1
EVALUATION AND
TREATMENT OF MYOCLONUS
Introduction
Myoclonus is one of the most common movement disorders.
The differential diagnosis of the patient with myoclonus is broad.
Definition
Is a sudden, brief, shocklike involuntary movements arising from the
central nervous system.
It is of two types:
1. Positive myoclonus caused by sudden contraction of muscle or
group of muscles.
2. negative myoclonus (muscle-tone lapses) caused by brief loss of
muscle tone in agonist muscles followed by a compensatory jerk of
antagonistic muscle. Asterixis, as seen in hepatic and uremic
encephalopathy, and the postural lapses of posthypoxic myoclonus
(Lance-Adams Syndrome) and stiff person syndrome are examples of
negative myoclonus.
When we face myoclonus we have to ask ourselves 4 question:
1. What is the cause of the myoclonus?
2. From which part of the nervous system does this myoclonus
originating?
3. Are the myoclonic jerks positive or negative or both?
4. How should the patient be treated?
What Is the Cause of Myoclonus?
Physiological
1. Hypnic jerks upon falling asleep.
2. Startle myoclonus.
3. Hiccup which is myoclonus of diaphragm.
4. Benign infantile myoclonus.
2
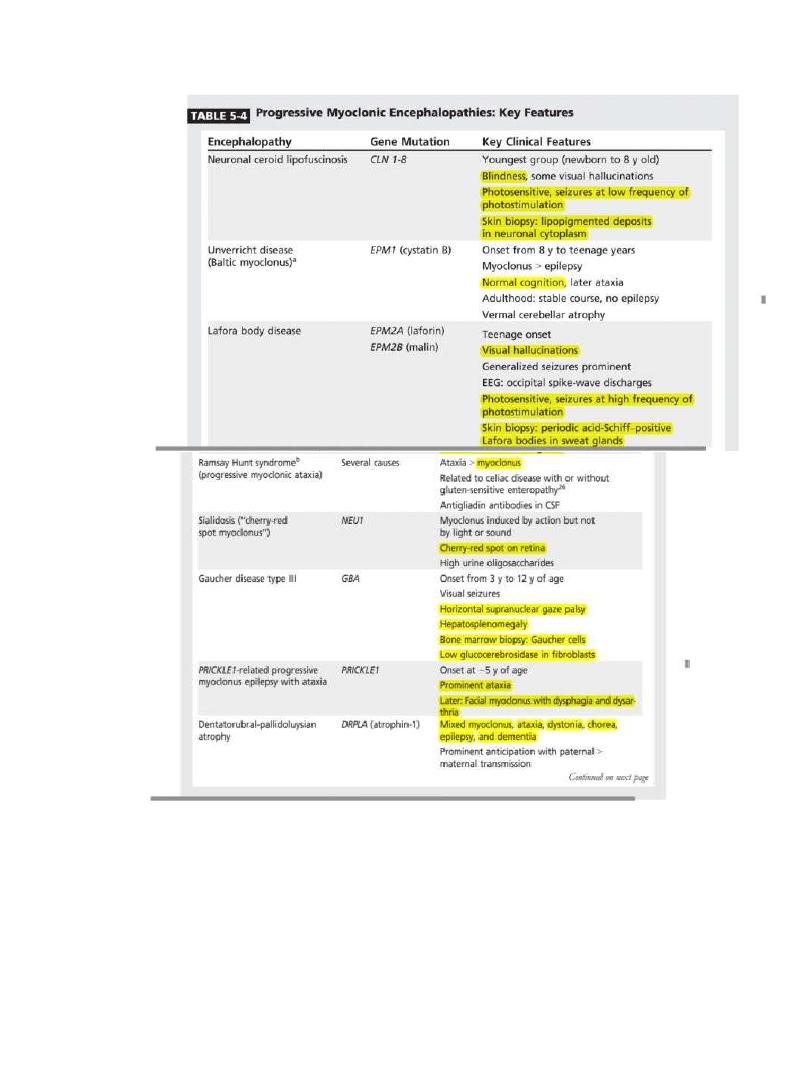
Progressive Myoclonic Encephalopathies
The progressive myoclonic encephalopathies belong to the spectrum of
myoclonic epilepsies and characterized by the presence of
1. progressive childhood or juvenile onset myoclonus.
2. multiple seizures “generalized tonic- clonic, partial seizures”.
3. cognitive deterioration.
4. cerebellar impairement.
5. and history of consanguinity.
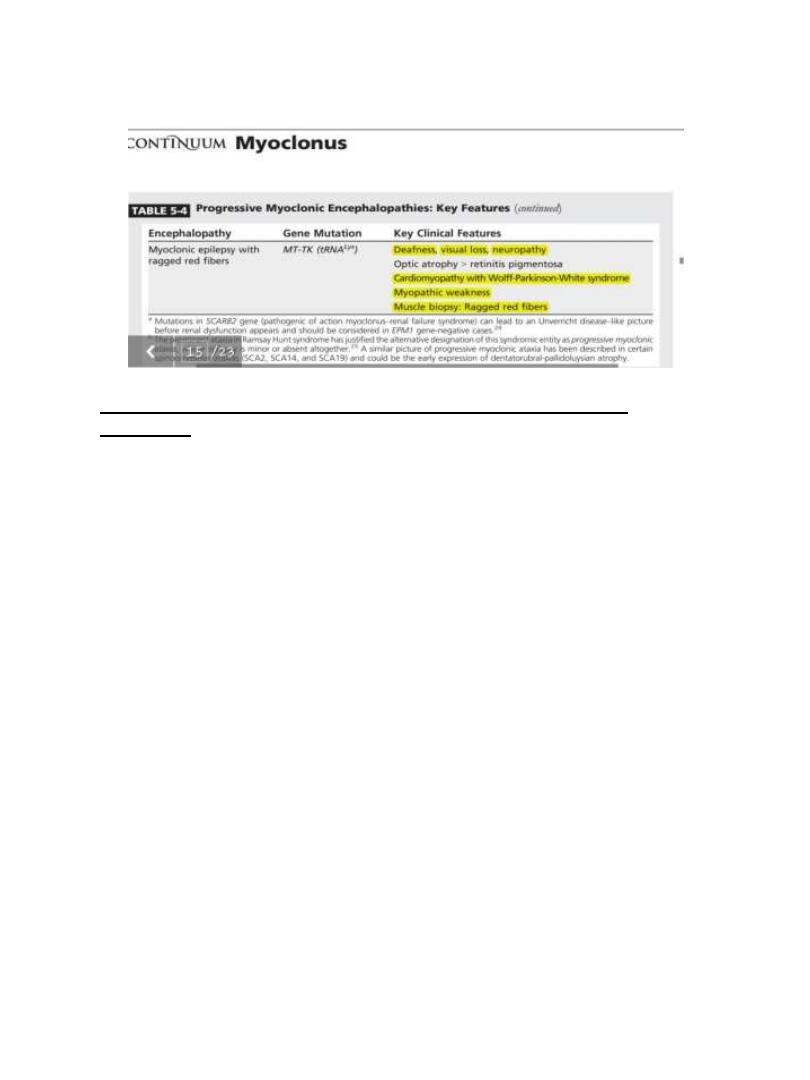
Most of the disorders in this category are autosomal recessive except
for Dentatorubral-Pallidoluysian atrophy (DRPLA), which is autosomal
dominant, and myoclonic epilepsy with ragged red fibers (MERRF),
which is of maternal inheritance.
Progressive myoclonic encephalopathies may be misdiagnosed early on
as juvenile myoclonic epilepsy or as one of the pure myoclonic
epilepsies.
Myoclonus-dystonia
Epileptic myoclonus
1.
Juvenile myoclonic epilepsy.
2.
Epilepsia partialis continua.
3.
Infantile spasms.
Progressive myoclonic epilepsy
see table
Symptomatic myoclonus
1.
Posthypoxic myoclonus (Lance-Adams
syndrome).
2.
Posttraumatic myoclonus.
3.
Infectious and Postinfectious
myoclonus (subacute sclerosing
panencephalitis)
4.
Myoclonic dementias (Alzheimer’s
disease, Jacob-Creutzfeldt).
5.
Basal ganglia disorders
I.
Parkinson disease,
II.
parkinsonian syndrome as
Corticobasal degeneration and
multiple system atrophy.
III.
Huntington’s disease.
6. Metabolic myoclonus.
7. Toxic induced myoclonus.
8. Drug induced myoclonus
3
4
From which part in the Nervous System does this Myoclonus
Originate?
Myoclonus may originate from the cerebral cortex, subcortical
structures, brain stem, spinal cord, or peripheral nerve.
Deciding whether myoclonus is cortical, subcortical, brain stem, spinal,
or peripheral in origin is the single most important information to
determine the suitable antimyoclonic therapy.
Cortical myoclonus typically involves an arm, a leg, or the face; is
triggered by action or intention; and is often stimulus sensitive.
Subcortical myoclonus refers to myoclonus that cannot be linked to a
specific cortical discharge. Thalamic myoclonus is frequently negative
and often produces asterixis in an arm.
Brainstem myoclonus occurs in three forms: startle, palatal, and
reticular reflex “proximal, generalized and stimulus sensitive”.
Spinal myoclonus occurs in two forms: segmental and propriospinal.
Spinal segmental myoclonus is usually restricted to several adjacent
segments of the spinal cord, usually the cervical or thoracic cord, and is
typically rhythmic and stimulus insensitive.
Propriospinal myoclonus usually originate from thoracic cord and
spread slowly up and down the cord.

5
peripheral nerve myoclonus for example hemifacial spasm, is limited
to the involved peripheral nerve, is irregular, and is typically stimulus
insensitive.
NB brainstem, spinal and peripheral myoclonus is easily distinguished
but It is often impossible to differentiate cortical from subcortical
myoclonus, as cortical myoclonus may occasionally be regular and
stimulus insensitive, and subcortical myoclonus may occasionally be
stimulus sensitive.
Although clinical examination can aid in localizing the origin of the
myoclonus, a definitive answer requires electrophysiological testing
and the most important is any form of myoclonus is electromyograms
(EMGs) using surface electrodes. In order to find the distribution and
spread of myoclonus, it is better to record simultaneously from as
many muscles as possible. Cortical myoclonus is associated with an
EMG discharge of abrupt onset and short duration, lasting less than 50
m/s. Myoclonus may spread from proximal to distal muscles at the
speed of about 50 m/s, which approximately corresponds to the
conduction velocity of -motor fibers. The second method is (EEG)-EMG
polygraph detect time and spatial relationship between the EEG spikes
and myoclonus.
The third method is Somatosensory evoked potentials (SEPs) by
delivering electric shocks to the median nerve at wrist with the pulse
duration of 0.2 m/s to 0.3 m/s.
According to the cause and site of origin, myoclonus can be classified
into:
1. Primary myoclonus can be subdivided into
1.physiologic (eg, Hypnic jerks), •
2. essential (idiopathic or hereditary), or
3. purely epileptic.
2. Secondary myoclonus in which the myoclonus is a manifestation of
an underlying disorder which can be further subdivided depending on
6
whether the myoclonus is of cortical or subcortical origin. Whereas
cortical myoclonus predominantly affects the face, arm or leg and
tends to be action induced stimulus sensitive especially tactile.
subcortical myoclonus tends to be unilateral segmental or generalized,
present both at rest and on action and is more often sensitive to
auditory stimuli.
Is the Myoclonus Positive or Negative?
Positive myoclonus is more common than negative myoclonus in the
outpatient clinic, while negative myoclonus is frequently seen in the
hospital setting. Positive myoclonus often responds to treatment,
whereas therapy for negative myoclonus is extremely limited. Often
patients have both positive and negative jerks, and differentiating the
two may be difficult.
How Should Myoclonus Be Treated?
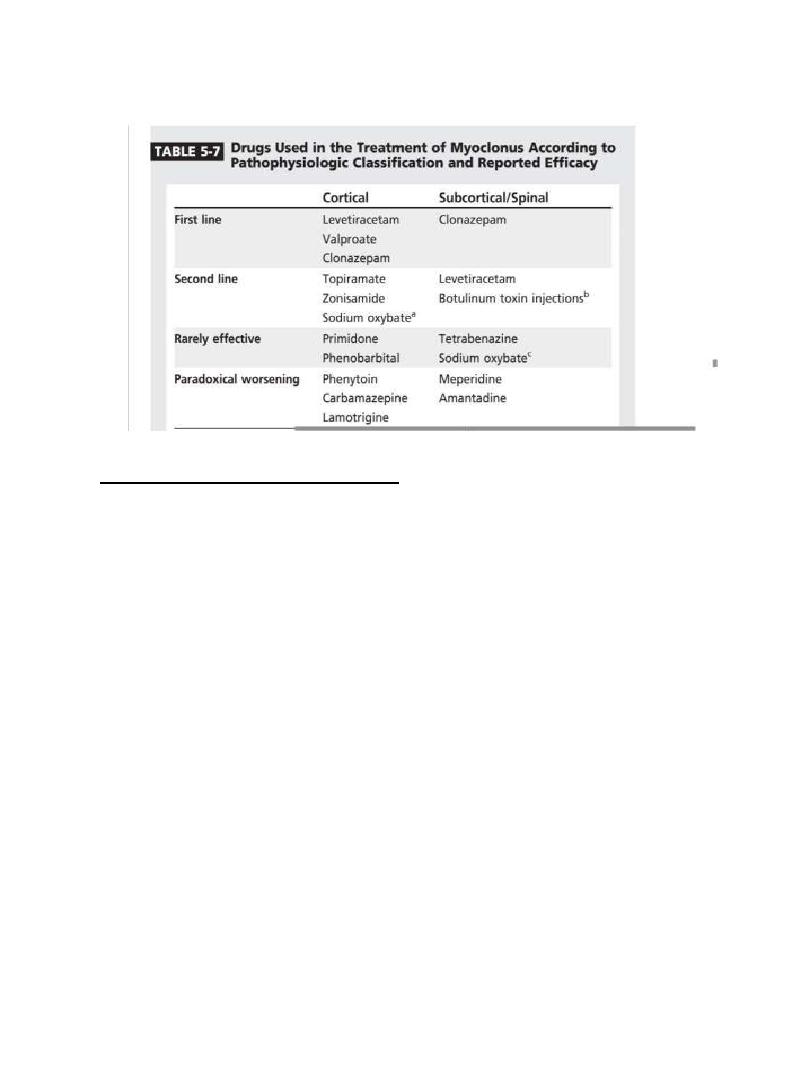
As mentioned the most important factor that determine treatment of
myoclonus is the site of origin within the neural axis, underlying
pathology and side effect profile.
Unlike the treatment of epilepsy, antimyoclonic agents are usually
used in combination, and it is rare for one agent to achieve complete
control of myoclonus.
First line
Second line
levetiracetam ,Valproate and clonazepam
topiramate and zonisamide
7
SPECIFIC MYOCLONUS DISORDERS
Posthypoxic Myoclonus
•
It is a subcortical myoclonus that occur days to weeks after
recovery of consciousness in survivors of cardiorespiratory arrest
mainly asthma in 75% of cases.
•
It is characterized by severe action and intention myoclonus.
•
Treatment drug of choice is levetiracetam in doses of 1000 mg/d
to 1500 mg/d. Other agents that have been used to treat posthypoxic
myoclonus include valproic acid, clonazepam. Also patient show
dramatic response to alcohol although it is short lived.
