BLEEDING TENDENCY
Dr. Mohammad Harith Al- saaty
Bleeding can occur after surgery or trauma , pathological
bleeding occur when structurally abnormal vessels rupture
or when a vessel is breached in the presence of a defect in
hemostasis , this may be due to
1.Platelets deficiency
2. Platelets dysfunction
3. Coagulation defects.
Clinical assessment :
.1
History :
a. Site of bleeding : bleeding into the muscles and joints , along
with retroperitoneal & intracranial hemorrhage indicates a likely
defect in coagulation factor .
Purpura , prolonged bleeding from superficial cuts , epistaxis , or
menorrhagia is more likely to be due to thrombocytopenia ,
platelets dysfunction or von willebrand disease .
b. Duration of history : since childhood ? , recent onset ?
c. Precipitating factors : if there is trauma or occur spontaneously.
Bleeding that occur spontaneously indicate a more severe defect .
d. Surgery : ask about operations , dental extraction , tonsillectomy and
circumcision .
Immediate post-surgical bleeding suggest defective platelet plug
formation and primary hemostasis , delayed hemorrhage is more
suggestive of coagulation defect
e. Family history :
It is important to ask about family history , because it may be positive in
patient with inherited disorders , but keep in mind that the absence of
affected relatives does not exclude a hereditary bleeding disorders (
one third of cases of hemophilia arise in individuals without family hx) ,
it is also important to ask about consanguineous marriage because
autosomal recessive disorders are common in those populations .
f. Drug history :
Many drugs can cause bleeding like antiplatelets ( aspirin ,
clopidogrel ..) , anticoagulants ( heparin , warfarin ) ,
thrombolytics ( alteplase , streptokinase …) & even herbal
remedies like ginseng , ginkgo biloba …
Clinical examination :
Signs of bleeding tendency include :
1. Petechial purpura : minor bleeding into the dermis , flat &
non blanching , it may indicate thrombocytopenia or
platelets dysfunction .


petechi

petechi

2. Palpable purpura
Associated mostly with vasculitis .
Other causes of purpura :
* Senile purpura
* Factitious purpura
* Purpura fulminans : e.g in DIC secondary to sepsis
* Paraprotenemia

purpura

3. Ecchymosis or bruising :
More extensive bleeding into the deeper layers of the skin ,
initially dark red or purple then blue , then green & then
yellow as hemoglobin degraded.

bruises
Full examination is important in case of bleeding tendency
e.g in abdominal examination u may find flank hematoma (
retroperitoneal bleeding ) , joint examination may reveal
hemarthrosis )
Systemic examination may give u a clue to the underlying
disease such as hematological malignancy , liver disease ,
renal failure , CT diseases … etc.
Investigations
- CBC , specially concentrating on platelets ( normal range
: 150 -400 * 10^9/l)
- Prothrombin time ( PT) : ( NR. 9-12 second )
Causes of elevated PT :
1. Factor VII deficiency ( isolated PT prolongation) !
2. Liver disease
3. Warfarin therapy
4. Vitamin k deficiency
- Activated partial thromboplastin time ( APTT)
( NR. 26
– 36 sec.)
causes of isolated elevation of APTT
a. Factor VIII deficiency ( hemophilia A )
b. Factor IX deficiency ( hemophilia B ) ( christmas
disease)
C. Factor XI & factor XII deficiency
d. Heparin therapy
e. Von willebrand disease ( mild elevation )
causes of elevated both ( PT & APTT) :
1. Factor II deficiency
2. Factor V deficiency
3. Factor X deficiency
4. Fibrinogen deficiency
5. DIC
6. Severe liver disease & severe vitamin K deficiency
** don’t forget that there are diseases that can cause bleeding
with normal PT , APTT & platelets like : platelet dysfunction (
congenital or acquired ) , factor XIII deficiency ….

Investigation ( continue..)
- Fibrinogen concentration :
( NR : 1.5
– 4 g/l)
Occur in diseases that cause hypofibrinogenemia
Like : DIC & liver failure
-
Factors assay : like factor VIII , factor IX … etc
- Platelet function : previously has been assessed by
bleeding time ( the time to stop bleeding after an incision ) (
normally less than 8 min. ) , but now more recent studies
has been done to assess platelets function like measuring
platelets aggregation in response to adrenalin, ADP ,
collagen ,,, etc.

Thrombocytopenia
Causes of thrombocytopenia :
1. Decrease or abnormal production
2. Increased consumption
(1) Decreased production :
-aplastic anemia
-fanconi anemia
- Megaloblastic anemia
- Leukemia
-drugs : chemotherapy
(2) Increased consumption :
- ITP ( immune thrombocytopenic purpura)
- DIC
- Hypersplenism
- HUS ( hemolytic uremic syndrome)
-TTP ( thrombotic thrombocytopenic purpura)
-liver disease
Note : there is what is called pseudothrombocytopenia or
sporious throbocytopenia due to platelet clumping in the sample
specially when the sample contain EDTA as anticoagulant , in
such case reviewing the peripheral blood smear will show the
clumps , furthermore drawing blood into a sample that contain
citrate instead of EDTA will eliminate the clump .
Immune thrombocytopenic purpura
( ITP)
This condition is caused by autoantibodies mainly directed
against the platelet membrane glycoprotein IIb/IIIa ,
resulting in premature removal from the circulation .
It is usually associated with underlying diseases like :
- C.T. diseases
- HIV infection
- Malignancies
- Pregnancy
Clinical feature of ITP :
Depend on the degree of thrombocytopenia , there may be
bruising , epistaxis , petechi .
Spontaneous bleeding usually occur when platelet count
below 20 * 10 ^9/l .
There may be feature of the underlying disease e.g SLE .
b. Film will show reduced no. of platelets , Bone marrow
will show increased no. of megakaryocytes ( but bone
marrow is rarely needed in ITP , bone marrow is indicated
in pt. older than 60 years , resistant cases & to exclude
marrow fibrosis before splenectomy is done ) .

Management of ITP :
Treatment indicated when there is bleeding , severely
reduced platelet count & when there is upcoming surgery
or biopsy to be taken .
1
st
line therapy is steroid ( prednisolon 1mg /kg daily to
suppress the antibody .
When there is slow response to steroids or there is severe
bleeding : IV IG ( immunoglobulin) .
In more severe cases : platelet transfusion , splenectomy ,
thrombopoietin analogue ( romiplostim ) or the
thrombopoietin receptor agonist eltrombopag , & if no
response immunosuppressants should be considered like
rituximab , ciclosporin …
Haemophilia A
Is a very common congenital coagulation disorder caused
by deficiency of factor VIII , factor VIII is synthesized in the
liver & endothelial cells & protected in the circulation by
binding to von willebrand factor .
Haemophilia A is sex linked disorder because the gene is
located on X chromosome , all daughters of hemophiliacs
are obligate carriers , & in turn have 1 in 4 chance in each
pregnancy resulting in the birth of of an affected male ,
normal male , carrier female & normal female .
Antenatal dx. By chorionic villous sampling is possible .
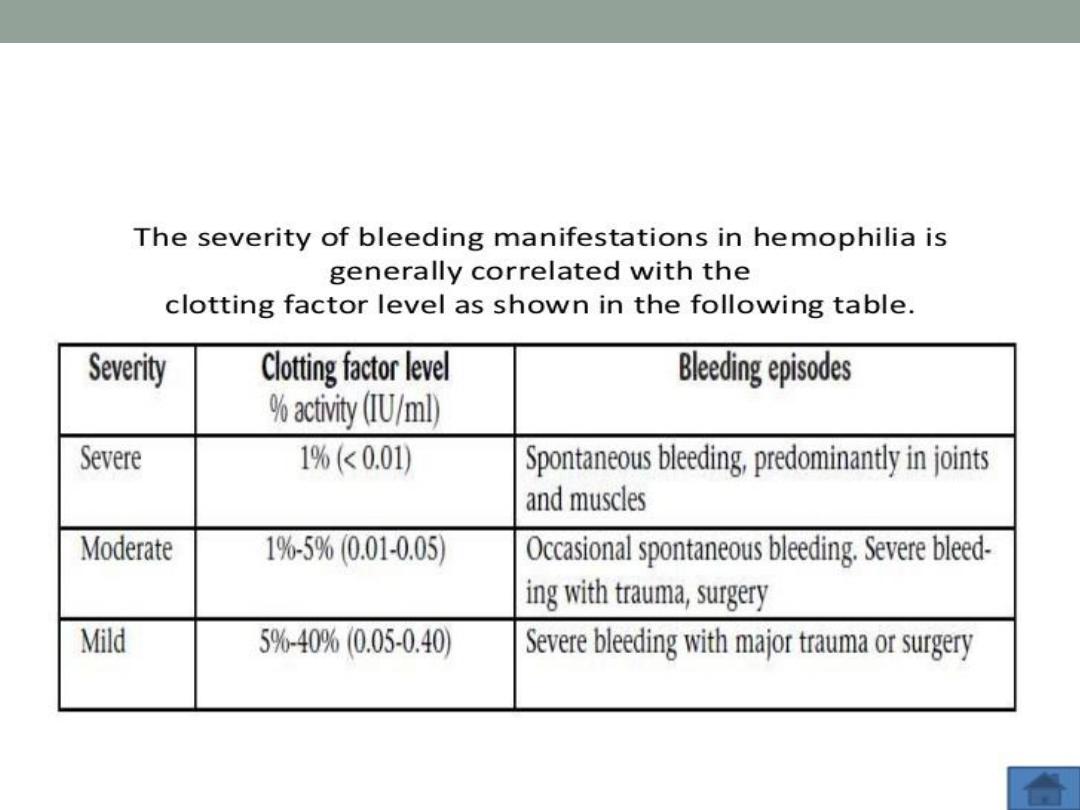
Severity of hemophilia A according to
factor level
Clinical feature
The main feature is bleeding , & this is depend on the
severity of factor VIII D- , severe cases present with
spontaneous bleeding into the skin , muscles , & joints ,
retroperitoneal & CNS bleeding are also features of severe
cases .
Mild to moderate cases also present with bleeding but it is
usually provoked bleeding , i.e. after trauma or surgery .
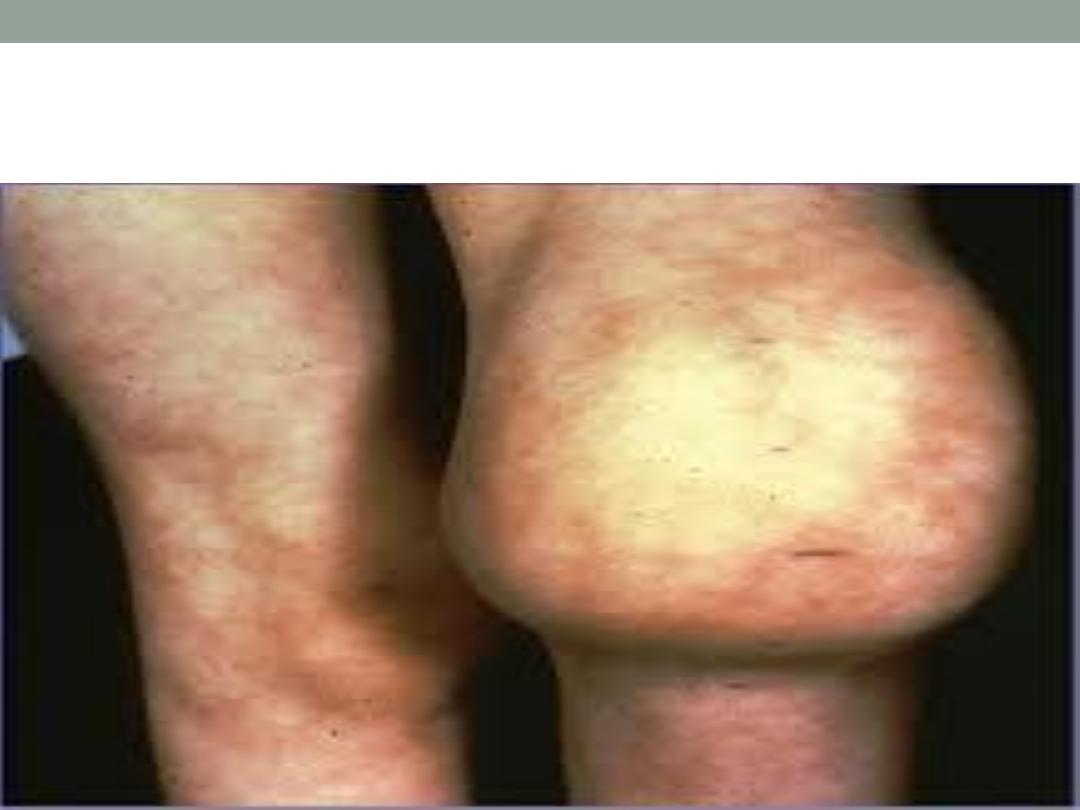
Hemarthrosis & muscle hematoma are characteristic ,
common sites for hemarthrosis are the knee joint & ankle
joint , for the muscle , calf & psoas muscle hematoma are
also common .

Recurrent hemarthrosis can lead to secondary
osteoarthritis ( due to synovial hypertrophy & destruction of
the cartilage).
Psoas M. hematoma can lead to compression of the
femoral nerve , calf hematoma can lead to compartment
syndrome ( ( ischemia , necrosis & fibrosis of the fascial
sheath) .
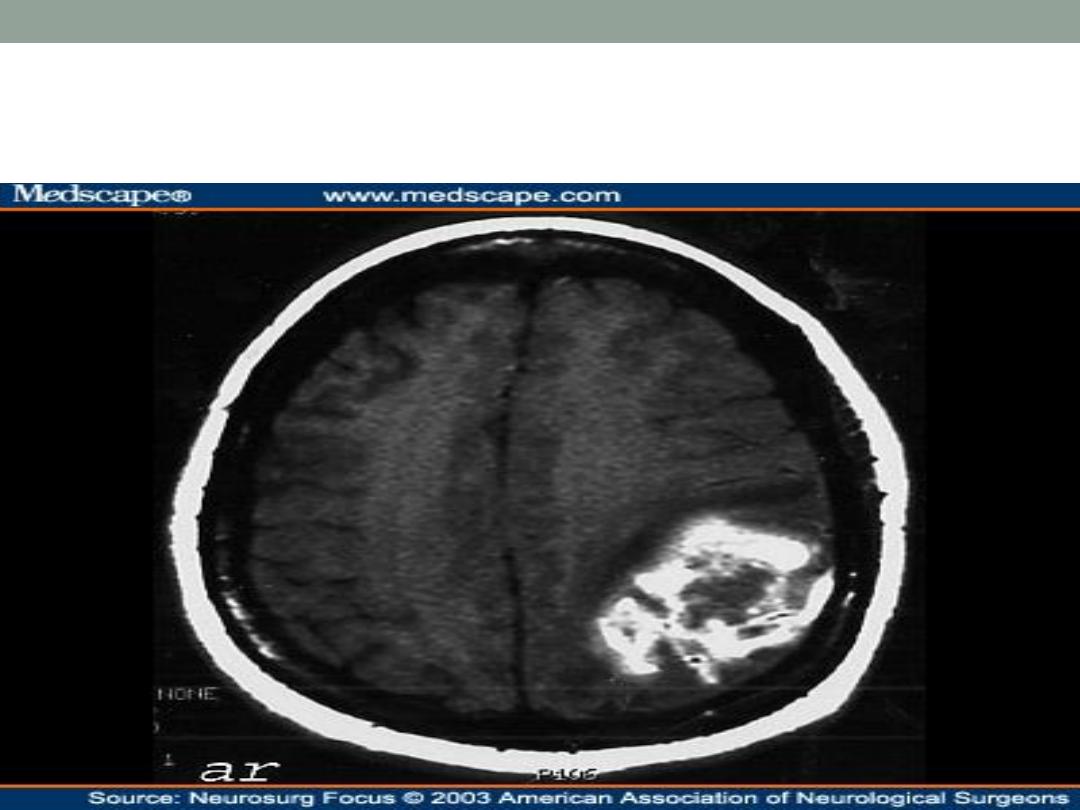
CNS bleeding is the most dangerous form of bleeding &
always should be suspected in hemophilic pt. with
headache or other neurological symptoms.


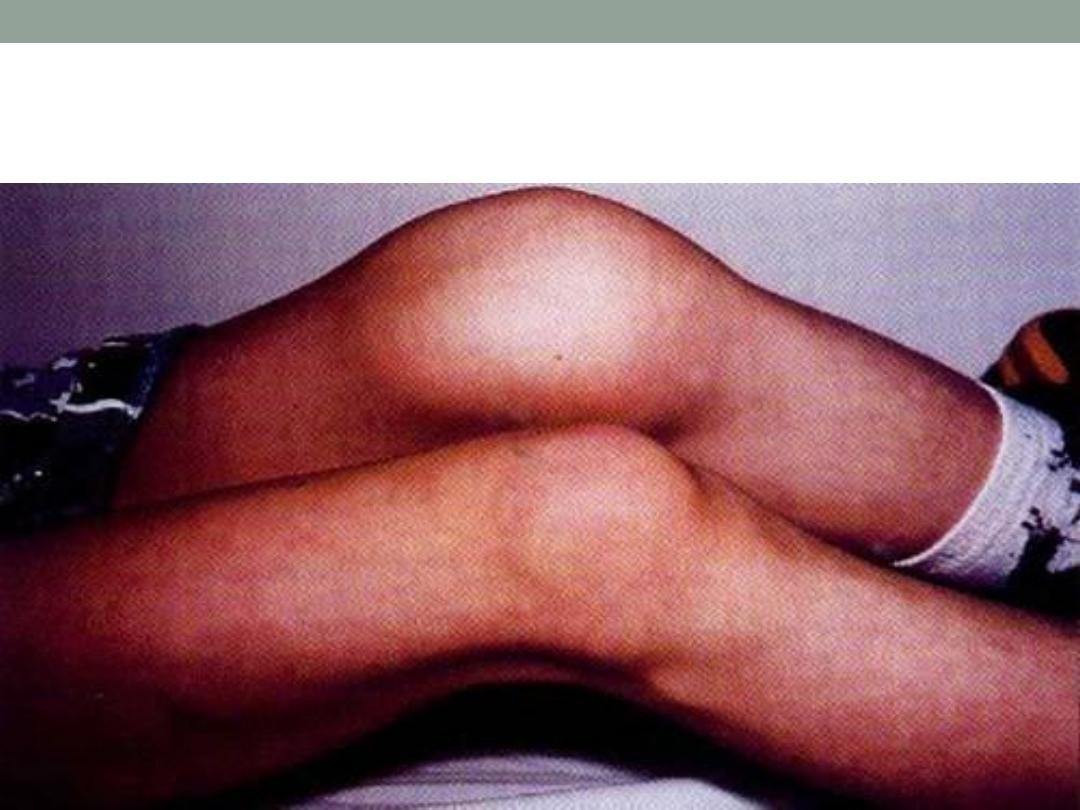
Hemarthrosis

Ct scan : bleeding
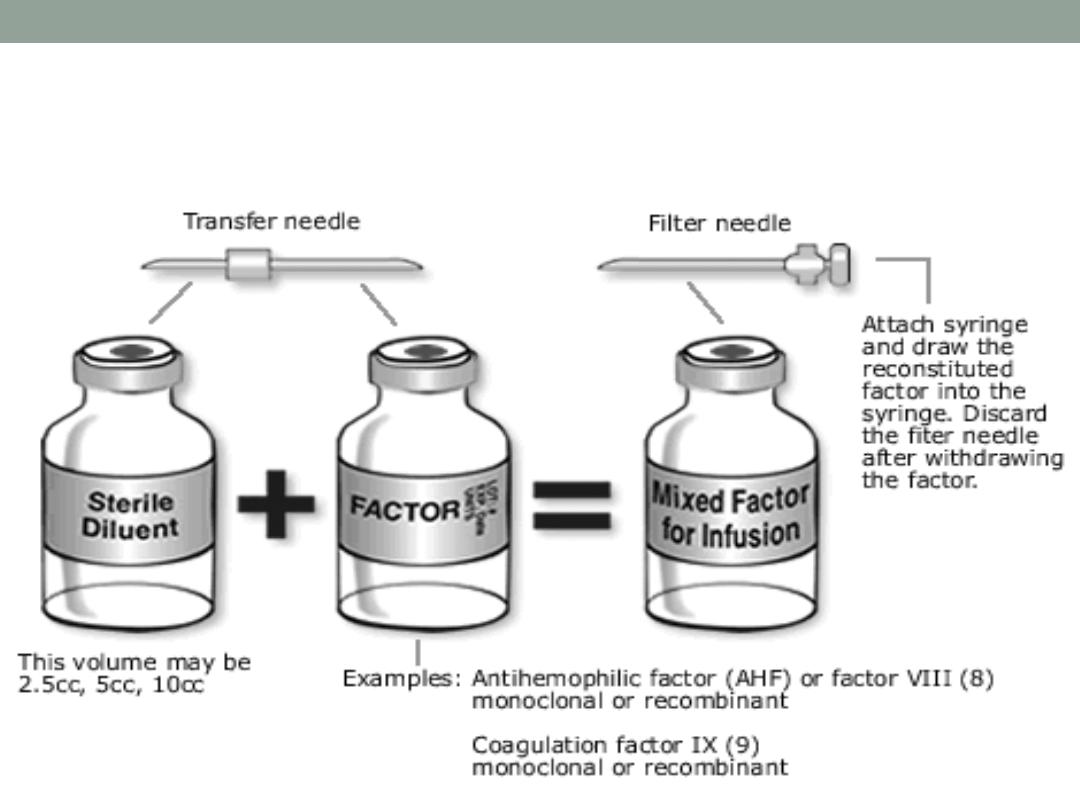
Management of hemophilia A
All patients should avoid trauma & any drug that can cause
bleeding , the main treatment is to give factor VIII
intravenously. Factor VIII should be stored at refrigerator &
thus pts can treat themselves at home at the earliest
indication of bleeding .
The dose can be calculated by :
Wieght * % of bleeding / 2
e.g. 70 kg , bleeding 100%
The dose will be : 70 * 100 = 7000/2 = 3500 IU
the half life is 8-12 hours , so it should be given twice daily
- Desmopressin ( DDAVP) is vasopressin receptor agonist
, it raise the von willebrand factor & factor VIII by 3-4 fold , it
is useful in treatment of mild to moderate bleeding .the
dose is usually 0.3 ug / kg IV or SC or intranasal
adminstration of 300 ug ( be ware of water retention ,
hyponatremia , & it is contraindicated in severe arterial
disease because of risk of thrombosis ) .
- Tranexamic acid ( cycklokapron) : antifibrinolytic drug ,
used as adjunctive therapy to control mild to moderate
bleeding from the gum or oral cavity & sometimes GIT ,
BUT it is contraindicated when there is hematuria bec.
There is risk of clot formation in the lumen of GU tract .

If Factor VIII is not available , cryoprecipitate can be used
sometimes , bec each bag contain around 80 unit of factor VIII.
* Complication of therapy :
1. Inhibitor formation :
One of the major complication of factor VIII therapy is the
development of anti factor VIII antibodies , occur in about 20 %
of severe hemophiliacs . Such antibodies neutralise the
therapeutic infusion making treatment relatively ineffective .
When u suspect inhibitors formation , we should do what is
called ( mixing study ) , which include mixing plasma of
hemophilic pt. with normal plasma ( 1:1) , in normal pt. ( no
inhibitors ) such mixing will correct the APTT completely , while
if there is inhibitors , the APTT will not be corrected .
Treatment of such problem is to give activated clotting factor like
factor VII a or factor VIII inhibitor bypass activity ( FEIBA).
2. Transmission of infections :
specially hepatitis C virus which is major cause of morbidity
in hemophilic patient . Other type of infections include HBV
, HIV , CJD …
Recombinant factor VIII associated with decrease risk of
viral infection .

VON WILLEBRAND DISEASE
a common but mild bleeding disorder , caused by
deficiency of von willebrand factor which is involved in both
platelet function & coagulation .
VWF act as a carrier protein for factor VIII. So deficiency of
VWF lower the plasma factor VIII level.
Clinical feature : the patient presented with bleeding
tendency similar to those with reduced platelet function ,
superficial bruising , epistaxis , & commonly menorrhagia in
females, the bleeding is usually less severe than
hemophilia .
Treatment :
Many mild cases can be treated by local means only or
with desmopressin ( enhance release of VWF from
endothelial cells )
Tranexamic acid may be useful in mucosal bleeding , for
more serious bleeding using selected factor VIII
concentrate which contain considerable quantities of VWF
in addition to factor VIII .
Disseminated intravascular coagulation (
DIC)
Characterized by activation of the pathways involved in
coagulation & its regulation , this may result in generation
of intravascular fibrin clots causing multiorgan failure with
consumption of both platelets & coagulation factors causing
bleeding
Clinically there will be bleeding , oozing from venipuncture
sites , petechi , ecchymosis , GIT blleding & even CNS
bleeding . There is also hypercoagulability state resulting in
occlusion of the vessels in the microcirculation resulting in
organ failure & shock state .
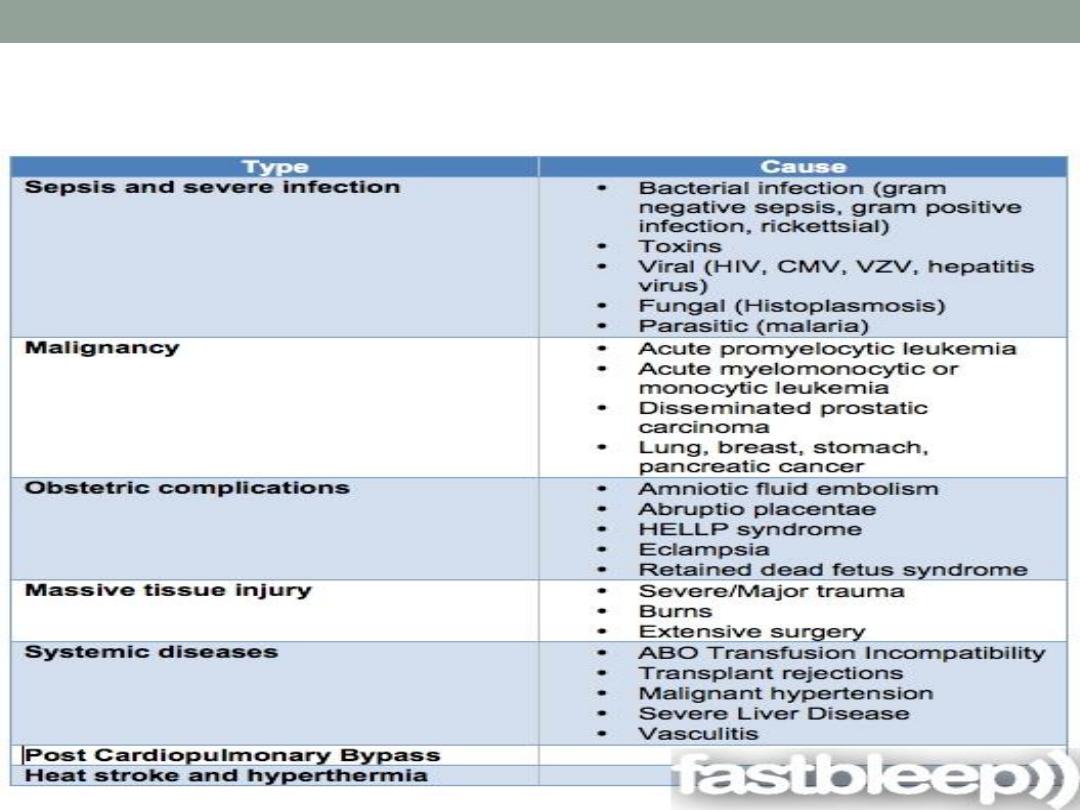
Causes of DIC
Investigations
1. Low platelets
2. Low fibrinogen
3. Prolonged PT
4. Prolonged APTT
5. Elevated D dimer .
6. Evidence of organ failure
Management
Treatment is mainly to correct the underlying cause , the pt.
is usually treated at the ICU , to deal with the concomitant
issues like , dehydration , acidosis , multiorgan failure &
hypoxia .
Fresh frozen plasma , cryoprecipitate & platelet transfusion
may be necessary if the patient has bleeding .
If there is evidence of thrombosis , treatment with heparin (
cautiously !! ) should be done with close monitoring .
Acquired bleeding disorders
-liver disease :
In severe parenchymal liver disease bleeding may arise
from different causes :
*GIT bleeding from esophageal varices or peptic ulcer
* Reduced hepatic synthesis of of factor V, VII , VIII ! , IX, X,
XI , prothrombin & fibrinogen .
*thrombocytopenia secondary to hypersplenism
*vitamin K deficiency ( specially in cholestatic jaundice).
Renal failure :
This is mainly proportional to the elevated urea level , the
causes of bleeding are multifactorial including platelets
dysfunction & blood loss during dialysis .
THANK
YOU
FOR LISTENING
