Integrated Management of Child Health
What is the IMCI strategy?The Integrated Management of Child Health (IMCI) strategy is a public health strategy that aims at improving the quality of health care provided to children under 5 years of age both at primary health care facilities and at home, through its three components:
• Improvement of health providers’ performance;
• Improvement of related elements of health system support;
• Improvement of family and community practices.
1
This primary child health care strategy promotes a holistic approach to the management of under-five children, addressing promotive and preventive aspects of child health, as well as curative aspects of priority child health problems in a country.
2
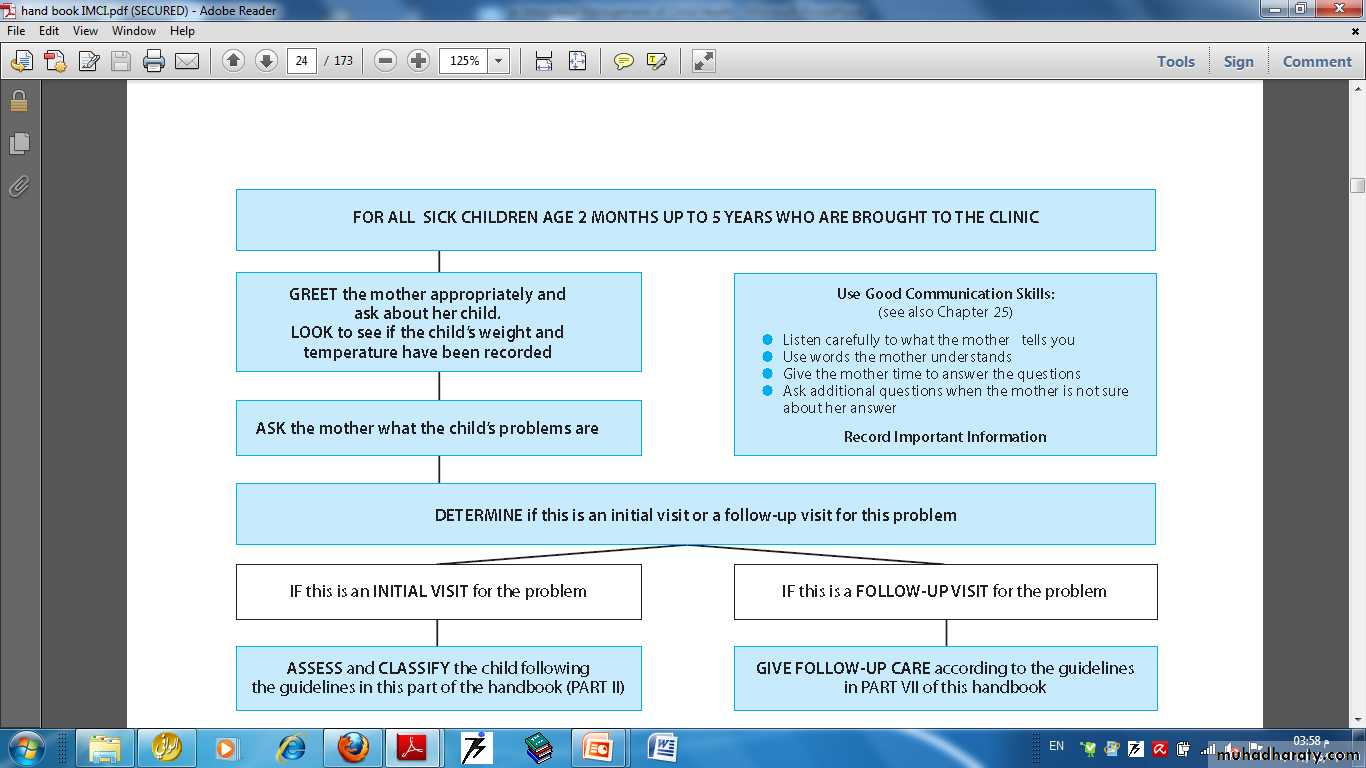
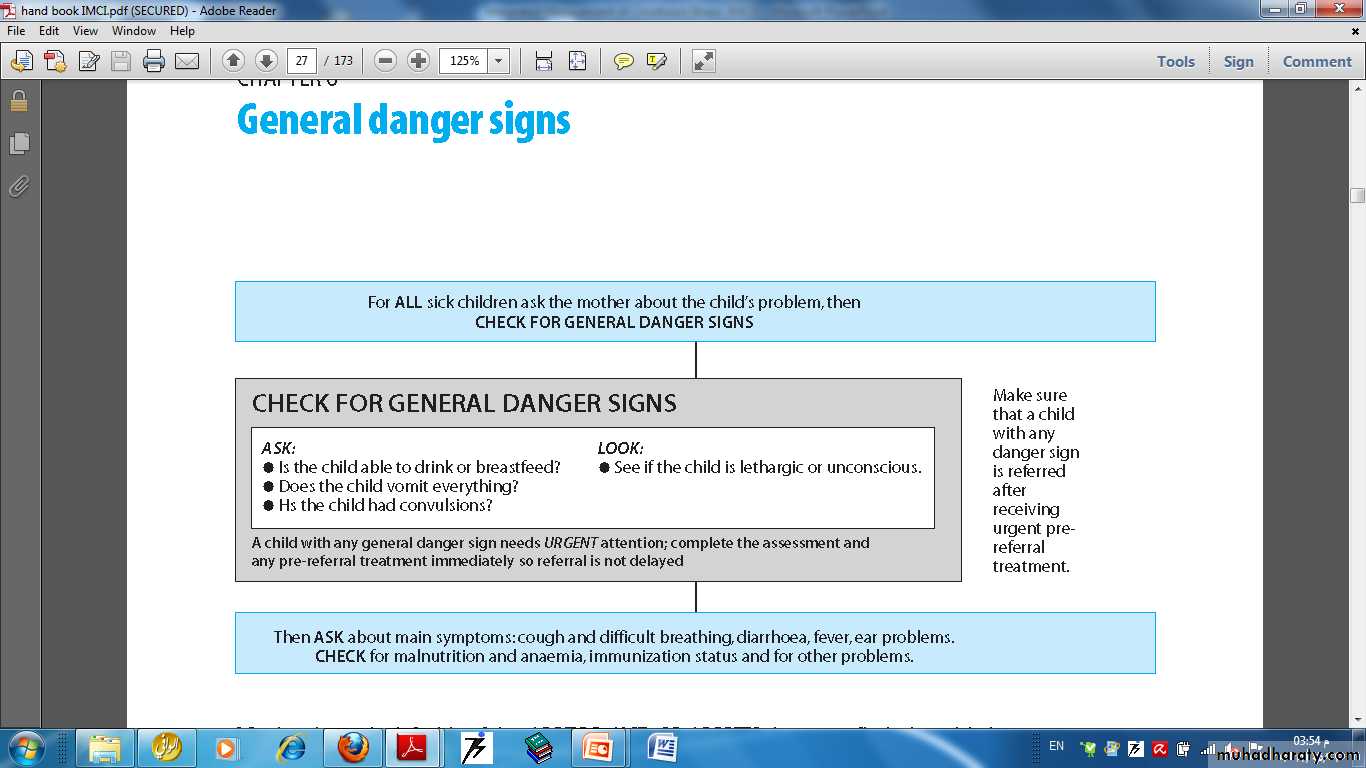
The IMCI guidelines describe how to care for a child who is brought to a clinic with an illness, or for a scheduled follow up visit to check the child’s progress. The guidelines give instructions for how to routinely assess a child for general danger signs (or possible bacterial infection in a young infant), common illnesses, malnutrition and anaemia, and to look for other problems. In addition to treatment, the guidelines incorporate basic activities for illness prevention.
3
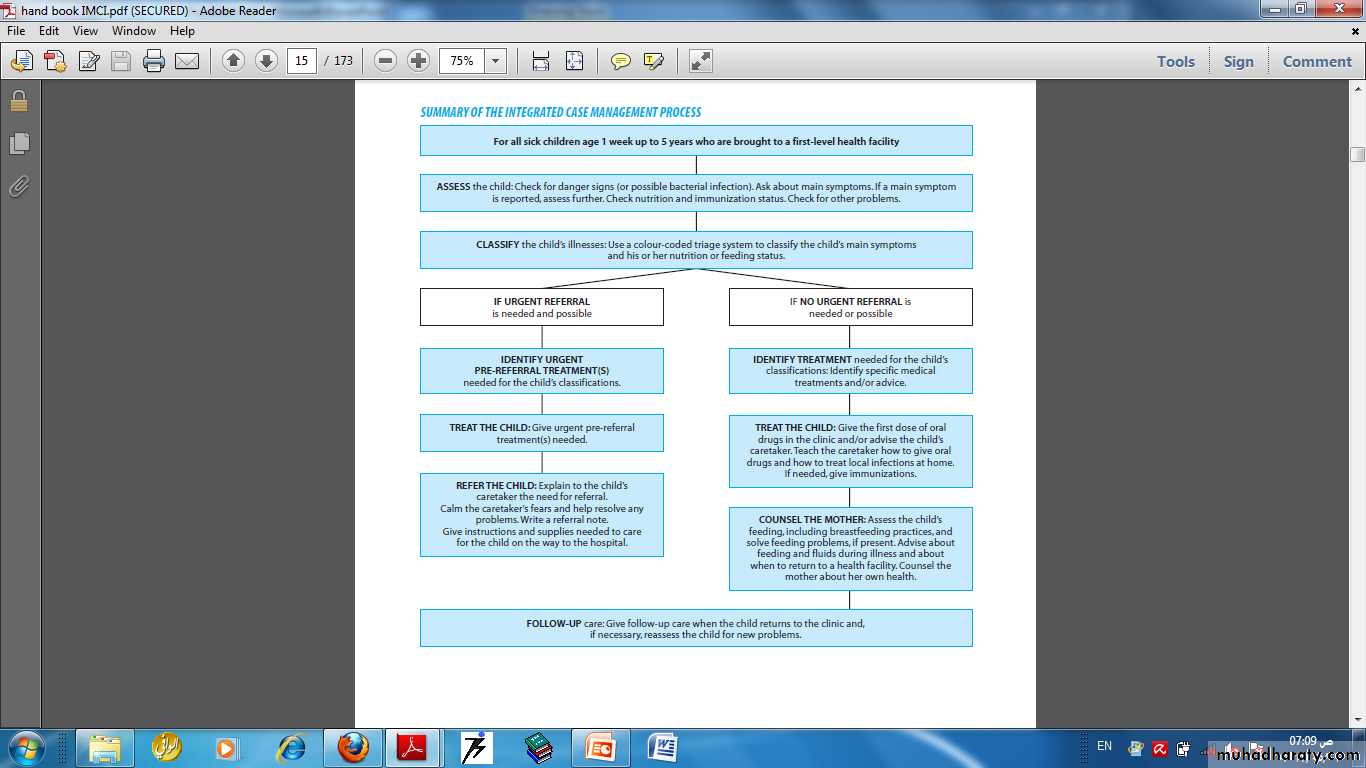
The complete IMCI case management process involves the following elements:
■ Assess a child by checking first for danger signs(or possible bacterial infection in a young infant), asking questions about common conditions, examining the child, and checking nutrition and immunization status. Assessment includes checking the child for other health problems.
4
■ Classify a child’s illnesses using a colour-coded triage system. Because many children have more than one condition, each illness is classified according to whether it requires:
— urgent pre-referral treatment and referral (red), or
— specific medical treatment and advice (yellow), or
— simple advice on home management (green).
5
■ After classifying all conditions, identify specific treatments for the child. If a child requires urgent referral, give essential treatment before the patient is transferred. If a child needs treatment at home, develop an integrated treatment plan for the child and give the first dose of drugs in the clinic. If a child should be immunized, give immunizations.
6
■ Provide practical treatment instructions, including teaching the caretaker how give oral drugs, how to feed and give fluids during illness, and how to treat local infections at home. Ask the caretaker to return for follow-up on a specific date, and teach her how to recognize signs that indicate the child should return immediately to the health facility.
7
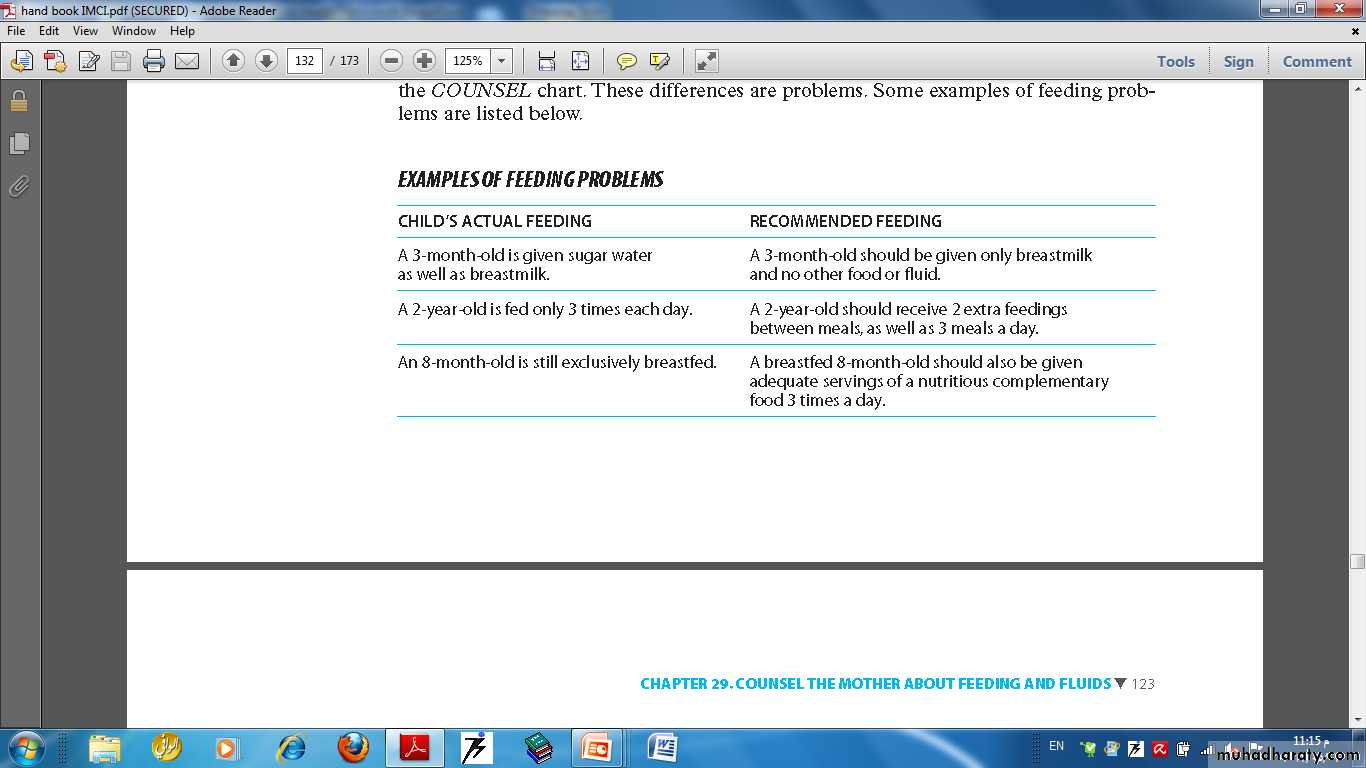
■ Assess feeding, including assessment of breastfeeding practices, and counsel to solve any feeding problems found. Then counsel the mother about her own health.
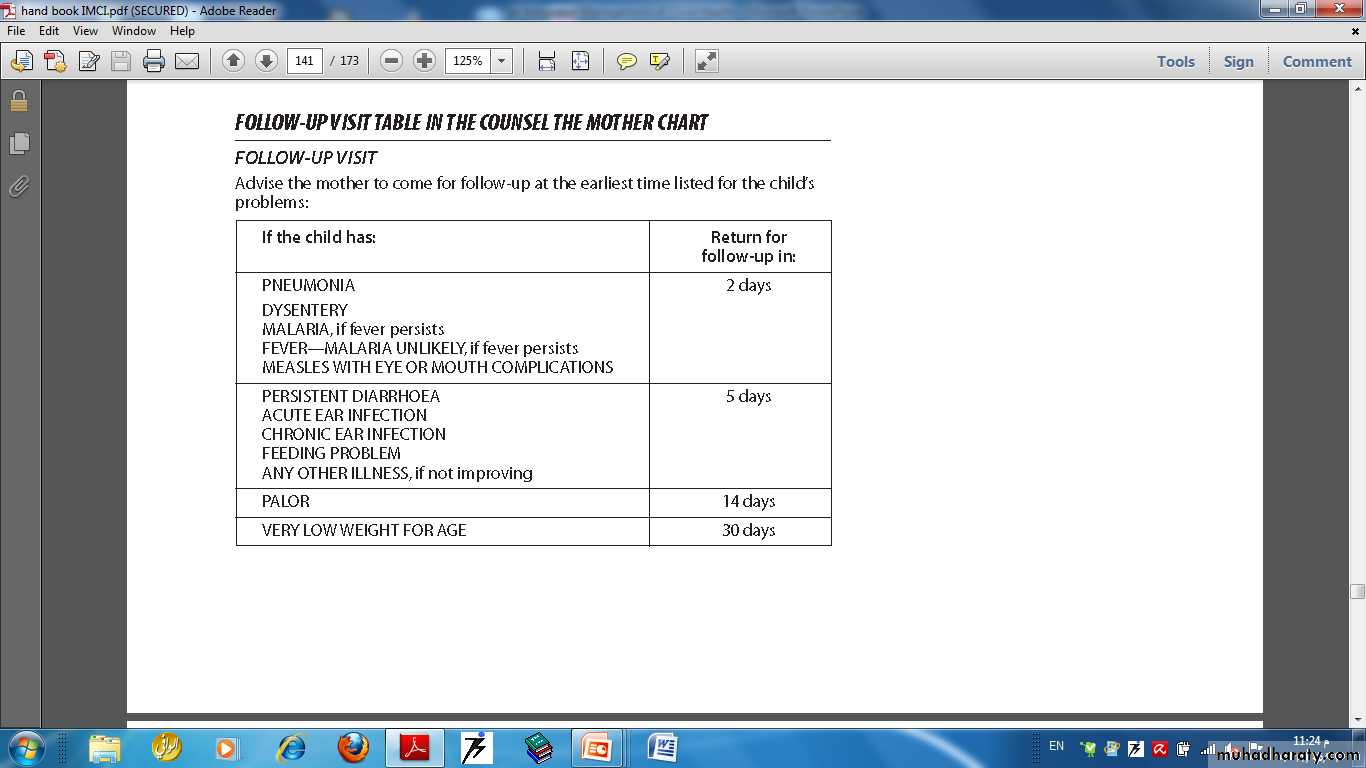
■ When a child is brought back to the clinic as requested, give follow-up care and, if necessary, reassess the child for new problems.
8
Case management can only be effective to the extent that families bring their sick children to a trained health worker for care in a timely way.
If a family waits to bring a child to a clinic until the child is extremely sick, or takes the child to an untrained provider, the child is more likely to die from the illness.
Therefore, teaching families when to seek care for a sick child is an important part of the case management process.
9
10
11
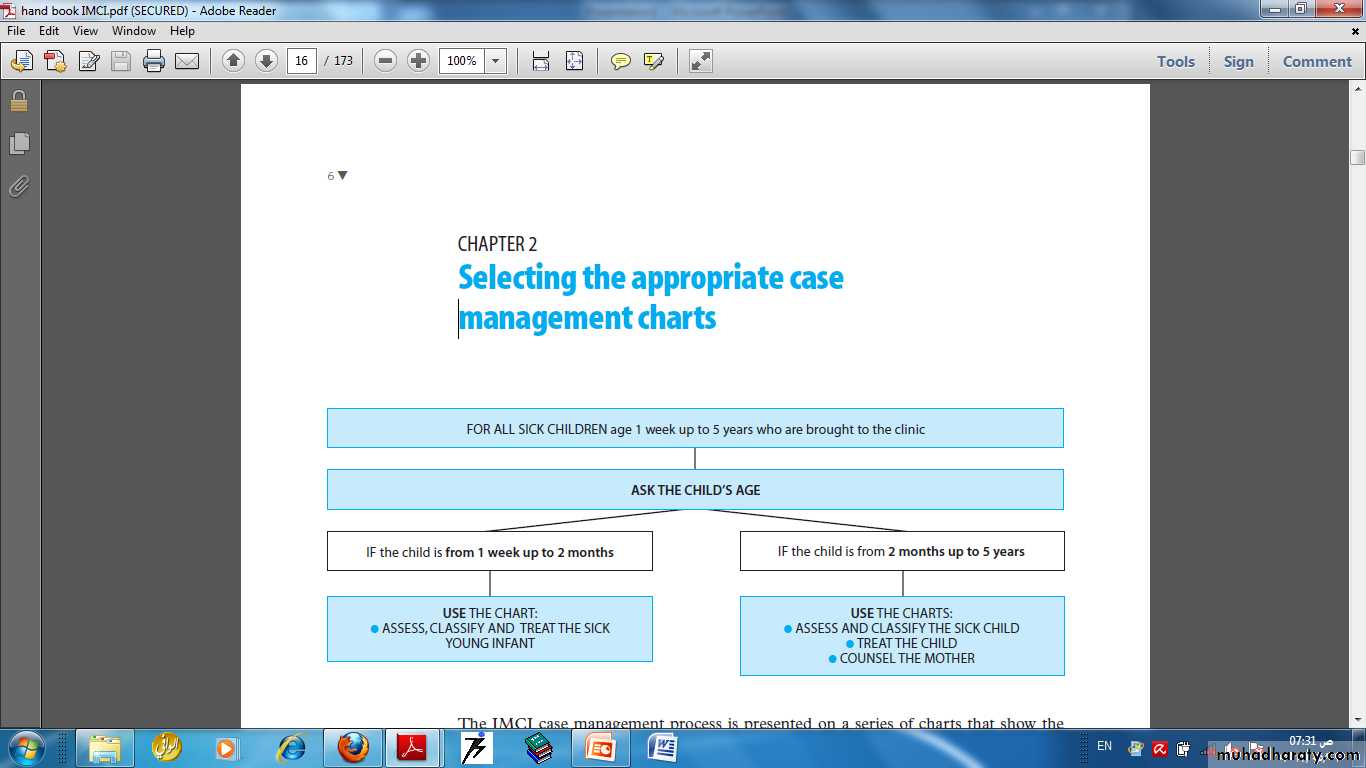
The IMCI chart booklet contains three charts for managin sick children age 2 months up to 5 years, and a separate chart for managing sick young infants age 1 week up to 2 months.
Up to 5 years means the child has not yet had his or her fifth birthday. For example, this age group includes a child who is 4 years 11 months but not a child who is 5 years old. A child who is 2 months old would be in the group 2 months up to 5 years, not in the group 1 week up to 2 months.
The case management process for sick children age 2 months up to 5 years is presented on three charts titled:
■ ASSESS AND CLASSIFY THE SICK CHILD
■ TREAT THE CHILD
■ COUNSEL THE MOTHER
12
If the child is not yet 2 months of age, the child is considered a young infant. Management of the young infant age 1 week up to 2 months is somewhat different from older infants and children. It is described on a different chart titled:
■ ASSESS, CLASSIFY AND TREAT THE SICK YOUNG INFANT.
13
The IMCI case management charts and recording forms guide you through the following steps:
■ Assess the sick child or sick young infant
■ Classify the illness
■ Identify treatment
■ Treat the child or young infant
■ Counsel the mother
■ Give follow-up care
The case management steps are the same for all sick children from age 1 week up to 5 years.
14
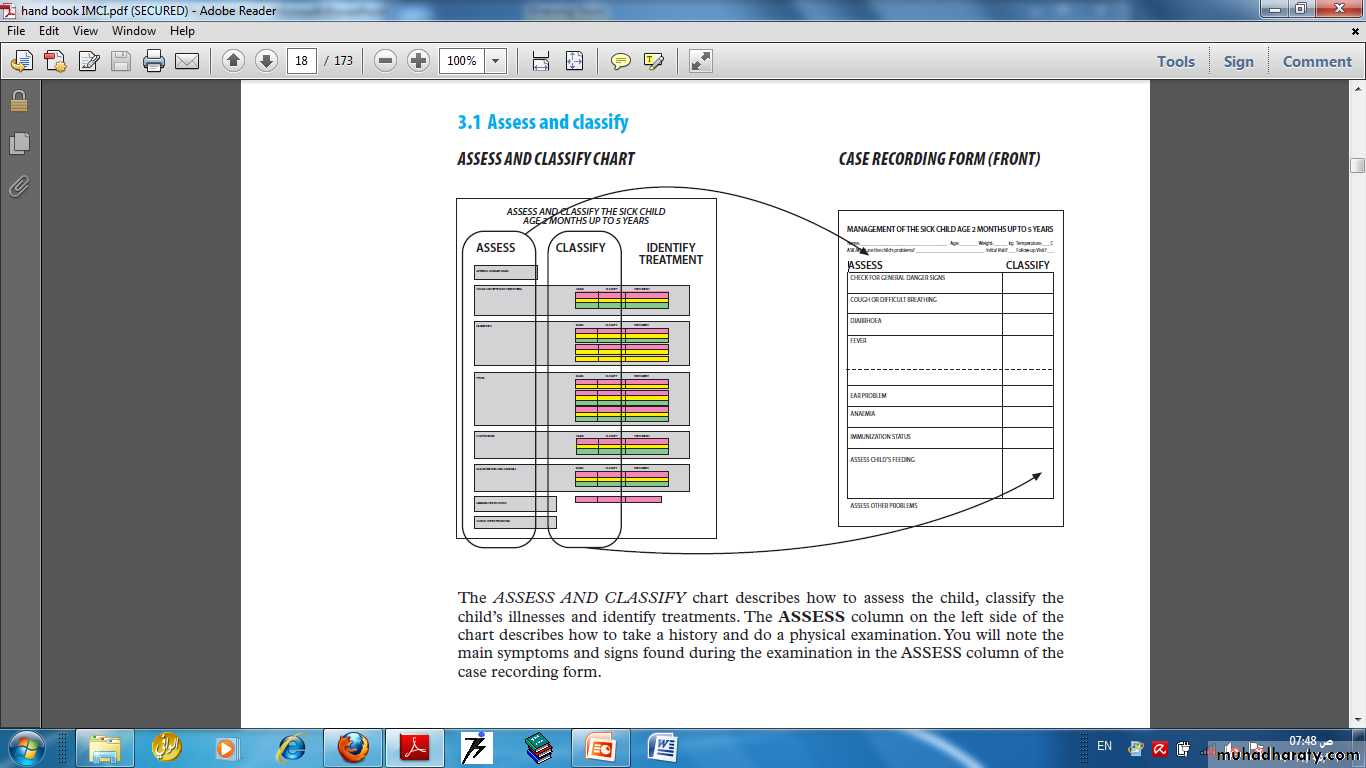
The ASSESS column on the left side of the chart describes how to take a history and do a physical examination. You will note the main symptoms and signs found during the examination in the ASSESS column of the Case recording form.
15
16
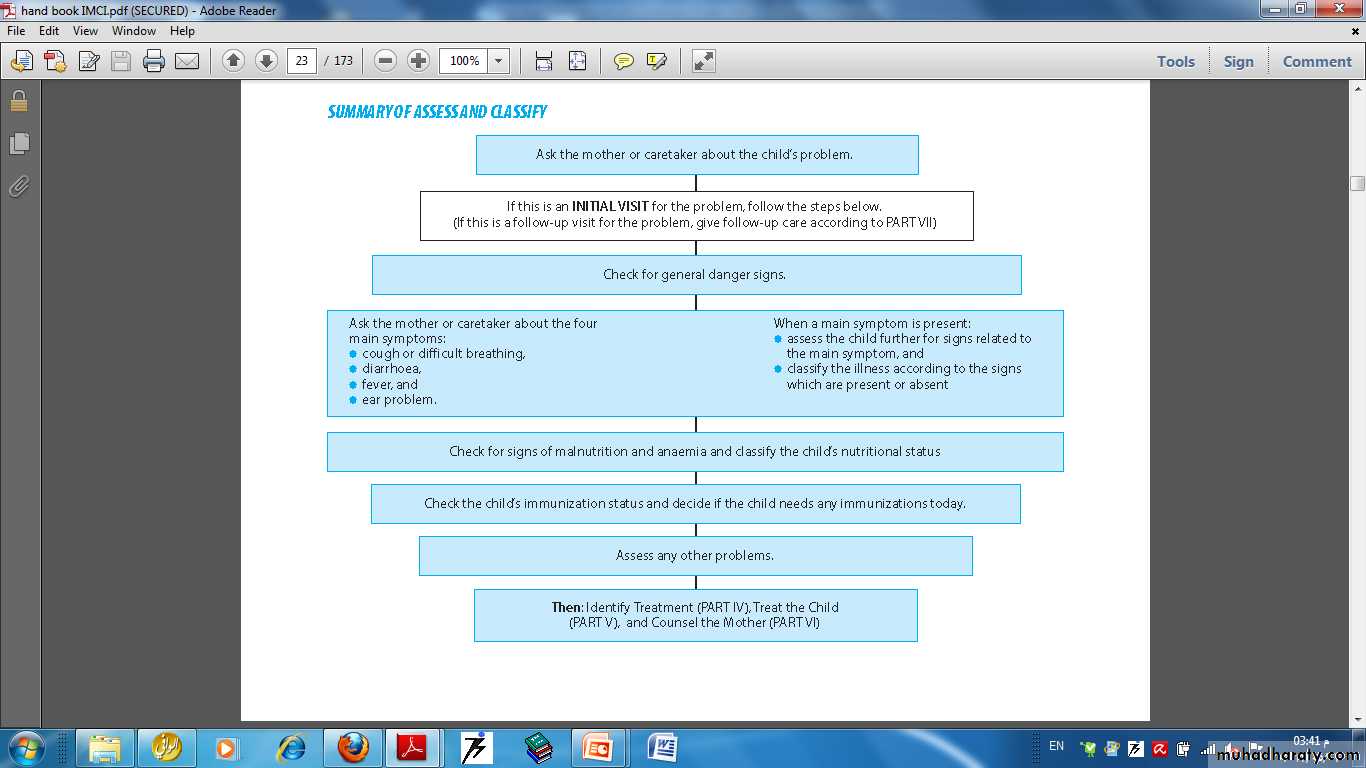
When a child is brought to the clinic
17General danger signs
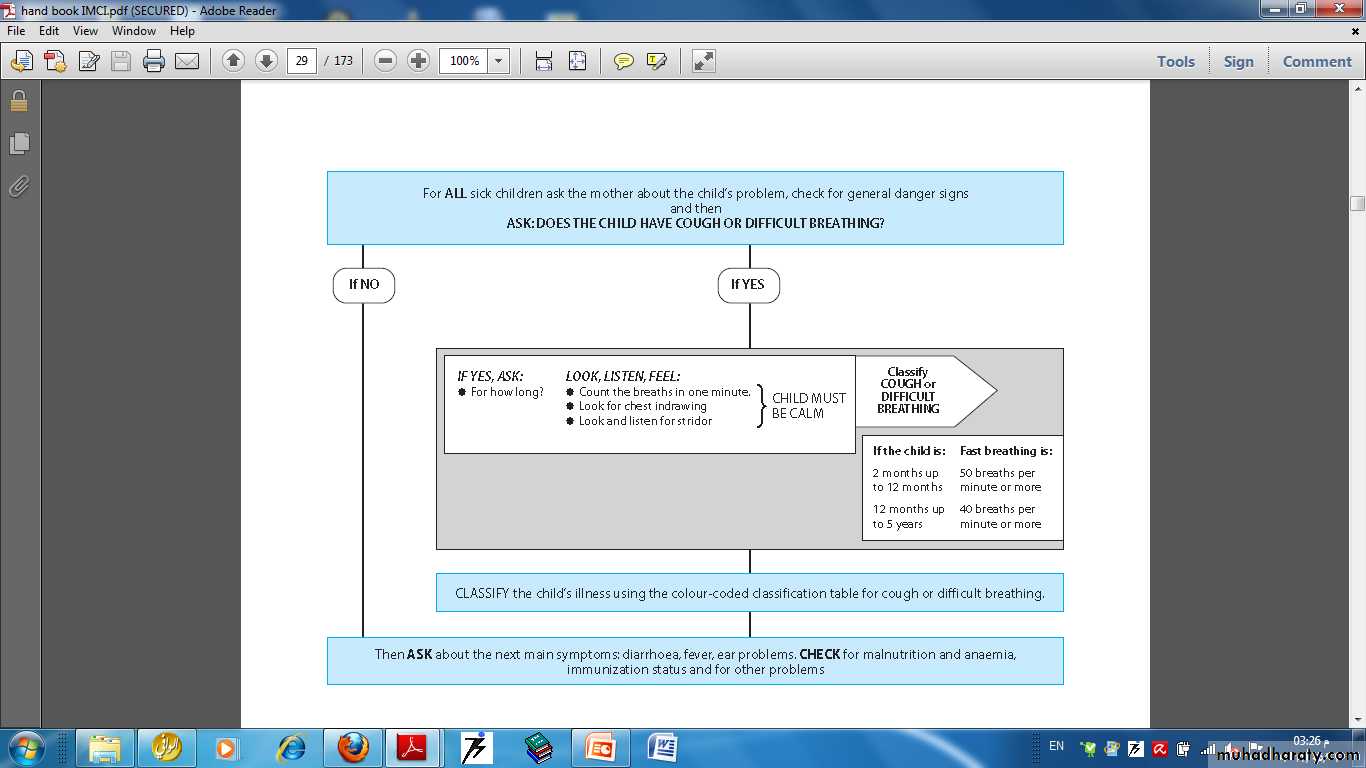
18Cough or difficult breathing
19
Cough or Difficulty of Breathing
• Any general danger sign or• Chest indrawing or Stridor in a calm child
• SEVERE PNEUMONIA OR VERY SEVERE DISEASE
• Give first dose of an appropriate antibiotic
• Refer URGENTLY to a hospital
• Fast breathing
• PNEUMONIA
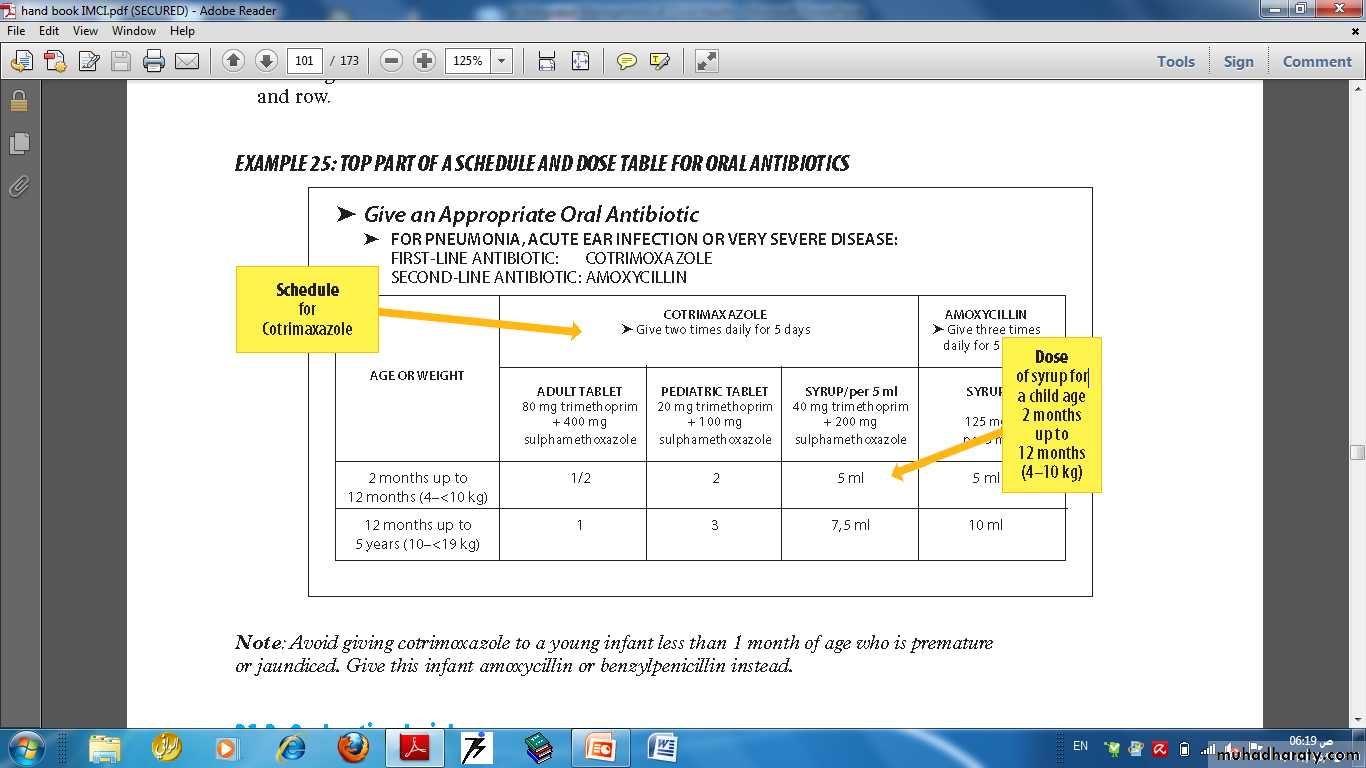
• Give an appropriate oral antibiotic for 5days
• Soothe the throat and releive the cough with a safe remedy
• Advise mother when to return immediately
• Follow-up in 2days
• No signs of pneumonia or very severe disease
• NO PNEUMONIA, COUGH OR COLD
• If coughing >30days refer for assessment
• Soothe the throat and releive the cough with a safe remedy
• Advise mother when to return immediately
• Follow-up in 6days if not improving
SIGNS CLASSIFY AS IDENTIFY TREATMENT
20
Treatment
Soothe the throat, releive the cough with a safe remedy
Safe remedies to recommend:
Breastmilk for exclusively breastfed infant; tamarind, calamansi, gingerHarmful remedies to discourage:
Codeine cough syrupOther cough syrups
Oral and nasal decongestants
21
22
23
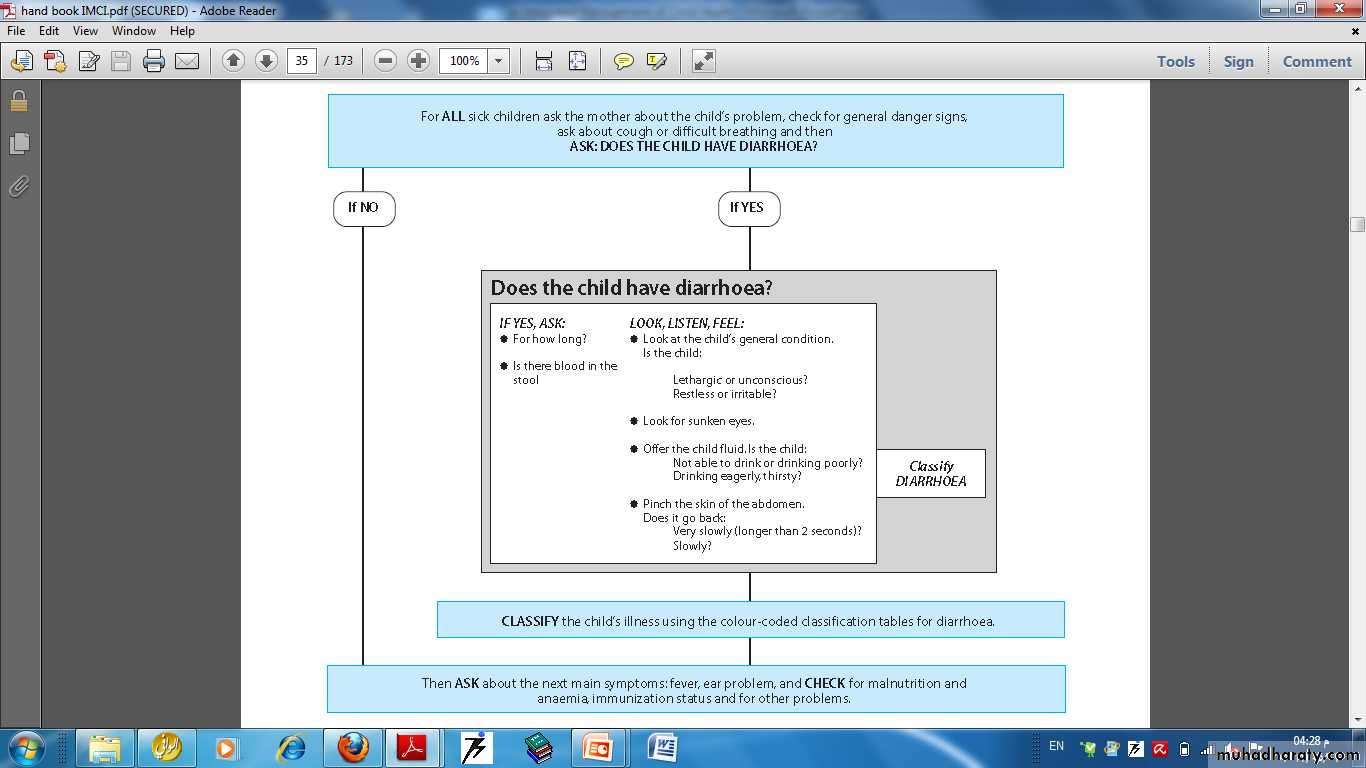
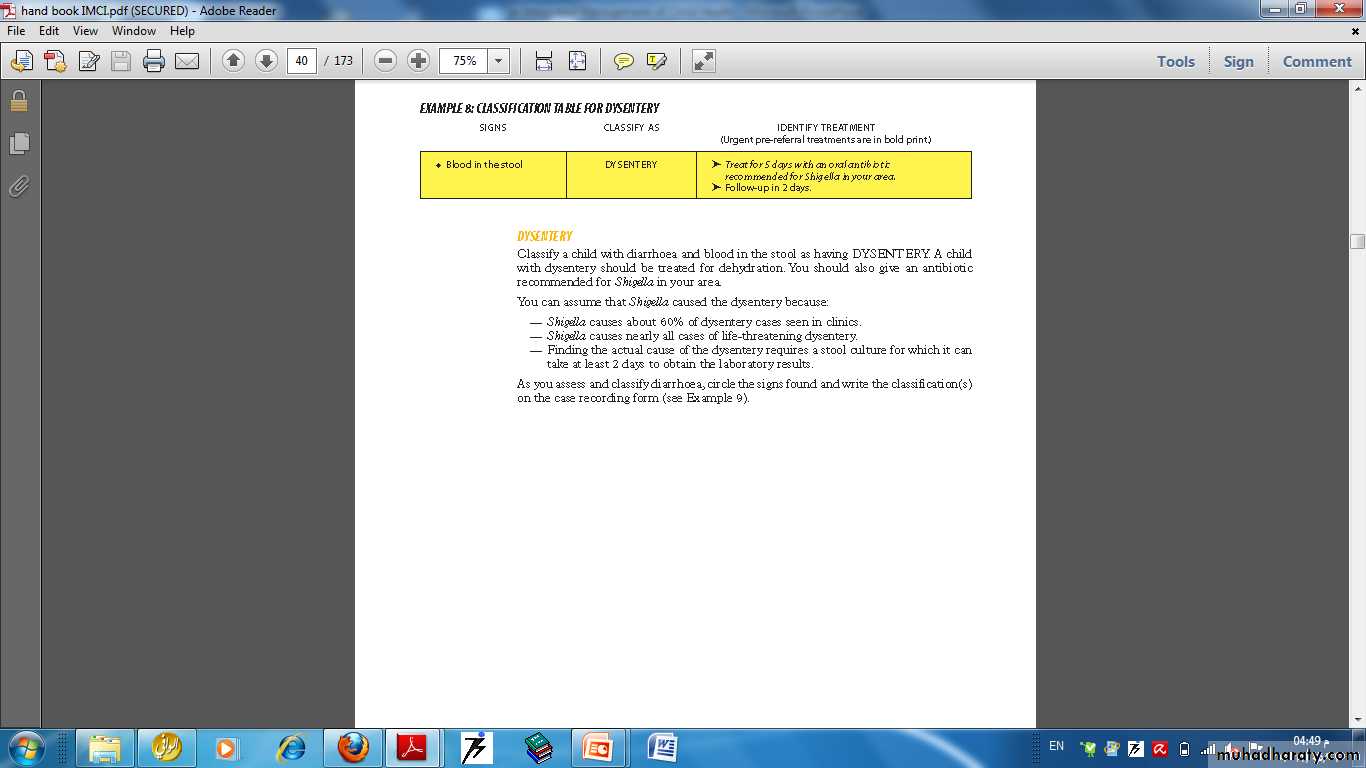
DIARRHEA
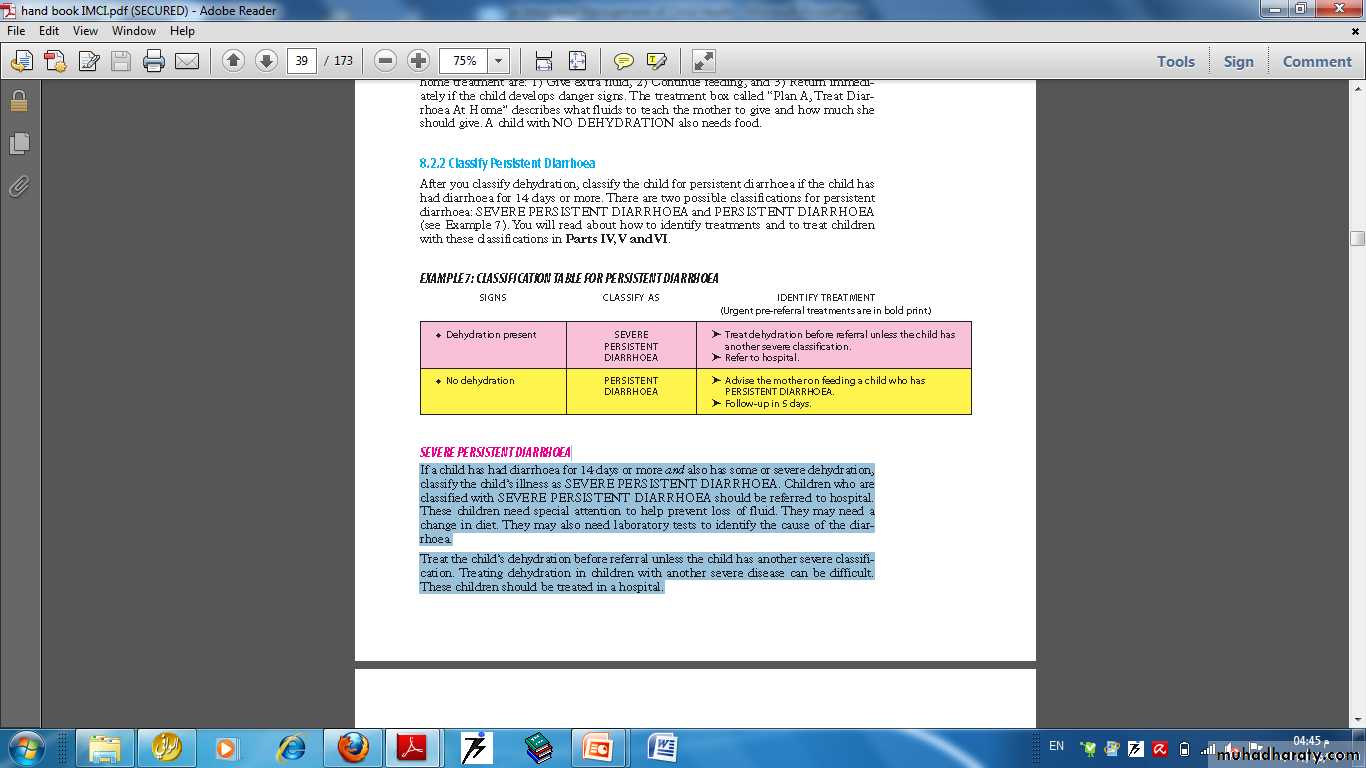
If a child has the main symptom of diarrhea, the child can be classified for dehydration, for persistent diarrhoea and for dysentery.When classifying diarrhea:
■ all children with diarrhea are classified for dehydration
■ if the child has had diarrhea for 14 days or more, classify the child for persistent diarrhea
■ if the child has blood in the stool, classify the child for dysentery.
24
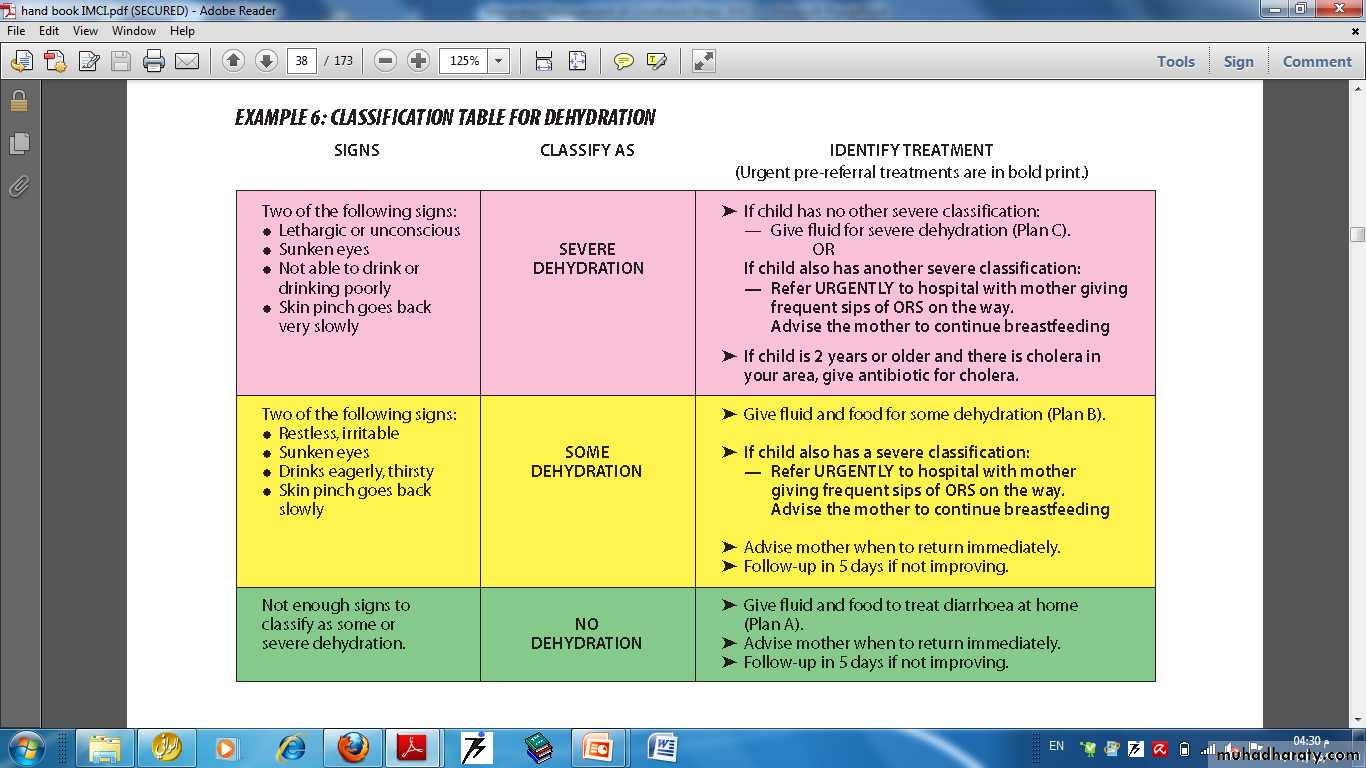
CLASSIFICATION TABLE FOR DEHYDRATION
25Plan A: Treat diarrhoea at home
Treat a child who has diarrhoea and NO DEHYDRATION with Plan A. The 3 Rules of Home Treatment are:1. GIVE EXTRA FLUID (as much as the child will take)
2. CONTINUE FEEDING
3. WHEN TO RETURN
If a child is not exclusively breastfed, give one or more of the following:
— ORS solution
— Food-based fluids
— Clean water
26
No Dehydration
Treatment Plan A
Age Amount of Fluid Type of Fluid
< 2 yrs 50-100 ml (¼-½ cup) after each loose stool
2-10 yrs 100-200 ml (½-1 cup) after each loose stoolORS, rice water, yogurt, soup with salt
Give frequent small sips from a cup.If the child vomits, wait 10 minutes. Then continue, but
more slowly.Continue giving extra fluids until the diarrhea stops.
27• Treatment Plan B Some dehydration
Give frequent small sips from a cupIf the child vomits, wait 10 minutes. Continue afterwards, but more slowly
Continue giving extra fluids until the diarrhea stops . Inform the mother how much ORS to administer over the next 4 hours. If less than 2 years show her to give a spoonful frequently.
Reassess after 4 hours and classify the child for dehydration
28
Age Up to 4 mos 4mos - 12mos 12mos – 2years 2 years – 5years
Treatment Plan B Some Dehydration
WEIGHTIn ml
< 6 kg 6 - <10 kg 10 - <12 kg 12 – 19 kg
200-400 400-700 700-900 900-1400
The appropriate amount of ORS can also be calculated by multiplying the child’s weight in kg by 75.
29
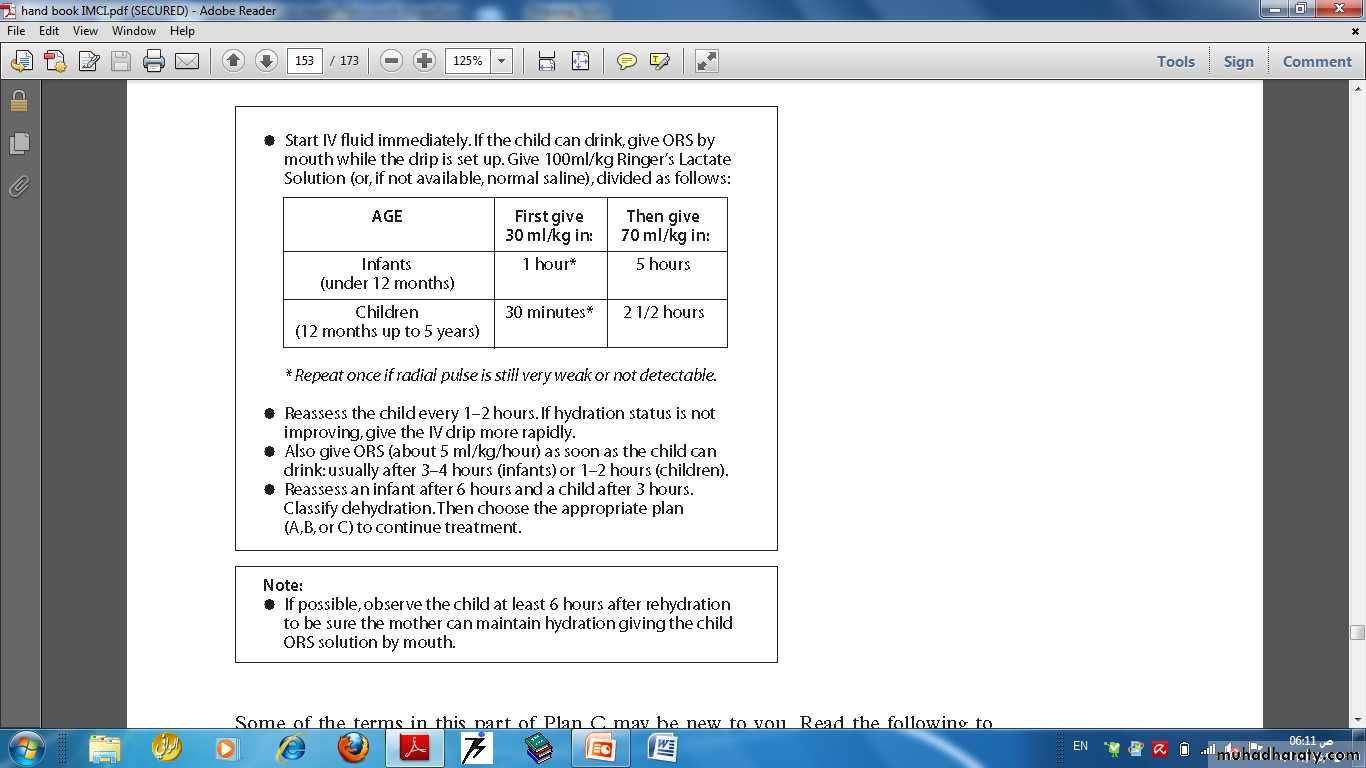
PLAN C – TREAT SEVERE DEHYDRATION QUICKLY
3031
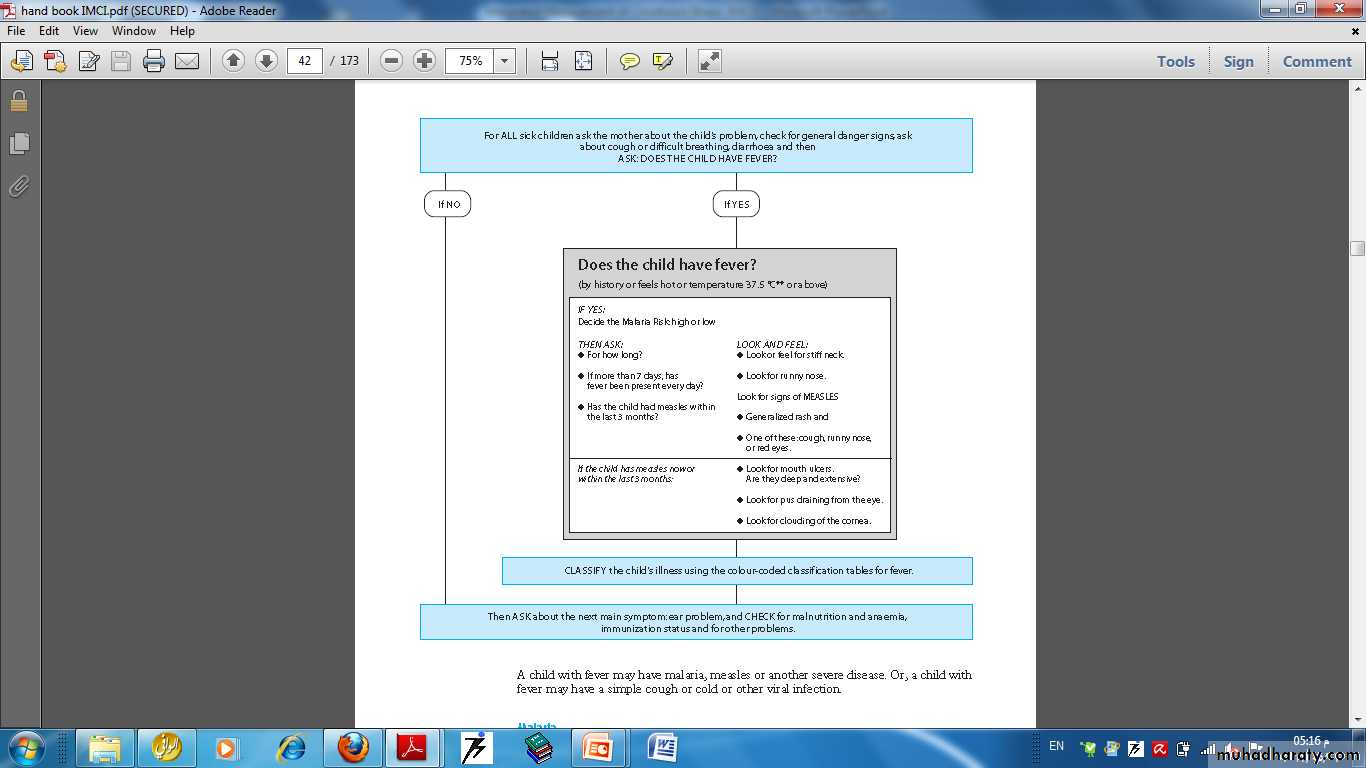
A child with fever may have malaria, measles or another severe disease. Or, a child with fever may have a simple cough or cold or other viral infection.
32
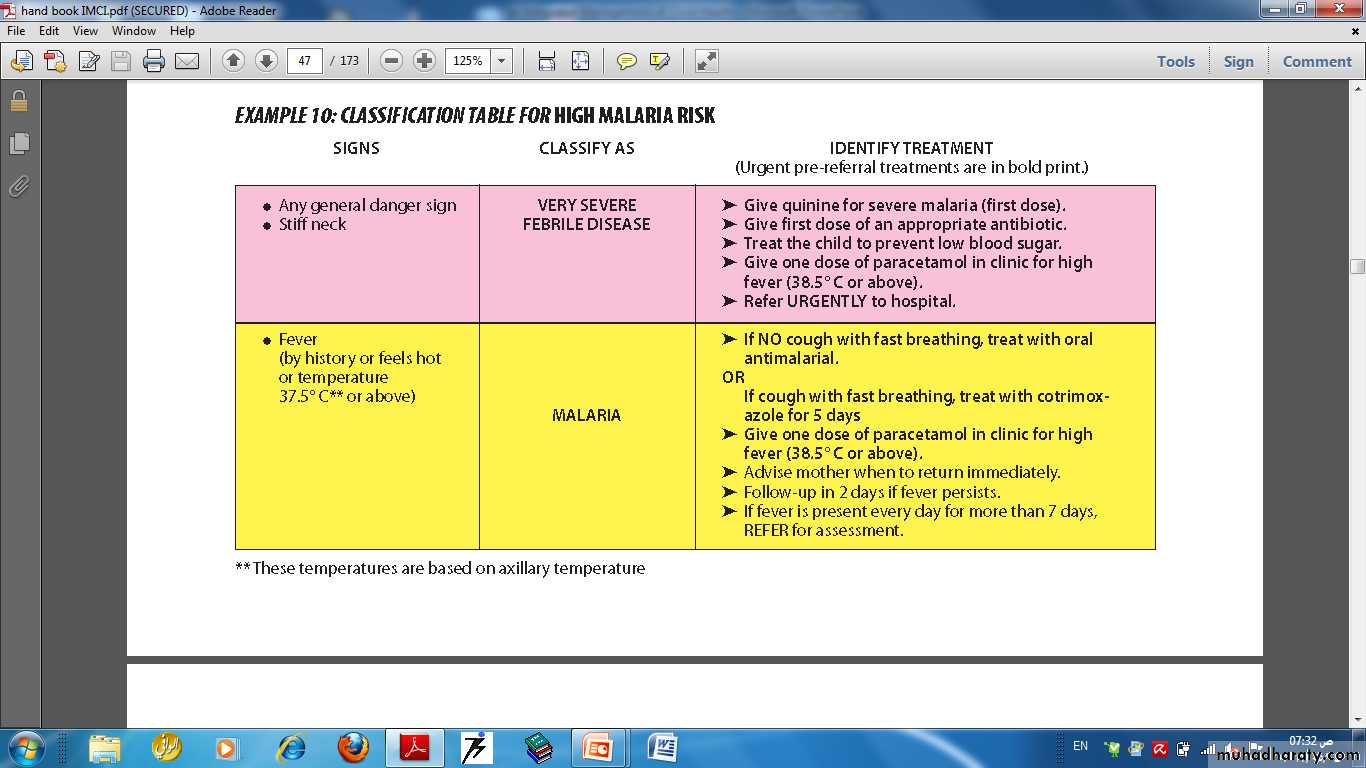
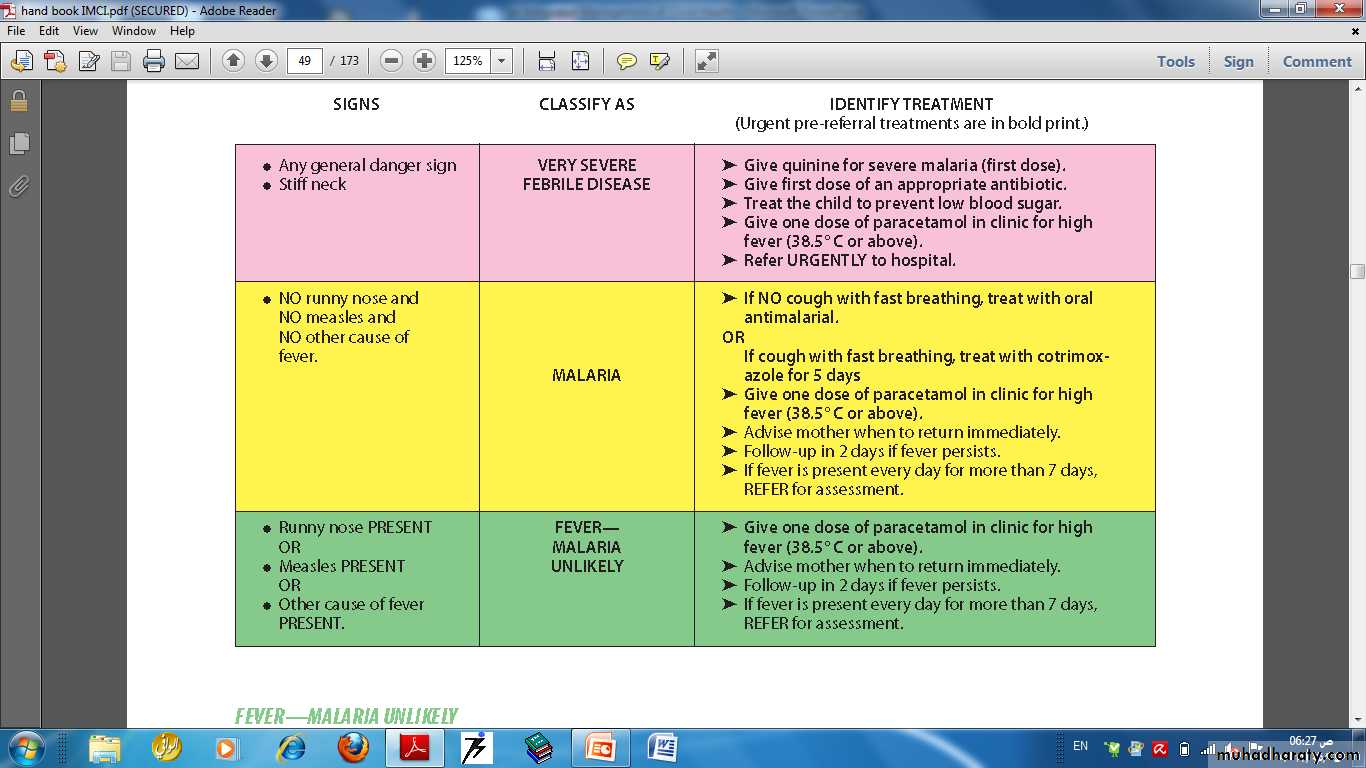
How to classify fever
If the child has fever and no signs of measles, classify the child for fever only. If the child has signs of both fever and measles, classify the child for fever and for measles.The ASSESS & CLASSIFY chart has more than one table to classify fever. One is used to classify fever when the risk of malaria is high. The others are used to classify fever when the risk of malaria is low or no. To classify fever, you must know if the malaria risk is high, low or no. You should also know if the child has travelled outside the area in the last 2 weeks. Then select the appropriate classification table.
33
34
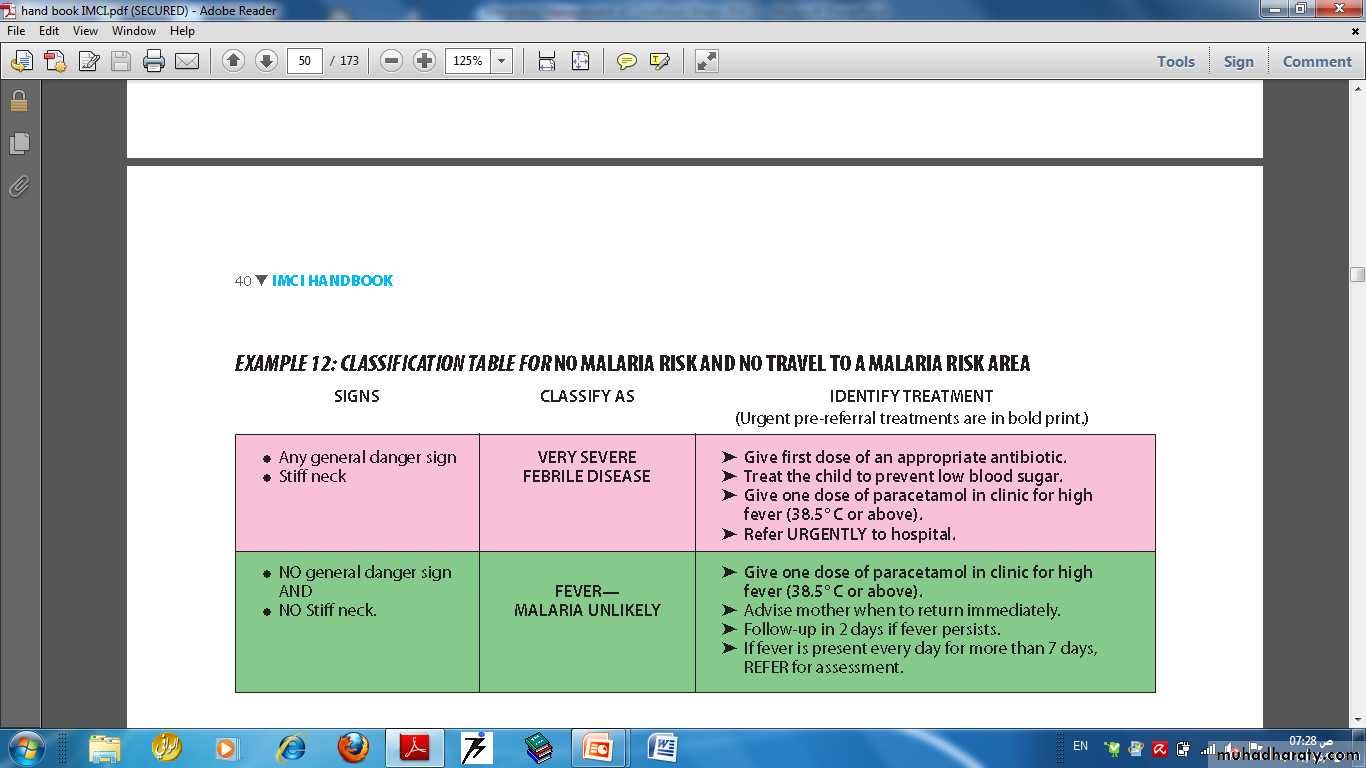
CLASSIFICATION TABLE FOR LOW MALARIA RISK AND NO TRAVEL TO A HIGH RISK AREA
3536
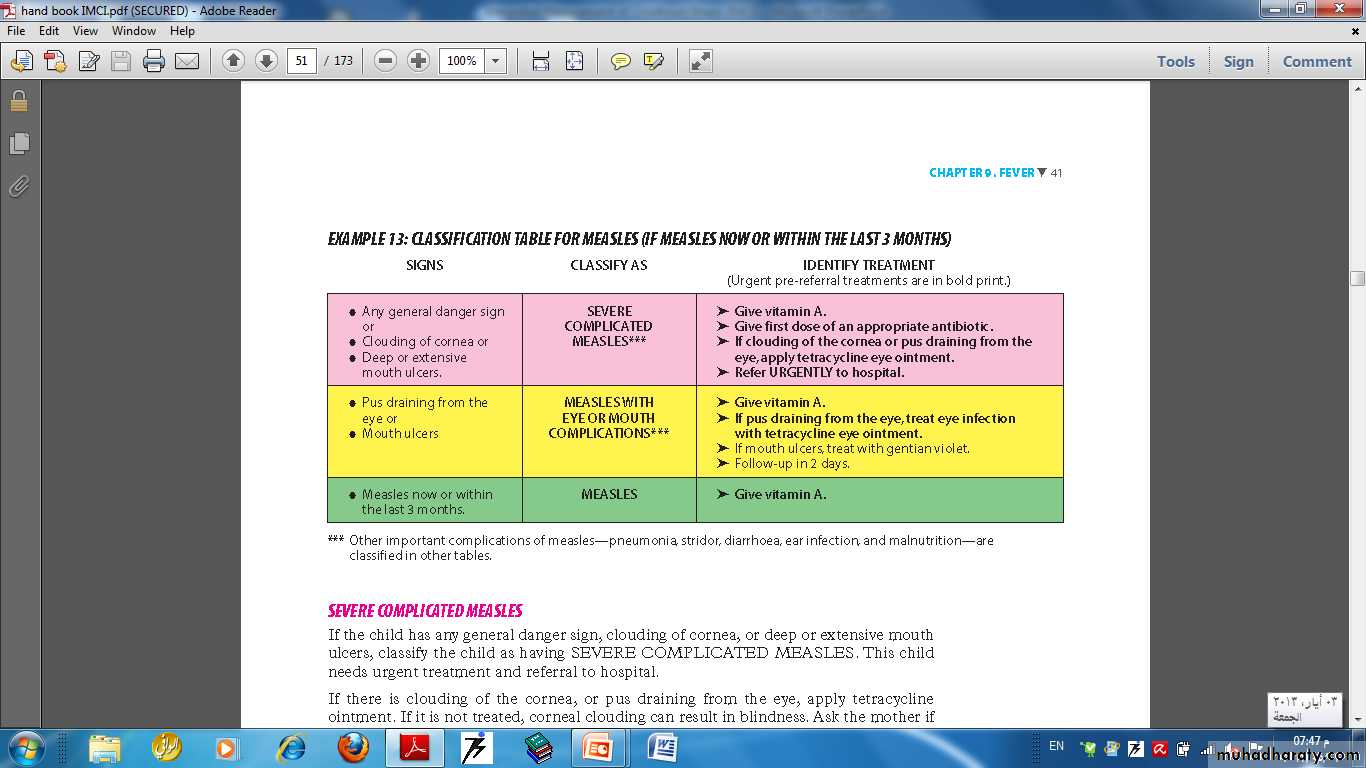
CLASSIFICATION TABLE FOR MEASLES (IF MEASLES NOW OR WITHIN THE LAST 3 MONTHS)
37Does the child have Fever?(by history, or feels hot or temp > 37.5)
if the child has fever, assess the child for additional signs related to feverIf the child does not have fever, tick “no” on the recording form for the sick child, then ask about the next main symptom (ear problem)
38
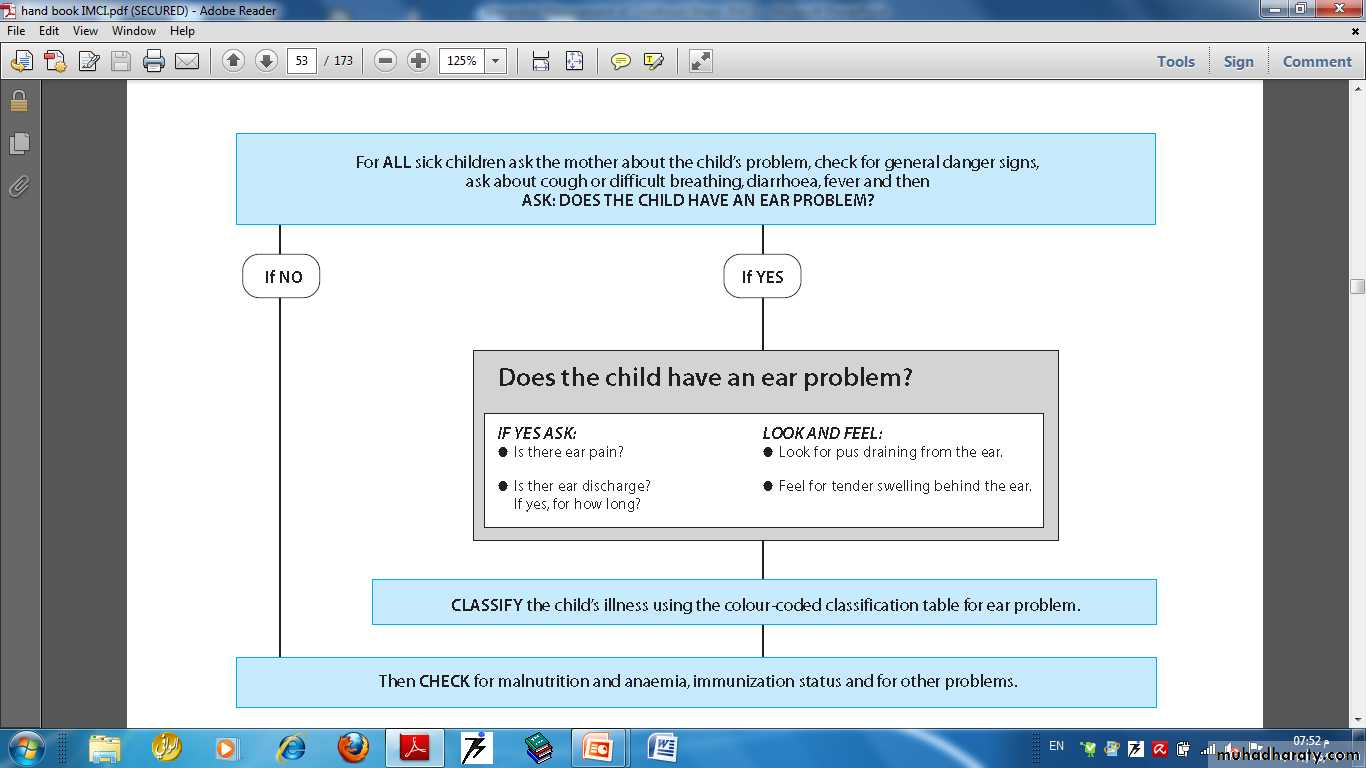
Ear problem
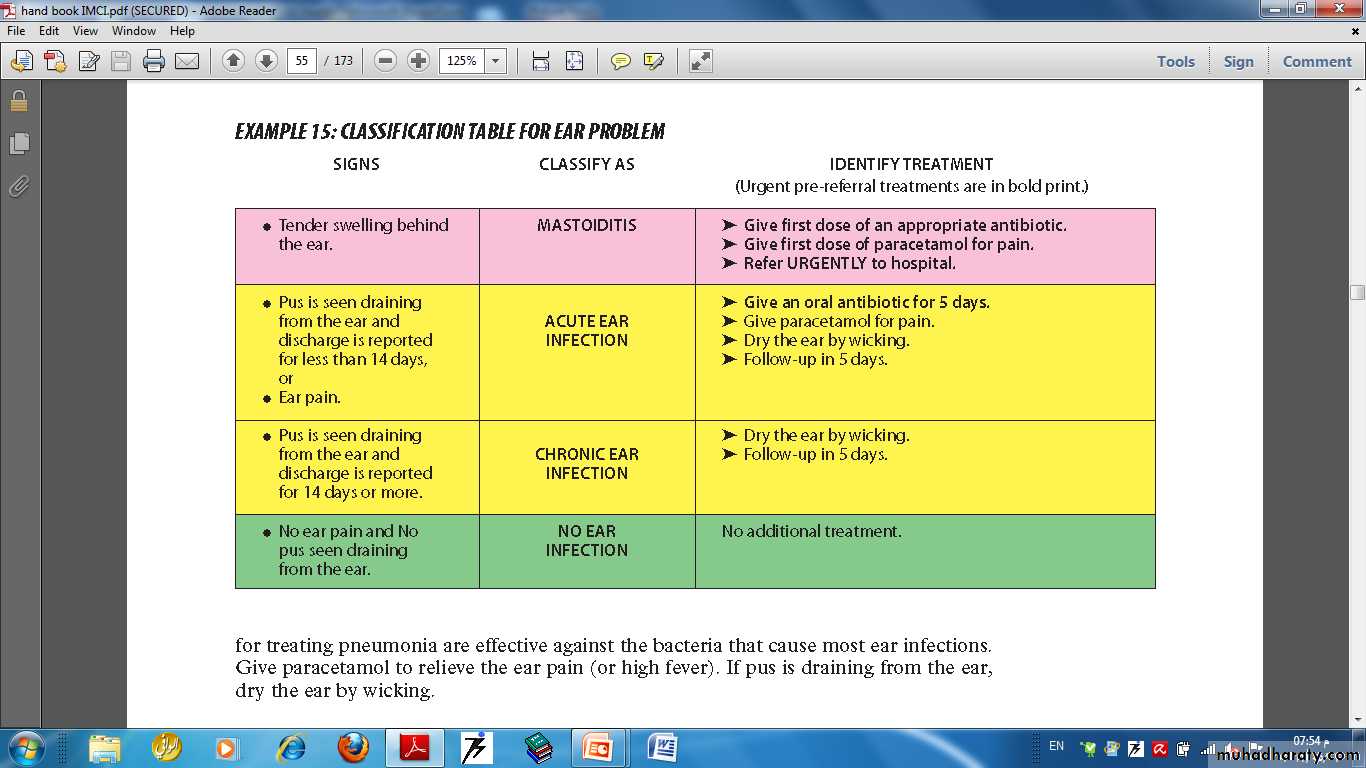
39CLASSIFICATION TABLE FOR EAR PROBLEM
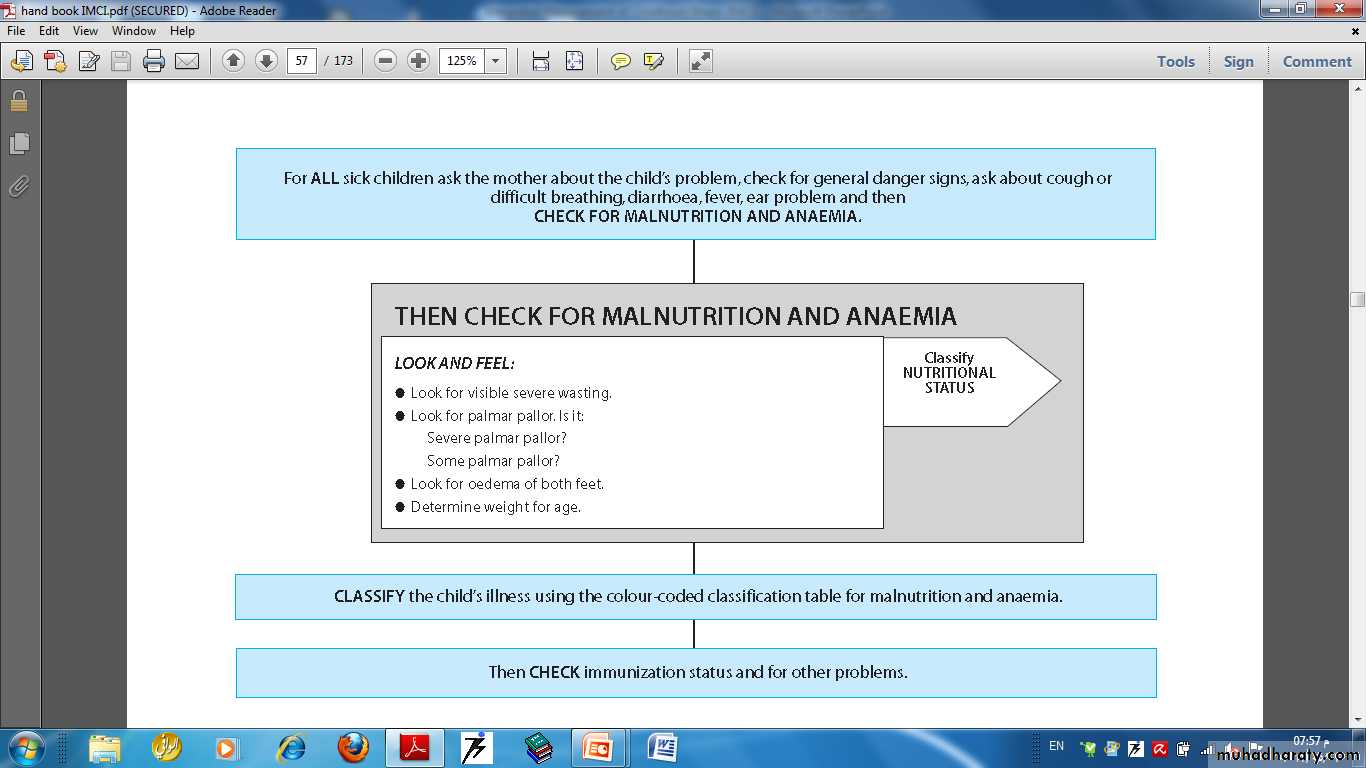
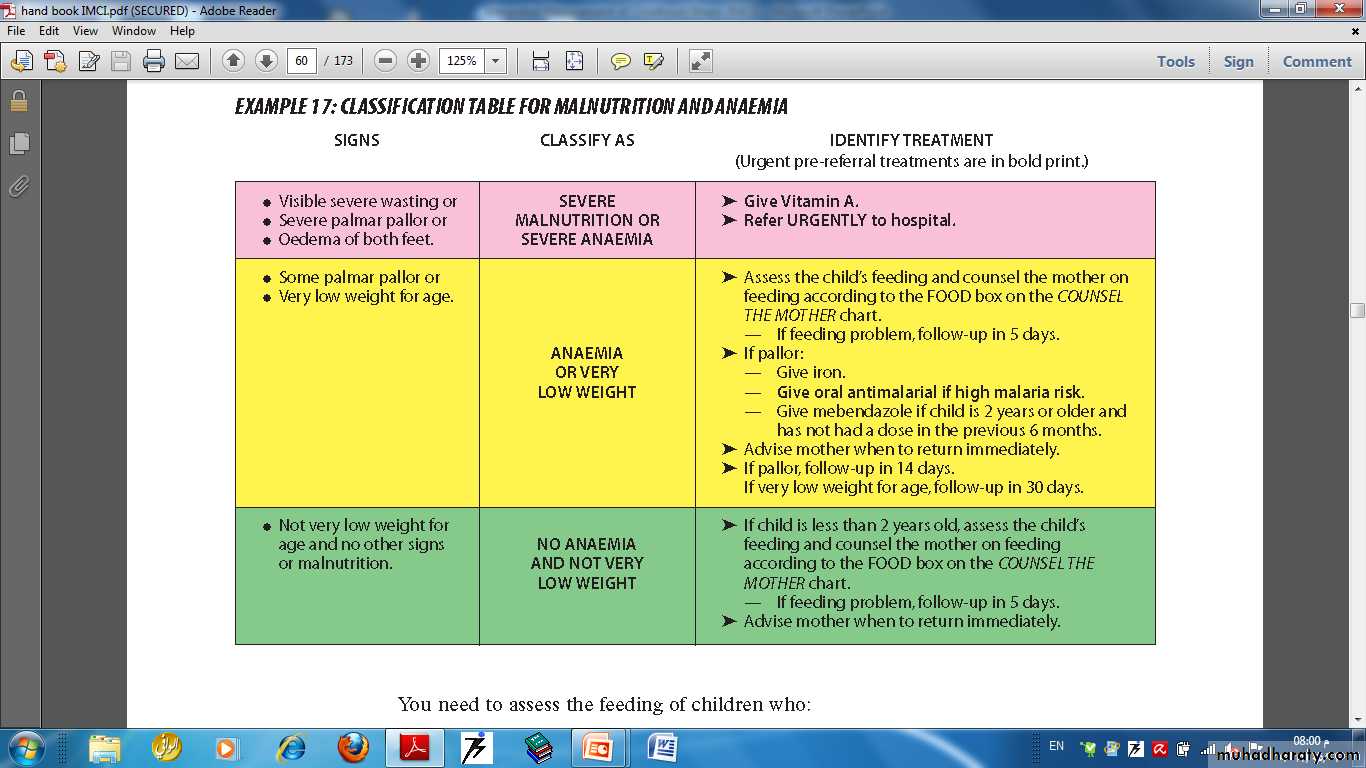
40Malnutrition and anaemia
41CLASSIFICATION TABLE FOR MALNUTRITION AND ANAEMIA
42
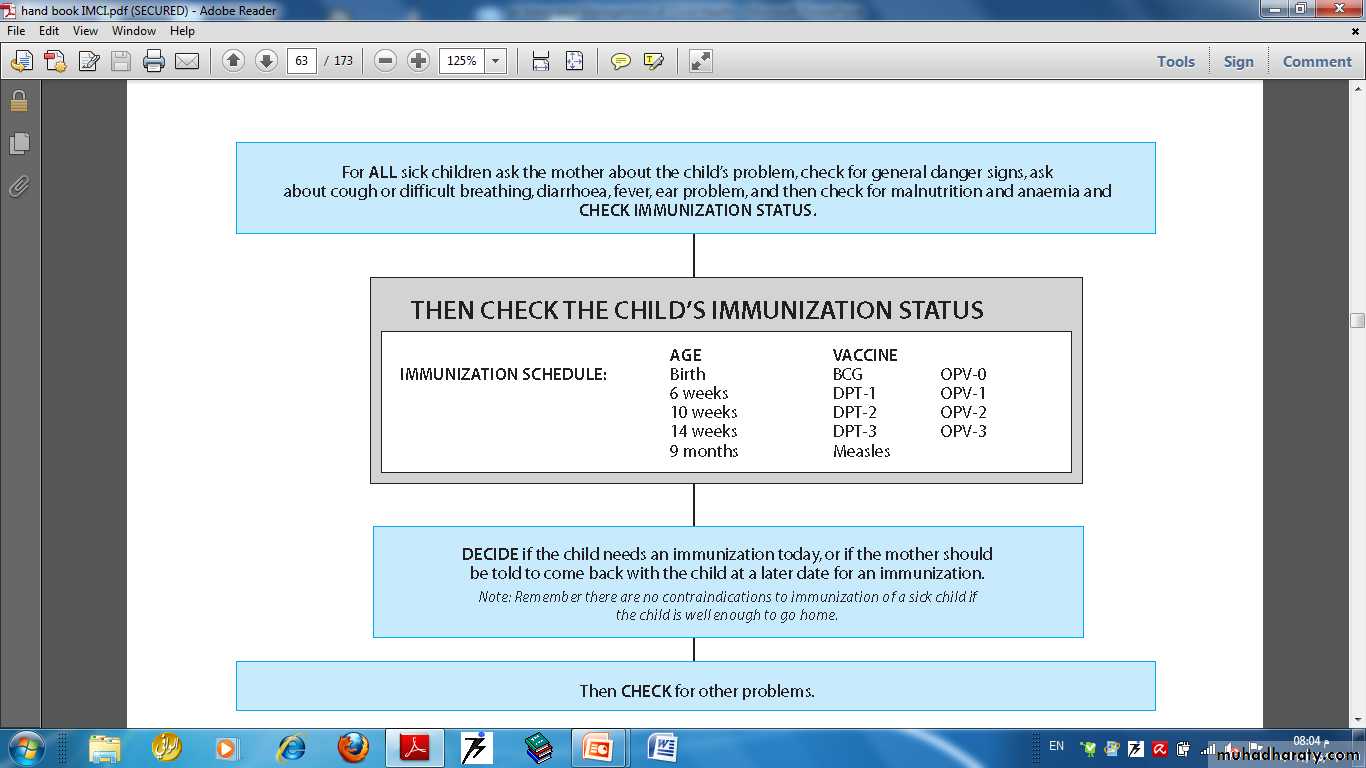
Immunization status
43There are only three situations at present that are contraindications to immunization:
■ Do not give BCG to a child known to have AIDS.■ Do not give DPT 2 or DPT 3 to a child who has had convulsions or shock within 3 days of the most recent dose.
■ Do not give DPT to a child with recurrent convulsions or another active neurological disease of the central nervous system.
OPV ■ If the child has diarrhoea, give a dose of OPV, but do not count the dose. Ask the mother to return in 4 weeks for the missing dose of OPV.
In all other situations, here is a good rule to follow: There are no contraindications to immunization of a sick child if the child is well enough to go home.
44
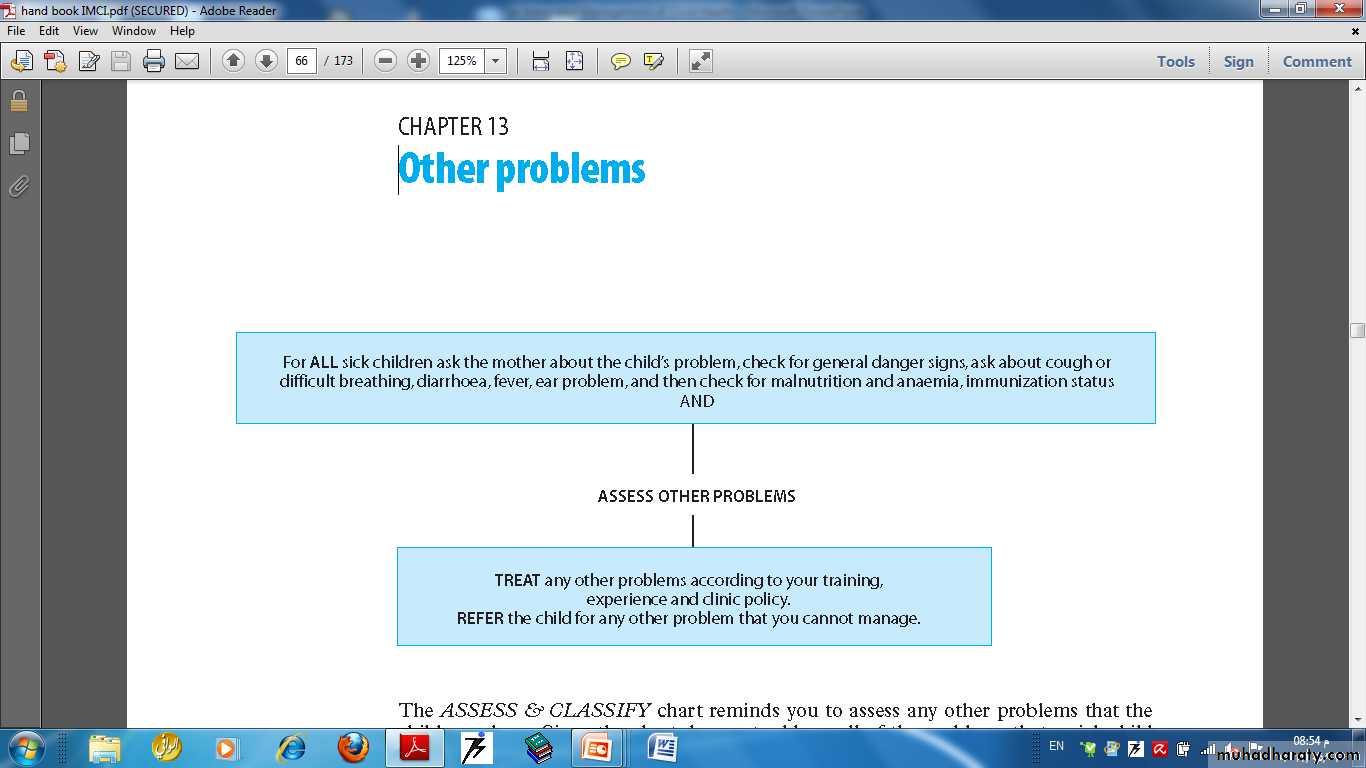
Other problems
45Counsel the mother about breastfeeding problems
If a mother is breastfeeding her infant less than 8 times in 24 hours, advise her to increase the frequency of breastfeeding. Breastfeed as often and for as long as the infant wants, day and night.
■ If the infant receives other foods or drinks, counsel the mother about breastfeeding more, reducing the amount of the other foods or drinks, and if possible, stopping altogether. Advise her to feed the infant any other drinks from a cup, and not from a feeding bottle.
■ If the mother does not breastfeed at all, consider referring her for breastfeeding counselling and possible relactation. If the mother is interested, a breastfeeding counselor may be able to help her to overcome difficulties and begin breastfeeding again.
46
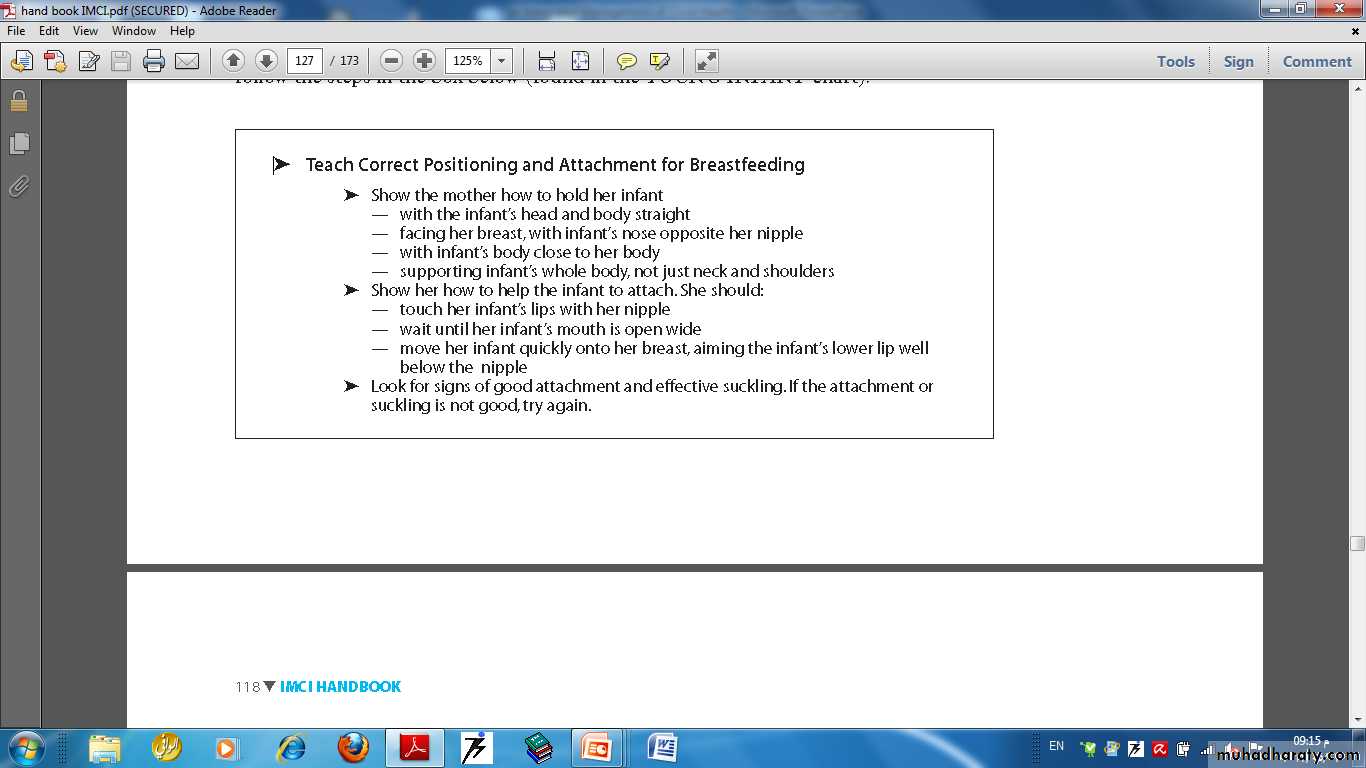
• Improving Positioning and Attachment
47The advantages of breastfeeding :
Breast milk contains exactlythe nutrients needed
These nutrients are more
easily absorbed
Breastmilk provides all the water an infant needs, even in a hot, dry climate.
Breastmilk protects an infant against infection.Breastfeeding helps a mother and baby to develop a close, loving relationship.
Breastfeeding protects
a mother’s health.
Protein, Fat, Lactose (a special milk sugar), Vitamins A , C and Iron
contains essential fatty acids needed for the infant’s growing brain, eyes, and blood vessels.
helps the uterus return to its previous size. This helps reduce bleeding and prevent anaemia. also reduces the mother’s risk of ovarian cancer and breast cancer.
48
49
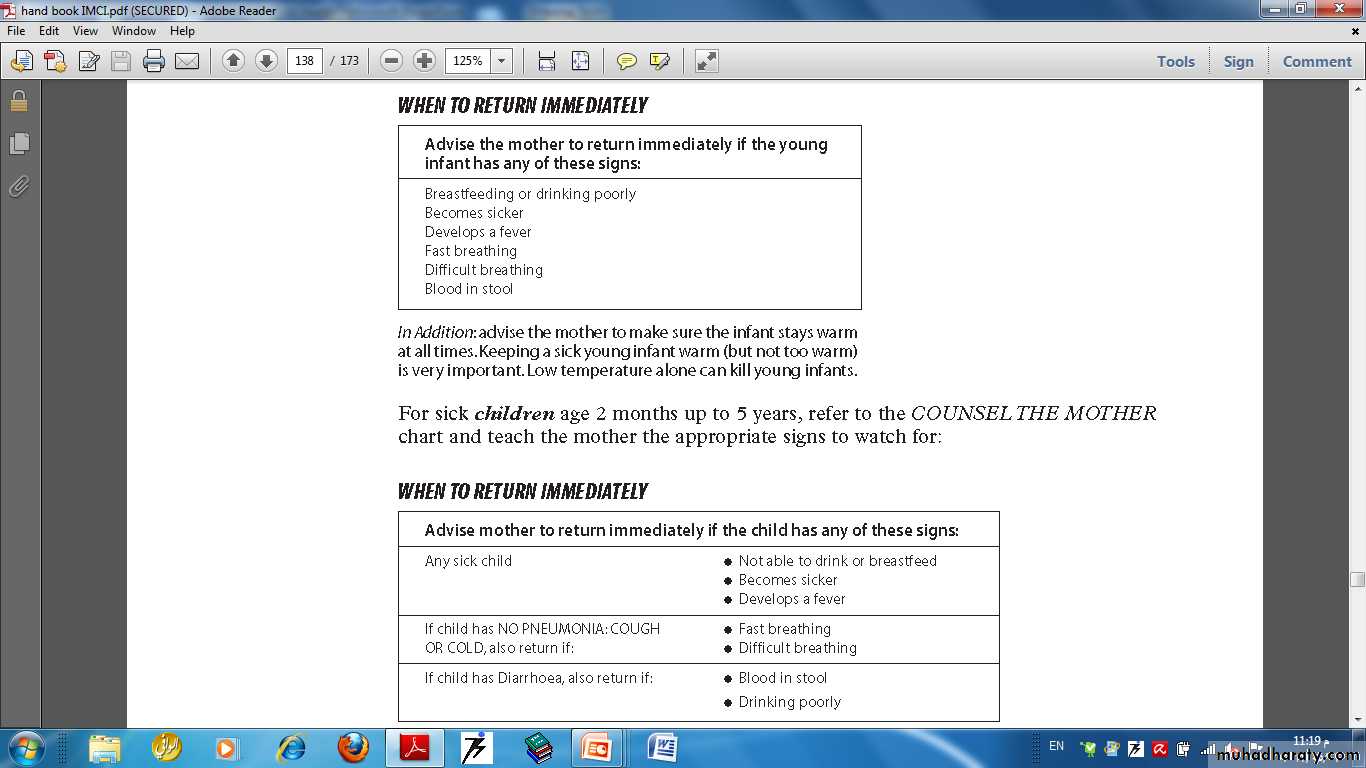
Counsel the mother about when to return and about her own health
For sick young infants age 1 week up to 2 months50
51