Group c
Medicine
NO
4
د
.
ظاهر
2/11/2017
Acute respiratory distress syndrome (ARDS)
and Acute Lung Injury (ALI)
THE EARLY HISTORY OF ARDS:
In 2012, the ARDS Definition Task Force met in Berlin and decided on a new and
improved definition of ARDS using 3 mutually exclusive categories of ARDS based on
the degree of hypoxemia:
≤300 mm Hg),
FIO2
2/
<pao
(200 mm Hg
Mild
≤200 mm Hg),
<pao2/FIO2
(100 mm Hg
Moderate
≤100 mm Hg).
(PaO2/FIO2
Severe
ALI and ARDS are clinical syndromes characterized by the acute onset(<7 days)of
hypoxaemia with bilateral pulmonary infiltrates in the absence of clinical evidence of
left atrial hypertension
causes :
ARDS may follow a diverse group of direct and indirect insults
Direct insults include :
1.Aspiration of gastric contents .
2.Near drowning .
3.Toxic gas injury .
4.Smoke inhalation .
5.Diffuse pneumonia .
6.Lung contusion .
Indirect (systemic) insults include :
1.Spsis.
2.Multiple blood transfusion .
3.Acute pancreatitis .
4.Drugs like opioids ,aspirin, barbiturates ,and thiazide .
5.Multiple trauma (including fractures)
6.Necrotic tissue .
7.Severe burns .
8.Cardiac pulmonary bypass .
9.Fat embolism .
10.Obstetric events : eclampsia and amniotic fluid embolism .
Pathology :
It is characterized by neutrophil sequestration in pulmonary capillaries , increased
capillary permeability , protein-rich pulmonary edema with hyaline membrane
formation , damage to type 2 pneumocytes leading to surfactant depletion , alveolar
collapse and reduction in lung compliance .
If this early phase doesn’t resolve with treatment of underlying cause , a fibro-
proliferative phase ensues and causes progressive pulmonary fibrosis .
Clinical Course:
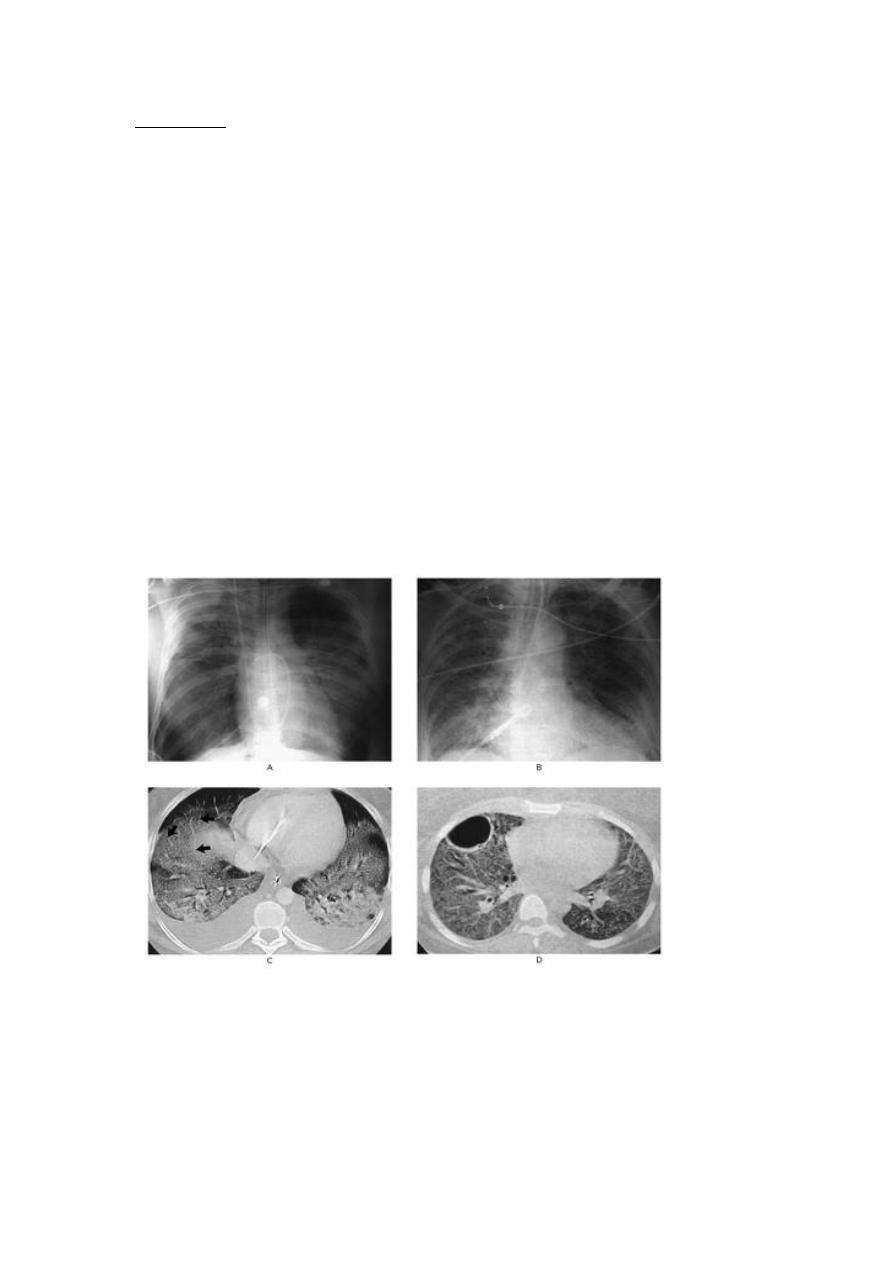
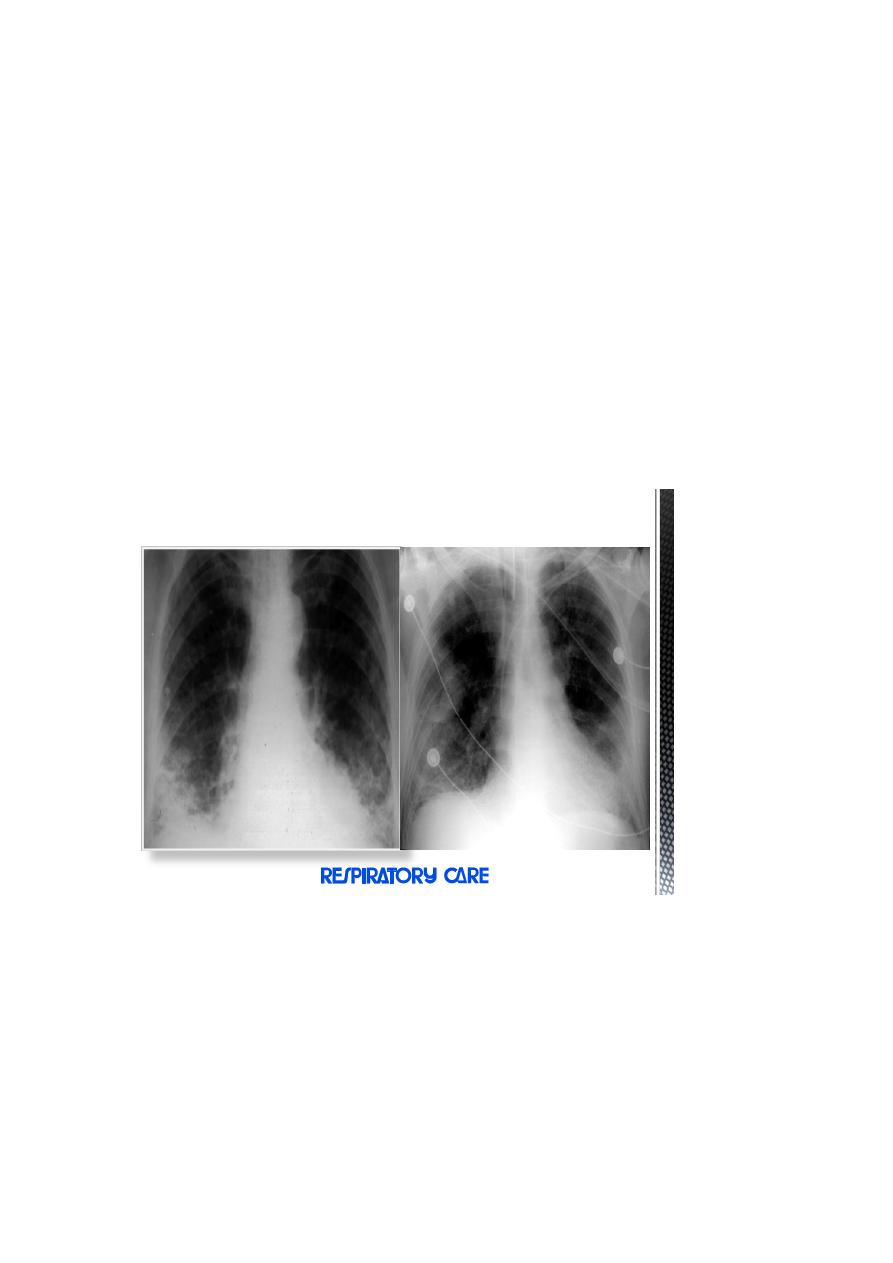
Early findings on the chest radiograph include normal or diffuse alveolar opacities
(consolidation), which are often bilateral and which obscure the pulmonary
vascular markings.
Later, these opacities progress to more extensive consolidation that is diffuse, and
they are often asymmetrical.
Effusions and septal lines are not usually seen on chest radiographs of patients
affected by ARDS, although these findings are commonly seen in patients with
congestive heart failure (CHF).
Radiographic findings tend to stabilize (part of the clinical definition of ARDS);
if further radiographic worsening occurs after 5-7 days, another disease process
should be considered.
Acute Phase
Rapid Onset
Exudates
Consolidations
Respiratory failure
Hypoxemia refractory to O2
Inflammation (even in non-edematous lung)IL-1,6,8,10, Cytokines
Diminished Lung compliance
Patchy infiltrates Coalesce
Air Bronchograms
Pulmonary Hypertension
Intrapulmonary Shunting
Endogenous Vasoconstrictors
Hyperadrenergic State
Fibroproliferative phase
Persistent Hypoxia
Pulmonary Fibrosis
Worsening Compliance
Neovascularization
Pulmonary Hypertension
Macrophages clear neutrophils
Chronic Inflammation
Chest xray shows linear opacities consistent with evolving fibrosis.
Pneumothorax in 10-13% of patients.
CT: diffuse interstitial opacities and bullae.
Histologically, fibrosis, mesenchymal cells, vascular proliferation, collagen
and fibronectin accumulation.
Can start 5-7 days after symptom onset.
Not present in every patient with ARDS, but does portend poorer prognosis

Lung injury score according to
CXR
and
PaO
2
/FiO
2
CXR
No consolidation ..0
Confined to 1 quadrant …1
2- quadrant ……….2
3- quadrant ……….3
4 -quadrant ……….4
PaO
2
/FiO
2
>300……..0
225-299 …1
175-224 …2
100-174 …3
<100……..4
Add the sum of each component and divide by the number of
components used
0- No lung injury
0.1-2.5 – Mild to moderate lung injury
>2.5 – Severe lung injury (ARDS)
Management :
Management generaly remains supportive , aiming at :
1.Elimination of underlying precipitating condition like treating infection or shock.
2.Maintaining oxygenation and ventilation .
3.Preventing complications .
In early stages suplemmental oxgen and physiotherapy may suffice , but
endotracheal intubation (or tracheostomy ) and mechanical ventilation is required in
vast majority of cases.
Ventilator Strategies:
A-Lung recruitment maneuvers
B-Prone positioning
C-High-frequency oscillatory ventilation (HFOV)
Lung Recruitment
A-To open the collapsed alveoli
B-A sustained inflation of the lungs to higher airway
pressure and volumes
Ex.: PCV, Pi = 45 cmH2O, PEEP = 5 cmH2O, RR = 10
/min, I : E = 1:1, for 2 minutes.
Potentially recruitable (PEEP 5
15 cmH2O)
Increase in PaO2:FiO2
Decrease in PaCO2
Increase in compliance
The effect of PEEP correlates with the percentage of potentially
recruitalbe lung
The percentage of recruitable lung correlates with the overall
severity of lung injury
NEJM 2007; 354: 1775-1786
Sensitivity : 71%
Specificity : 59%
NEJM 2007; 354: 1775-1786
Positive End-Expiratory Pressure (PEEP):
Titrate PEEP to decrease FiO2
Goal sat 88% with FiO2 <60%
• Minimize oxygen toxicity
PEEP can improve lung recruitment and decrease end-expiratory
alveolar collapse (and therefore right-to-left shunt)
Can also decrease venous return, cause hemodynamic compromise,
worsen pulmonary edema
ARDSnet PEEP trial of 549 patients show no difference in mortality or days on
ventilator with high vs low PEEP
PEEP level separation at various Fi
O2
levels was in the range of 6 cm H
2
O (mean of 14
versus 8 cm H
2
O) .
The use of 6 ml/kg PBW tidal volume strategy and PEEP–Fi
O2
scale as a starting point
for ventilation is recommended but routine use of recruitment maneuvers is not.
However, it would be reasonable to reserve higher levels of PEEP and/or recruitment
maneuvers for patients with refractory hypoxemia in an attempt to improve
oxygenation when severity of the oxygenation defect is the most immediate threat
to survival.
Prone Position advantages and disadvantages
Prone Position advantages and disadvantages
Mechanisms to improve oxygenation:
a-Increase in end-expiratory lung volume
b-Better ventilation-perfusion matching
c-More efficient drainage of secretions
d-Improve oxygenation in about 2/3 of all treated patients
c-No improvement on survival, time on ventilation, or time in ICU
f-Might be useful to treat refractory hypoxemia
g-Optimum timing or duration ?
h-Routine use is not recommended
Side effects of Prone Position
A-Facial edema, Airway obstruction Skin lesions
B-Difficulties with enteral feeding, Hypotension
C-Transitory decrease in oxygen saturation. Arrhythmias
D-Loss of venous accesses and probes,
E-Increase need for sedation.
F-Loss of dialysis drains and catheters, Accidental extubation.
G-Apical atelectasis due to incorrect positioning of the tracheal tube
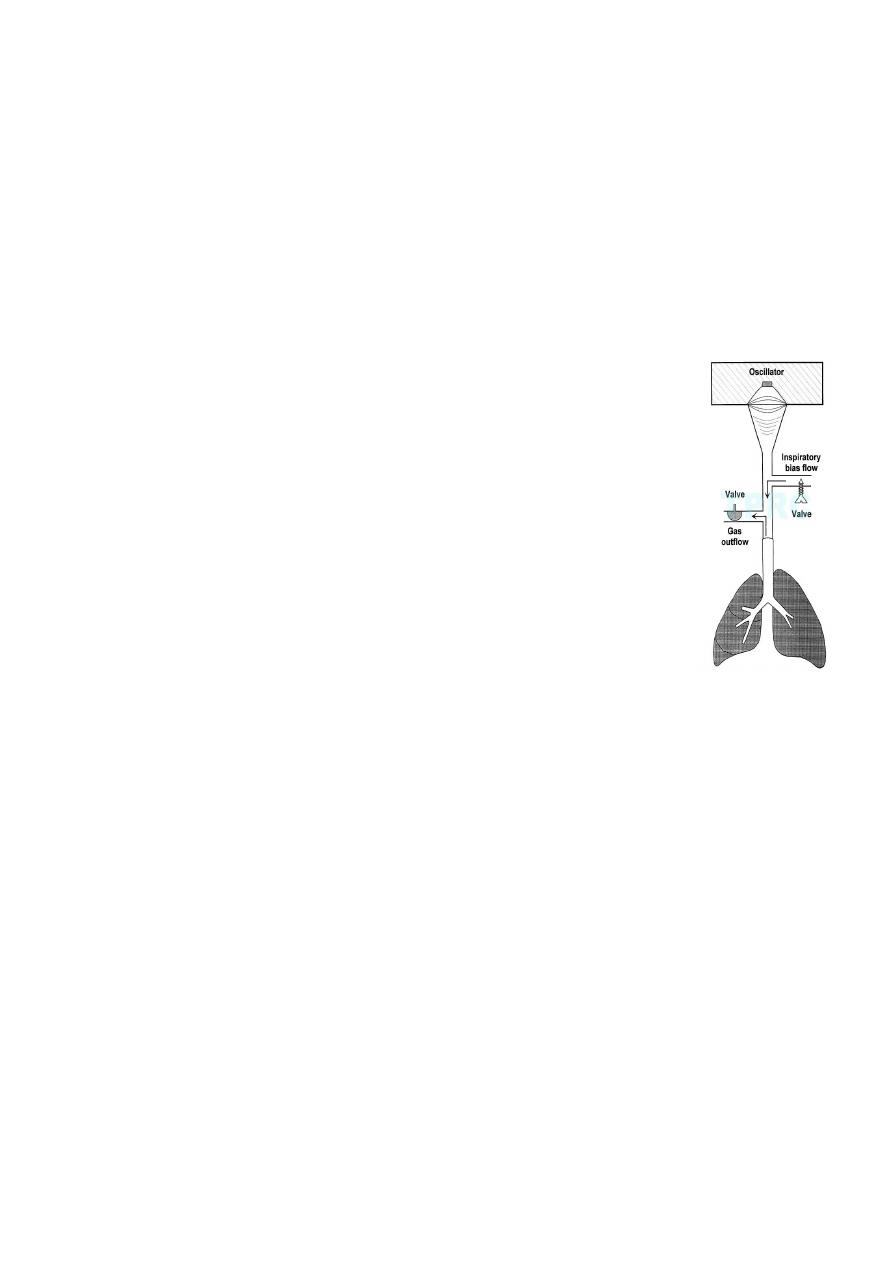
High-Frequency Oscillatory Ventilation (HFOV):
• High frequency oscillatory ventilation shown no benefit over low
tidal volume ventilation
• 30 day mortality not statistically significant (37% vs
52%, p=0.10)
• Earlier recovery from hypoxia
Adjunctive Therapy:
A-Steroid treatment
B-Fluid management
C-Extracorporeal membrane oxygenation (ECMO)
D-Nitric oxide
E-Others

Steroid therapy:
A-Increase the number of ventilator-free and shock-free days during the first 28 day
B-Improve oxygenation, compliance and blood pressure
C-No increase in the rate of infectious complications
D-Higher rate of neuromuscular weakness
E-Routine use of steroid is not supported
F-Starting steroid more than 14 days after the onset of ARDS may increase mortality
Nitric Oxide,Vasodilator ,Improve oxygenation and pulmonary vascular
resistance.
No improvement on survival
Extracorporeal Membrane Oxygenation (ECMO), No improvement on survival
or time on ventilation.
The only treatment that shows mortality benefit:
lung-protective ventilation strategy
Low tidal volume (6ml/Kg), high PEEP, adequate Pplat (<30 cmH2O)
Modalities to improve oxygenation:
Prone position, steroid, fluid treatment, steroid, HFOV, NO
Combining other treatments:
Activated protein C, antibiotics, EGDT…etc
Supportive treatments:
Fluid balance
Sepsis management
Restrictive transfusion
Specific strategies (pharmocological interventions)
Activated protein C
Mesenchymal stem cells

Fluid Management:
• Study of conservative vs liberal fluid management
5
• 60 day mortality: 25.5 vs 28.4% p=0.30
• 1
st
28 days ventilator free: 14.6 vs 12.1 p<0.001
• 1
st
28 days ICU free: 13.4 vs 11.2 p<0.001
• Difference in organ failure and need for dialysis not
statistically significant
• No specific mention of CVP/ PAOP levels which to aim for
• Conservative = 4mmHg Liberal = 10-14mmHg CVP
A variety of coagulation inhibitors have been tested including heparin, antithrombin,
tissue factor pathway inhibitor, factor VIIa, activated protein C, and thrombomodulin
in animal models and/or humans with either sepsis or ALI .
To date only activated protein has been proven useful in severe sepsis, though it is
not clear that it directly improves lung function
