PROM
Premature Rupture of the Membrane; PROM:Defined as :rupture of the membrane before the onset of spontaneous uterine activity.
Incidence is 10% in pregnancies (majority)
Preterm premature rupture of the membrane (PPROM): if PROM occurs before 37 completed weeks.
Incidence is 2% of pregnancies.
Risk of PROM:
Maternal :Infection:chorioaminionitis,rarely systemic infection.
Abruptio placentae
Induction of labour .
Operative delivery.
PPH.
Smoking
Body mass index (BMI) <20
Fetal risk:
Prematurity,75% will deliver with in 2 weeks.
Neonatal sepsis.
Oligohydramnios.
Hypoxia: cord prolapse and copmression.
Morbidity from delivery because of increased incidence of malpresentation and oligohydramnios.
Pulmonary hypoplasia :in fetus with PPROM
at early gestational age (10% at gestation of 24 weeks) especially if the pool of amniotic fluid is less than 2 cm.
Management of PROM:
• Diagnosis of PPROM:• Suggestive history :gush of liqour,
• gestational age ,uterine contraction ,reduced
• fetal movement with oligohydramnios .
• Sterile vaginal speculum examination.
• -amniotic fluid draining through the cervix.
• -vaginal fluid with alkaline PH (in case of doubt). By nitrazine testing
• Ultrasound :for evaluation of the amniotic fluid volume.
• Fetal Fibronectin immunoassay.
During initial clinical assessment exclude:
Overt chorioamnionitis:maternal tachycardia ,pyrexia ,uterine tenderness,
purulent vaginal discharge and fetal tachycardia.
Evaluation of the fetal gestational age:
history;Lmp,examination and US.
fetal well being:
Examination ,CTG.
Maternal well-being
Genital tract swab
Exclusion of abruptio placentae and preterm labour.
Amniocentesis
Management
• Management still controversial between :
• No clear evidence on the ideal management.
Conservative management include:
Surveillance for chorioamnionitis :-temperature ,pulse ,CTG.
-WBC,C-reactive protein.
-Lower genital tract swab and culture and sensitivity
Corticosteroid administration .
Tocolytic drugs
Post Term Pregnancy
Post term pregnancy:of 294 days duration or more from the onset of last menstrual
Period are defined as Post term,post-date (prolonged) pregnancy
Incidence : 6 – 12 % of all pregnancies .
Risk factors/associations
Poor (wrong) dating; prior post-term pregnancy;long (> 28 days) cycles without early ultrasound; placental sulfatase deficiency; anencephaly; male fetus .Prolonged pregnancy is increased in first pregnancies,but is not related to maternal age. Women with a body mass index greater than30 are at increased risk of prolonged pregnancy. The cause is unknown in most instancesComplications
Perinatal
Meconium aspiration, intrauterine infection,oligohydramnios,macrosomia, non-reassuring fetal heart testing low umbilical artery pH, and low 5-minute Apgar score
Maternal
Women giving birth post-term are at increased risk of labor dystocia, perineal injury, and cesarean delivery
pathophysiology of post term pregnancy :
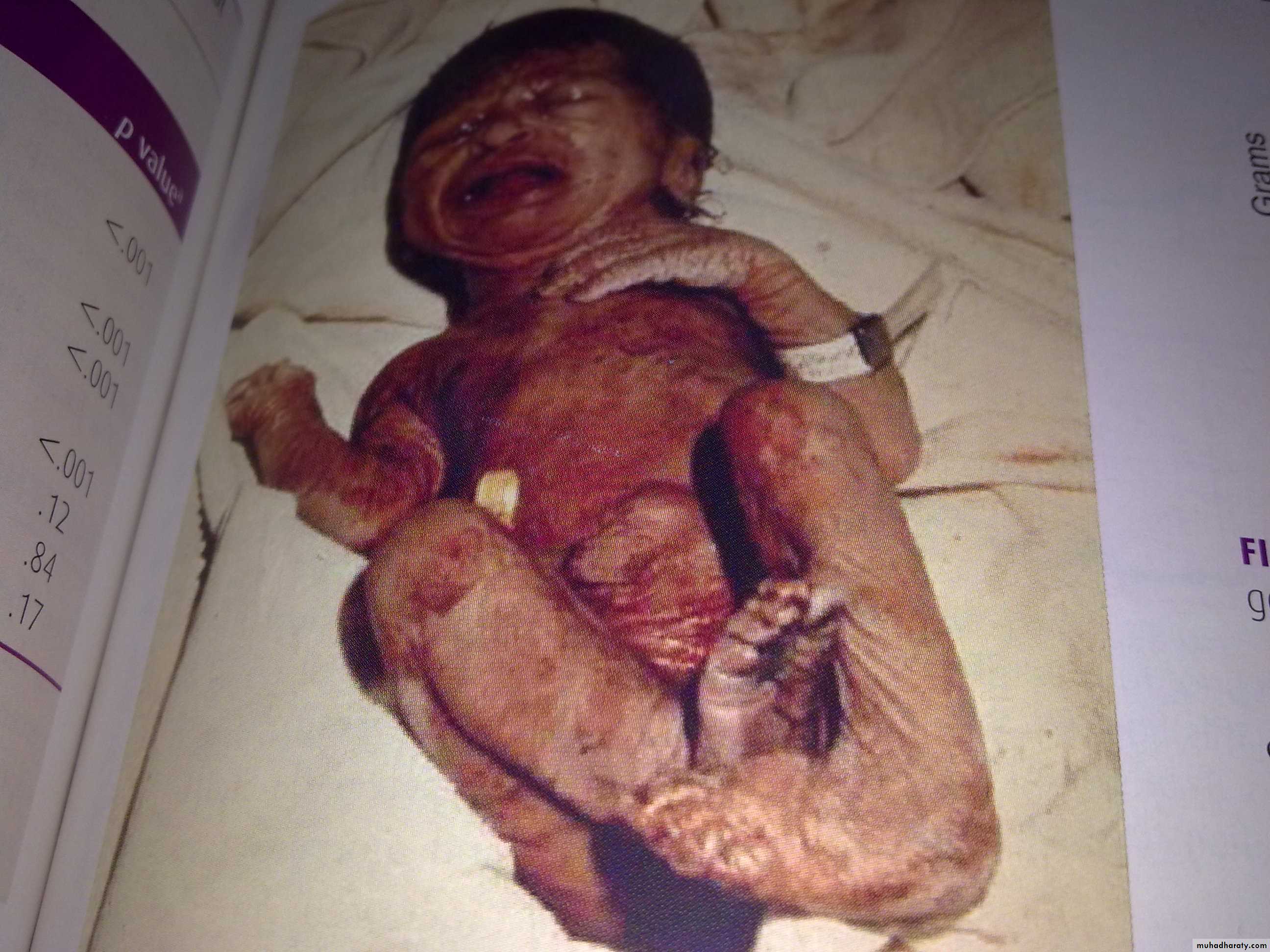
1-Postmaturity(dysmaturity) syndrome :Occuring in 20-30% of post term infants present a unique & characterstic appearance which includes wrinkled (prominent in palms &soles) ,patchy peeling skin ,long nails ,a long ,thin body suggesting wasting &advanced maturity because the infant is open- eyed allert warry appearance.
2-placental dysfunction /insufficiency : related to placental aging and infarction result into.
Intrauterine hypoxia may be manifested as meconium staining.
3-fetal distress &ligohydrmnio
4-fetal growth restriction
Factors evaluated in dating pregnancy
Accurate date of Lmp.Uterus size/date discrepancy during antenatal care.
Gestational age when the fetal heart beats first heard (doppler ultrasound at 12-14 weeks).
Gestational age when the fetal heart first heard
(stethoscope 18-20 weeks).
Date of quickening(18-20 w in primi 16-18 in multi)
Sonographic parameters (bipariatal diameter
between 16-20 weeks)
Management of post term pregnancy
Women with post-term pregnancies should undergo labour induction.
•patients who have unfavourable cervices Prostaglandin can be used in post-term pregnancies to promote cervical ripening and induce labour.
• Delivery should be effected if there is evidence of fetal compromise or oligohydramnios.
If induction leads to fetal distress at any stage, cesarean section should be done
prevention of post term pregnancy
Antepartum management ; Decision of delivery :If the patient is <42 weeks with engaged
head and favorable cervix then labour should
be induced .
Patient with <42 week and unfavorable
cervix:Twice weekly NST and BPP.
AFI amniotic fluid index (sum of 4 pocket of liquor in 4 quadrant).
If the result is reassuring then follow up and
delivery is indicated :-until the cervix is favorable .
-result is abnormal (deceleration, AFI is
oligohydramnia <=5) .
-Fetal macrosomia .
-42 weeks regardless of other factors
because of increased perinatal morbidity
and mortality .
routine induction of labor at ≥ 41 weeks reduces perinatal mortality by 80%
Labor is dangerous time for post-term infants therefore early admission is needed
Labor evaluated, perform amniotomy to identify thick meconium (but it can enhance cord compression) ?
Continuous electronic fetal monitoring
during induction of labour.
apply internal electrodes.
If there is fetal distress (fetal blood sampling) then C.S. is indicated .