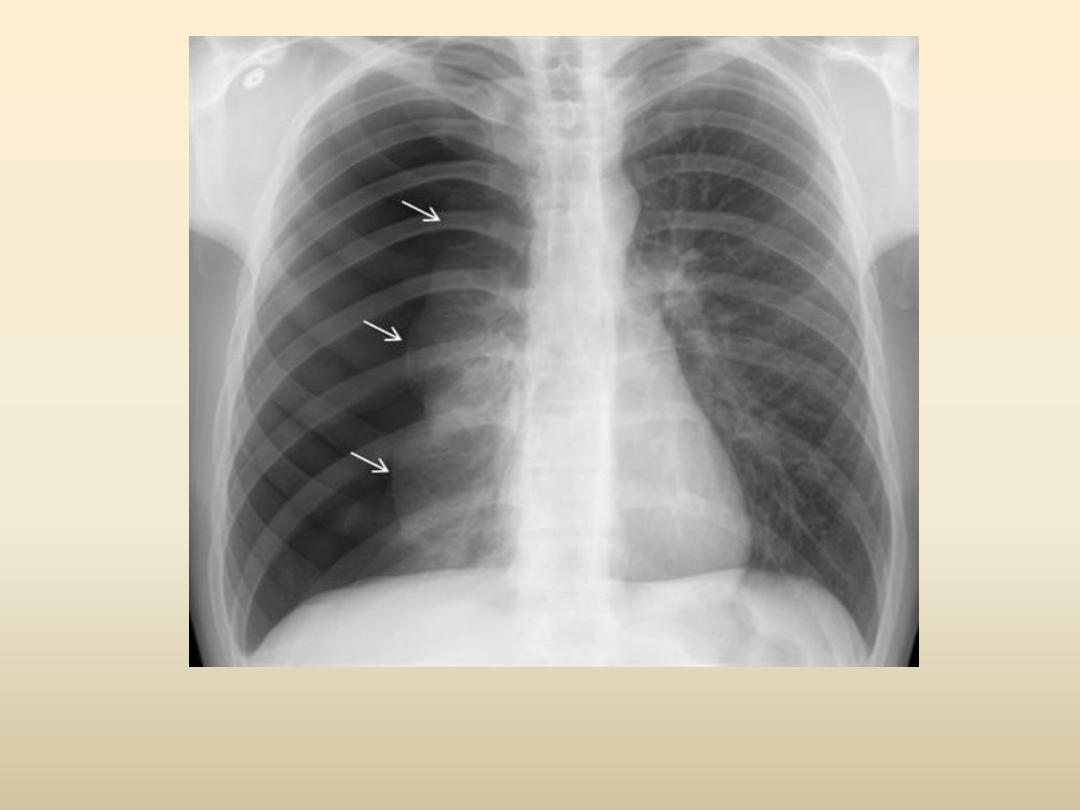
investigations
• chest X-ray shows the sharply defined edge of
the deflate lung with complete translucency
(no lung markings) between this and the chest
wall,also show degree of shift and underlying
disease
• CT scan in difficult cases
p

management
• a moderate or large spontaneous primary
pneumothorax, by
percutaneous needle aspiration
• Chest tube in patient with underlying lung diseases.
• tension pneumothorax, immediate release of the
positive pressure by
insertion of a blunt cannula
,allowing time to prepare chest tube
• Supplemental Oxygen
may speed the resolution
• Advise to Avoid flying
• Recurrent of spontaneous may need surgical
intervention (
Pleurodesis
)