Chronic liver Diseases
Supervised By
:
Dr. Ismael dawood saeed
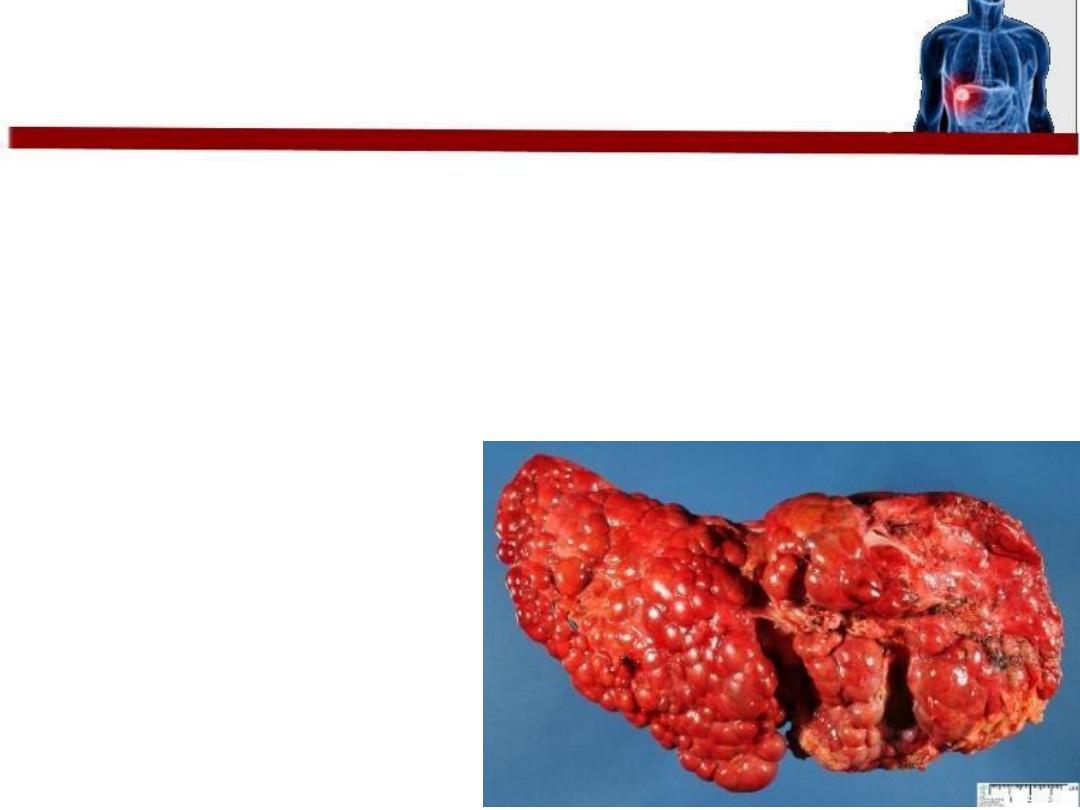
What is Cirrhosis???
• Cell necrosis
• Fibrosis
• Nodules formation
• Loss of normal architecture
CAUSES OF CIRRHOSIS
???
1. Alcohol
2. Chronic viral hepatitis Bor C
3. Non-alcoholic fatty liver disease
4. Immune
1.
Primary sclerosing cholangitis
2.
Autoimmune liver disease
5. Biliary
1.
Primary biliary cirrhosis
2.
Cystic fibrosis
6
.
Genetic
1
.
2
.
3
.
Haemochromatosis
α
1
-antitrypsin deficiency
Wilson's disease
7. Cryptogenic (unknown)
8. Drugs
amiodarone, methyldopa, methotrexate
The Approach to a patient with cirrhosis
• History
• Physical examination
• Investigations
• Management & follow-up
History of the present illness and review of other systems
• asymptomatic !!! Or non-specific symptoms : weakness,
fatigue, muscle cramps, weight loss, anorexia, nausea,
vomiting and upper abdominal discomfort “
Compensated
”
• Symptoms of
“decompensation”
: abdominal distension,
coffee-ground vomiting and/or black tarry stool
“melaena”,bleeding from the nose, menorrhagia, altered
mental status, lower extremity swelling, jaundice, and
pruritus.
• Other less common symptoms : SOB
Past medical history
•
Jaundice (very important!!!)
•
chronic liver disease.
•
metabolic syndrome (diabetes, dyslipidaemia, obesity, HTN)
•
autoimmune disorders.
•
blood transfusion
Past surgical history
•
Previous operations and dental procedures
Drug history
• Medications with hepatotoxic effects.
• Over-the-counter medications, vitamins, and herbal and dietary
supplementation
.

Social history
• alcohol history
• intravenous drug use
• unprotected intercourse
• tattoos.
• Sharing of toothbrushes
Family history
• Haemochromatosis.
• Wilson's disease.
• Alpha-1 antitrypsin deficiency.

General examination
Head and neck
• Spider naevi
• Yellowish discoloration of sclerae
• Skin pigmentation
• Parotid gland swelling
• Bruising
• Epistaxis
• Bluish discoloration of lips
and mucous membrane
General examination
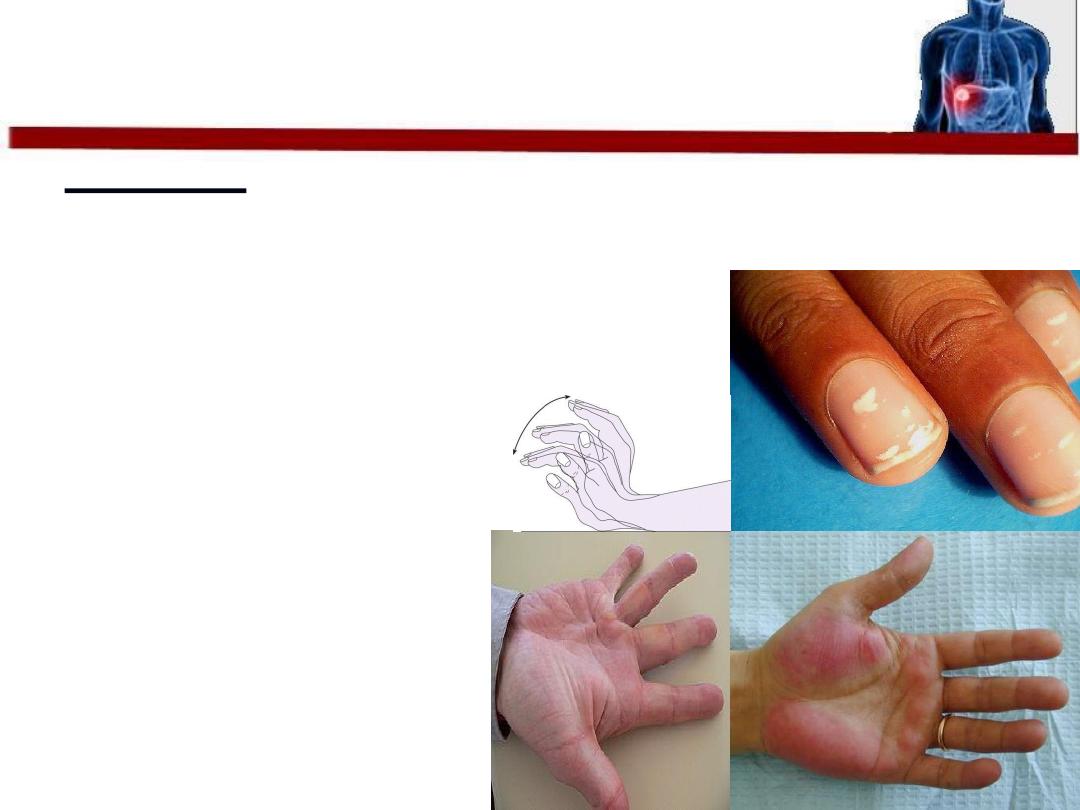
Upper limbs
• Palmar erythema
• Leukonychia (white nails)
• Finger clubbing
• Flapping tremor
• Spider naevi
• Bruising
• Dupuytren contracture

General examination
Limbs
Lower
• Bilateral pitting edema
• Loss of hair
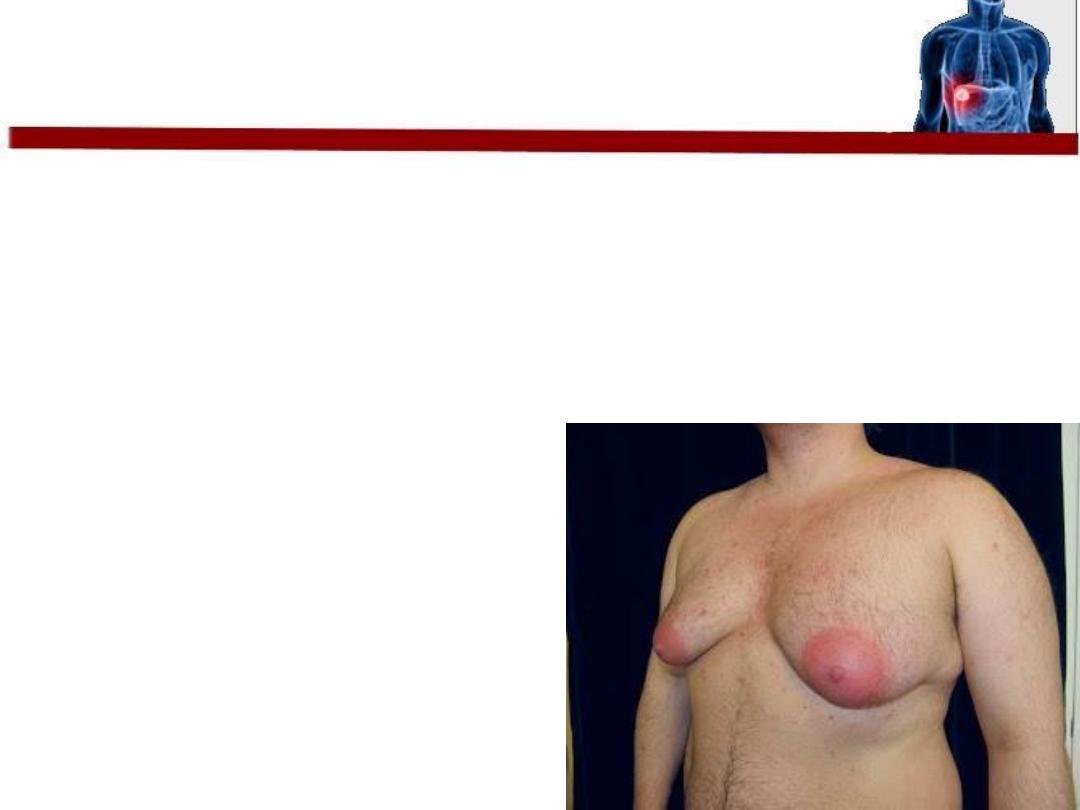
Chest examination
• Gynaecomastia and loss of secondary sexual hair in
men
• Breast atrophy in women.
• Spider naevi
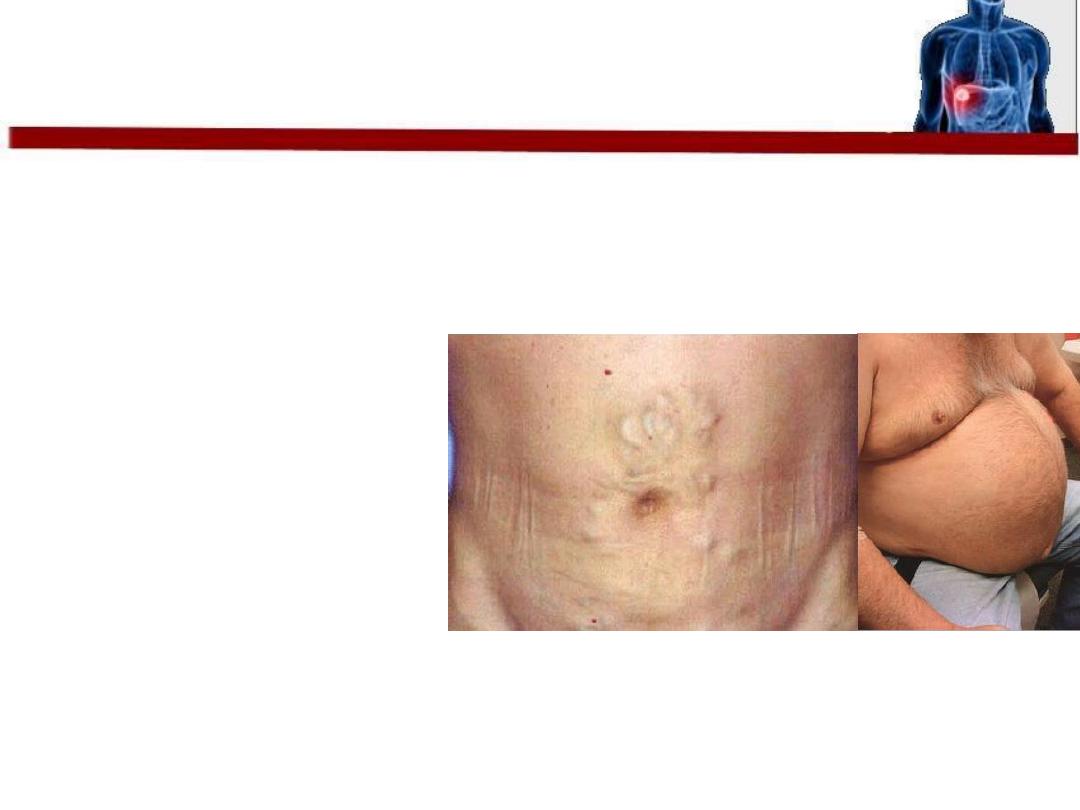
Abdominal examination
• Generalized Abdominal distension (especially in the flanks) ,shifting
dullness , transmitted thrill
• Caput Medusae
• Hepatomegaly
???
• Splenomegaly
• Bruising
• Loss of secondary sexual hair and testicular atrophy in men.

•Blood tests :
Full blood count , B suger ,B.uria, S.creatinin ,S. Electrolytes.
•Liver Function Test :ALT, AST, ALP, S.Bilirubine ,S.Albumin , PT
• U\S of liver ,Biliary Passage ,abdomen
•Liver Biopsy Gold stander
•Investigation of the Cause :viral study ,Haemochromayosis ,
•Investigation of complication : Ascites ,portal hypertension,hepatic
encephalopathy , renal failure, liver cancer
.

1
Lifestlyle and diet modifications (avoid alcohol,
avoid hepatotoxic drugs, limit salt ….etc).
2
treat underlying cause
3Treat complications ( ascites, esophageal varices ,
hepatic encephalopathy ….etc).
4regular screening for esophageal varices and
hepatocellular carcinoma
5Liver transplantation
???
Liver transplantation
Indicted in :
Sign of liver failure
First episode of bacterial pertonitis
Diuretic resistant Ascites
Recurrent variceal bleeding
Liver cancer less than 5 cm
persistent hepatic encephalopathy
Liver transplantation
contraindication
sepsis
Extrahepatic malignancy
Active Alcoholic or substance misuse
Cardiopulmonary dysfunction
• Portal hypertension develops when there is
elevation of portal pressure greater than 12
mmHg, while normal portal pressure is 5 –
10mmHg.
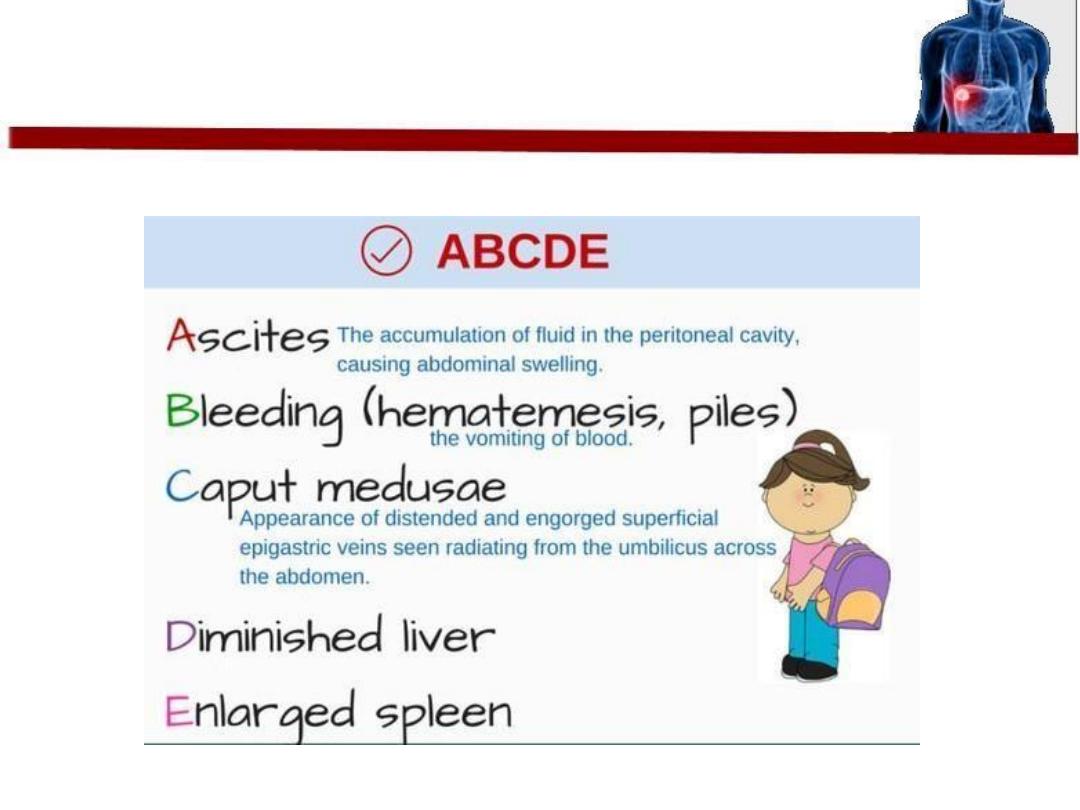
Portal hypertension
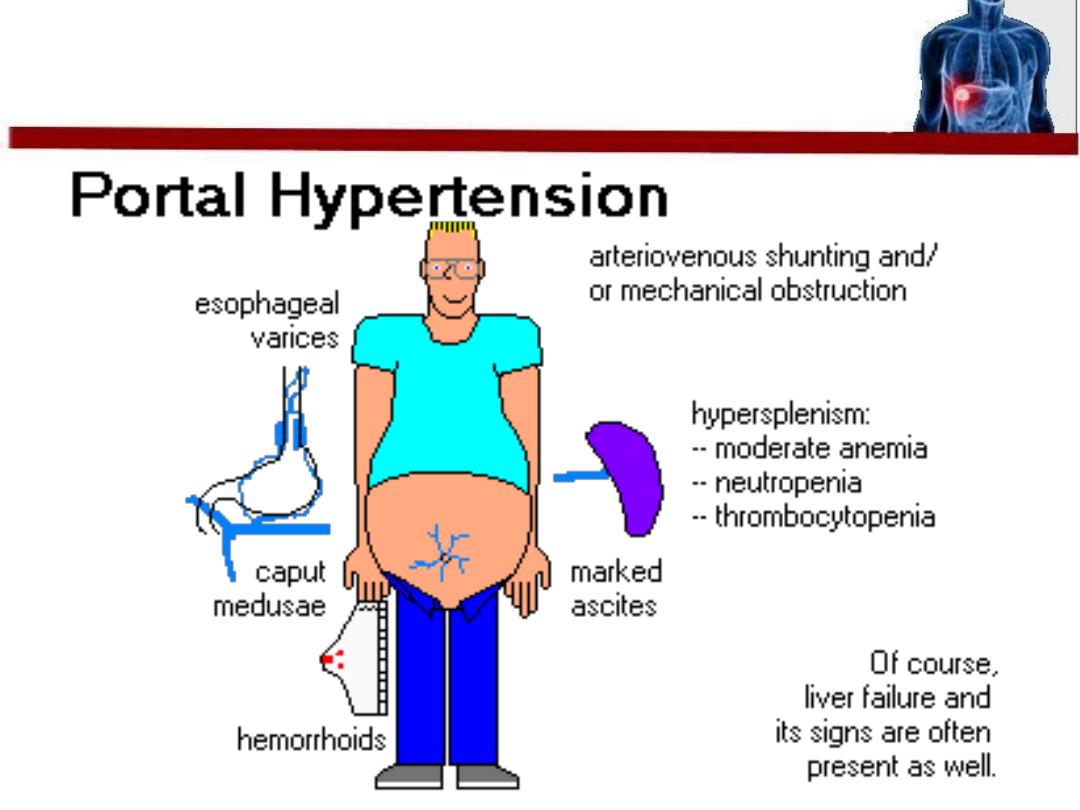
Features
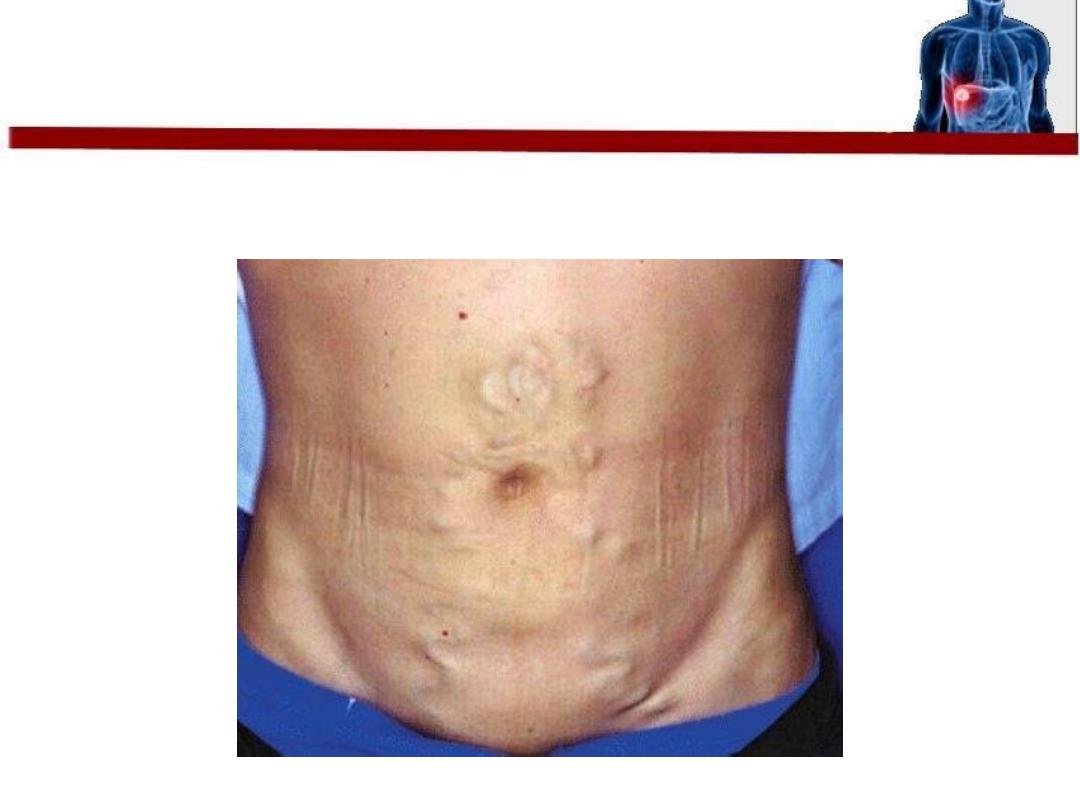
In abdominal examination you may see
this
• Clinical
• CBC : pancytopenia
• endoscopy.
• Abdominal imaging, either by CT or MRI can
be helpful in demonstrating a nodular liver
and in finding changes of portal hypertension
with intraabdominal collateral circulation.
Diagnosis
• Treat the cause !
• Gastroesophageal variceal hemorrhage is the
most dramatic and lethal complication of
portal hypertension; therefore, Medical care
includes emergent treatment, primary and
secondary prophylaxis, and surgical
intervention
• Pharmacologic therapy Includes the use of
beta-blockers, most commonly propranolol
and nadolol
Treatment
• Endoscopic procedures such as sclerotherapy
and variceal ligation can be used to prevent
the recurrence of variceal hemorrhage.
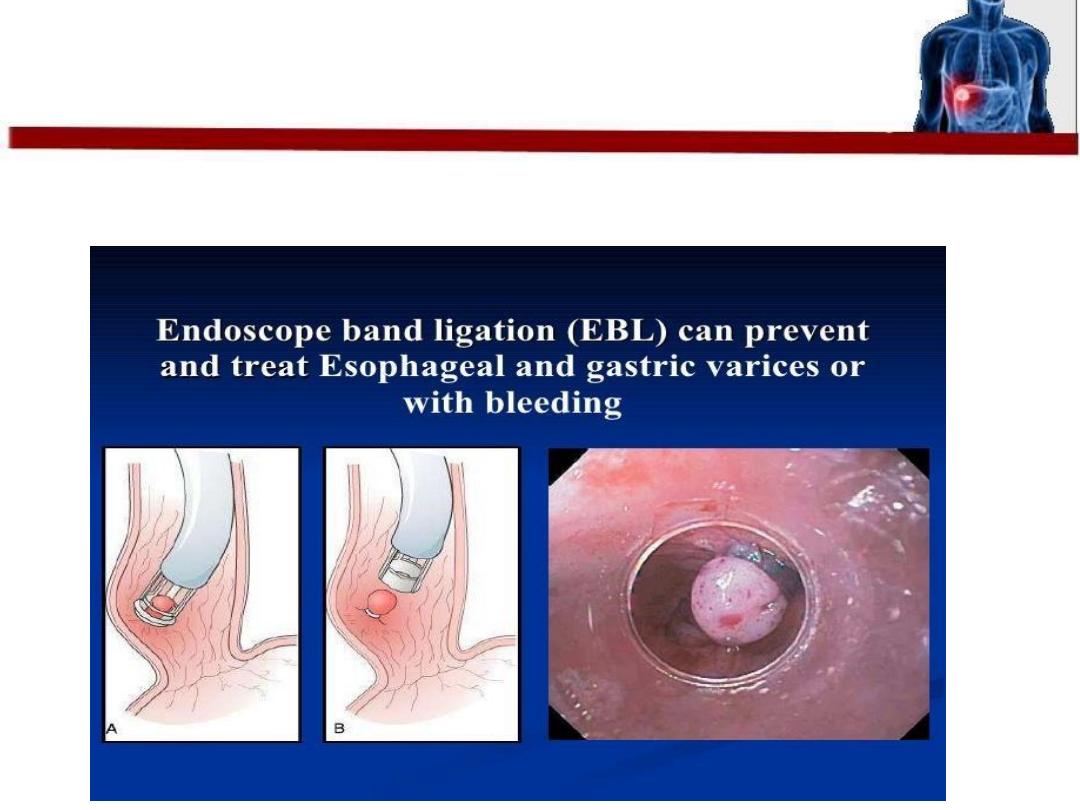
Complications of this procedure ?

Now what if the patent presented with
Ascites
?
Ascites is usually diagnosed clinically or by ultrasound
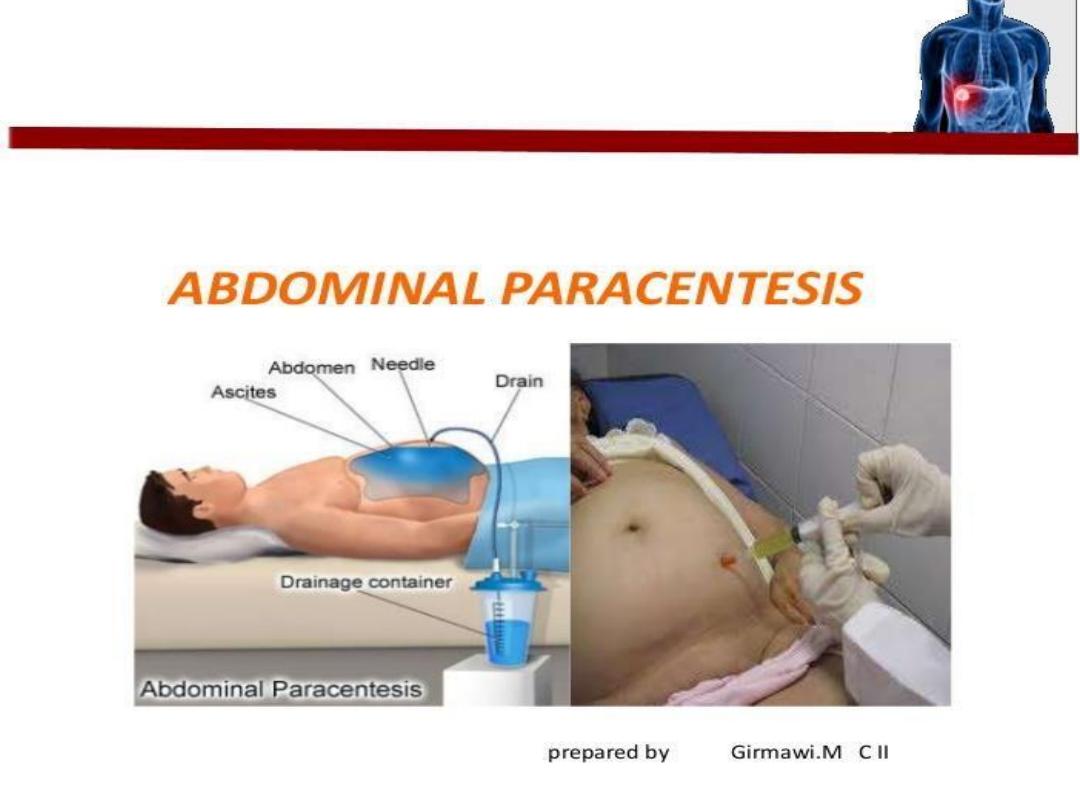
New development of ascites in a cirrhotic patient does not
routinely require paracentesis only if :
1 General condition deteriorates.
2 In presence of unexplained fever, abdominal pain,
encephalopathy.
3 Admission to hospital for any cause (SBP.)
4 Laboratory investigations indicating infection:
- Leucocytosis
- Acidosis
- Worsening of renal functions
Paracentesis
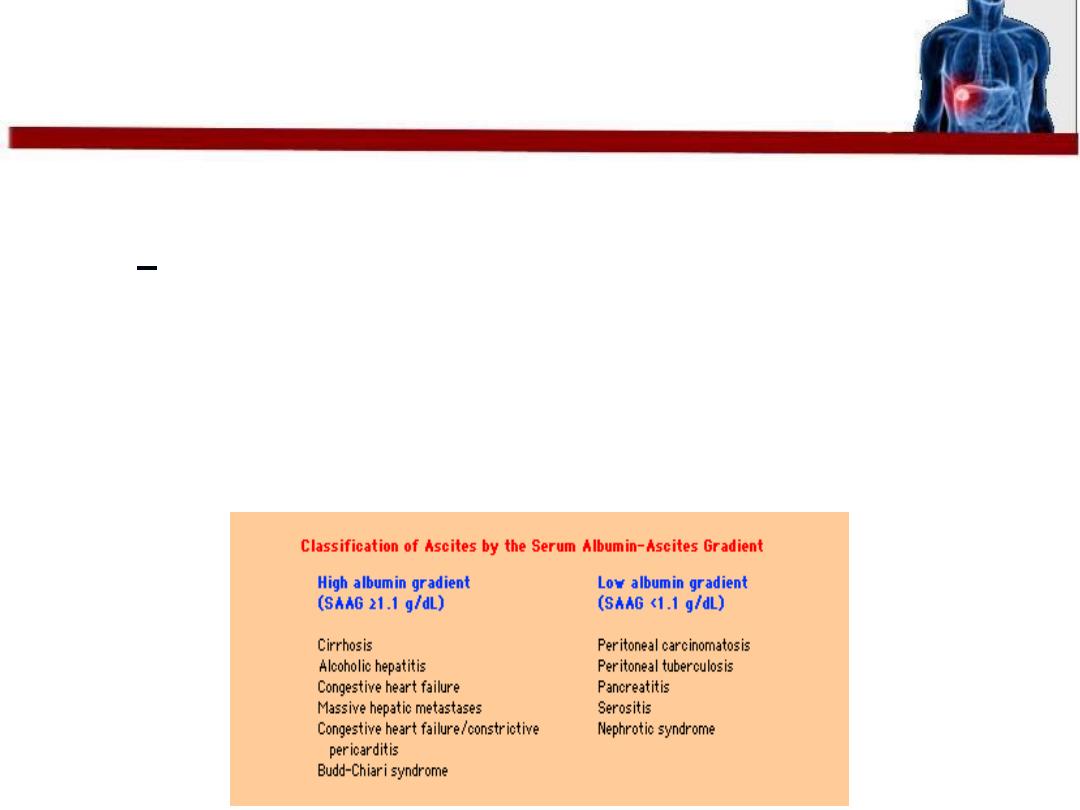
• Serum-ascites albumin gradient
(SAAG) = serum albumin - ascitic fluid albumin.
If > 1.1 g/dL, the patient has PH-related ascites.
If < 1.1 g/dL (about 97% accurate), the patient does
not have PH-related ascites.
The SAAG does not need to be repeated after the initial
measurement.
•
Bed Rest
Not recommended
!
• Bed rest promote muscle atrophy and other
complications and extends hospital stay
Treatment
• Restriction of dietary Na to 80 mmol/day (no
adding table salt.)
• If there is severe ascites we should restrict Na
to (40 mmol/day) and should avoid drugs
cause salt retention like
NSAIDs
.
• Restriction of water to about 0.5-1 L/day
which is important especially when Na fall
below 125 mmol/L (because dilutional
hyponatremia may occur.)
• Diuretic treatment: the best one is
spironolacton in (100-400mg/day). Side
effects are painful gynecomastia &
hyperkalemia
• Paracenthesis (aspiration of fluid LVP): 3-4 L
can be taken over 1-2 hours specially in
emergency to relieve the patient distress
• common and severe complication of ascites
• occurs in the absence of a visceral perforation and in
the absence of an intraabdominal inflammatory focus
• Its usually monomicrobial infection the presence of
more microorganisms in the culture (>1), must raise
the suspicion of secondary peritonitis
• The most common organisms are
Escherichia coli
and
other gut bacteria; however, grampositive bacteria,
including
Streptococcus viridans, Staphylococcus
aureus
, and
Enterococcus
sp., can also be found.
Spontaneous Bacterial Perotonitis
• Approximately 10% of the patients with SBP
are asymptomatic
• usually non specific symptoms
• The most frequently encountered symptoms
and signs are fever (69%), abdominal pain
(59%), signs of hepatic encephalopathy,
abdominal tenderness (very rare), diarrhoea,
ileus, shock and hypothermia.
Features
• The SBP diagnosis is established by analysis of
the ascitic fluid obtained at paracentesis.
• Paracentesis should be avoided only in case of
a suspicion of fibrinolysis or DIC
Diagnosis
• From the ascitic fluid a series of tests can be
performed, mandatory even in the case of a
therapeutic paracentesis
leucocyte count , serum and ascitic fluid
albumin levels
• SBP is suspected when the PMN number in
the ascitic fluid is over 250/mm 3
.
• .After paracentesis, the ascitic fluid should be
inoculated immediately (at the patient‘s
bedside) into blood-culture bottles (10ml in
each bottle). Using these recipients instead of
the usual ones increases the diagnosis rate of
ascites with neutrophils from 50 to 80%
.
• Immediate use of broad spectrum antibiotic
such as Cefotaxim
Treatment
There are three categories of cirrhotic patients
which are more at risk of developing SBP:
patients with digestive hemorrhage;
patients with ascitic fluid protein level less than
1g
patients who survived a prior SBP episode.
Prevention
• For those who have low protein level >>> give
Norfloxacin is administrated during
hospitalization
• Patients with digestive hemorrage 20% of
them have SBP at admission and 30-40% will
develop an infection during hospitalization.
These patients will receive 800 mg/ day
Norfloxacin through the nasogastric tube for 7
days
• In patients who survive an episode of SBP, a
long term prophylactic treatment (for
preventing recurrence) with Norfloxacin 400
mg/day will be administered.
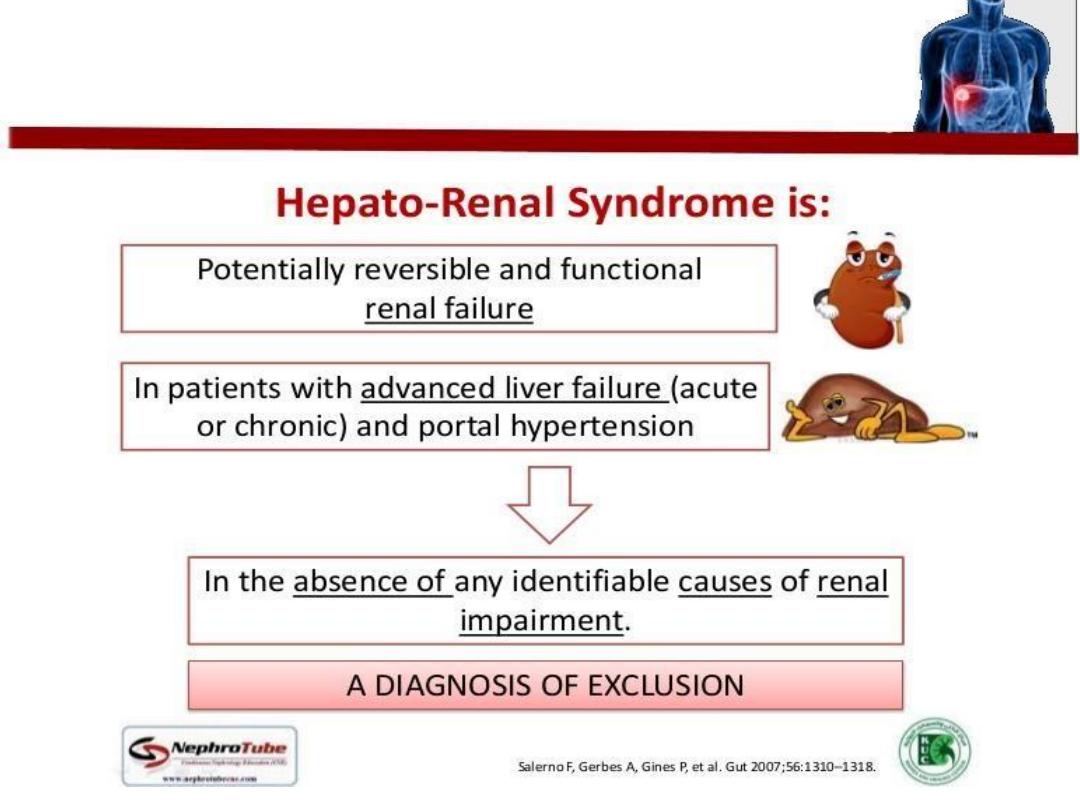
Hepatorenal Syndrome
There are two
types
• Type 1 hepatorenal syndrome is characterized by
progressive oliguria, a rapid rise of the serum
creatinine and a very poor prognosis (without
treatment, median survival is less than 1
month.)
• There is usually no proteinuria, a urine sodium
excretion of less than 10 mmol/day
• Type 2 hepatorenal
s
yndrome usually occurs
in patients with refractory ascites, is
characterised by a moderate and stable
increase in serum creatinine, and has a better
prognosis.
• Tarlipressin
• Live transplantation is the treatment of choice
even after improvement in renal fuction since
prognosis is soo poor
Treatment
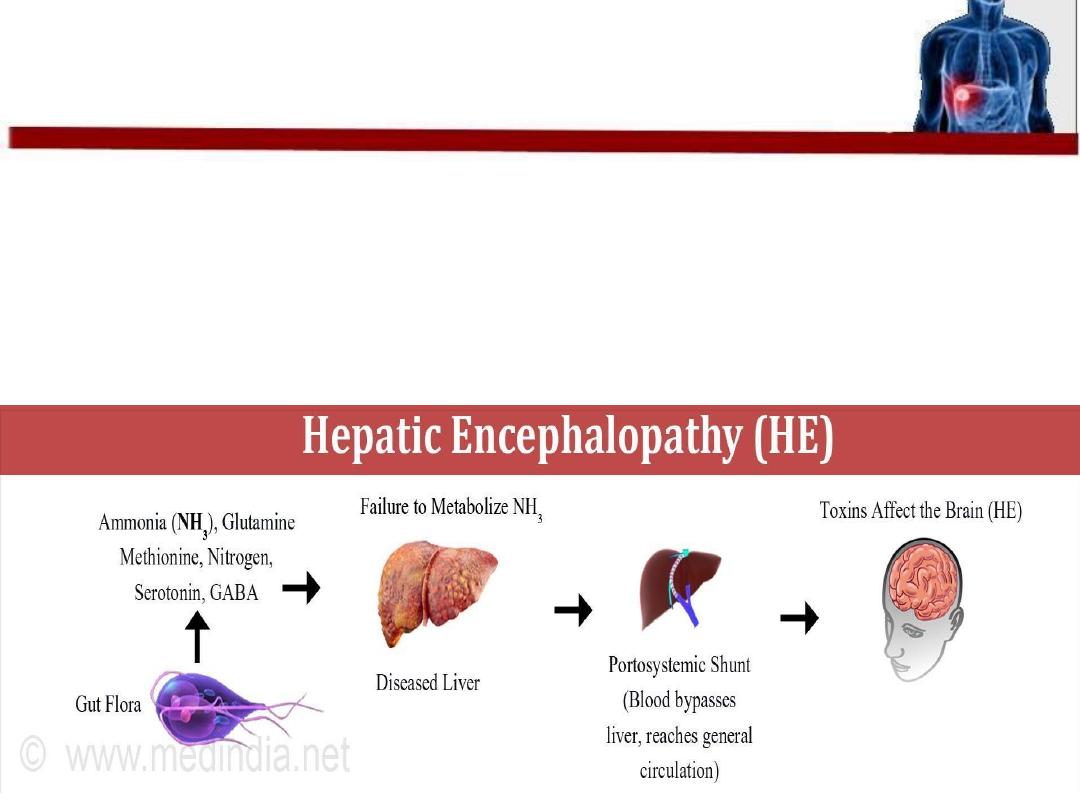
• alteration in mental status and cognitive
function
• occurring in the presence of liver failure
Hepatic encephalopathy
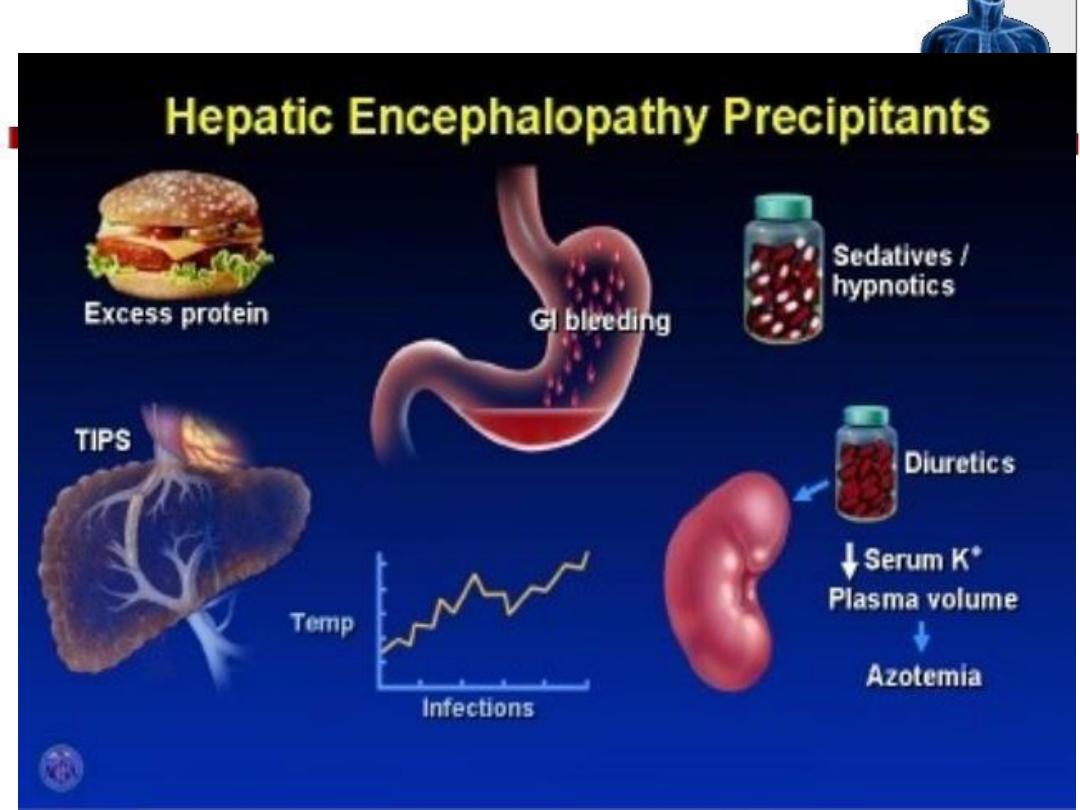
-
HEPATICUS
-
• H
aemorrhage
• E
lectrolye imbalance
• P
rotein
• A
lcohol/ Analgesics
• T
rauma
• I
nfxn
• C
onstipation
• U
raemia
• S
urgery (post systemic shunt)
Triggers
• Features of alterned mental state , personality
• Emotions and consciousness
• Convusion sometimes occur
In Examination
Fetor hepaticus , sweet musty breath odor
Asterixis
Hyperreflexia and bilateral planter response
Features
• Lactuloses: The goal of lactulose therapy is to
promote 2–3 soft stools per day.
• Antibiotics
:
Drugs like neomycin
• Change diet habit
• Skip
alcohol
: Even a little bit can be risky
• Stop some medications
Treatment
