Pharmacology
ثالث/أدوية الأربعاءد.شامل هاشم ألنعيمي 28/3/2018
Chemotherapy of infection(General Principles):
Definitions:
Antimicrobial Drugs:
The drug treatment of infections in which the infecting agents(viruses, bacteria, protozoa, fungi, worms) are destroyed or removed, without injuring the host.
Antibiotic:
A chemical substance produced by a micro organism that are antagonistic to the growth or life of other microorganisms.
Minimal inhibitory concentration (MIC):
In microbiology, MIC:Is the lowest concentration of an antimicrobial that will inhibit the visible growth of a microorganism, after overnight incubation.
Bacteriostatic:
Acts primarily by arresting bacterial multiplications.
Sulphonamides, Tetracycline, Chloramphenicol, Macrolides.
Bactericidal: Those drugs that are acting primarily by killing bacteria.
Penicillin, Cephalosporins, Aminoglycosides
Time dependent / Concentration Dependent
Time dependent bactericidal effect depends on the time in which the concentration of the drug is above the MIC:
“More time =More effect” e.g. Penicillins ,Cephalosporins
Concentration dependent bactericidal effect depends on the concentration of the drug above the MIC:
“More concentration=More effect” e.g. Amino glycosides, Quinolones
Classification of Antimicrobial drugs:
1- Antibacterial drugs.
2- Antiviral Drugs.
3- Antifungal Drugs.
4- Antiprotozoal drugs.
5- Anthelminthic drugs.
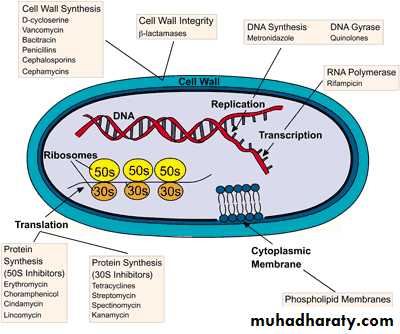
According to the Site of action:
1- The cell wall.
2- The cytoplasmic membrane.
3- Protein synthesis.
4- Nucleic acid metabolism.
General Principles of antimicrobial chemotherapy:
1-Make a diagnosis :As precisely as possible2-Remove barriers to cure: Lack of free drainage
3-Decide whether chemotherapy is really necessary.
e.g. Viral Infection?
4- select the best drug : according to
-Specificity.
-Pharmacokinetic factors.
-The patient. e.g. allergy
Any sampling for culture and sensitivity testing should be collected before administrating the antibiotic!
5- Administer the drug in optimal dosage and frequency, and by the most appropriate route.
Parenteral or oral?
Pareteral for serious infections (e.g. Intramuscular or intravenous) to get
high therapeutic concentration
Oral as soon as the patient can absorb the drug(GIT adverse reactions are more).
6- Continue therapy until apparent cure has been achieved.
Most acute infections for 5-10 days(Test for cure e.g. Urine Culture)
Combinations of Antimicrobials:
Why use combinations?
1-Avoid the development of resistance.e.g. TB
2-Broaden the spectrum of antibiotic therapy.
3-Obtaine potentiation. e.g. Synergy (1 + 1 = 5)
4-Enable reduction of dose of one component.
e.g. Amphotericin
Problems with antimicrobials :general problems
1-Resistance:
Mechanisms of resistance?
1-Naturally resistant strains.
3-Spontaneous mutation.
3-Transmission of genes from other organisms.(Most Common)
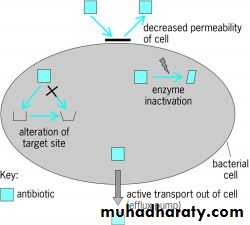
Resistance is mediated by:
1-Enzymes that modify the drug, “e.g. B-lactamase on penicillin”
2-Decrease passage or increase efflux of drug.
3-Modification of the target site.
4- By-passing the inhibited pathway.
Resistance can be limited by:
1- Ensure that antimicrobial is indicated and then use it for the proper time.2-Restrict the use of combination.
3-Limite the use of new drugs.
4-Monitoring resistance patterns in hospitals.
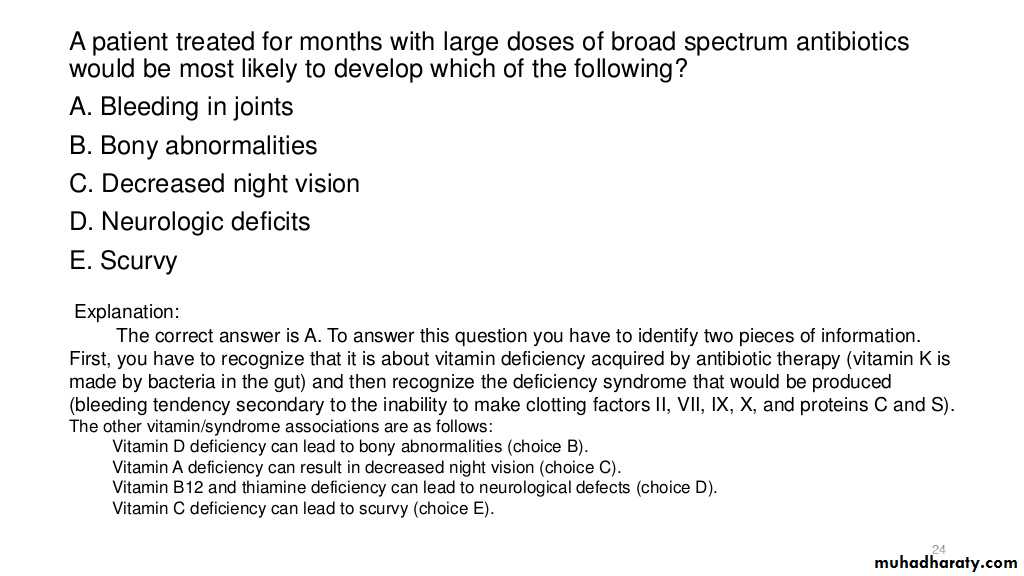
2-Super Infection:
Suppression of part of the normal flora. Antibiotic associated (clostridium difficile)
Several toxins that damage the mucosa of the bowl.
Injectable cephalosporins ,Amoxicillin/ Ampicillin
Study question