
Arrhythmias
• Disturbance of heart rhythm generation
and/or conduction.
• Arrhythmia :
– Tachyarrhythmia
– bradyaahythmia
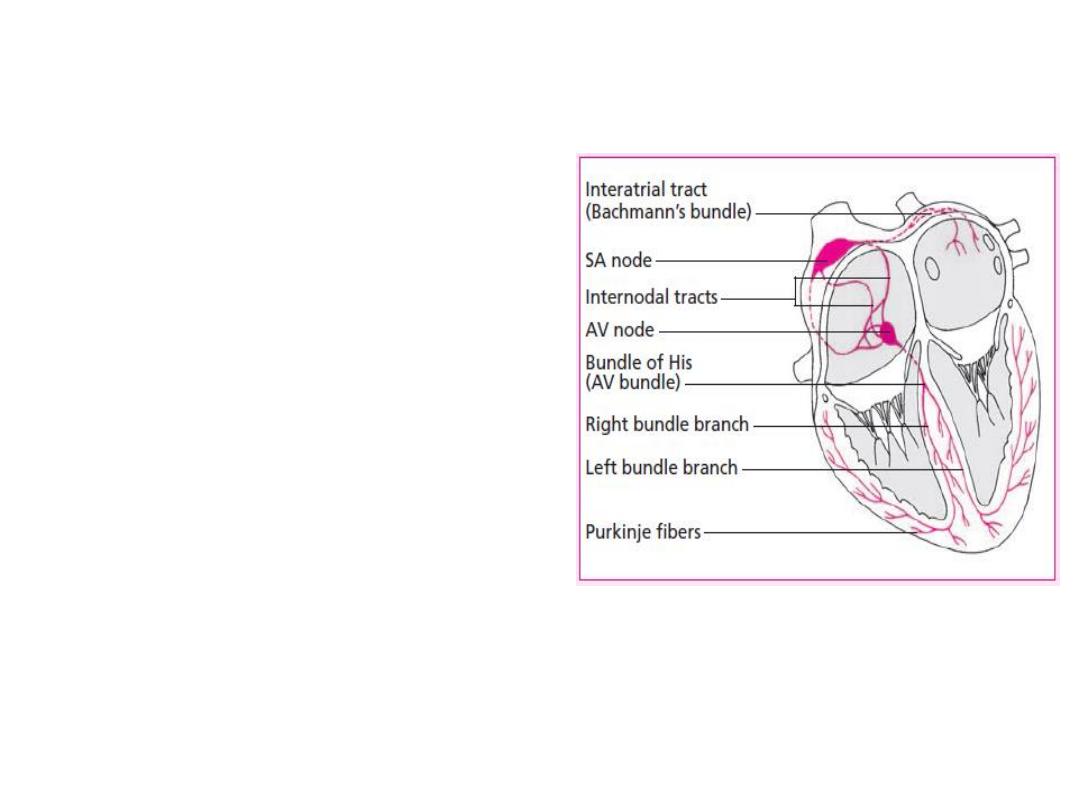
Conductive system of the heart
• SA Node
- Dominant
pacemaker with an
intrinsic rate of 60 -
100 beats/minute.
• AV Node
- Back-up
pacemaker with an
intrinsic rate of 40 - 60
beats/minute.
• Ventricular cells
- Back-
up pacemaker with an
intrinsic rate of 20 - 45
bpm.

Mechanism of Arrhthmogensis
1. Disorder of impulse formation.
a) Automaticity.
b) Triggered Activity.
1) Early after depolarization.
2) Delayed after depolarization.
2. Disorder of impulse conduction.
a)
Block – Reentry.
b)
Reflection.
3. Combined disorder.

Etiology
• Physiological
• Pathological:
Valvular heart disease.
Ischemic heart disease.
Hypertensive heart diseases.
Congenital heart disease.
Cardiomyopathies.
Carditis.
RV dysplasia.
Drug related.
Pericarditis.
Pulmonary diseases.
Others.

Arrhythmia Presentation
• Palpitation.
• Dizziness.
• Chest Pain.
• Dyspnea.
• Fainting.
• Sudden cardiac death.
Arrhythmia Assessment
• ECG
• 24h Holter monitor
• Echocardiogram
• Stress test
• Coronary angiography
• Electrophysiology study
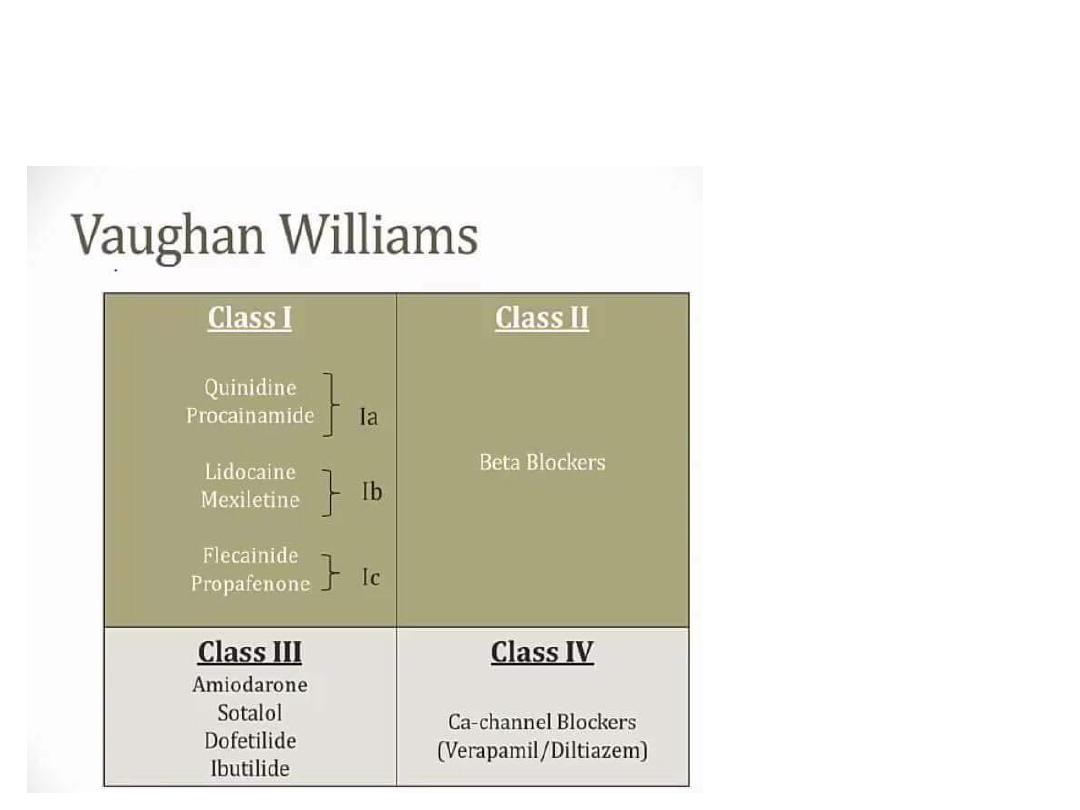
Antiarrhythmic drugs
• Digoxin
• Adenosine
• Atropine

Arrhythmias
• Sinus Rhythms
• Premature Beats
• Supraventricular Arrhythmias
• Ventricular Arrhythmias
• AV Junctional Blocks
pot.com

Sinus Rhythms
•
Sinus Bradycardia
•
Sinus Tachycardia
spot.com
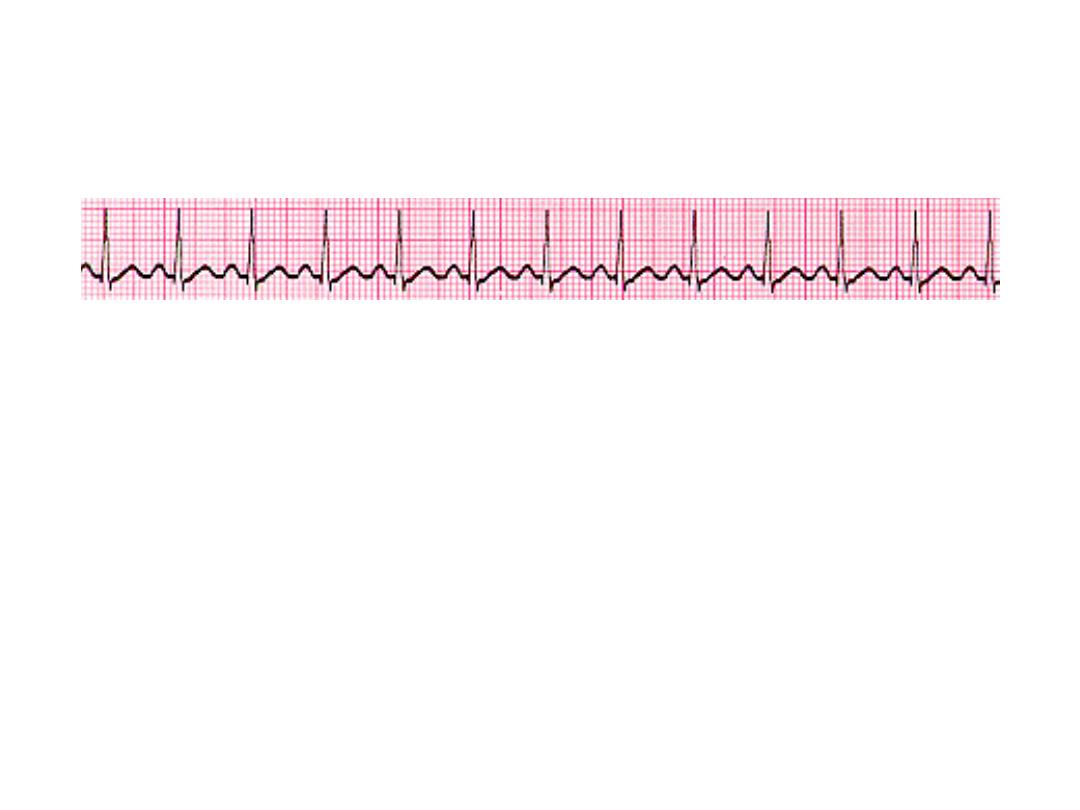
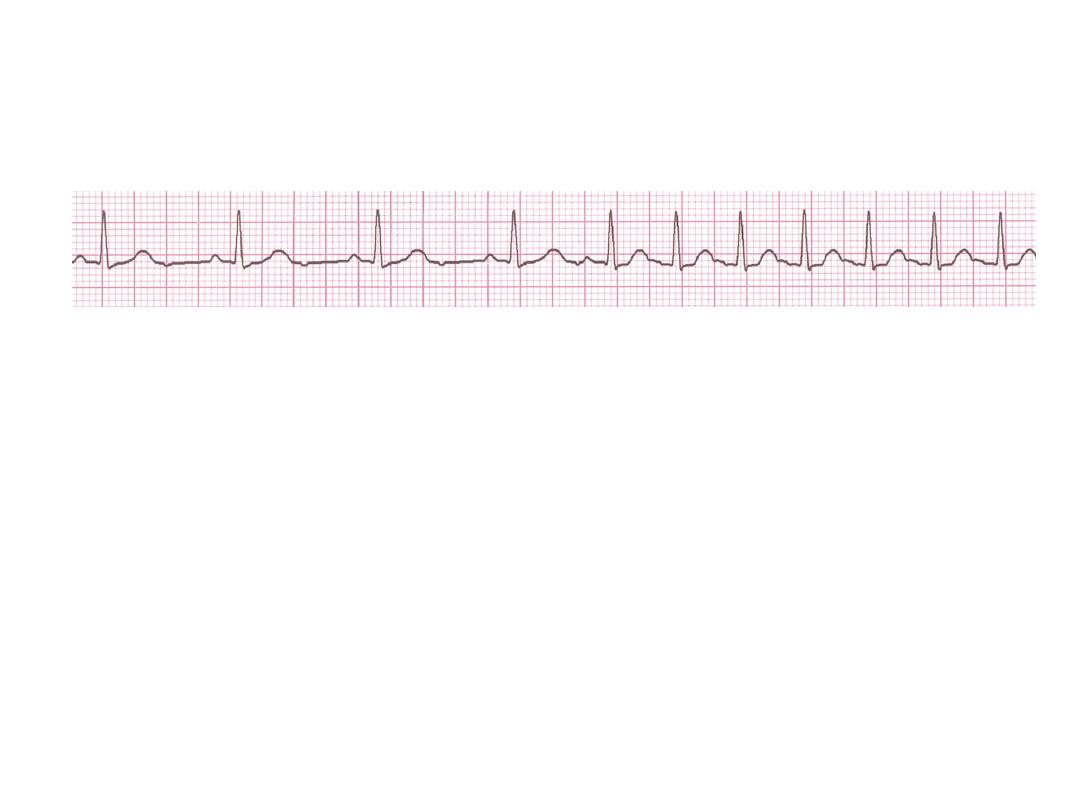
Sinus Bradycardia
• Deviation from NSR
A sinus rate of less than 60/min

Causes of Sinus Bradycardia
•
MI
• Sinus node disease (sick sinus syndrome)
• Hypothermia
• Hypothyroidism
• Cholestatic jaundice
• Raised intracranial pressure
• Drugs, e.g. β-blockers, digoxin, verap

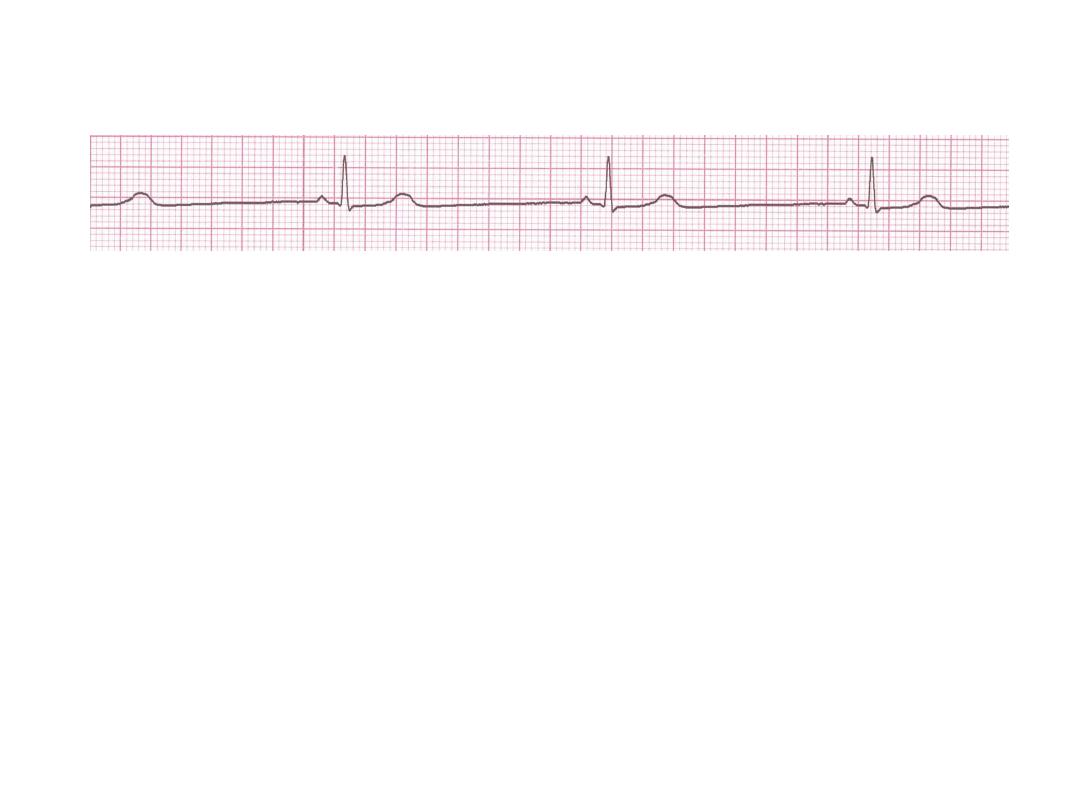
Rhythm
30 bpm
• Rate?
• Regularity?
regular
normal
0.10 s
• P waves?
• PR interval?
0.12 s
• QRS duration?
Interpretation?
Sinus Bradycardia
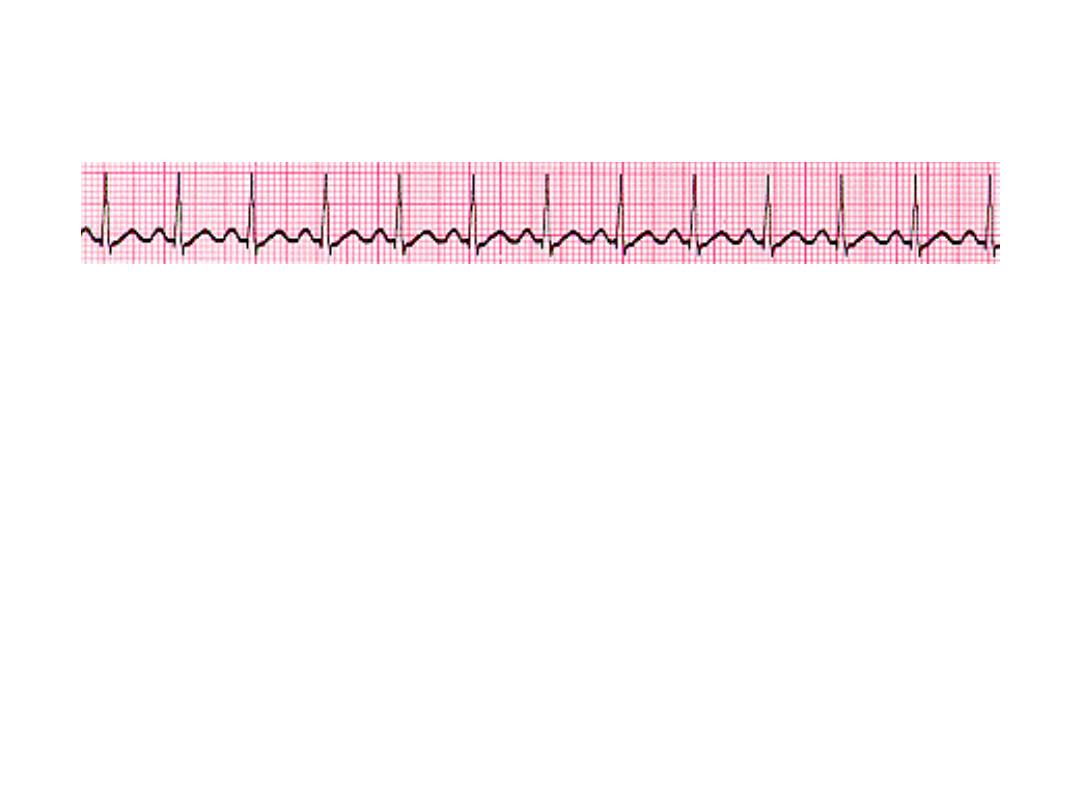
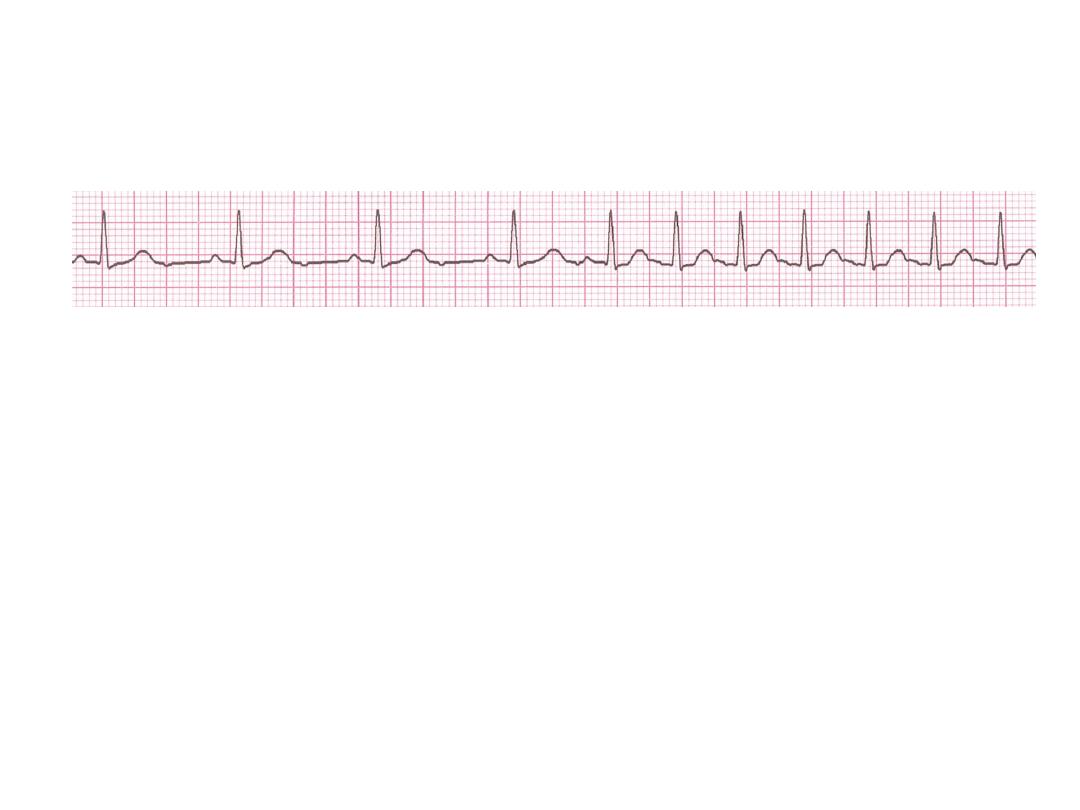
Sinus Tachycardia
• Deviation from NSR
-
a sinus rate of more than 100/min

Causes of Sinus Tachycardia
* Anxiety
• Fever
• Anaemia
• Heart failure
• Thyrotoxicosis
• Phaeochromocytoma
• Drugs, e.g. β-agonists (bronchodilators)
Rhythm
130 bpm
• Rate?
• Regularity?
regular
normal
0.08 s
• P waves?
• PR interval?
0.16 s
• QRS duration?
Interpretation?
Sinus Tachycardia

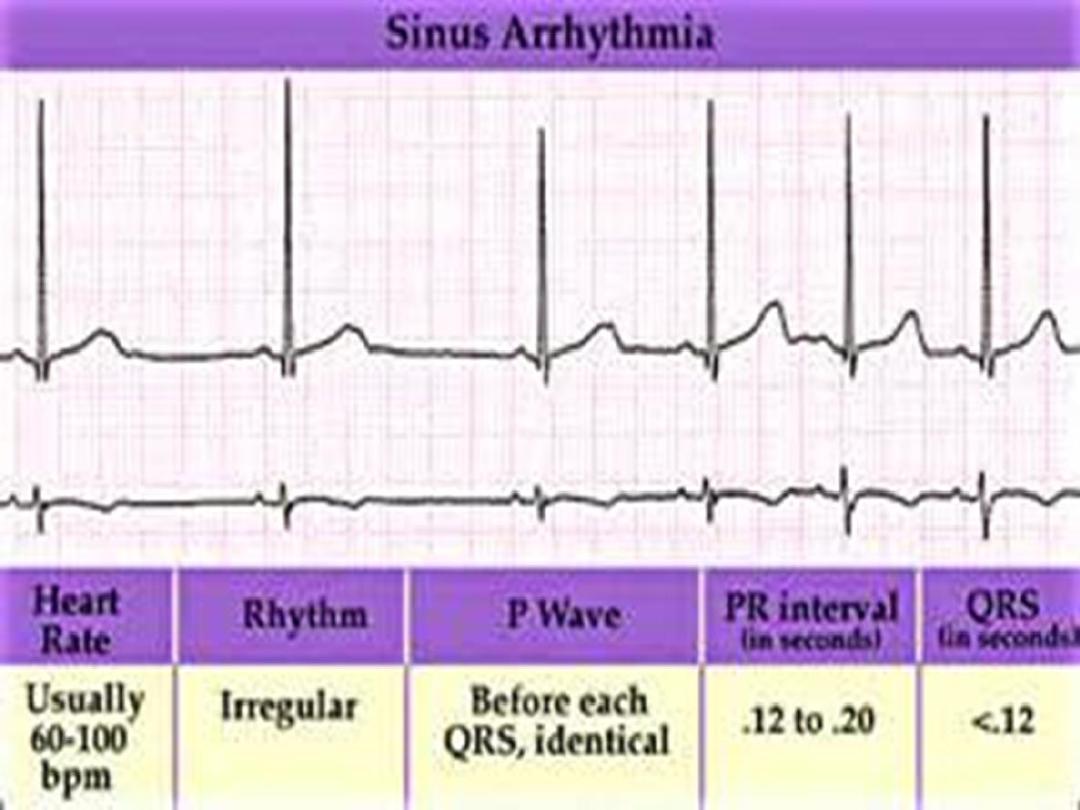
Sinus arrhythmia
• Phasic alteration of the heart rate during
respiration (the sinus rate increases during
inspiration and slows during expiration
For more presentations
www.medicalppt.blogspot.com
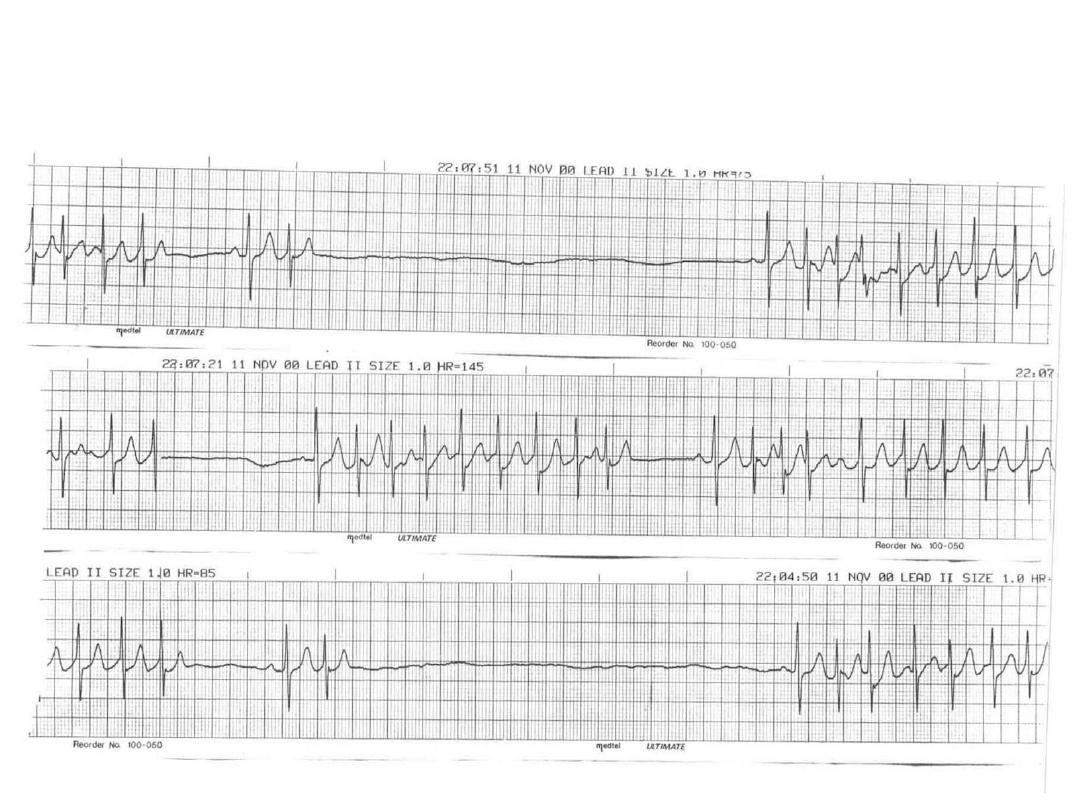
Sick Sinus Syndrome(SSS)

Supraventricular Arrhythmias
•
Atrial Fibrillation
•
Atrial Flutter
•
Paroxysmal Supraventricular Tachycardia

Premature Beats
•
Premature Atrial Contractions
(PACs)
•
Premature Ventricular Contractions
(PVCs)
Premature Atrial Contractions
• Deviation from NSR
– These ectopic beats originate in the atria
(but not in the SA node), therefore the
contour of the P wave, the PR interval, and
the timing are different than a normally
generated pulse from the SA node.

Atrial Fibrillation
• The most common sustained cardiac arrhythmia.
• AF can cause palpitation, breathlessness and fatigue. In
patients with poor ventricular function or valve disease, it
may precipitate or aggravate cardiac failure.
• AF is associated with significant morbidity (
Thromboembolic )and a twofold increase in mortality .
• AF can be classified as paroxysmal (intermittent episodes
which self-terminate within 7 days),
persistent
(prolonged
episodes that can be terminated by electrical or chemical
cardioversion) or permanent.
Common causes of atrial fibrillation
• Coronary artery disease (including acute MI)
• Valvular heart disease, especially rheumatic mitral valve
disease
• Hypertension
• Sinoatrial disease
• Hyperthyroidism
• Alcohol • Cardiomyopathy
• Congenital heart disease
• Chest infection
• Pulmonary embolism
• Pericardial disease
• Idiopathic (lone atrial fibrillation)

Atrial Fibrillation
• Deviation from NSR
– No organized atrial depolarization, so no
normal P waves (impulses are not
originating from the sinus node).
– Atrial activity is chaotic (resulting in an
irregularly irregular rate).
– Common, affects 2-4%, up to 5-10% if > 80
years old
AF
Management
• Rhythm control
• Pharmacologic cardioversion Flecainide
,Propafenon,Amiodaron
• Electrical cardioversion
- Less than 48 hours direct cardioversion.
- More than 48 hours +Anticoagulates for 4 weeks prior
and 3 months after.
Rate control
• Using Digoxin, β-blockers and calcium antagonists, such as
verapamil or diltiazem
• Catheter ablation in refractory cases

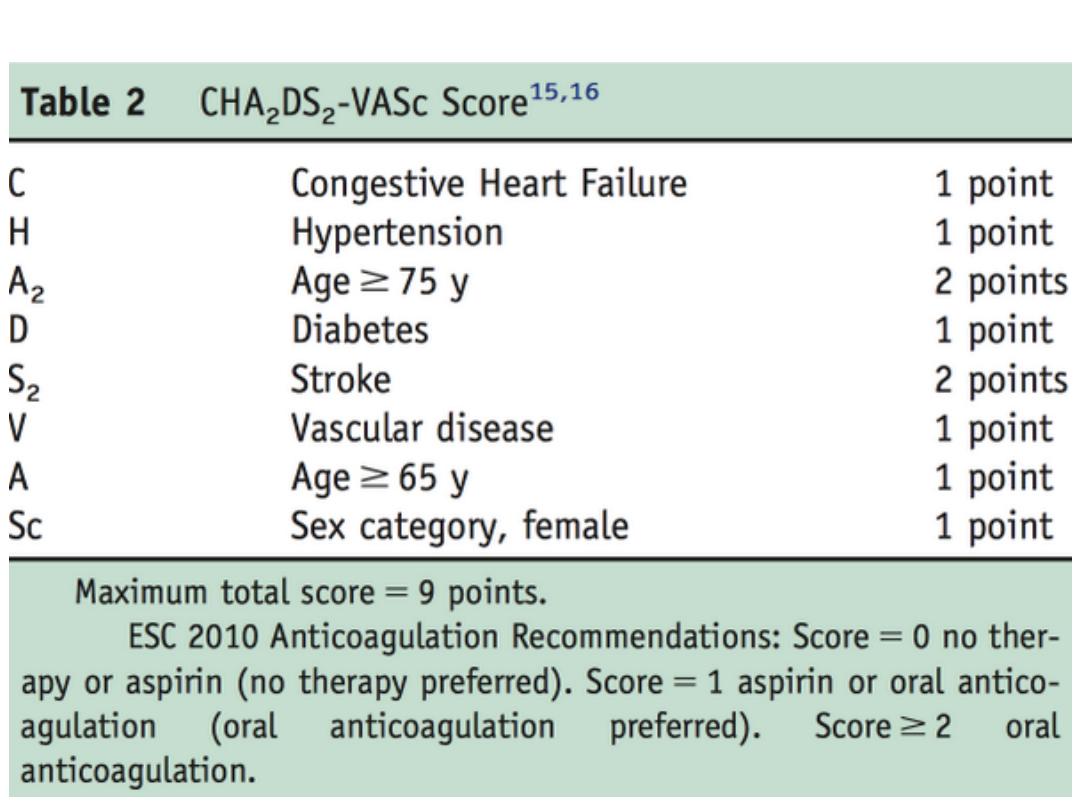
Prevention of thromboembolism
• Risk stratification is based on clinical factors
using the CHA2DS2-VASc scoring system.
• Warfarin INR 2-3
• Aspirin
Atrial Flutter
• Etiology:
a large (macro) re-entry circuit,
usually within the right atrium encircling the
tricuspid annulus with every 2nd, 3rd or 4th
impulse generating a QRS (others are blocked
in the AV node as the node repolarizes).

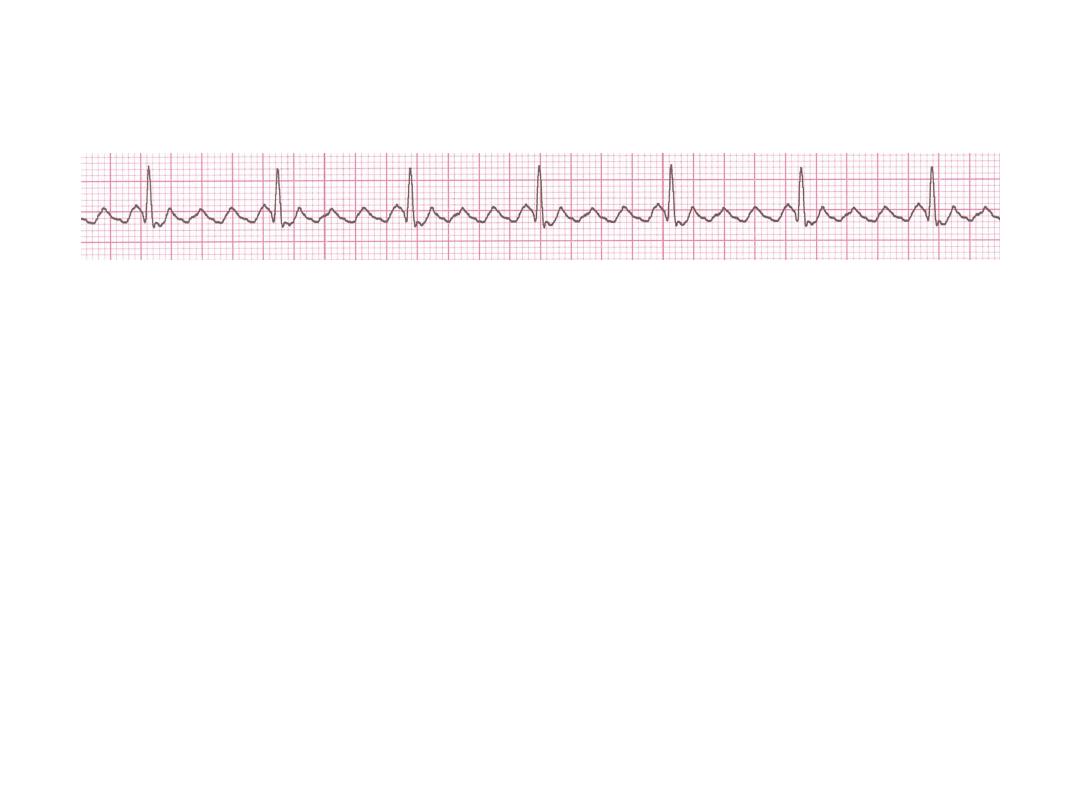
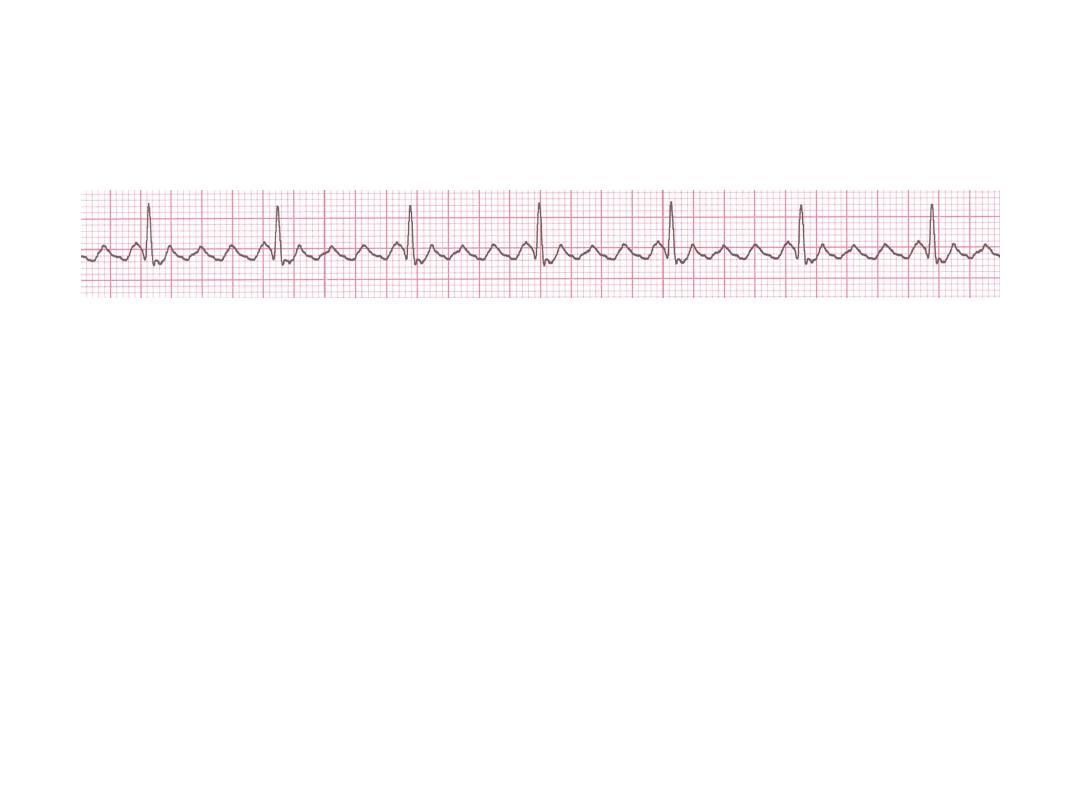
Atrial Flutter
• Deviation from NSR
– No P waves. Instead flutter waves (note
“sawtooth” pattern) are formed at a rate of
250 - 350 bpm.
– Only some impulses conduct through the
AV node (usually every other impulse)
Atrial F
70 bpm
• Rate?
• Regularity?
regular
flutter waves
0.06 s
• P waves?
• PR interval?
none
• QRS duration?
Interpretation?
Atrial Flutter
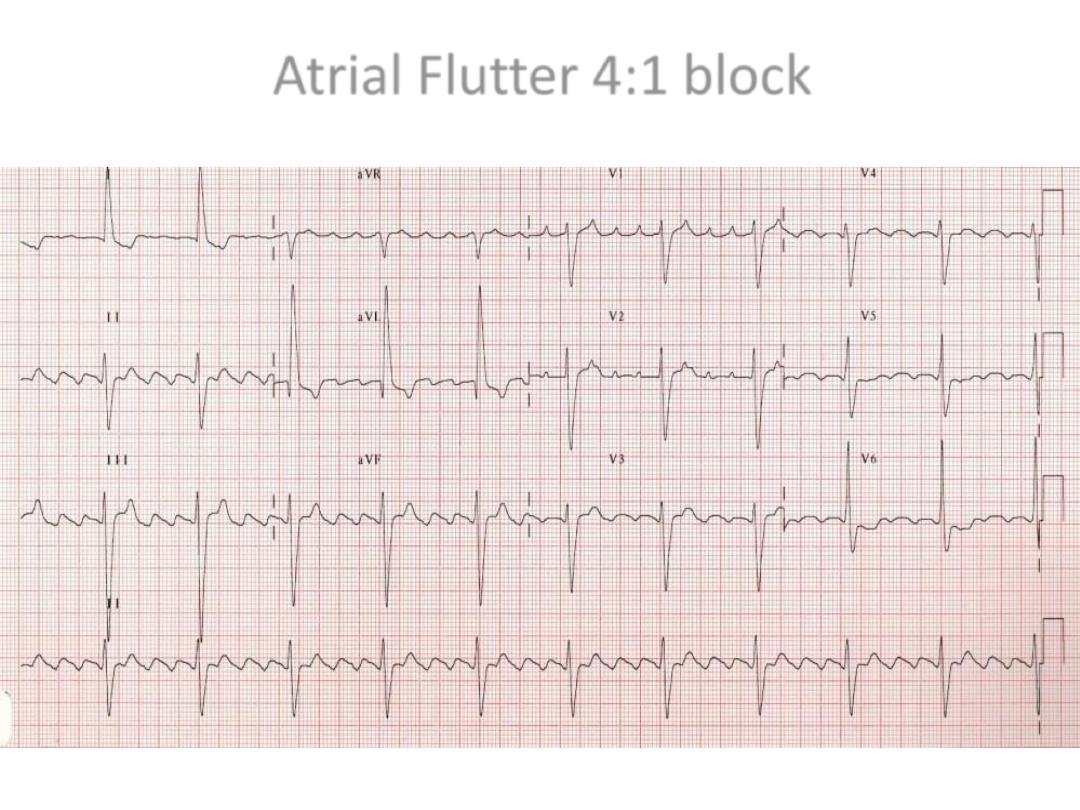
Atrial Flutter 4:1 block

Causes and Symptoms
• Similar to atrial fibrillation
• Management
• Treat the cause
• Rate control -Digoxine B blocker,verapamil.
• Rhythm control –Amiodaron ,DC
• Maintanance B- Blocker or amiodarone
• Anticoagulant
• Catheter ablation offers a 90% chance of complete cure and is
the treatment of choice for patients with persistent symptoms
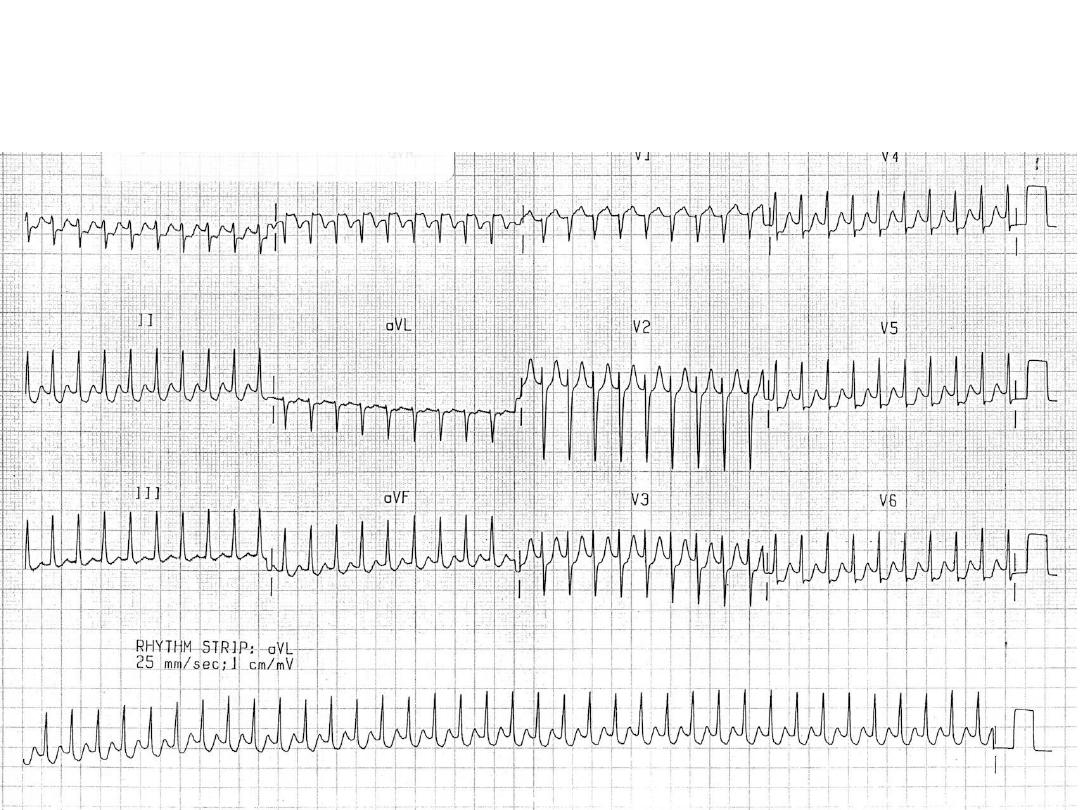
Paroxysmal Supraventricular
Tachycardia (PSVT)
• Deviation from NSR
– The heart rate suddenly speeds up, often
triggered by a PAC (not seen here) and the
P waves are lost.
– Tends to occur in normal heart.
PSVT
• Etiology:
There are several types of PSVT but all
originate above the ventricles (therefore the
QRS is narrow).
• Most common: abnormal conduction in the AV
node (reentrant circuit looping in the AV node).
• Rate 150-250
PSVT
For more presentations
www.medicalppt.blogspot.com

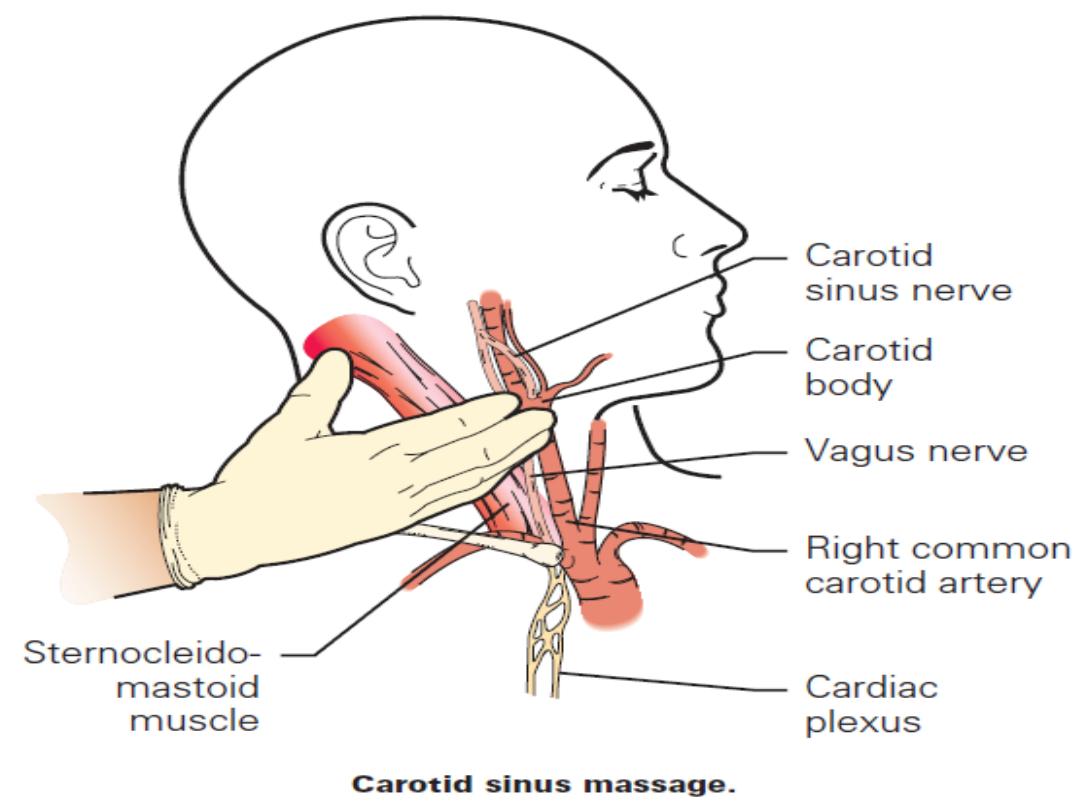
Management
• If pt is hemodynamically unstable( systolic
Bp<90mmhg, had chest pain, impaired sensorium or
pulmonary
oedema)
arrhythemia
should
be
terminated by synchronus DC cardioversion
• Episode may be terminated by carotid sinus pressure
or by the Valsalva manœuvre. Adenosine (3–12 mg
rapidly IV in incremental doses until tachycardia
stops) or verapamil (5 mg IV)
• Recurrent SVT, catheter ablation is the most effective
therapy and will permanently prevent SVT in more
than 90% of cases
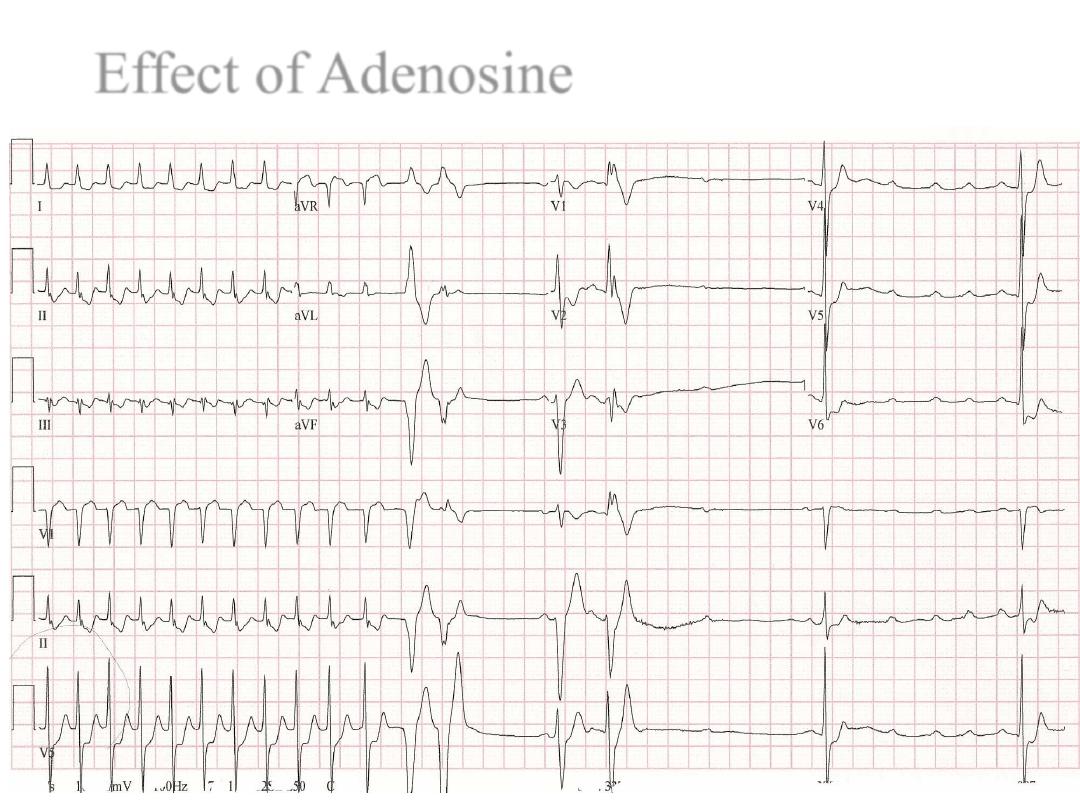
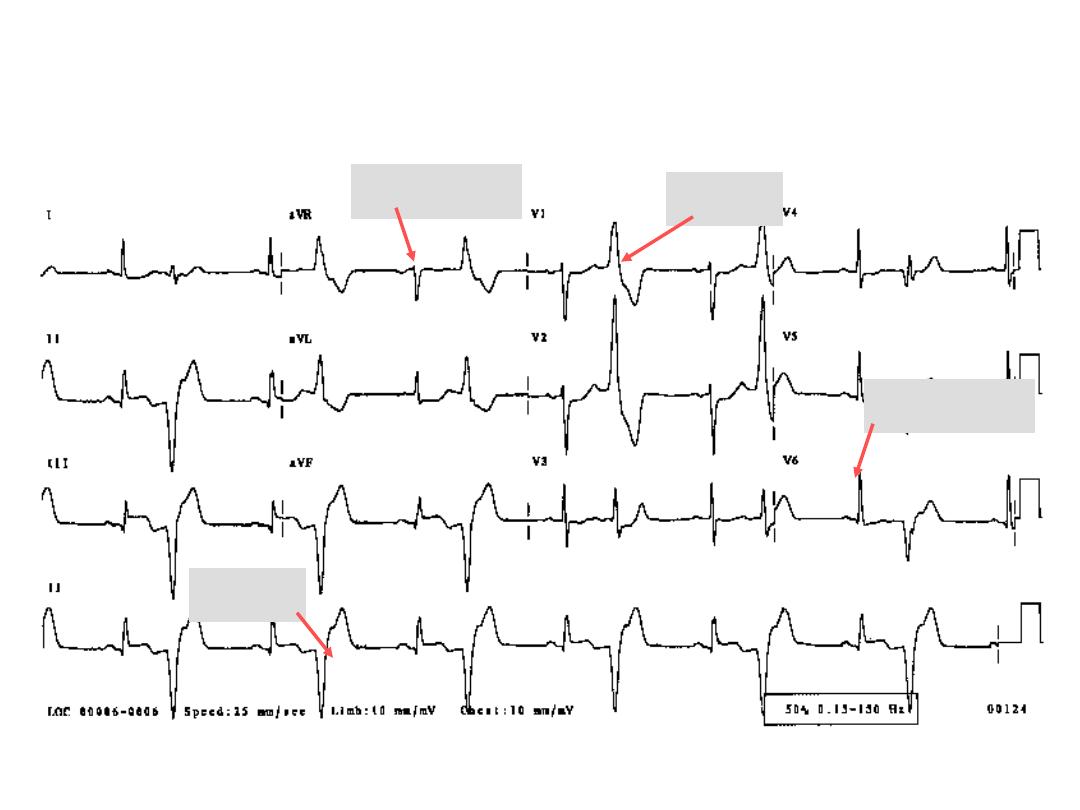
Effect of Adenosine
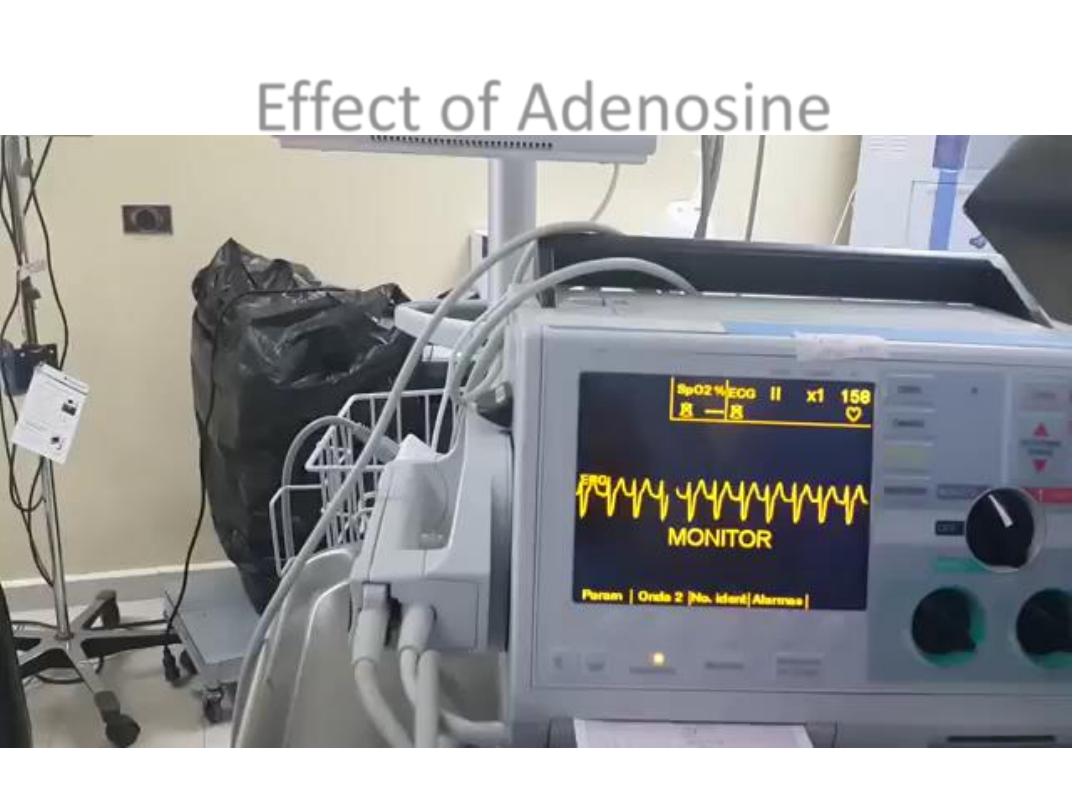
Effect of Adenosine
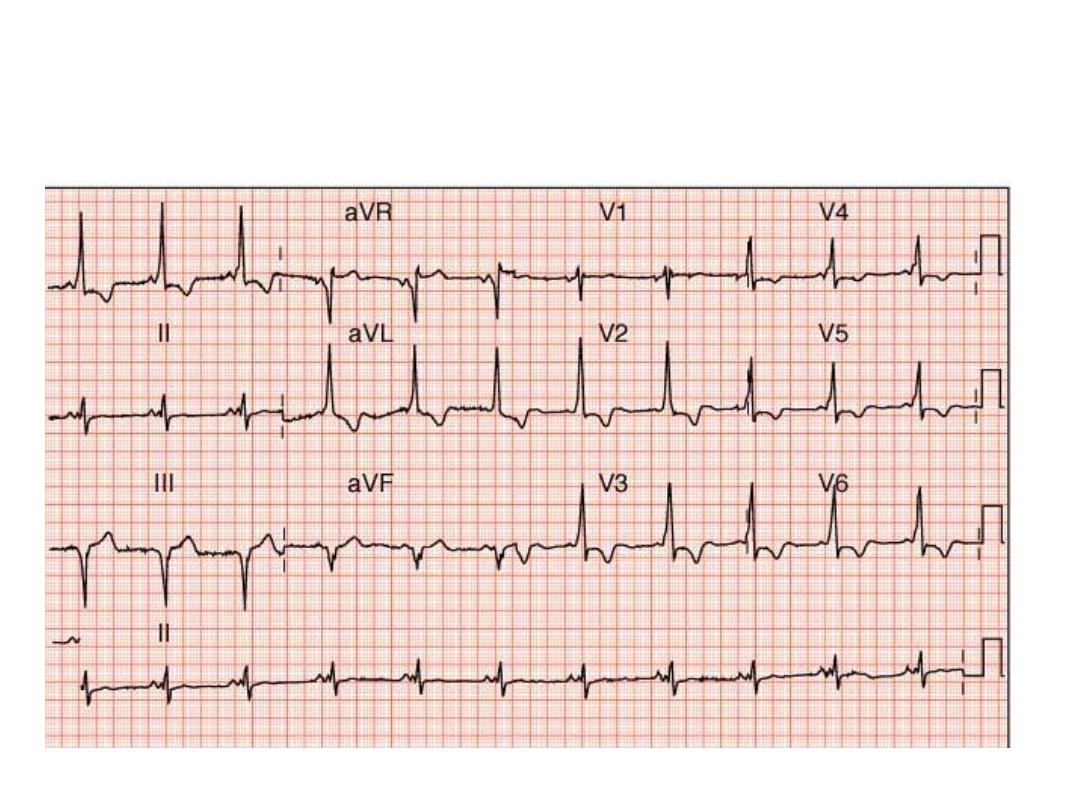
WPW Syndrome
Ventricular Arrhythmias
•
Premature Ventricular Contractions
•
Ventricular Tachycardia
•
Ventricular Fibrillation
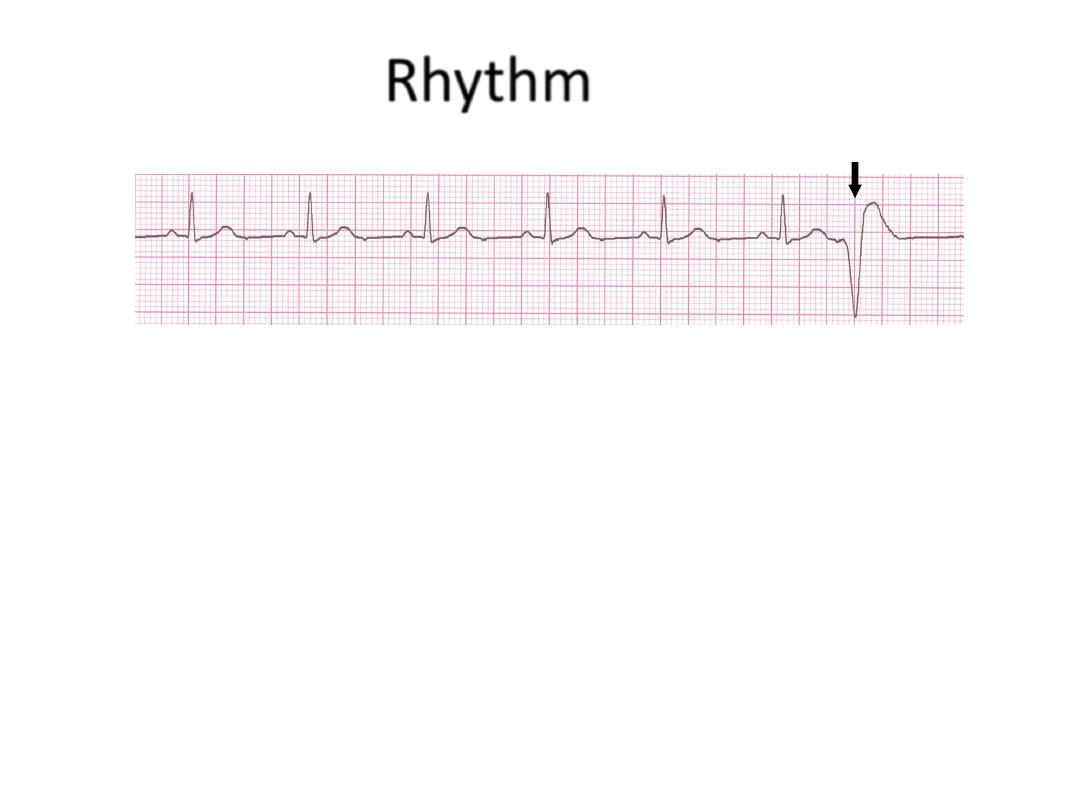
Rhythm
60 bpm
• Rate?
• Regularity?
occasionally irreg.
none for 7
th
QRS
0.08 s (7th wide)
• P waves?
• PR interval?
0.14 s
• QRS duration?
Interpretation?
Sinus Rhythm with 1 PVC
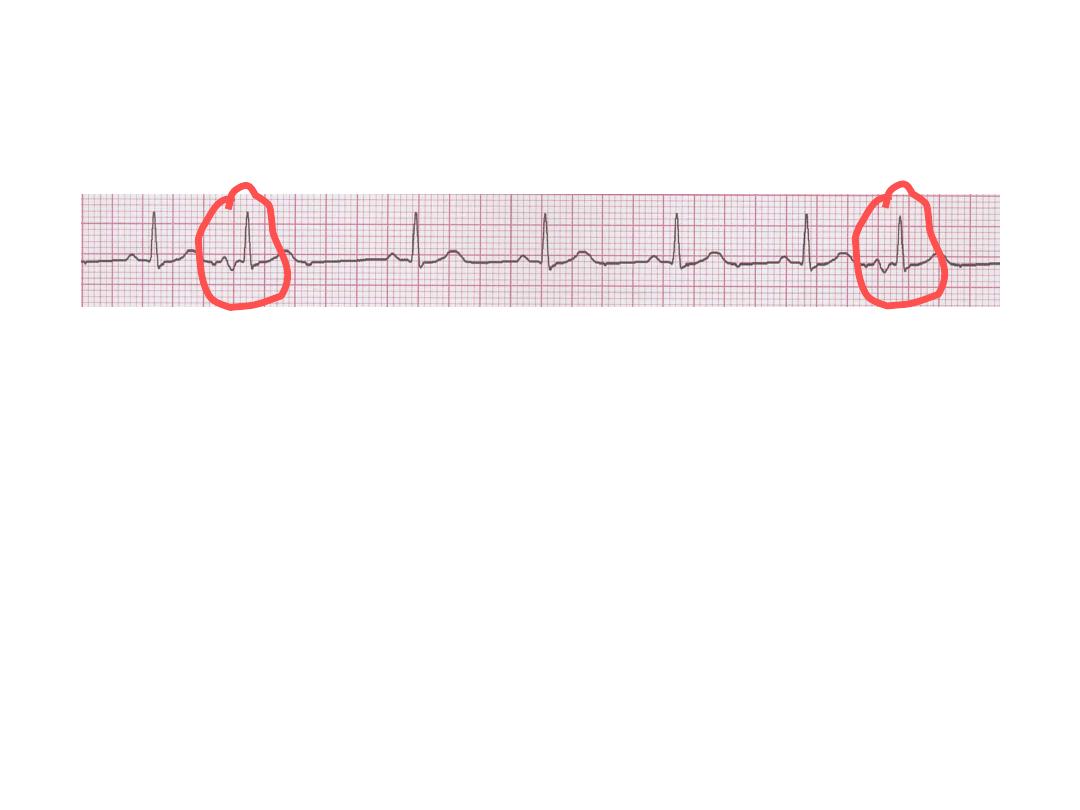
Ventricular Bigeminy
44
Normal
VPC
VPC
Normal

Ventricular Tachycardia
• Dangerous.
• Nearly in abnormal heart.
• 3 or more successive PVC at rate of more than
120.
• Can occur in normal heart.
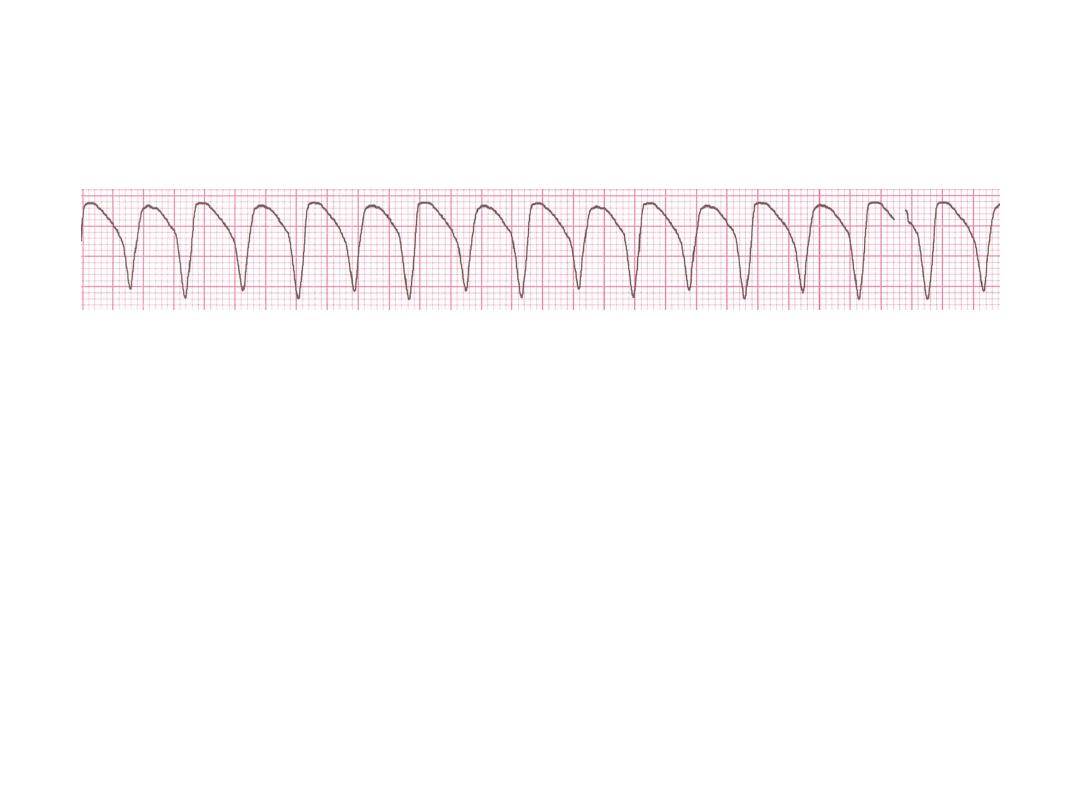
Ventricular Tachycardia
• Deviation from NSR
– Impulse is originating in the ventricles (no
P waves, wide QRS).
Ventricular Tachycardia
• Etiology:
There is a re-entrant pathway looping
in a ventricle (most common cause).
• Ventricular tachycardia (VT) occurs most
commonly in the settings of acute MI, chronic
coronary artery disease, and cardiomyopathy.
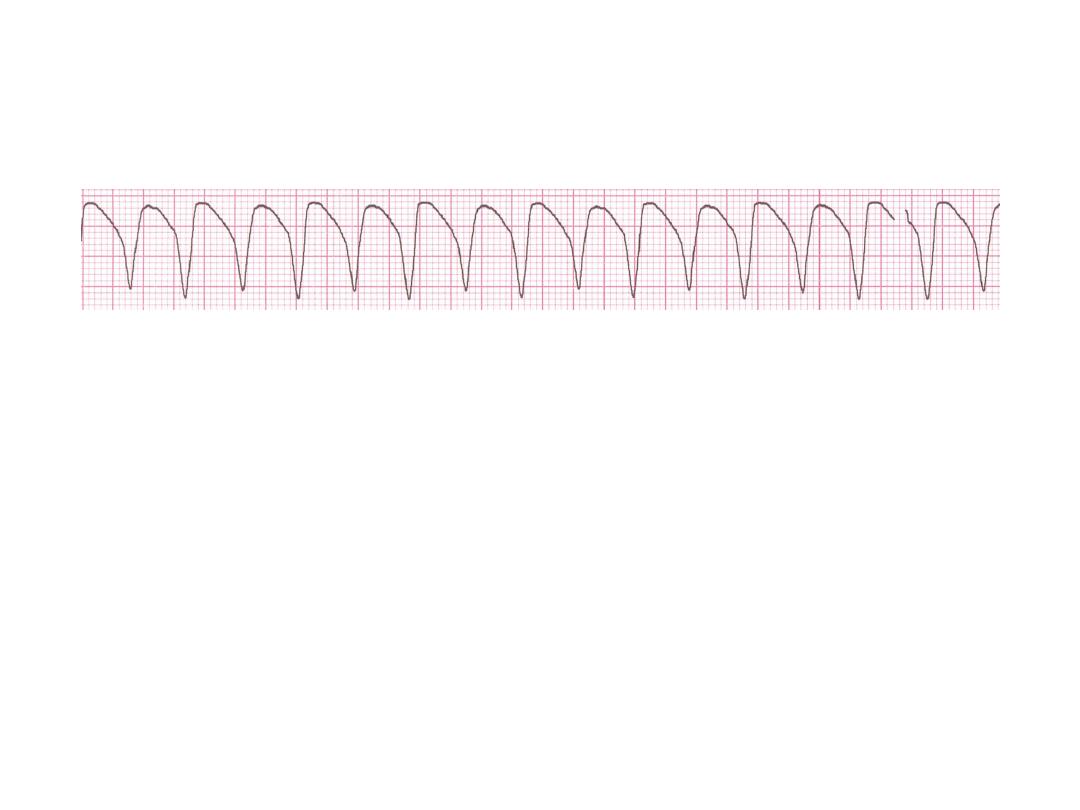
Rhythm
160 bpm
• Rate?
• Regularity?
regular
none
wide (> 0.12 sec)
• P waves?
• PR interval?
none
• QRS duration?
Interpretation?
Ventricular Tachycardia
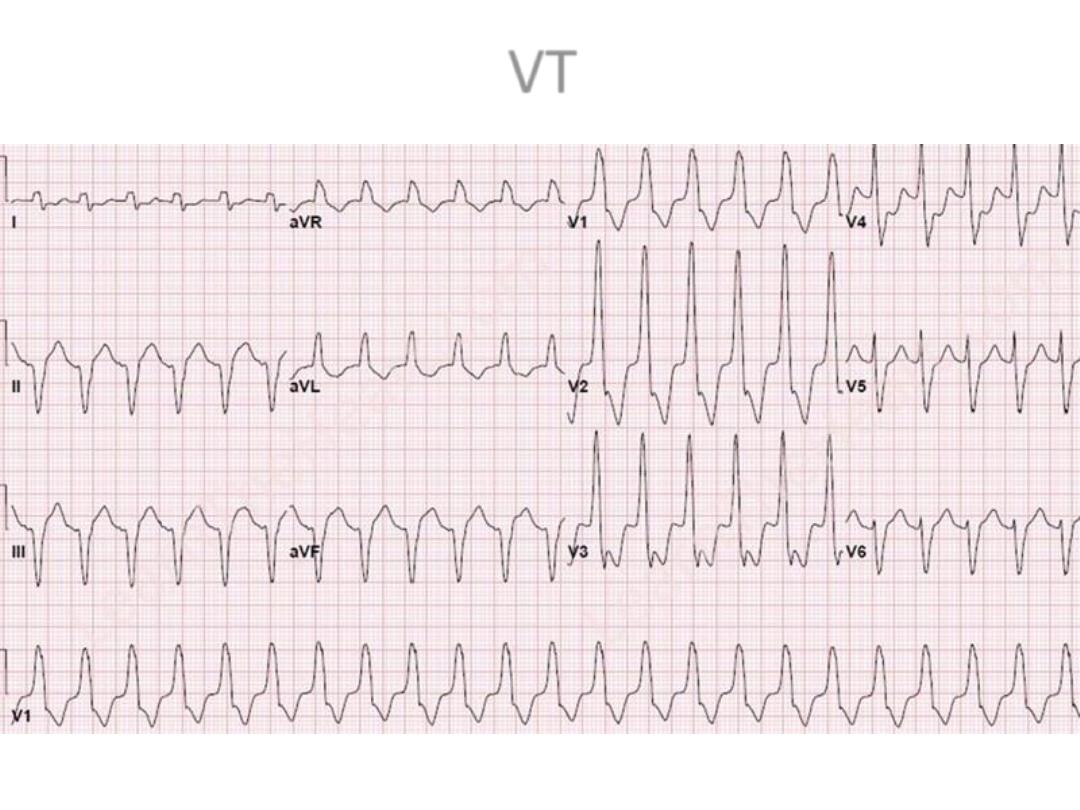
VT
Management
• Treat cause.
• Hemodynamically unstable DC
• Stable IV amiodarone or lidocaine.
• With poor LV function indication for ICD
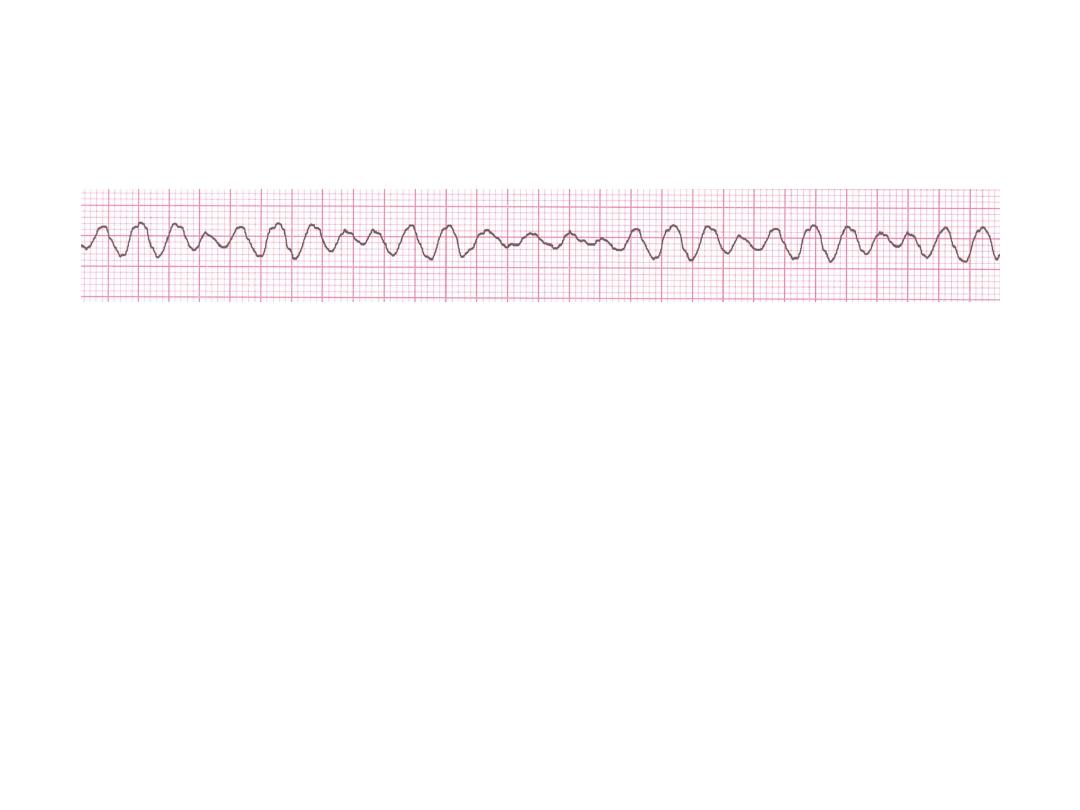
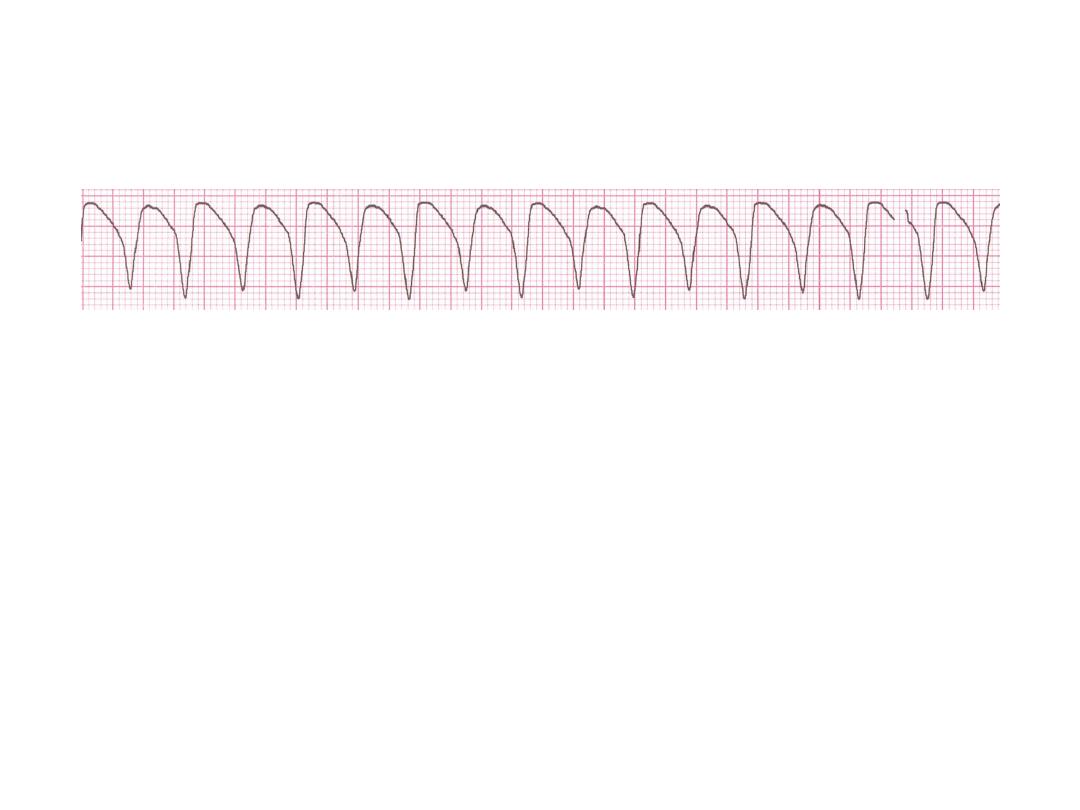
Ventricular Fibrillation
• Deviation from NSR
– Completely abnormal.
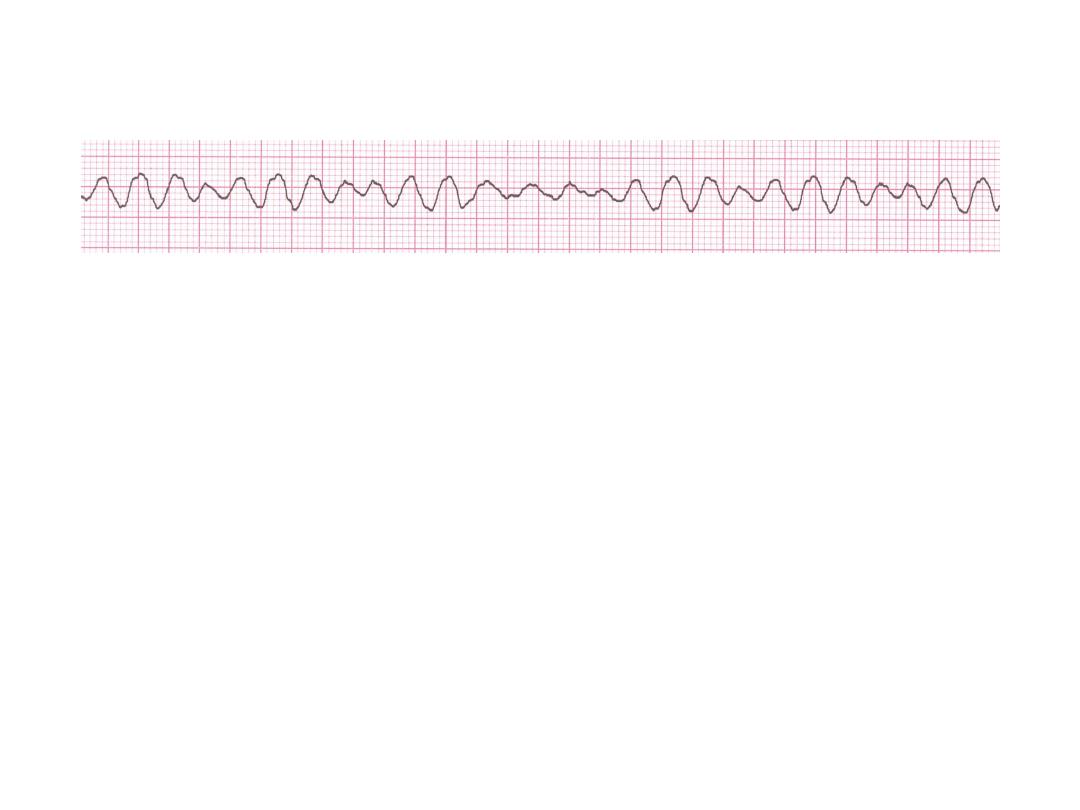
Ventricular Fibrillation
• Etiology:
The ventricular cells are excitable
and depolarizing randomly.
• Rapid drop in cardiac output and death occurs
if not quickly reversed
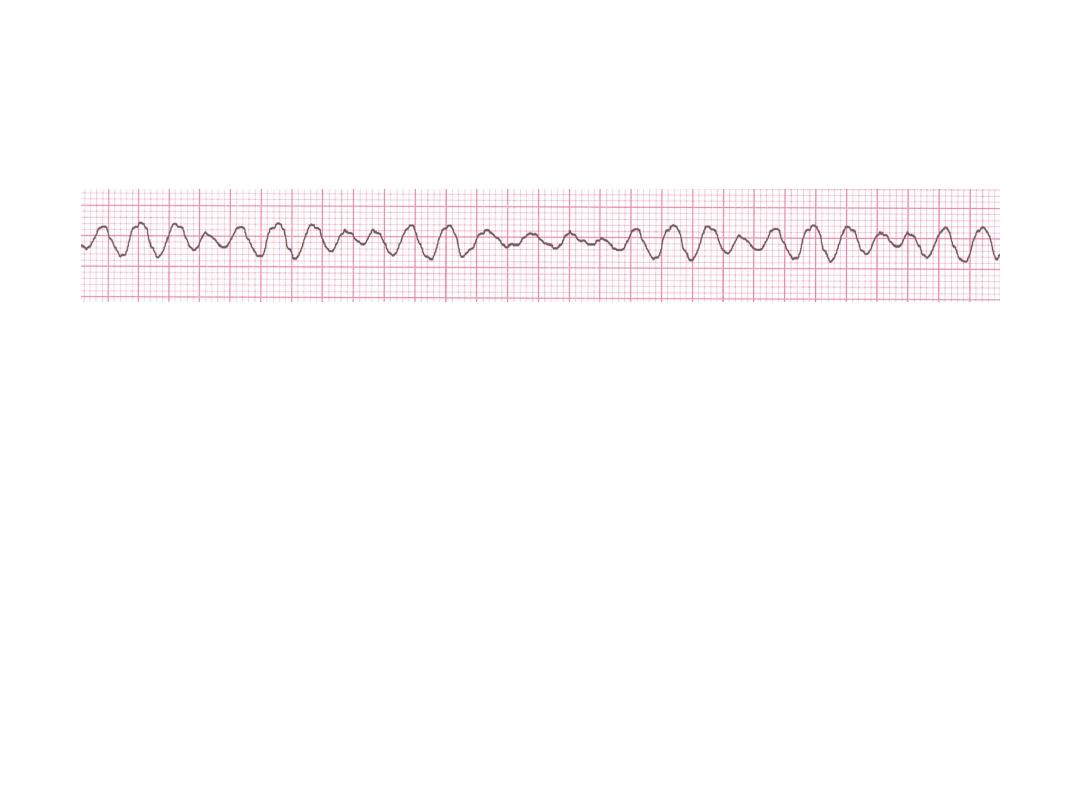
Rhythm
none
• Rate?
• Regularity?
irregularly irreg.
none
wide, if recognizable
• P waves?
• PR interval?
none
• QRS duration?
Interpretation?
Ventricular Fibrillation

Management
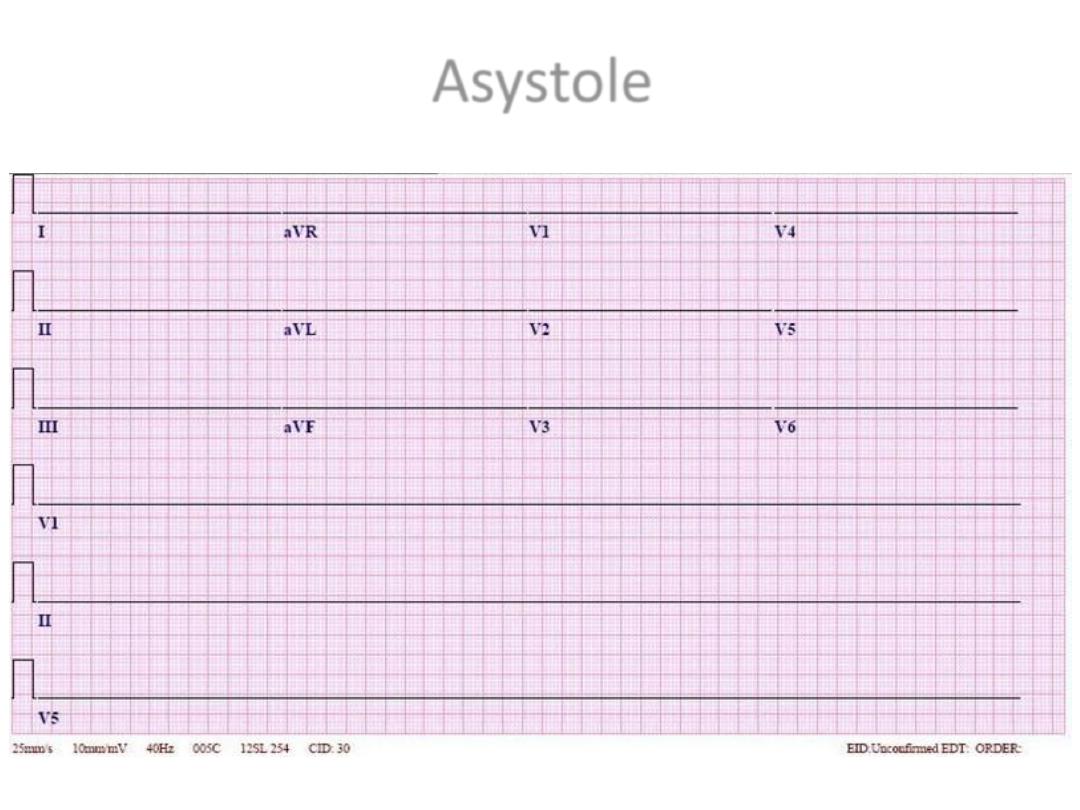
Asystole
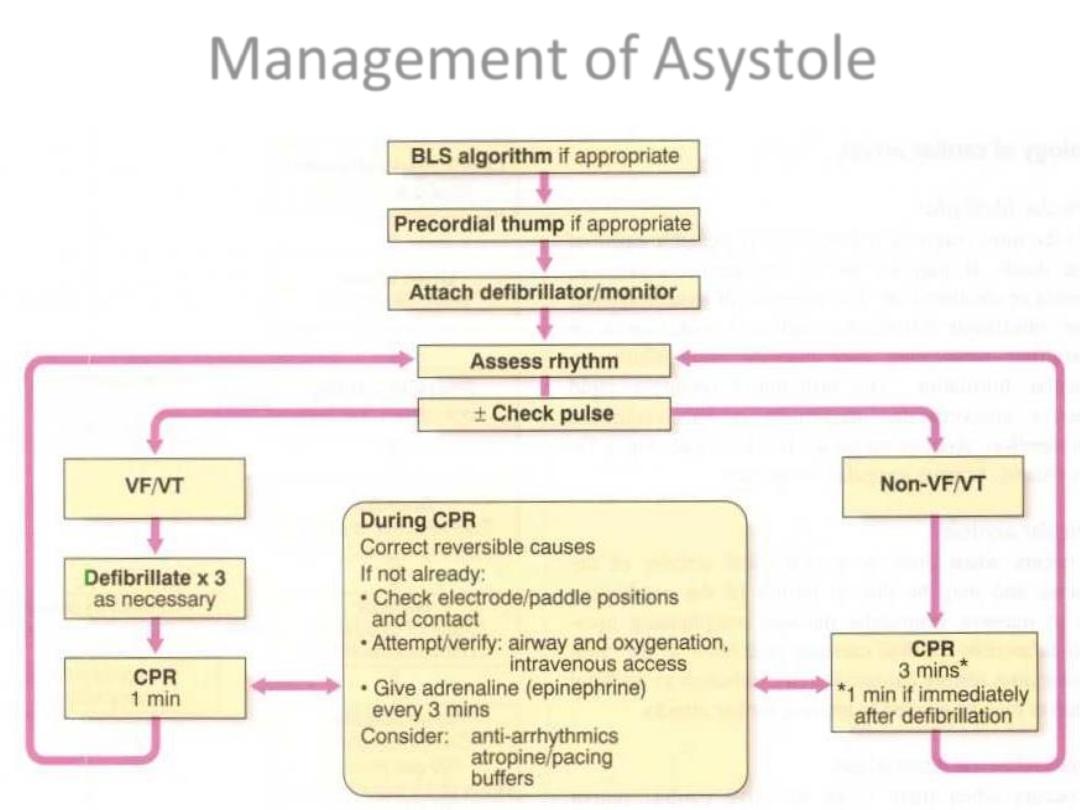
Management of Asystole
AV Nodal Blocks
•
1st Degree AV Block
•
2nd Degree AV Block, Type I
•
2nd Degree AV Block, Type II
•
3rd Degree AV Block
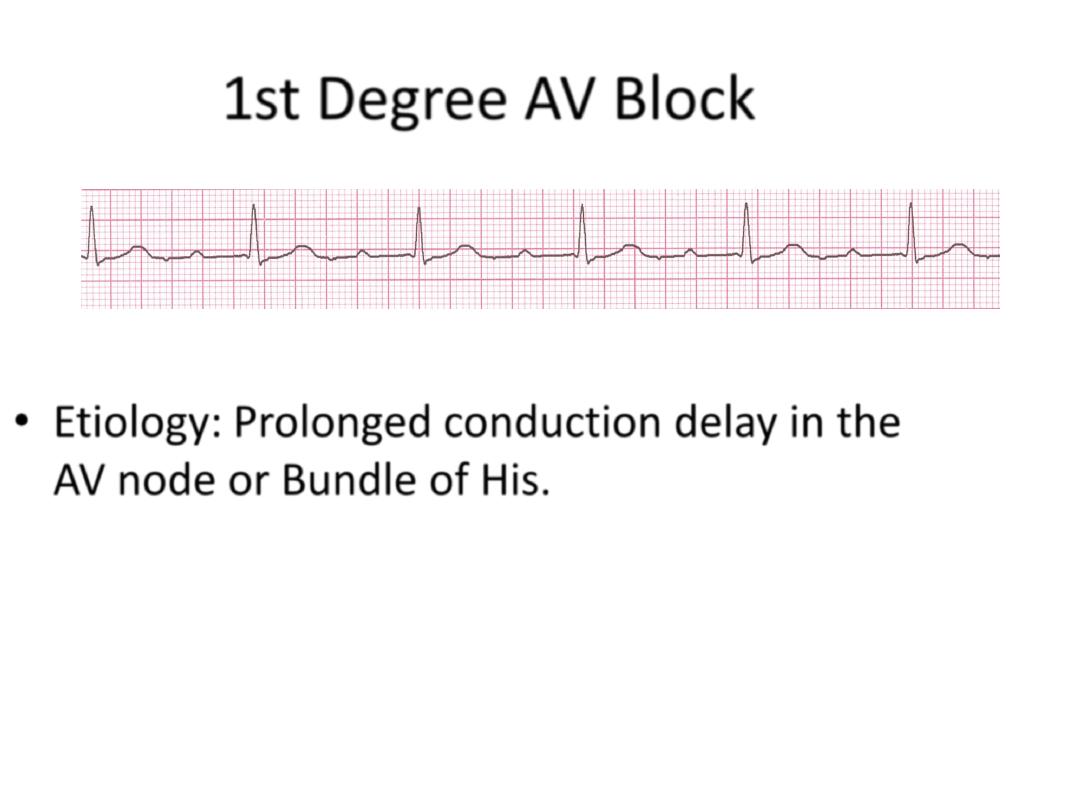
1st Degree AV Block
• Etiology:
Prolonged conduction delay in the
AV node or Bundle of His.
Rhythm
60 bpm
• Rate?
• Regularity?
regular
normal
0.08 s
• P waves?
• PR interval?
0.36 s
• QRS duration?
Interpretation?
1st Degree AV Block
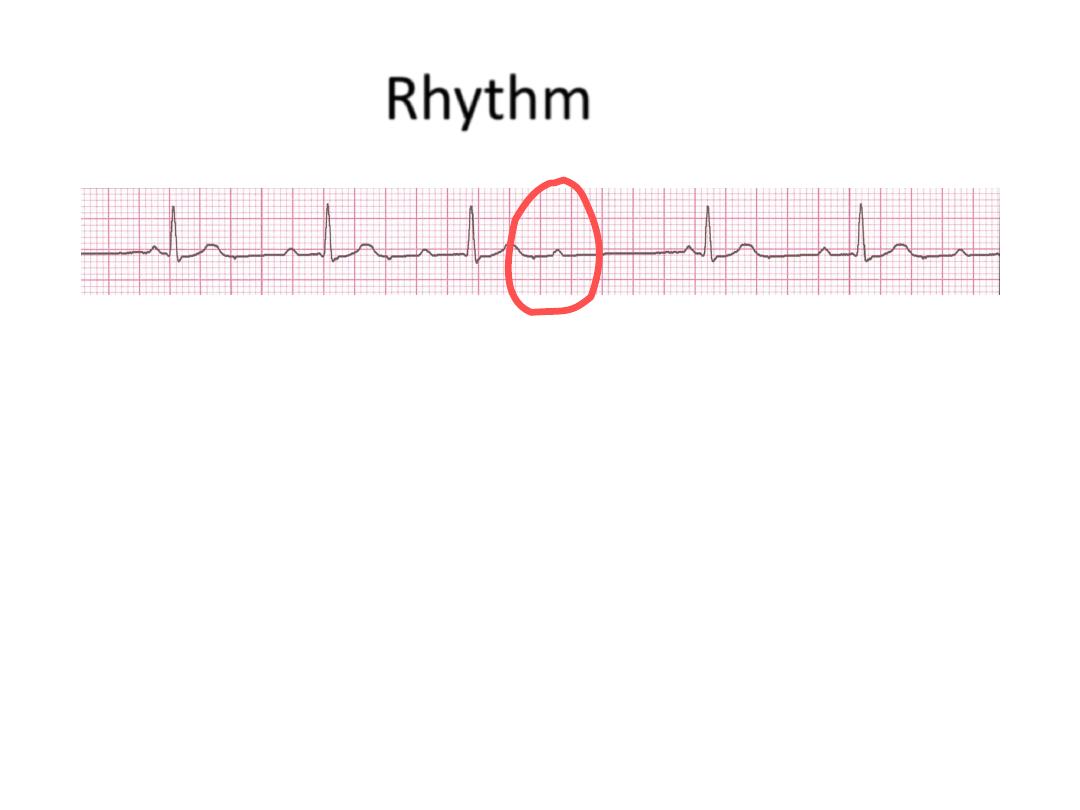
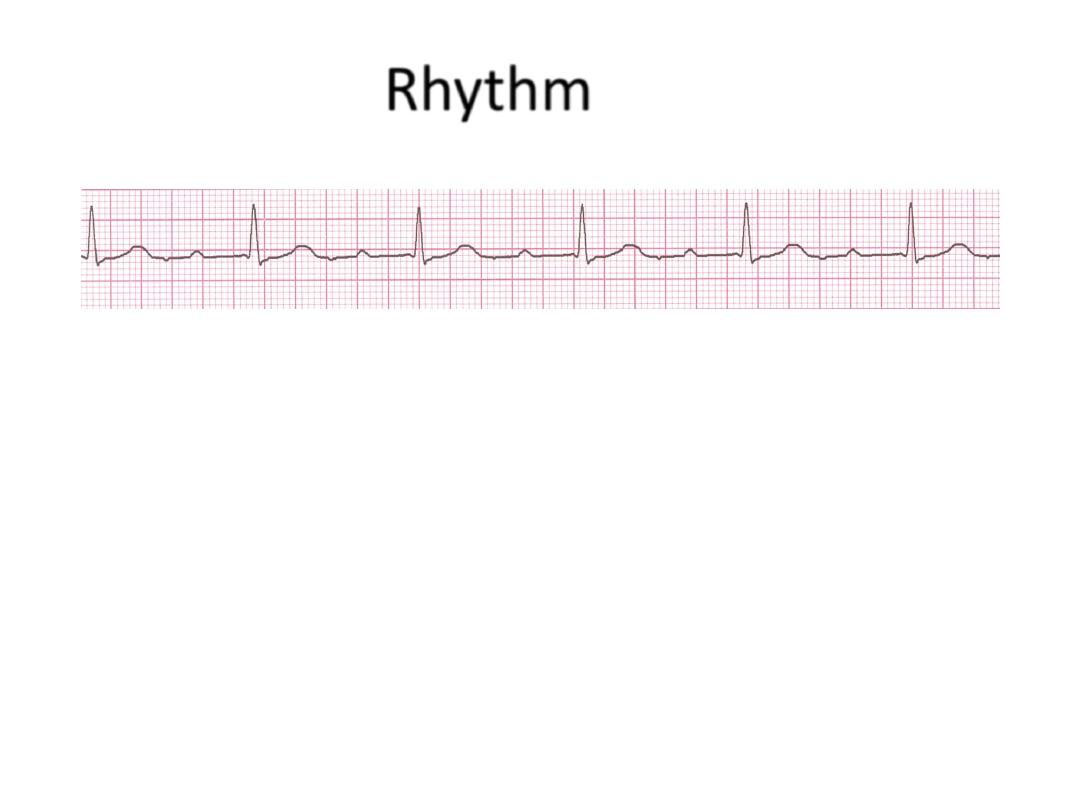
Rhythm
50 bpm
• Rate?
• Regularity?
regularly irregular
nl, but 4th no QRS
0.08 s
• P waves?
• PR interval?
lengthens
• QRS duration?
Interpretation?
2nd Degree AV Block, Type I
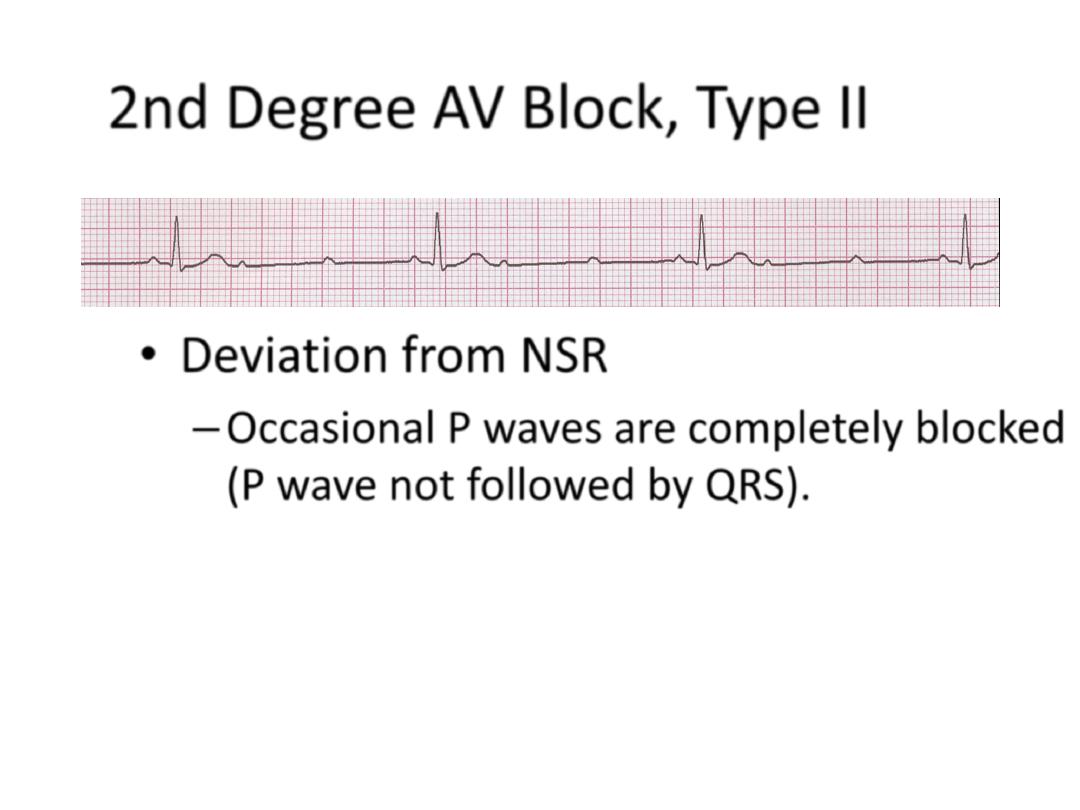
2nd Degree AV Block, Type II
• Deviation from NSR
– Occasional P waves are completely blocked
(P wave not followed by QRS).
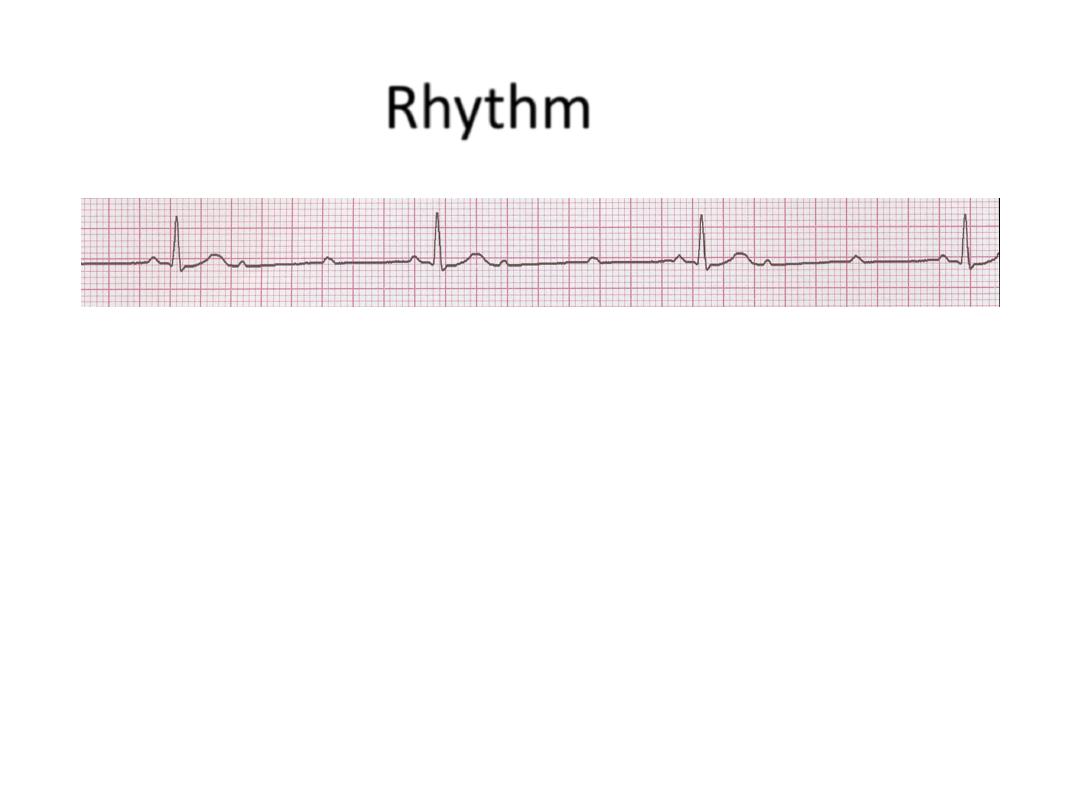
Rhythm
40 bpm
• Rate?
• Regularity?
regular
nl, 2 of 3 no QRS
0.08 s
• P waves?
• PR interval?
0.14 s
• QRS duration?
Interpretation?
2nd Degree AV Block, Type II
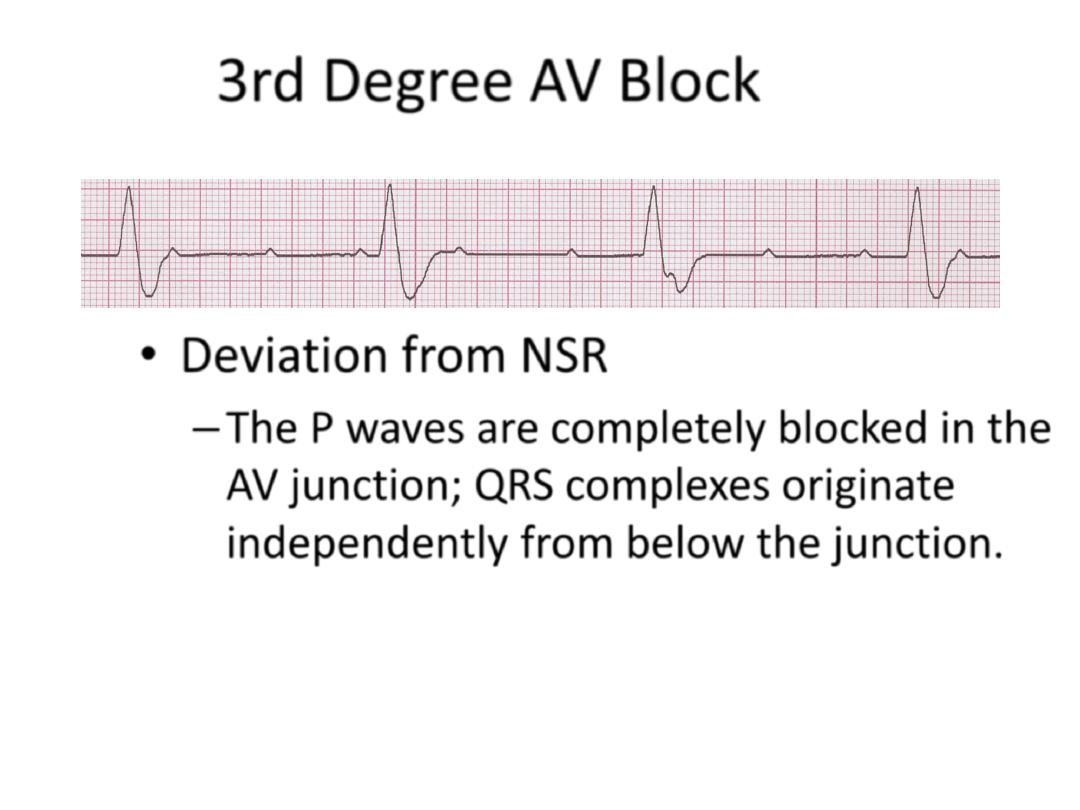
3rd Degree AV Block
• Deviation from NSR
– The P waves are completely blocked in the
AV junction; QRS complexes originate
independently from below the junction.
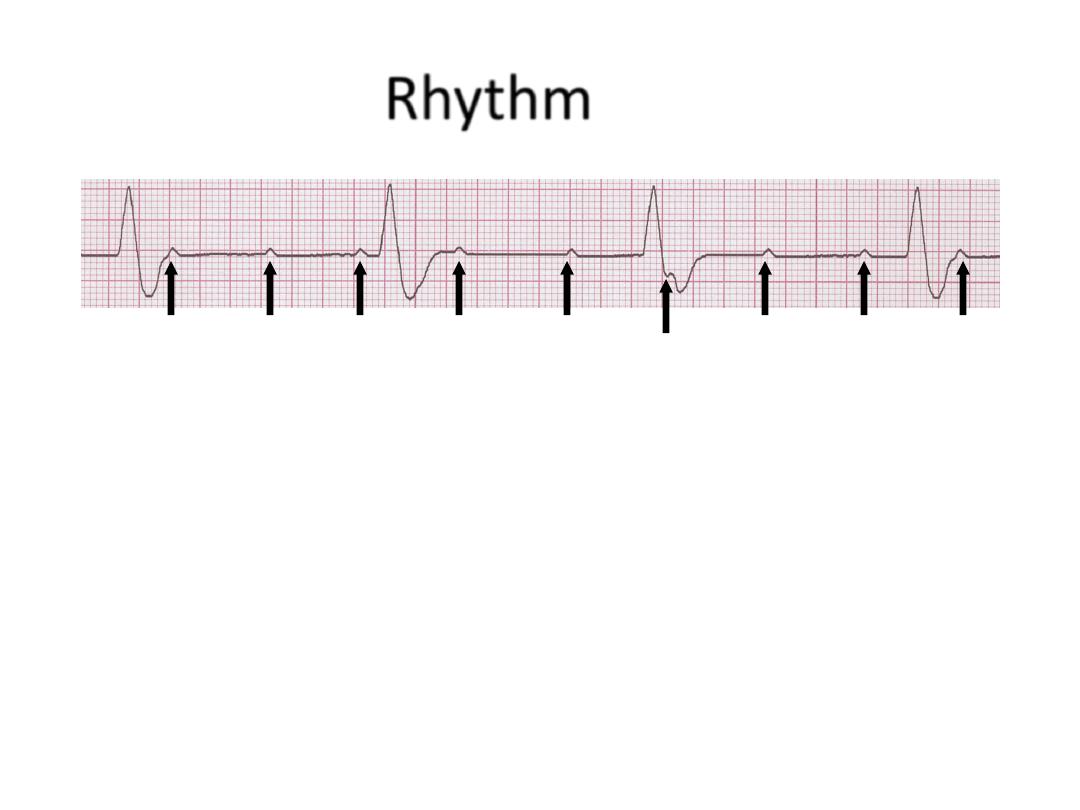
Rhythm
40 bpm
• Rate?
• Regularity?
regular
no relation to QRS
wide (> 0.12 s)
• P waves?
• PR interval?
none
• QRS duration?
Interpretation?
3rd Degree AV Block
Management of symptomatic heart block

Bundle branch block and hemiblock
• Left bundle branch block LBBB
• Right bundle branch block RBBB
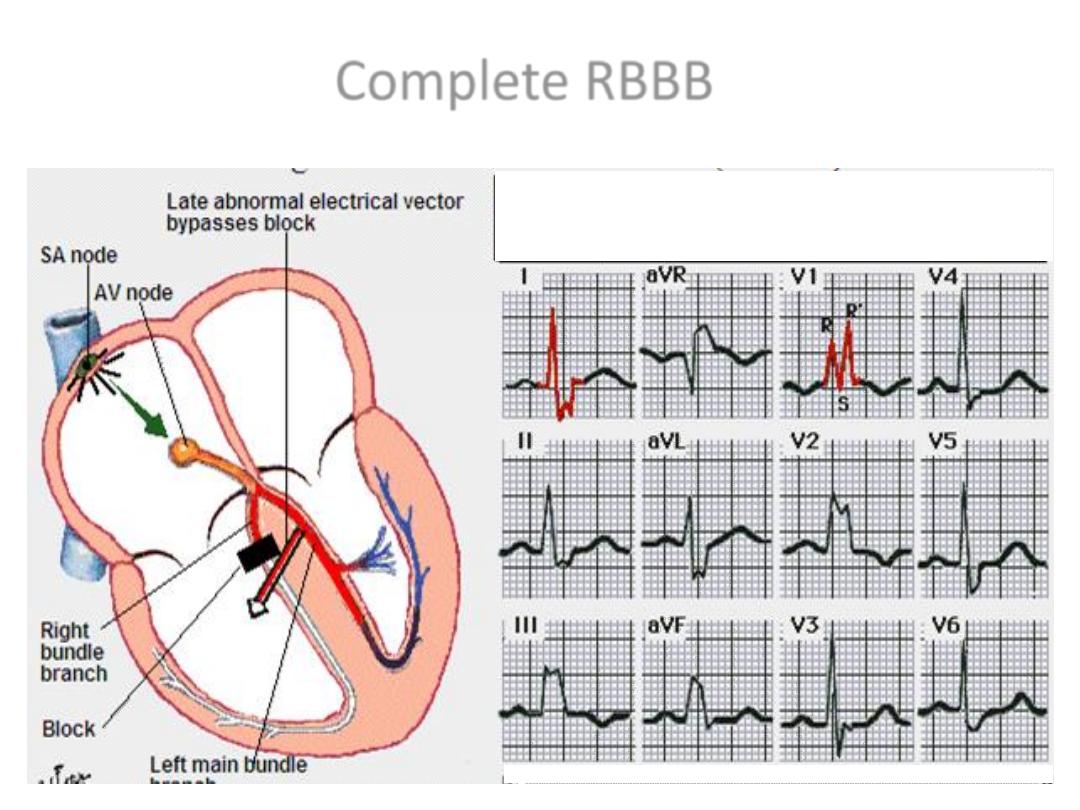
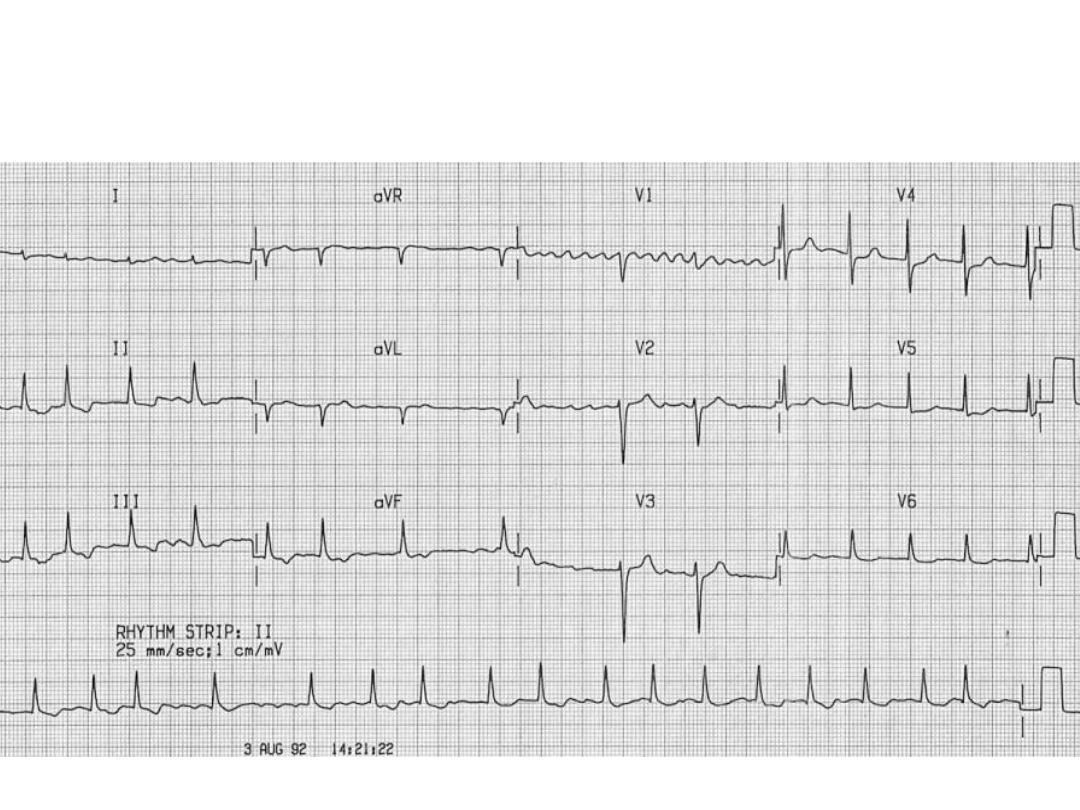
Complete RBBB
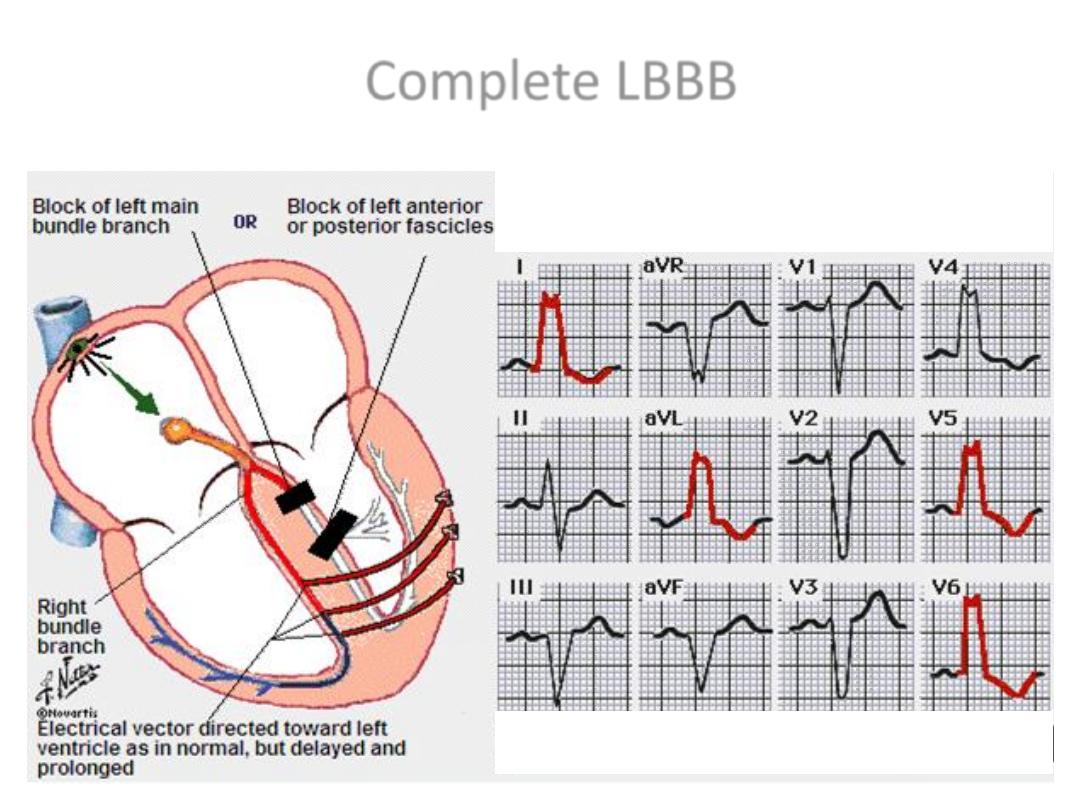
Complete LBBB
68
