Lec 1 & 2 Dr. Rana Mustafa
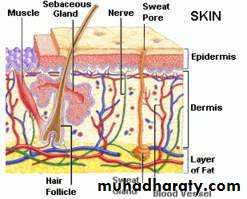
Integumentary systemIntegumentary system: This term involve the skin which covers the body with its appendages.
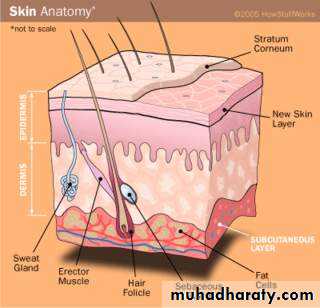
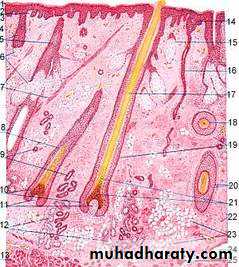
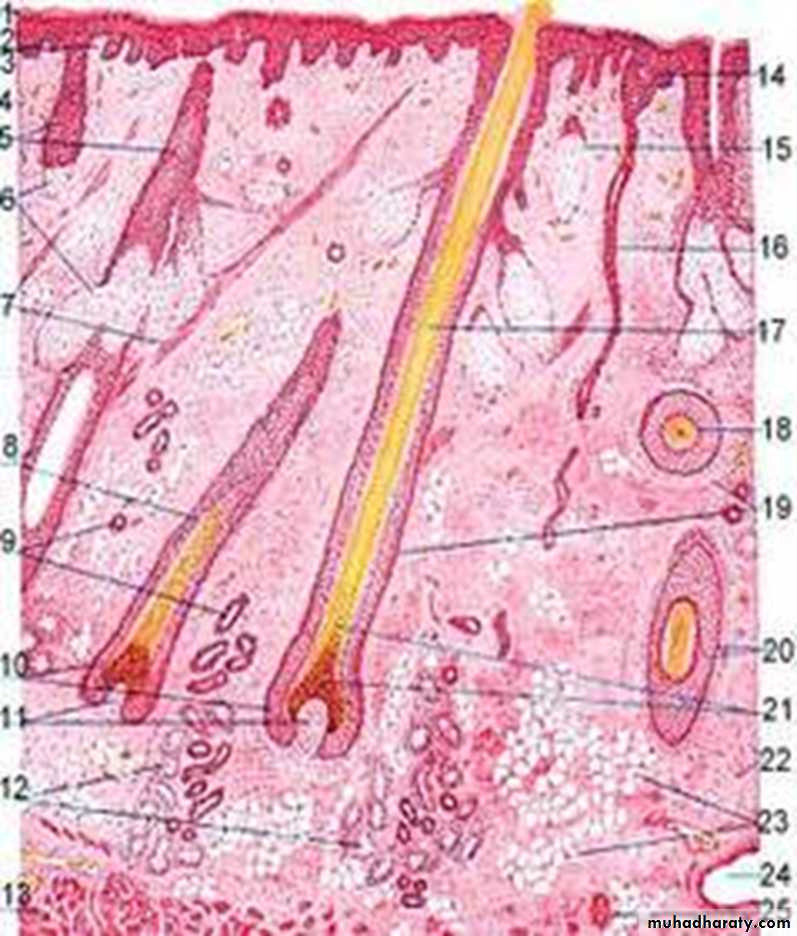
Skin (Cutis):the skin consists of two main parts (layers):
1. Epidermis: a layer derived from the ectoderm, it's the first layer for protection from invasion of foreign substances.
2.Dermis: a layer of connective tissue derived from the mesoderm.
Subcutaneous C.T. connect the skin to the underlying structures
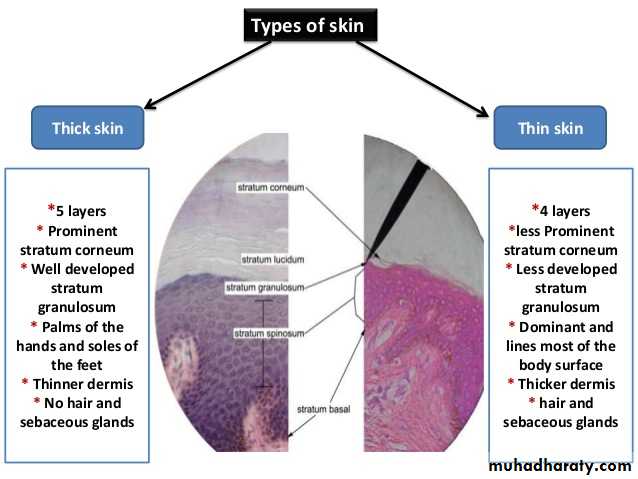
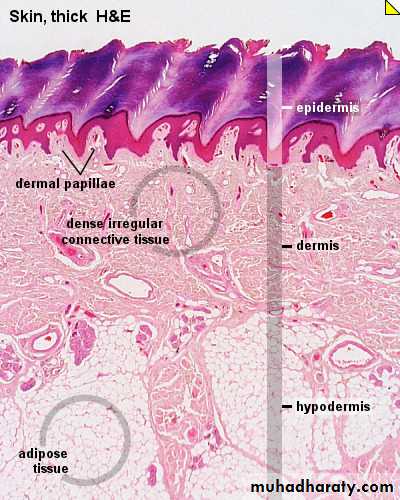
The thickness of the skin may involve the one or two layers. In thin skin (scalp) the thickness is in the dermis while in thick skin ( sole & palm), the thickness involve both dermis & epidermis but more in epidermis.
The whole surface of the skin is traversed by numerous fine furrows which run in different directions, in the finger tips, these ridges or furrows are arranged in a complicated loops & spirals which give a characteristic finger print for each individual.
Histology of the skin:
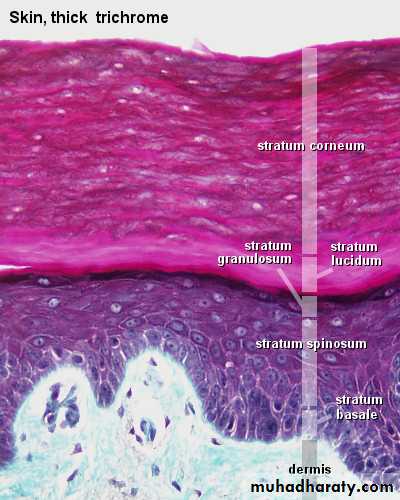
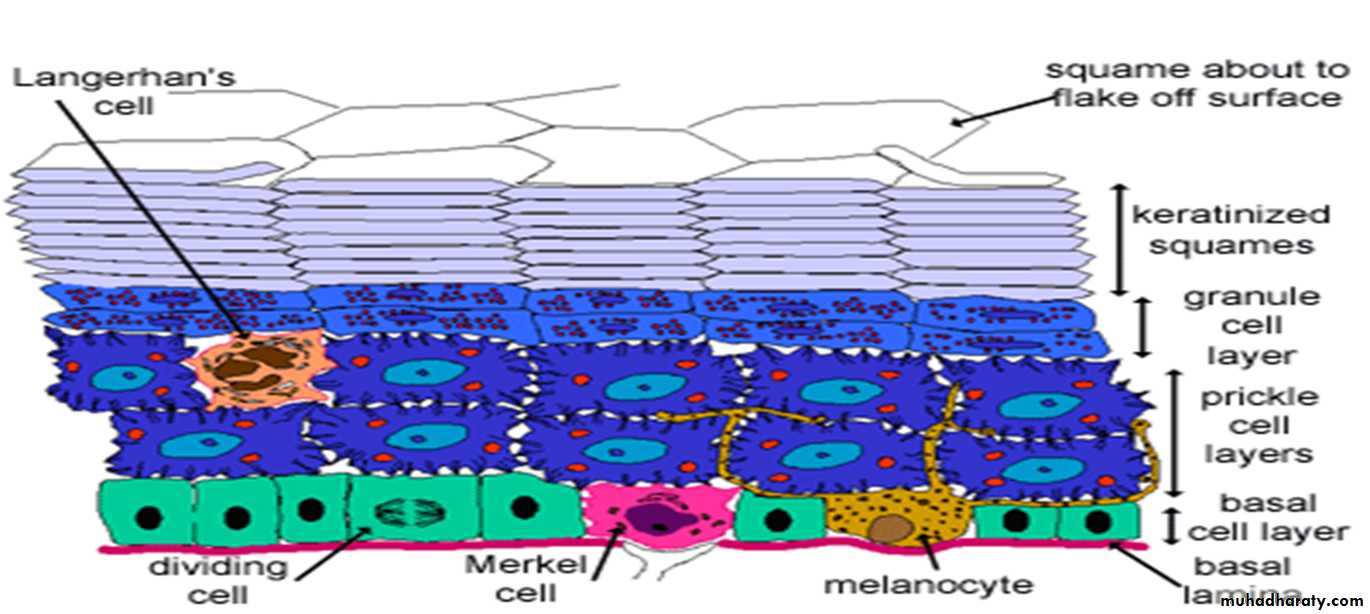
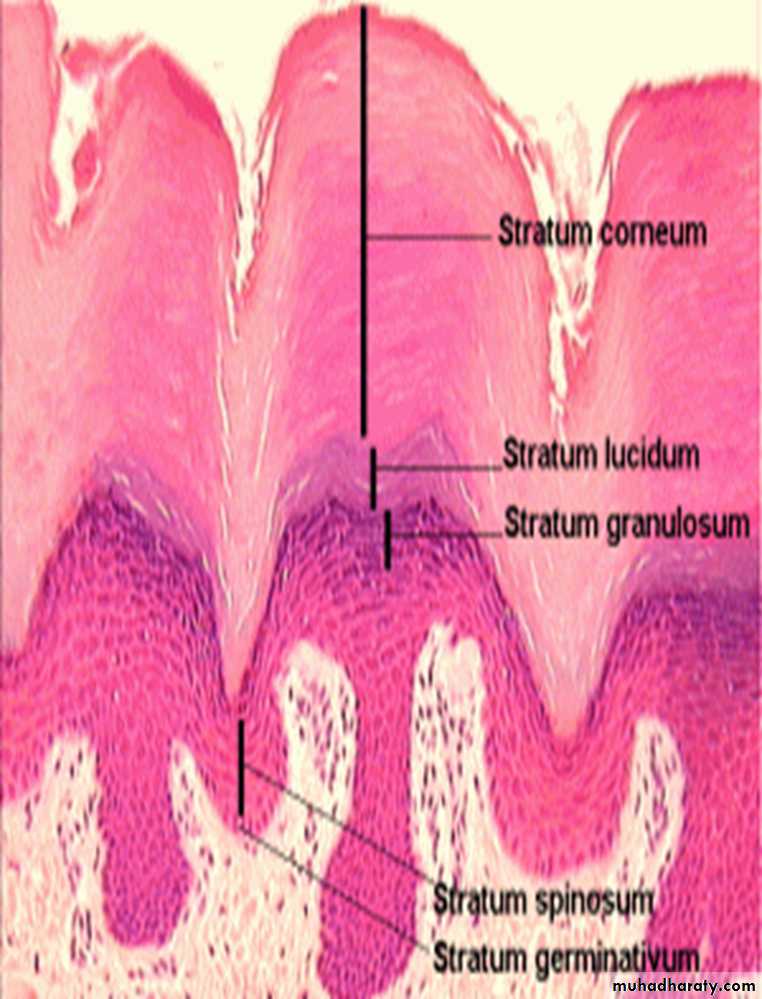
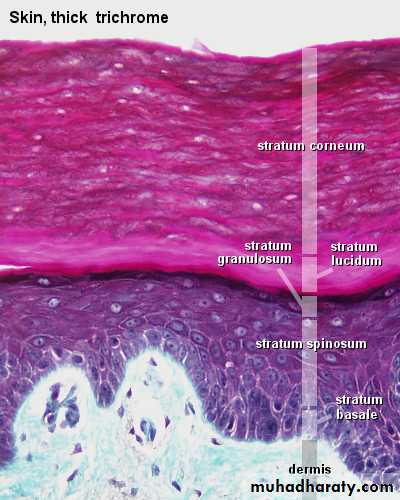
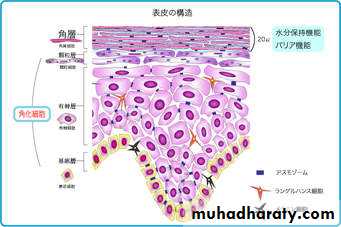
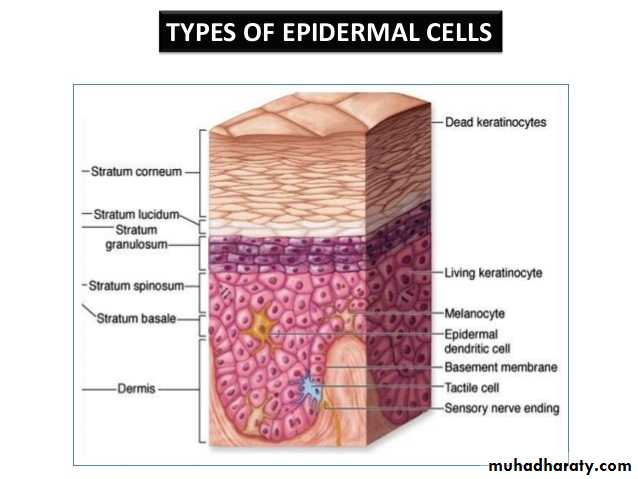
1.Epidermis: is a keratinized, stratified squamous epithelium.• Consist of:
• Stratum basale.
• Stratum spinosum.
• Stratum granulosum.
• Stratum lucidum.
• Stratum corneum.
• Stratum basale & spinosum are called stratum germinativum (germinal) or st. Malpighian.
•
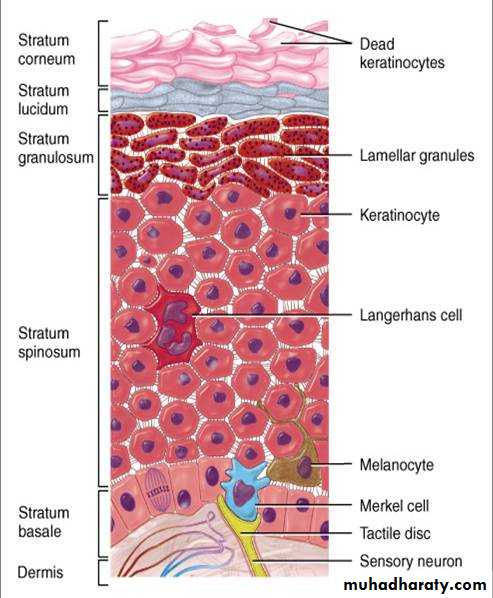
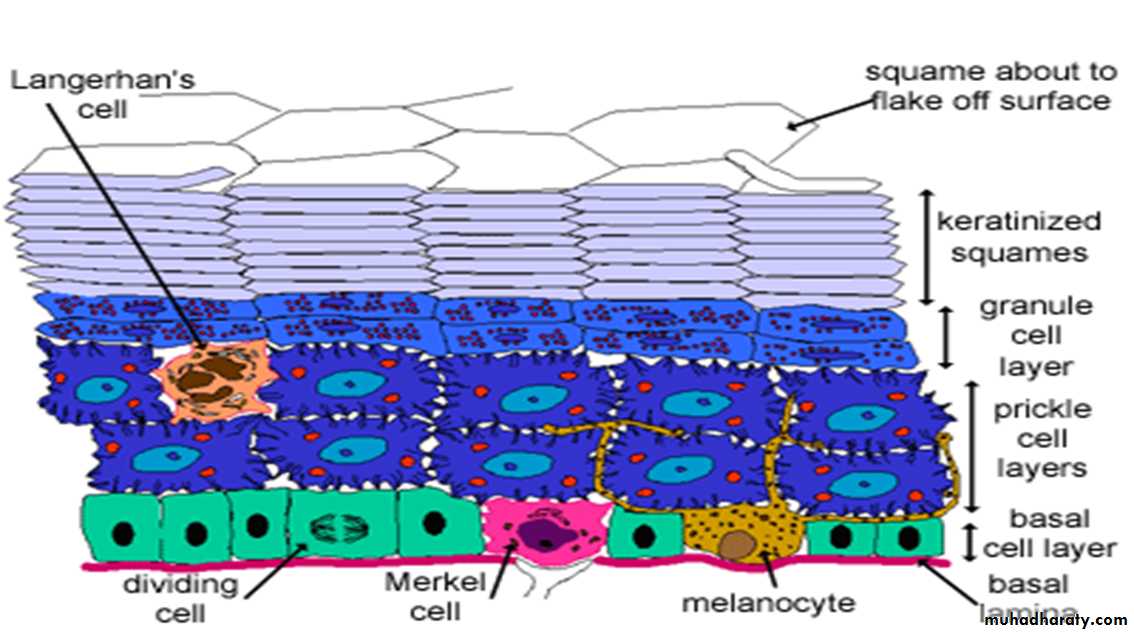
• A-Stratum basale:
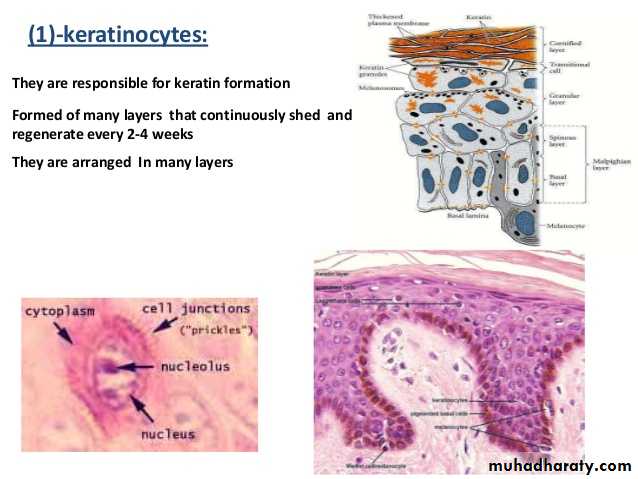
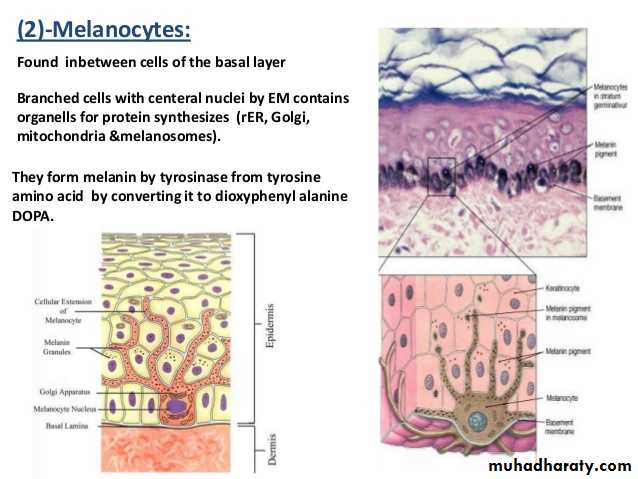
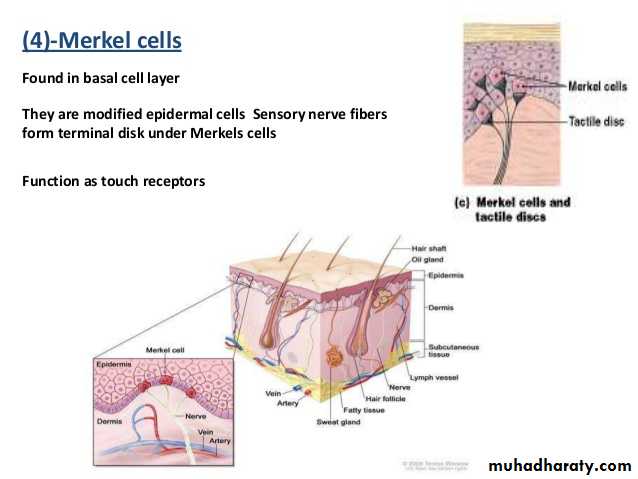
• Is a single layer of cells, closest to the dermis.• The cells present in this layer are keratinocytes cells among them lie melanocytes cells & merkel’s cells.
• This layer is separated from the dermis by a thin layer of basement membrane named as dermoepidermal junction..
Mitosis occurs mainly in the Stratum basale & occasionally in the Stratum spinosum, after that a newly formed cell will undergo a progressive maturation called keratinization or keratocytosis & move upward toward the surface as they differentiate, providing continuous regeneration.
keratinization is more rapid in the areas which are exposed to friction continuously as in the sole, also it is accelerated after injury & it is responsible for continuous renewal of the epidermal cells.
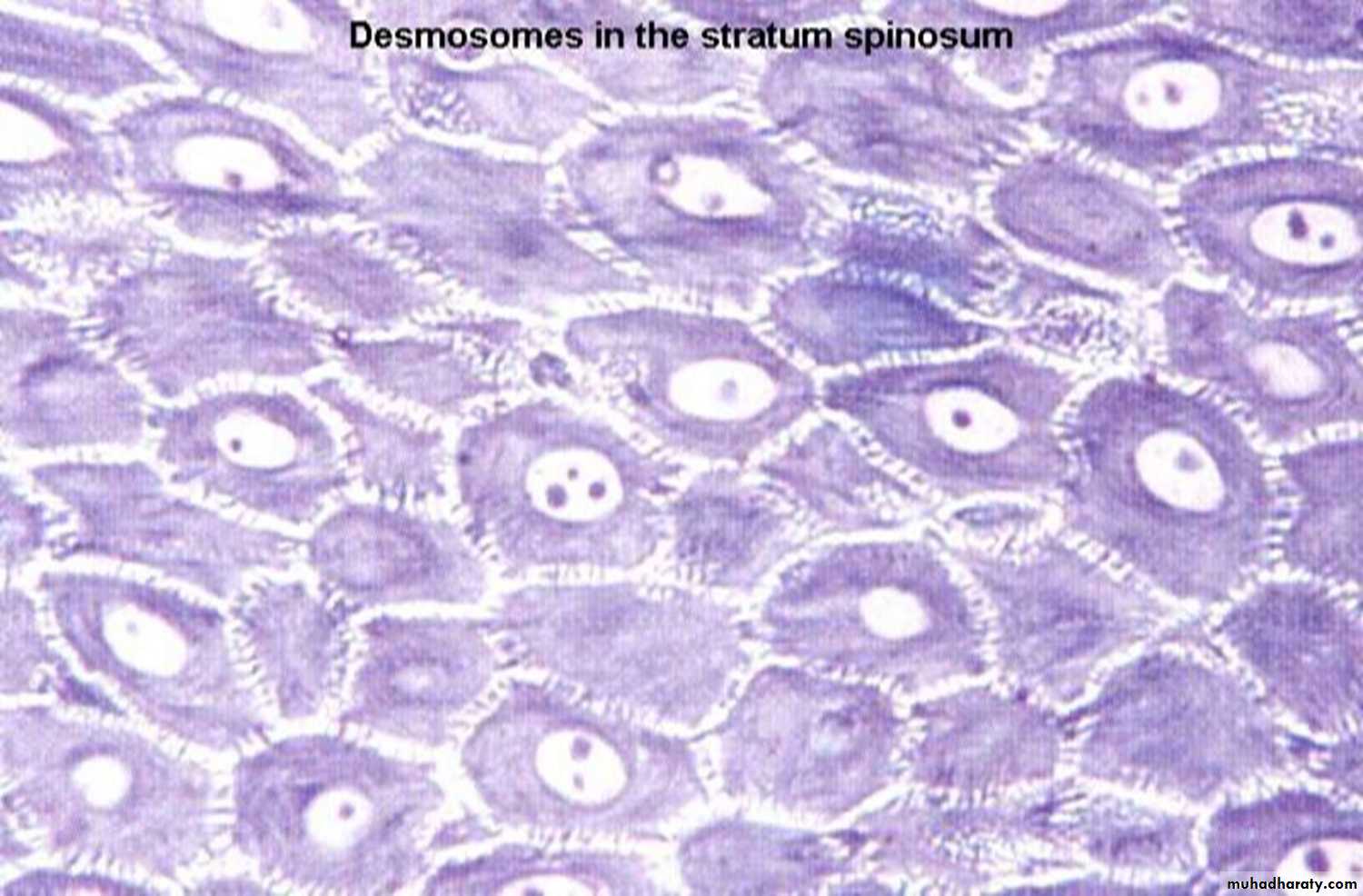
b-Stratum Spinosum:
• Is the next to basale about (8-10 layers of cells).• It consist of polygonal cells (or polyhedral) with rounded deeply chromatic nucleus, its develop from the proliferating keratinocyte.
• Have a lots of desmosomes on their outer surface, which anchor the cells to each other & when these cell shrinks slightly, during fixation, these cells become irregular & desmosomes that tight cells to each other becomes clear by using EM, and these desmosomes look like 'prickles' or 'spines', hence the name prickle cells layer.
• Such intercellular process maintain cohesion among the cells & help them to resist the effect of abrasion, therefore, the epidermis of the area subjected to continuous friction & pressure (sole) has a thicker stratum spinosum.
Stratum spinosum desmosome
c-stratum granulosum:
• Consist of (3-5 layers of cells).• the cells of stratum granulosum accumulate more dense basophilic granules called keratohyalin granules.
• These granules contain lipids, which along with desmosomal connections, help to form
a waterproof barrier that functions to prevent fluid loss fromthe body
• Its less developed in thin skin &mostly merge with st. lucidum.
d- Stratum lucidum :
• Consist of 1-2 rows of flattened non – nucleated cells.• The cytoplasm contain Eleidin pigment which is translucent substance is formed from keratohyaline & eventually transformed to keratin.
• This layer is well seen in thick epidermis and represent a transition from the st. granulosum ( nucleated) to st. corneum (non nucleated).
E- Stratum corneum :
• It is the outermost layers of the epidermis, consisting of dead cells (corneocytes) that lack nuclei & organelles.• Desquamation (the process of cell shedding from the surface of stratum corneum) balances keratinization (the process of cell proliferating keratinocytes that form in the stratum basale).
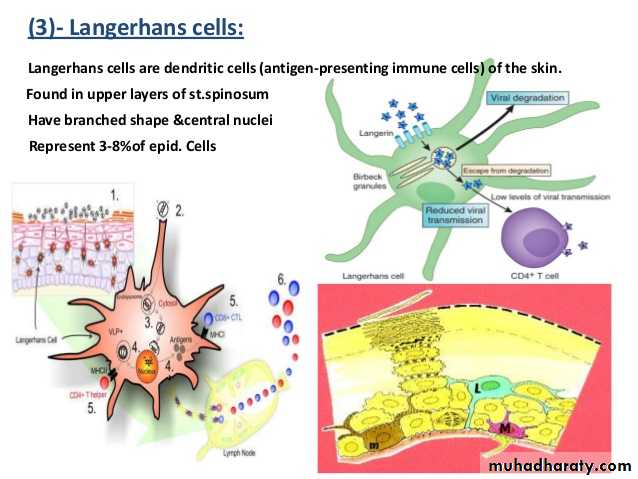
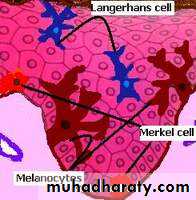
Types of epidermal cells
It consists of basophilic columnar or high cuboidal cells with oval deeply chromatic nuclei.
By EM the cytoplasm shows abundant ribosomes which are responsible for the protein synthesis activity of this layer , also the tonofibrills & tonofilaments are present which are important for the synthesis of filamentous elements of the matrix of stratum corneum.
Melanocytes can be recognize Dopa reaction which use dioxyphenyl alanine (Dopa) as reagent that stain cytoplasm as gray, gray-brown or black color.
So melanocytes are Dopa +ve cells.
Types of epidermal cells
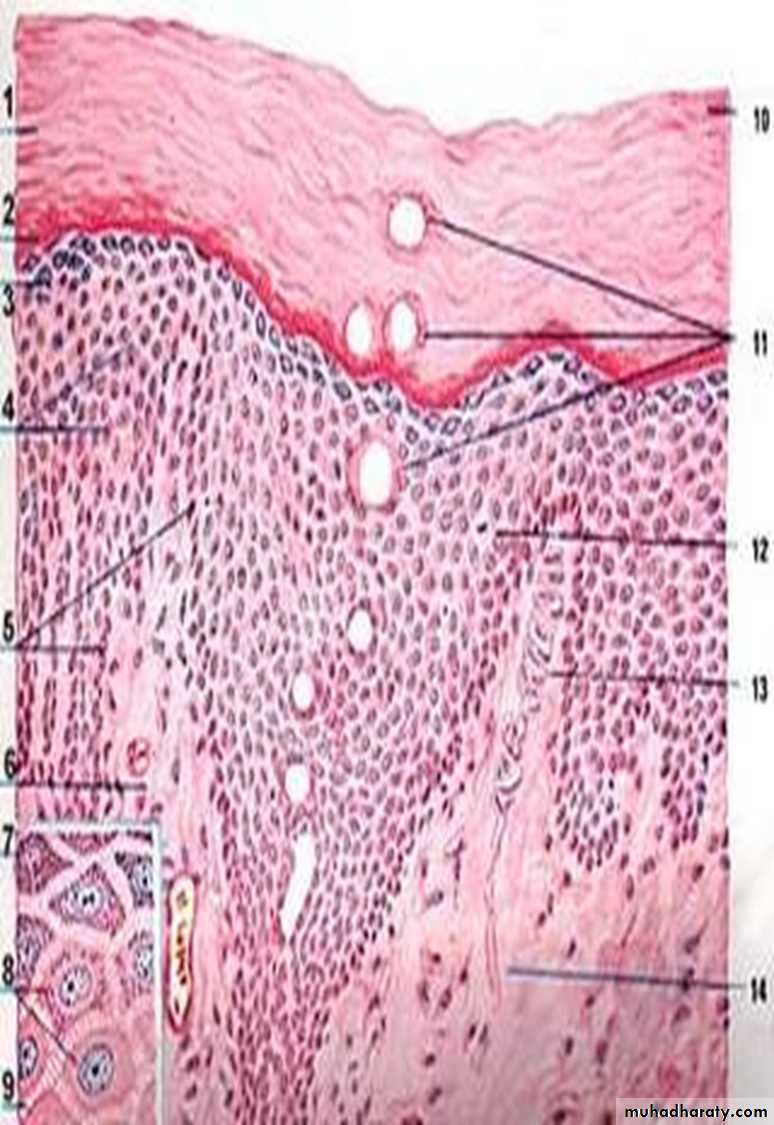
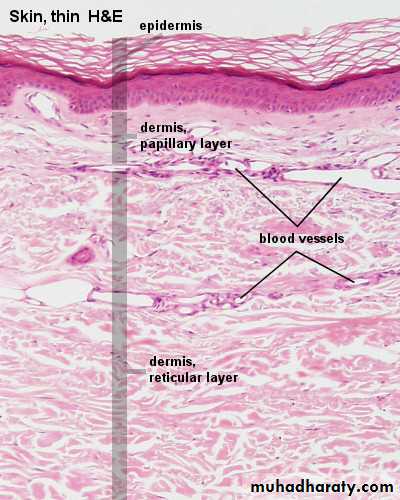
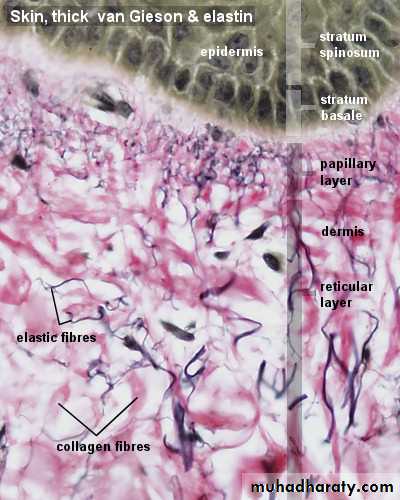
2- Dermis
It Composed of irregular connective tissues & lies next to epidermis & separated from it by irregular line & supply overlying avascular epidermisThe dermis composed of three major cell types : Fibroblast, Mast cell & Adipocytes which embedded in C.T. matrix made up of collagen( which provide strength) & elastin ( which provide elasticity) that is why dermis is responsible for elasticity & firmness of the skin & housing most of skin appendages.
• .
The dermis also contains epidermal derivatives such as hair follicle, sweat gland, sebaceous gland, rich supply of nerves & blood capillaries, Arrector pilli smooth muscle associated with hair follicles.
The dermis divided in to two layers:-
• 1- Papilary layer.
• 2- Reticular layer.
• 1-Papillary layer
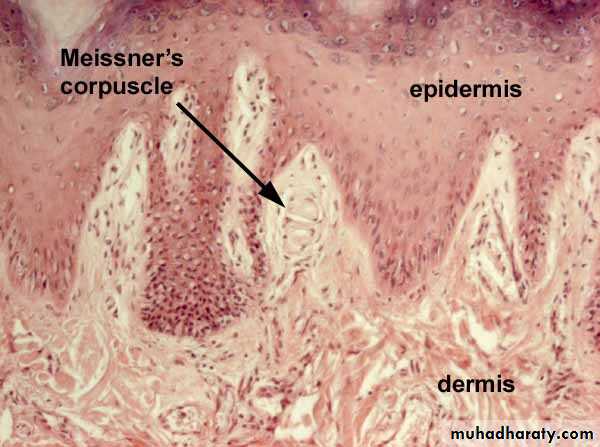
Consist of thin loose C. T., it so called papillary because it penetrates in to the epidermis as outgrowth projections called Dermal papillae.Types of Dermal papillae:
• Vascular papillae: which contain loop of capillaries.
• Nervous papillae: contain nerve ending sensory for touch (Tactile corpuscle) or Meissner’s corpuscle reiceve light touch and pressure.
Meissner’s corpuscule
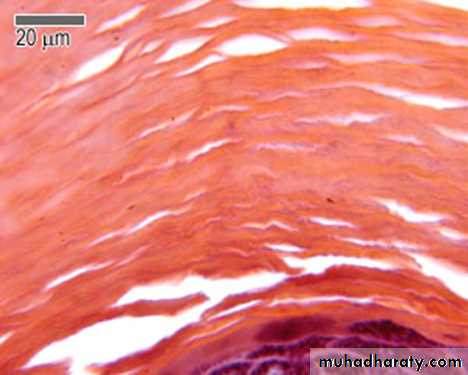
2- Reticular layer
Thicker & deeper, composed of irregular dense C.T. so it has more fibers & less cells than the papillary layer& housing the deepest part of sweat gland & hair follicles.
Subcutaneous tissue(Hypodermis)
Consist of loose C. T. layer which bind the skin to the subjacent organs & allowing it to slide over them & easy movement over the underlying tissues, it is more dense in the palm & sole.• It contains fat cells which vary in number & size according to the area of the body & nutritional condition of the individual.
• Fat is absent in the eyelids, scrotum.
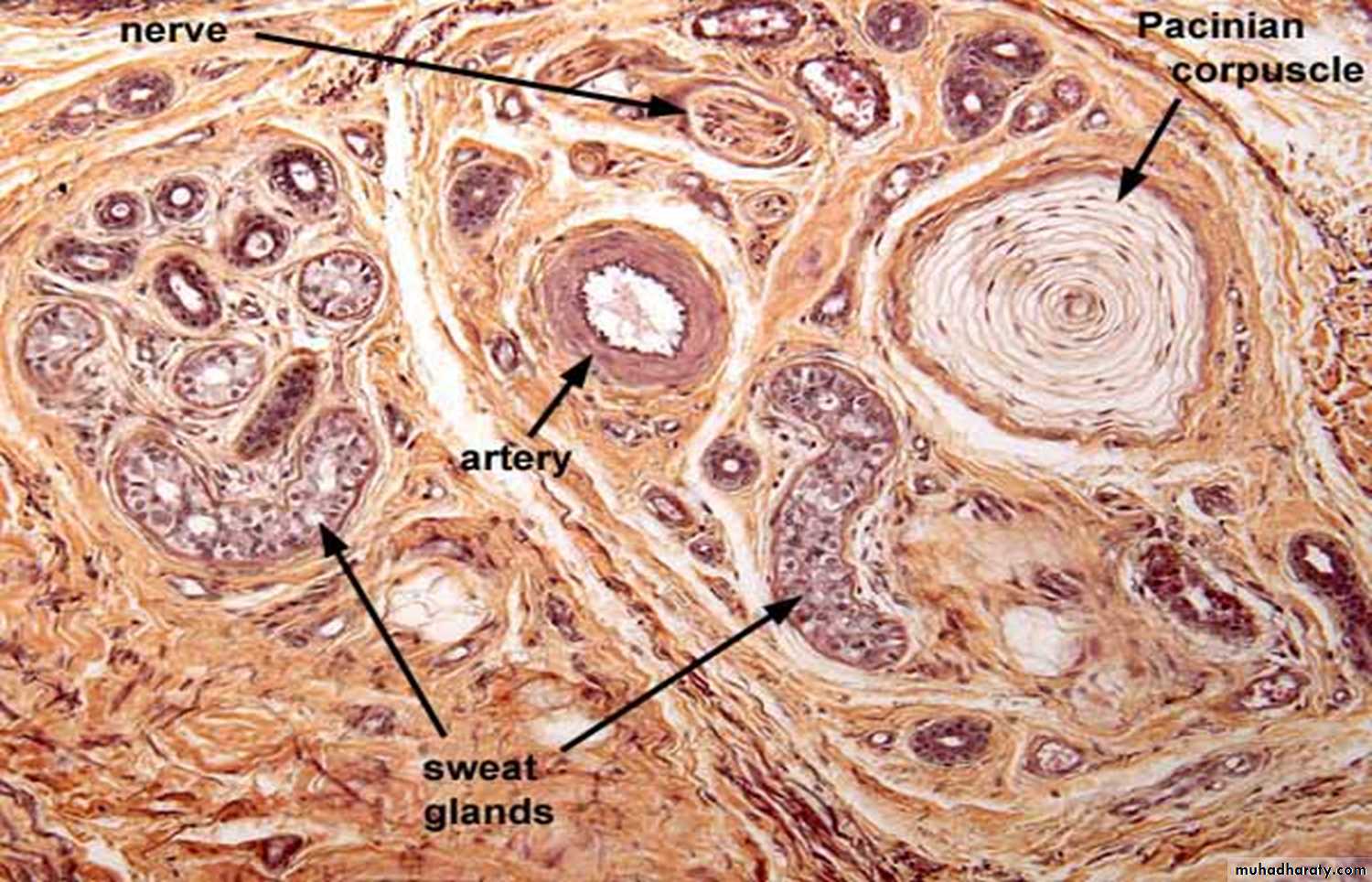
• Pacinian corpuscle lies in this layer, Sometimes the secretory part of the sweat gland, blood vessel & bulb of the hair follicle also present.
Types of nerve corpscules:
Meissner corpuscle(Tactile corpuscle) present in nervous papillae of dermis & contain nerve ending sensitive for light touch and pressure.• 2. Pacinian corpuscle present in subcutaneous tissue & its ovoid shape structure consist of concentric lamellae of compact collagenous fibers surrounding a central core of nerve fibers ending & the layers of lamellae resemble the appearance of a slice of onion & contain nerve ending sensitive for deep touch , pressure &pain.
:Color of skin
The skin color is due to a combination of :1-Carotene pigments deposit in stratum corneum.
Dermal blood vessels.
Melanin pigments present in melanocytes which distributed in stratum basale.
Functions of the skin:
These functions can be summarized in one word PHRASES.
Protection: of the underlying structure from injury, entrance of pathogen.
Heat regulatory function: sweating & cutaneous blood flow help in temperature regulation.
Receive sensation: via nerve fiber ending which become sensitive to touch , pain, heat & cold.
Absorption: of medication applied topically & sub. cut. injection.
Secretion of sebum: by sebaceous gland.
Excretory function: water, salt, fatty substances & urea are excreted through the secretion of glands of skin.
Synthesis of vitamin D : by the aid of UV light of sun.
The end
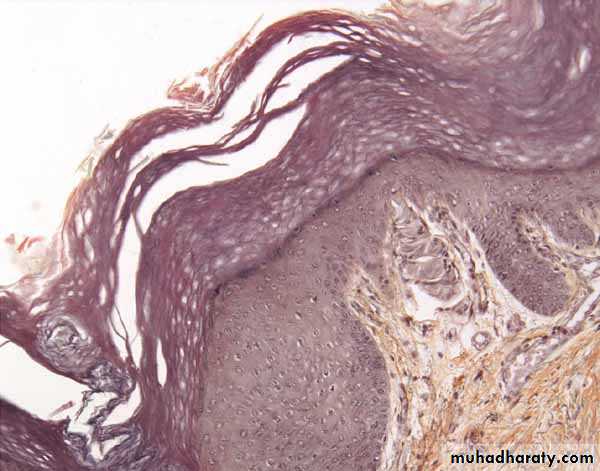
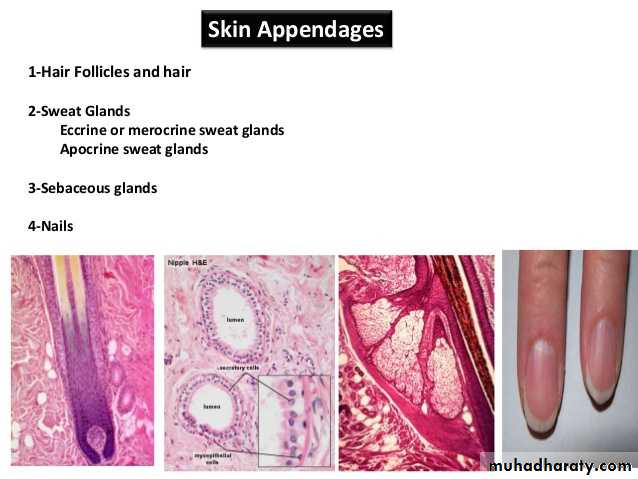
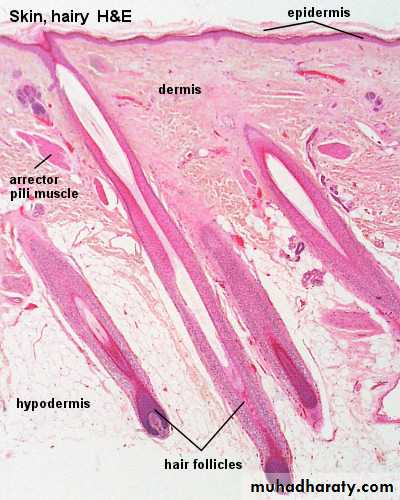
Hair
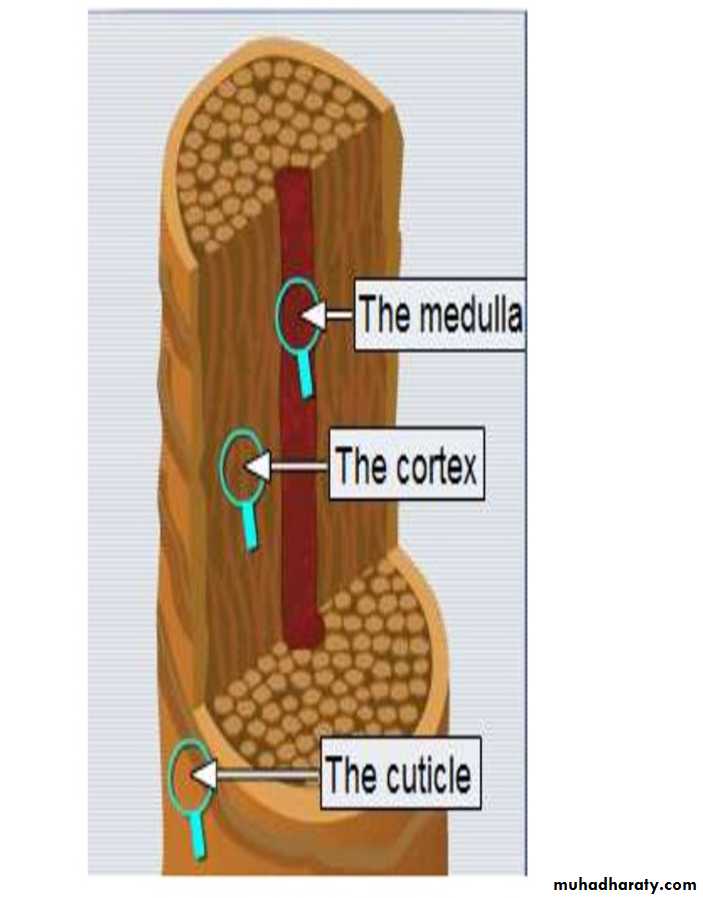
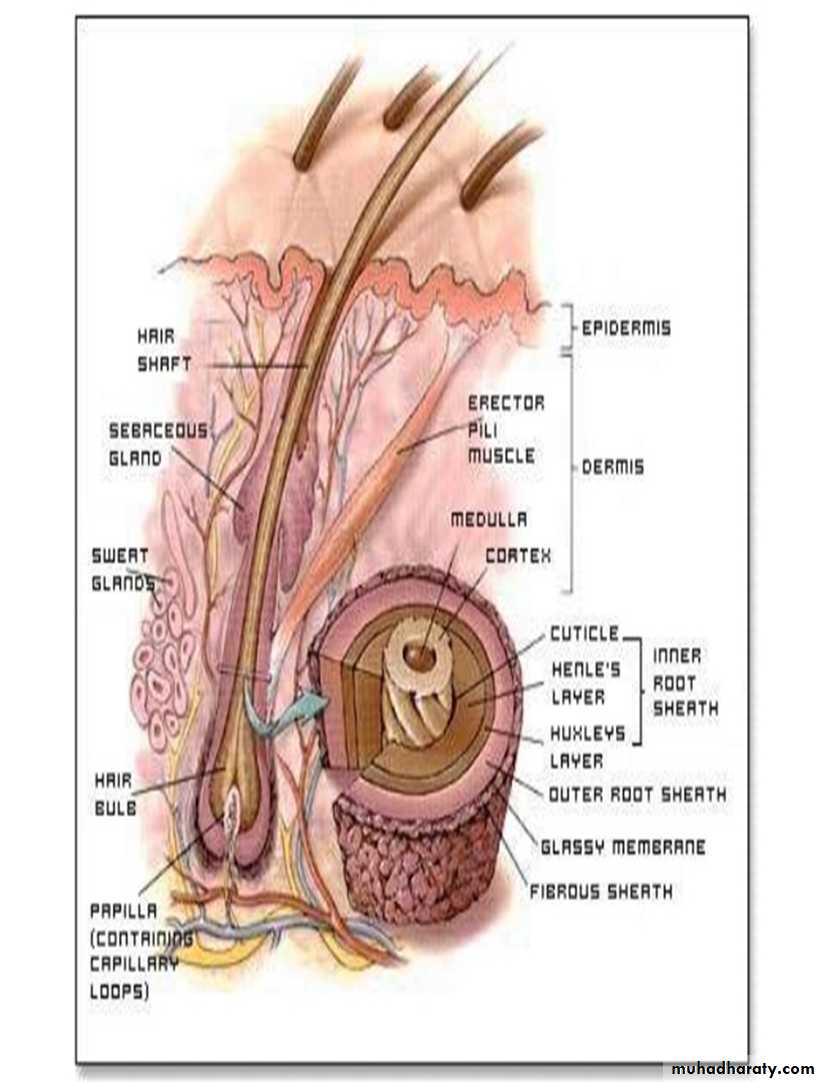
Hair are filamentous keratinized structures that project from the epidermal surface of the skin and are embedded into dermis or hypodermis.Structure of Hair
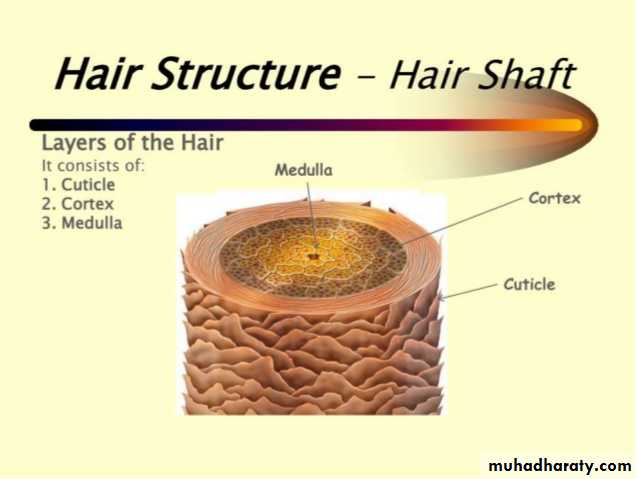
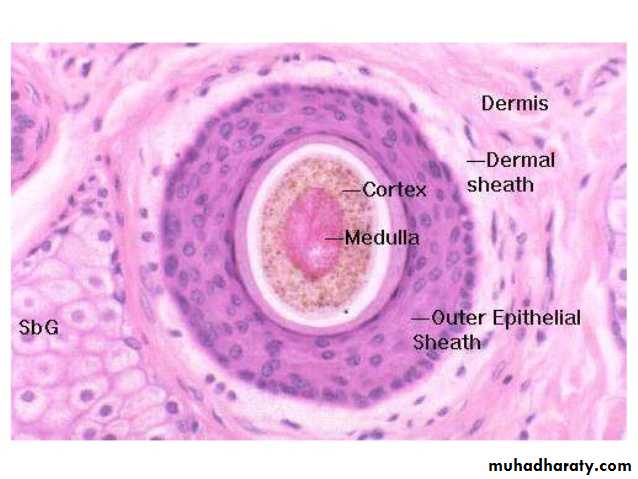
Hair itself consists ofa central pigment containing part (medulla) which surrounded by a multilayer part (cortex) and an outer single layer (cuticle).
.
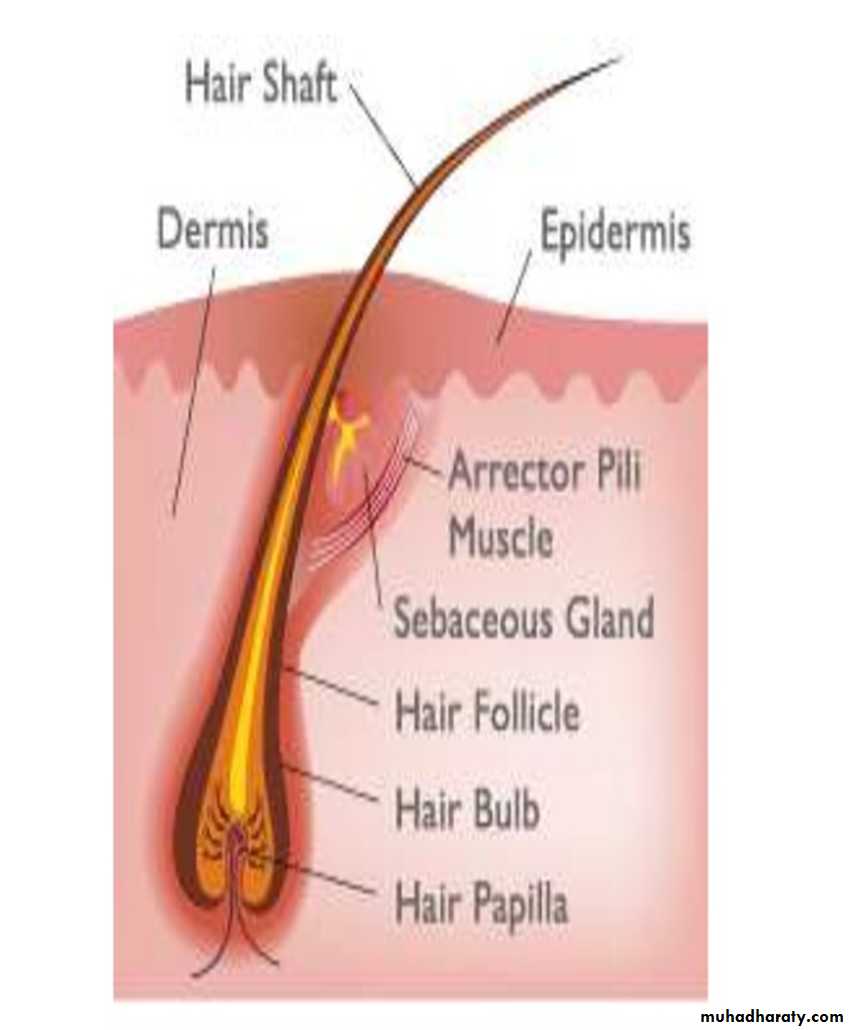
Hair has two recognized areas are shaft & root.
Shaft: Is the superficial part of hair projects above the surface of the skinRoot: Is the deep part of hair lie below the surface, penetrates in to the dermis and even in to the subcutaneous tissue.
Associated hair structures:
• 1- Hair follicle.
• 2-Arrector pilli muscle.
• 3- Sebaceous gland.
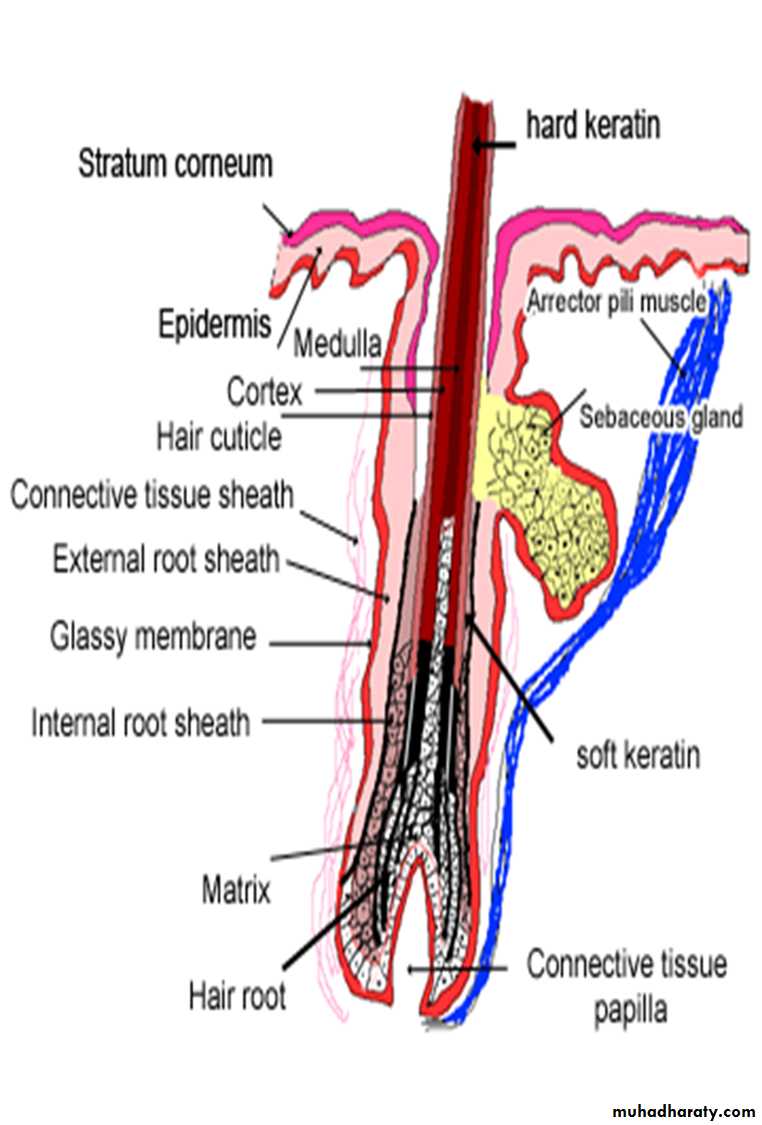
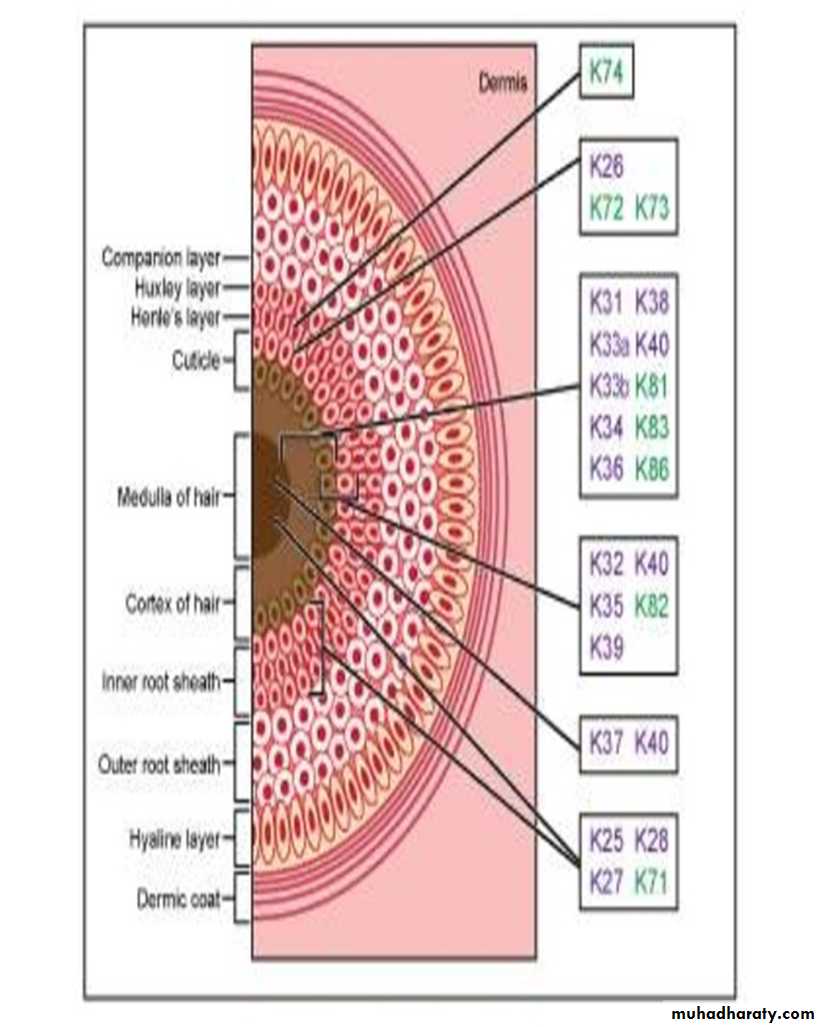
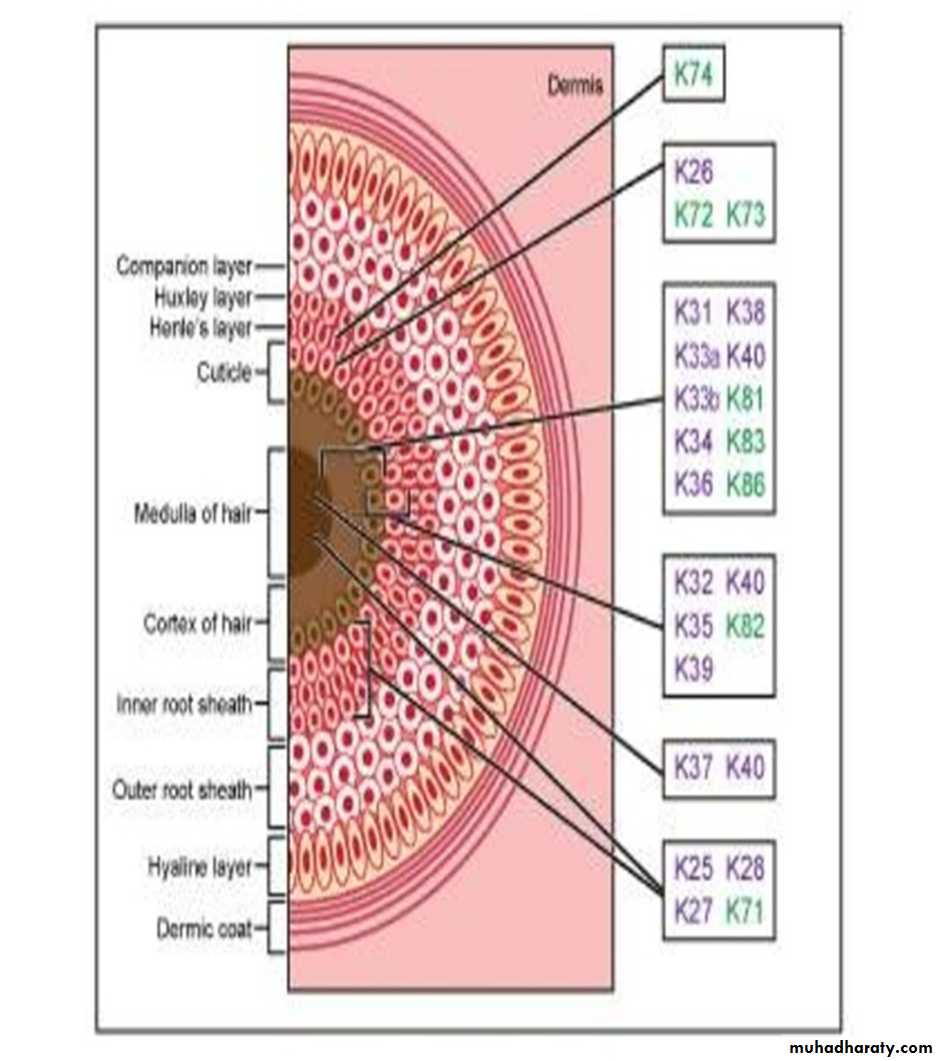
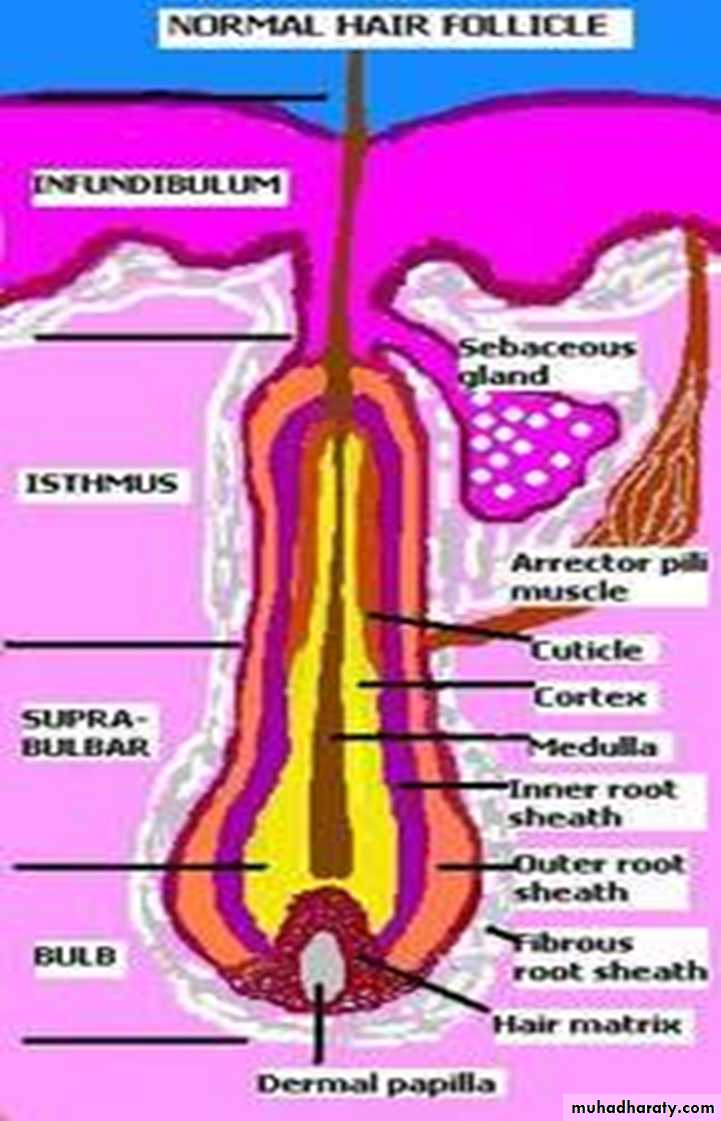
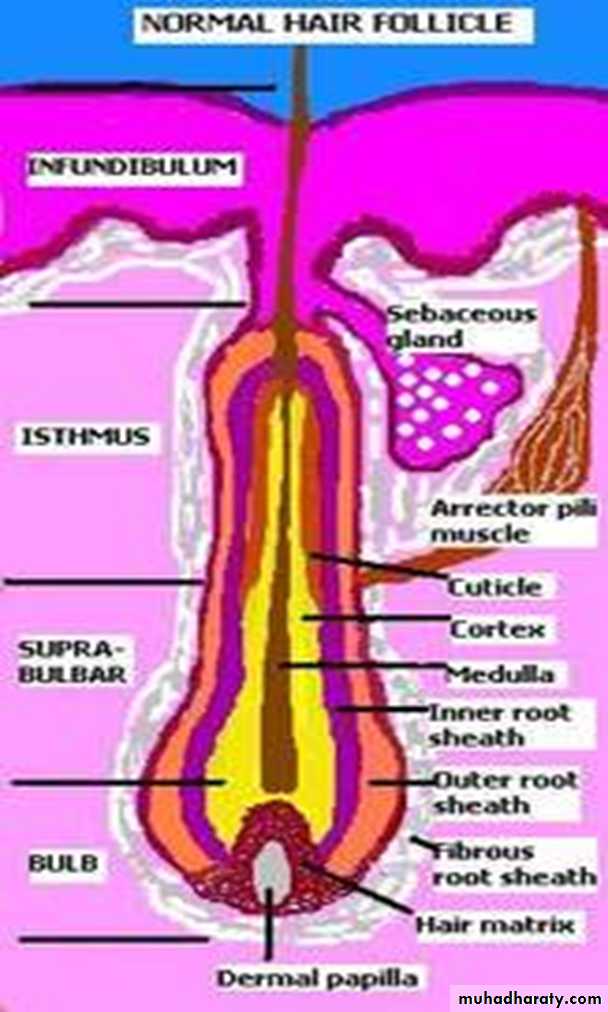
• 1- Hair follicle: dermal & epidermal sheath surround the hair root.
• These sheaths are :
• a - Internal root sheath:
• b- External root sheath.
• C- Fibrous root sheath.
a - Internal root sheath:
This sheath surround the hair toward the hair follicle & it consist of keratinized cells derived from the hair matrix.
This layer of cells disintegrates where the ducts of sebaceous glands enters the hair providing a lumen into which sebum and apocrine sweat are discharged.
Internal root sheath has three layers from outside to inside: -
• Huxley’s layer• Henle’s layer
• Cuticle layer
b- External root sheath:
This is a tubular invagination of the epidermis that surround the internal root sheathc- Fibrous root sheath:
This sheath form outer coat surrounding hair follicle & derived from the dermal C.T. & separated from external root sheath by a glassy basement membrane.
• The base of the follicle enlarged into an onion-shaped structure called "bulb" which contain:
1) Hair papillae indentation at base of bulb contains ( C. T. + many B.V.) & providing nutrition for the growing hair.
2) Matrix a region in bulb which is formed of stratum basale of the epidermis which are continuously dividing cells to produce new hairs to replace the shedding one.
• The color of the hair is due to different amount of melanin pigment produced by the melanocyte cells, distributed in the matrix of the bulb & in the hair follicles so the hair either black, brown or yellow.
Other associated structure of hair:
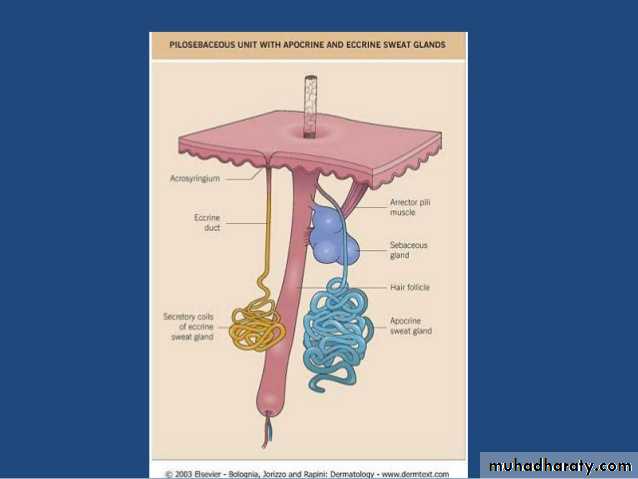
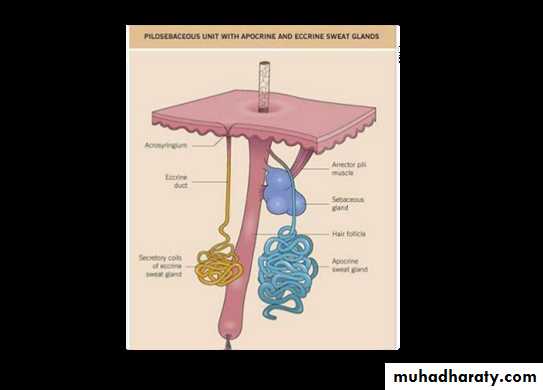
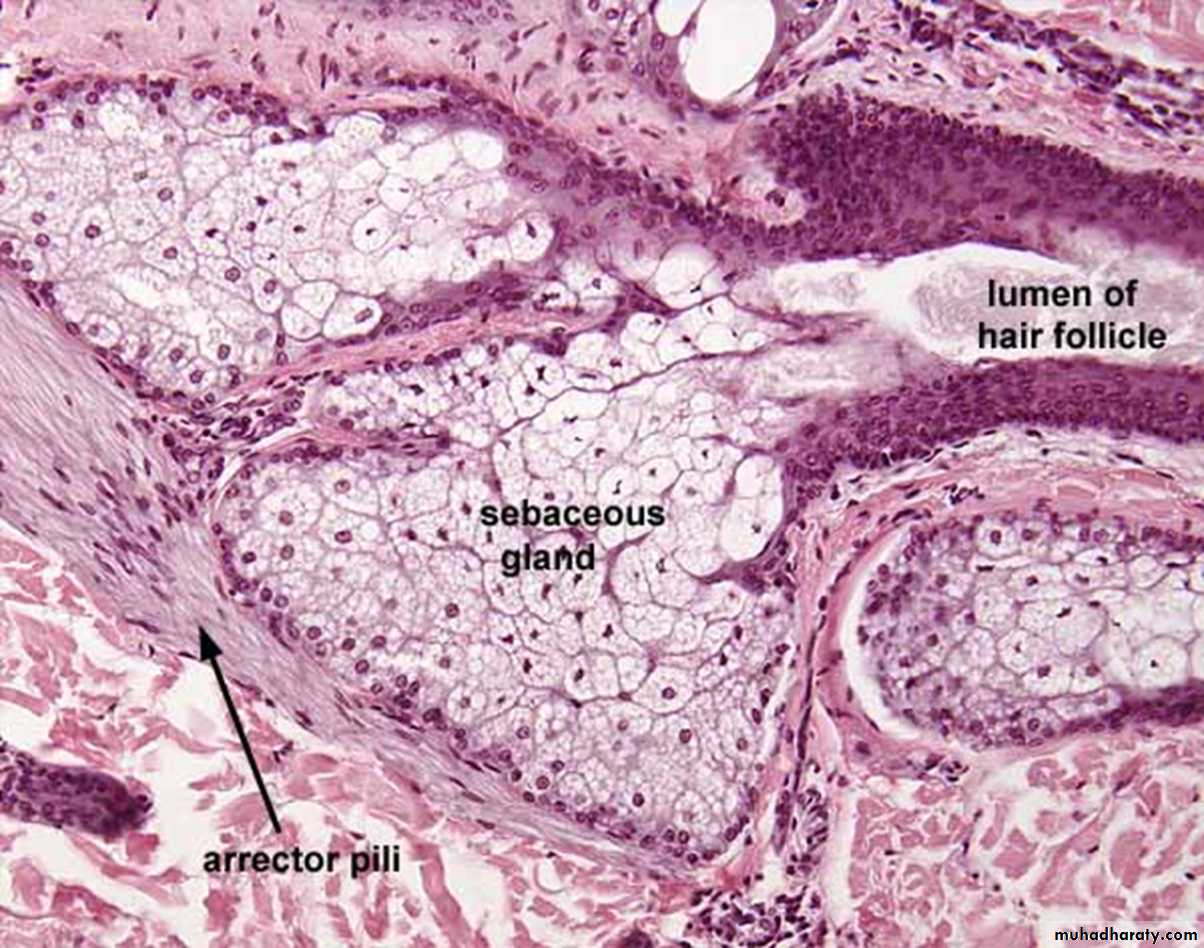
2- Arrector pilli muscle:This muscle is a bundle of smooth muscle fibers, run obliquely starting from below the dermal papillae toward the hair follicle, by their contraction help in erecting of the hair into a vertical position, they contract under stress, cold & fear & assist sebaceous gland to empty their secretion& its innervated by autonomic nerve fiber.
3- Sebaceous gland.
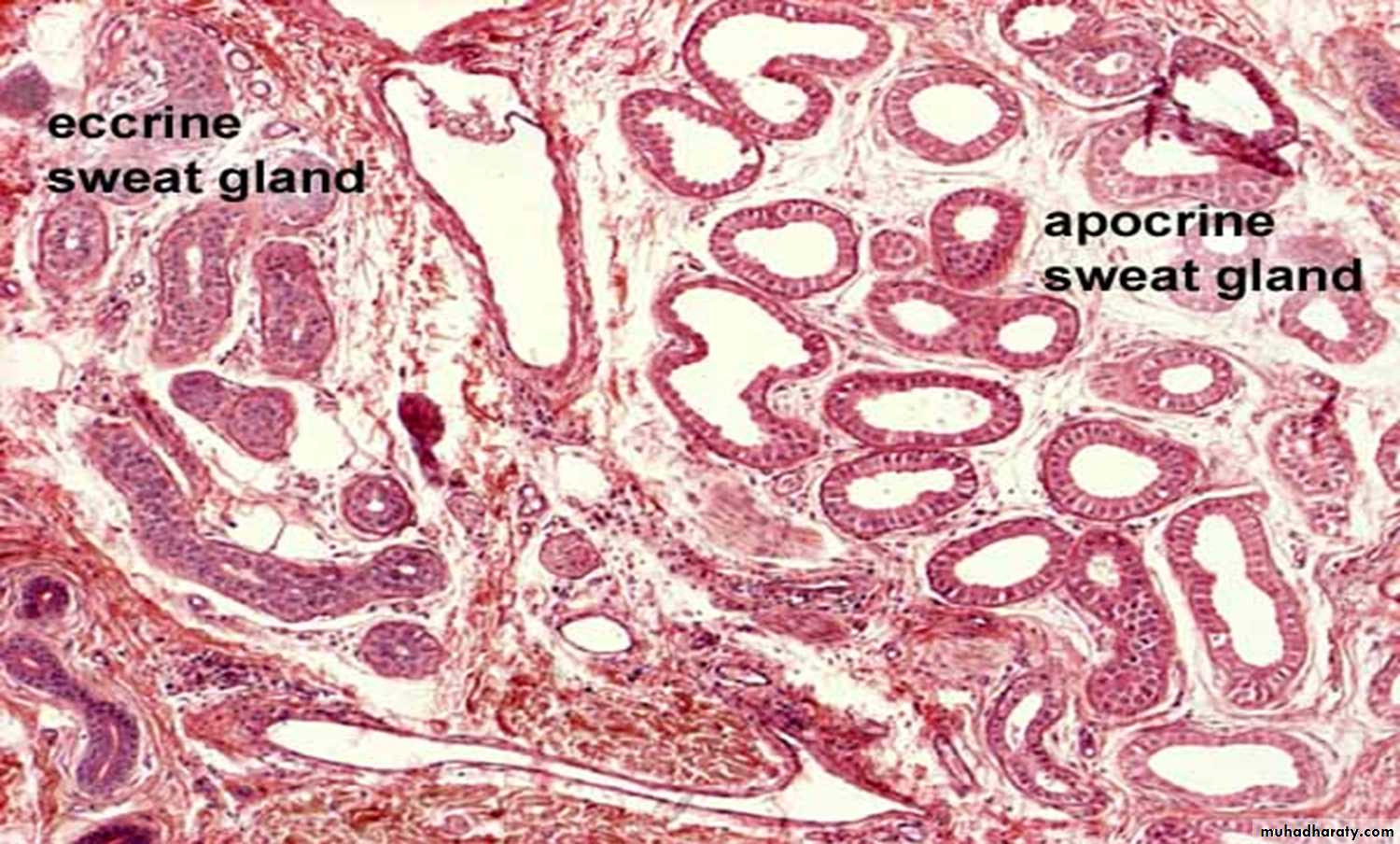
2- Sweat gland:
Sweat glands are a type of exocrine glands which are glands that produce and secrete substances onto an epithelial surface by way of a duct & its two types:a-Merocrine sweat gland.
b- Apocrine sweat gland.
Comparism
Merocrine sweat gland• 1-Present all over the body , mainly in palm & soles then forehead & less in extremities & trunk.
• 2-simple , coiled , tubular gland consist of secretory parts + ducts.
• 3-Empty directly onto skin surface through sweat pore.
• 4-Their product of secretion is secreted without destruction of any part of the cell by process of exocytosis.
• 5-The secretion of the gland is clear, watery (water, salt + urea, uric acid) .
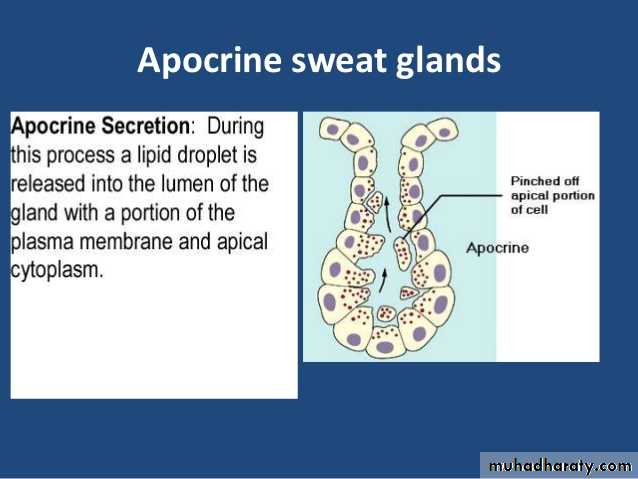
Apocrine sweat gland
• 1-Present in certain areas like, axilla, mammary gl., genital area& anal region & become functional at puberty, under the effects of sexual hormones2-Branched tubular gland ,wider & larger than the Merocrine gland.
3-Empty their secretion at upper border of hair follicles.
• 4-Portions of the cell are actually pinched off, and disintegrate later to excrete sweat.
• 5-Their secretion is viscous & thicker & provides nutrients for bacteria on the skin in which the bacteria's decomposition of sweat creates the a bad odor.
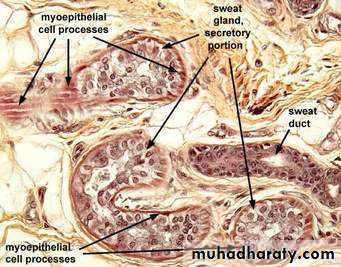
Merocrine sweat gland
• 6-The secretory portion lie in dermis & consist of a layer of cuboidal or low columnar cells which appear as two types clear cells & dark cells , as it has different shape so it appear as psedostratified cuboidal cells .In addition to these two types, there is a group of stellate – shaped cells called Myoepithelial cells ..
• 7- Ducts lined with double layers of cuboidal cells with myoepithelial cells (look darker), in the epidermis, the ducts losing their epithelium forming intercellular channel.
Apocrine sweat gland
• 6- The secretory portion has wide lumen consists of only one major cell type, which looks cuboidal or low columnar with more microvilli, numerous mitochondria & myoepthelial cells are prominent, their cytoplasm forms the slightly darker outline of the secretory tubules.•
• 7-The ducts open in to the hair follicles & not in the inter epidermal channels & their lining looks more uniform than that of merocrine sweat glands.
• .
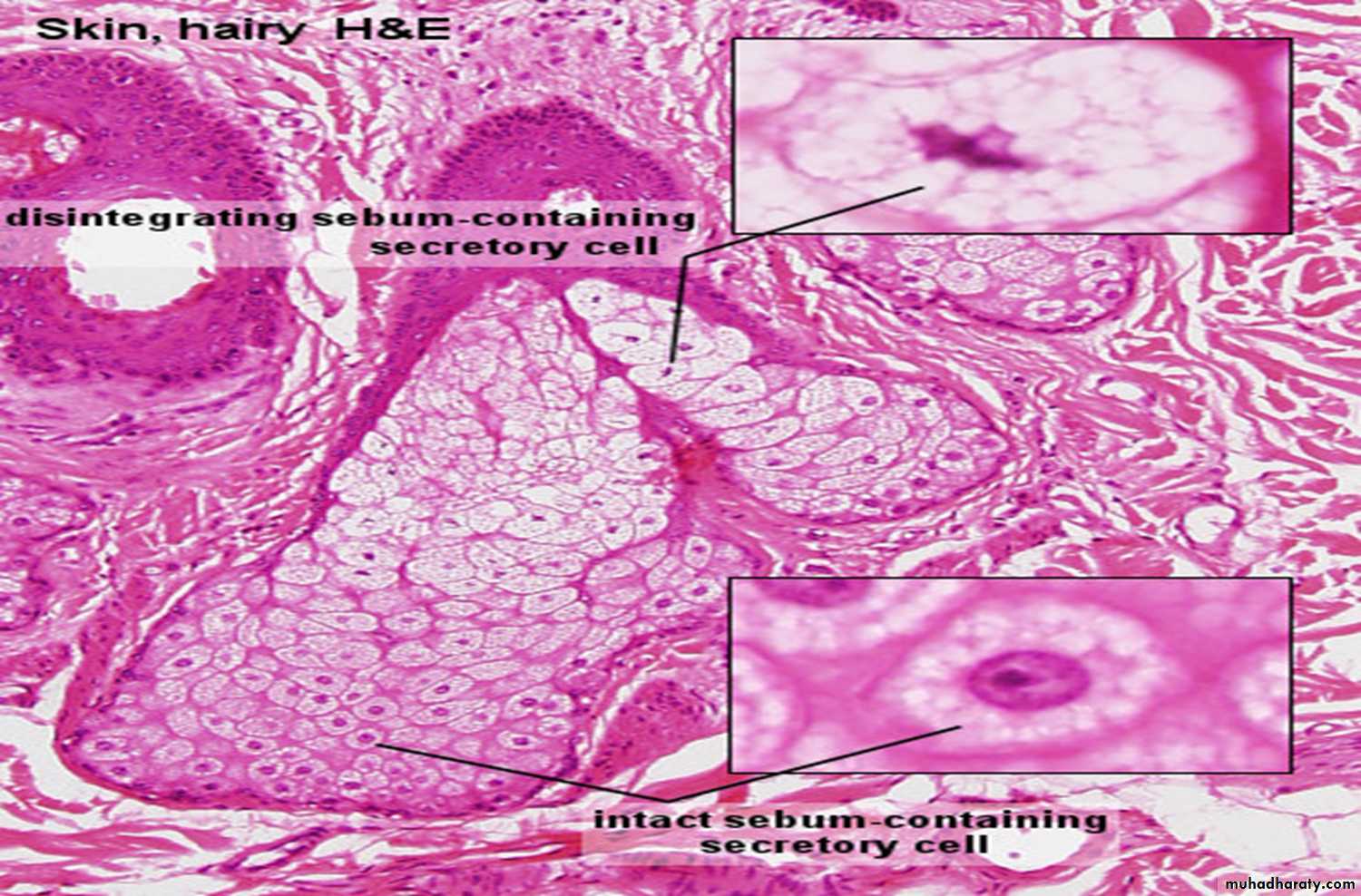
3- Sebaceous glands :
Are simple or branched alveolar gland.The sebaceous gland are found embedded in the dermis almost all over the skin of the body .
They consists of acini ,formed of external layer of undifferentiated flat epithelial cells resting on a basement membrane ,they proliferate & differentiate filling the acini with rounded or polyhedral cells containing abundant fat droplets in their cytoplasm ,their nuclei gradually shrink ,& the cells become filled with fat droplets & disintegrate releasing their secretion into the duct (holocrine gland).
• Holocrine secretion means the cells disintegrate releasing their secretion.
• The duct of the sebaceous gland end into the hair follicle at its upper border into which secretion is poured which is gradually moved to the surface of the skin .• The secretion is oily called "Sebum" which is a mixture of lipids containing [triglycerides, free fatty acids cholesterol & ester], the flow of secretion is continuous.
• Acne results if there is any disturbance in the flow & secretion of sebum.
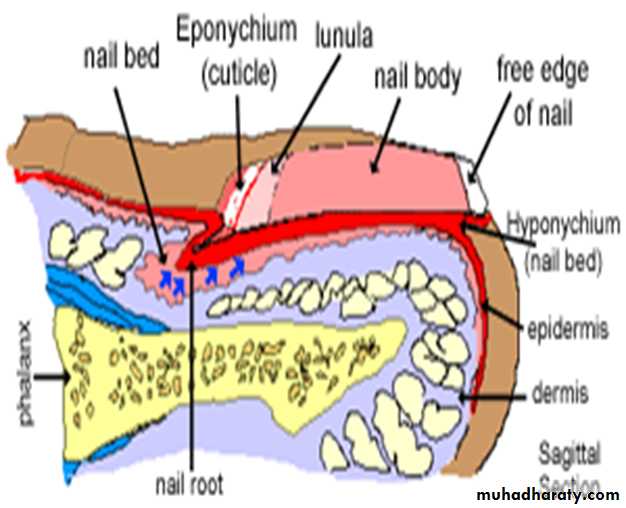
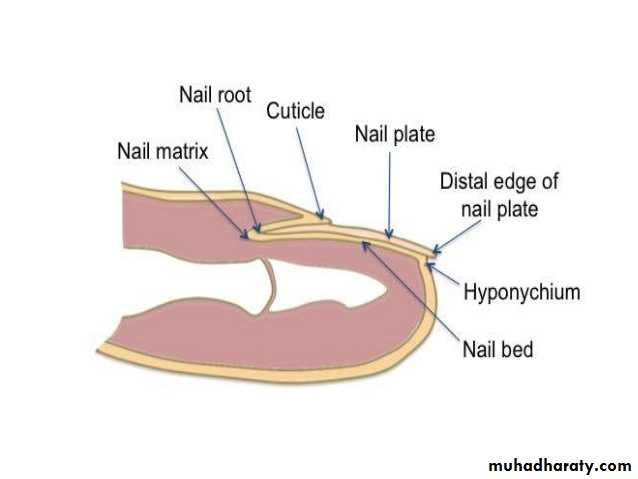
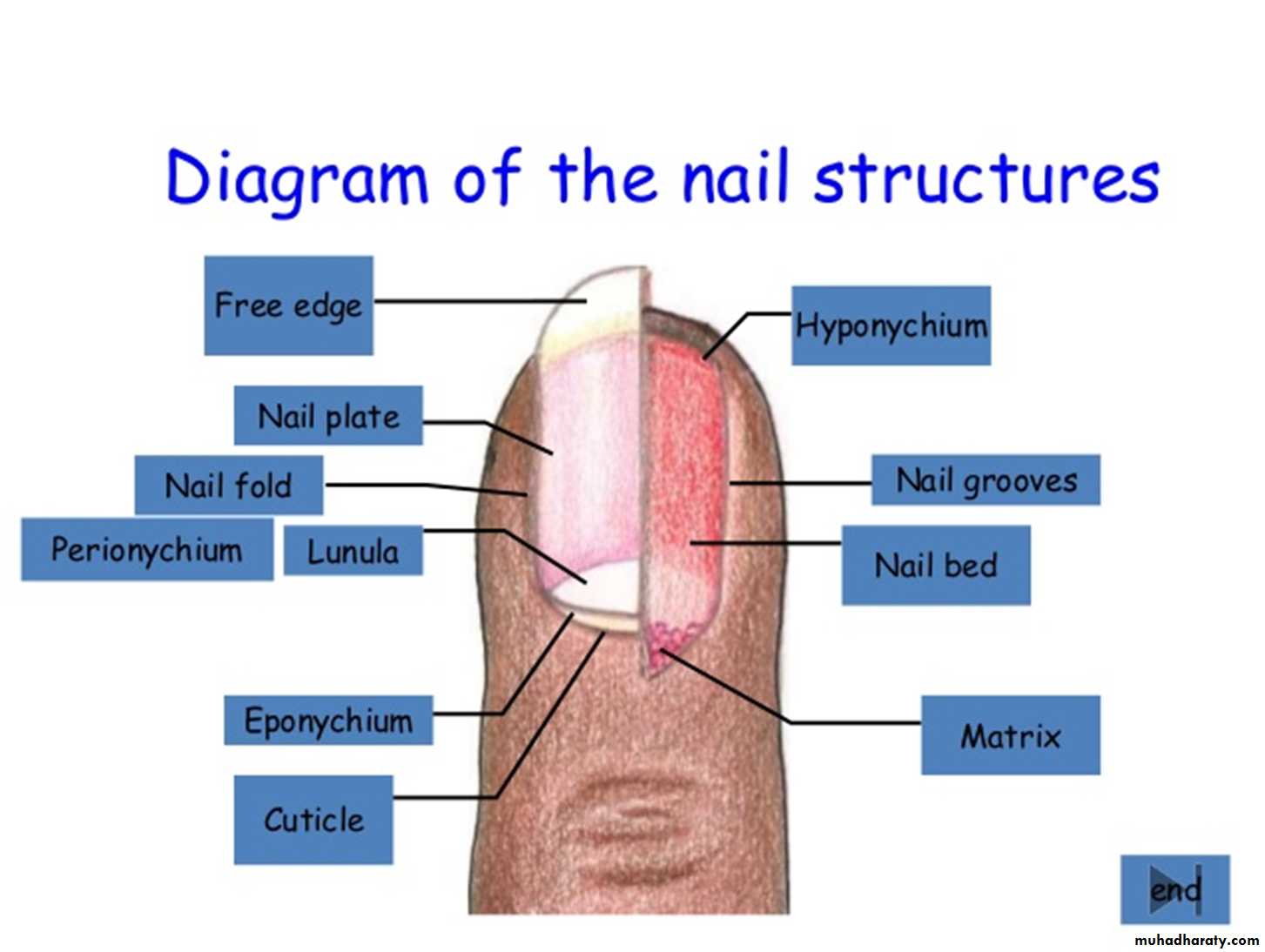
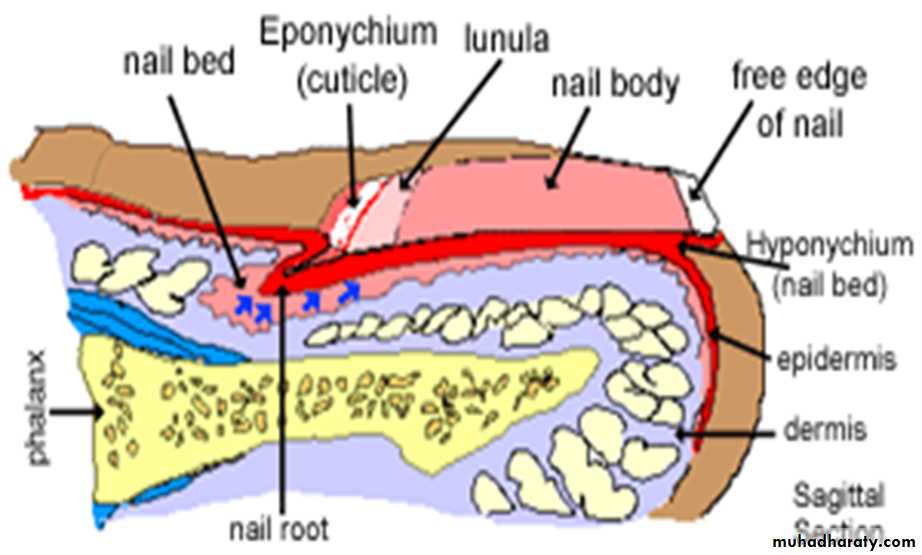
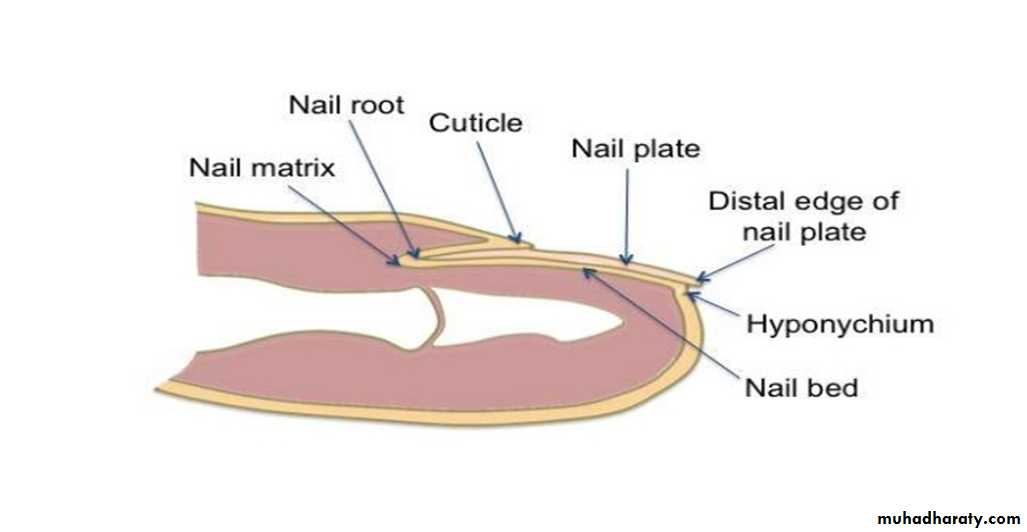
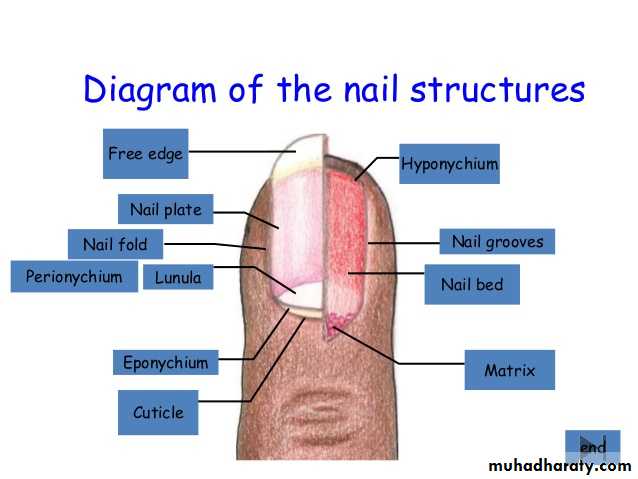
4- Nail:
A strong plate of hard keratin that protect the dorsal aspect of distal end of each digit is called a nail (nail plate), which grows out from a nail bed & surrounded by nail folds, the silt between the nail wall & the nail bed called "nail groove".Nail folds: there are proximal nail fold & lateral nail folds,
• the lateral folds have the same structure of the skin epidermis but as the skin epidermis turns inwards in to the nail groove, it loses stratum granulosum &stratum lucidum to form the nail bed while the stratum corneum form the nail plate.Nail bed, is a specialized form skin epidermis & its so thin & this is enough to visualize the color of vascular dermis below .
Nail plate is made up of hard , keratinized epidermal cells.
It consist of :• a) Root: is the proximal part of the nail which is covered by the proximal nail wall.
b) Body: which is the visible part of the nail.
c) Free edge: the anterior extension of the body.
• The proliferating cells in the nail root form the nail matrix, and their proliferation (in the stratum basale) make the nail elongate continuously.
• The white crescent at the proximal end is called the lunula. It is white because the underlying epithelium is thicker here, and the color of the dermis does not visualize through it.
• The keratinized layer of the proximal fold of the nail spread on the surface of the body of the nail is called "Eponychium“.
• Under the free edge of the nail the horny layer of stratum corneum is thickened to form "Hyponychium" that secures the nail to the finger tip, and lies below the nail plate..