د. عماد ادوية 8\4\2018
عدد الاوراق ( 6 ) م\3\موصل lec:8
AMINOGLYCOSIDES
The group include:
Gentamicin, Amikacin, Tobramycin
Kanamycin, Streptomycin , Netilmicin
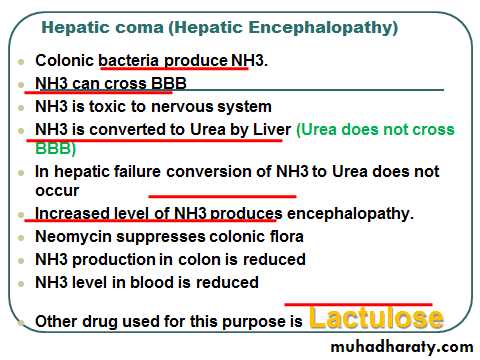
Framycetin (soframycin), Neomycin, Sissomicin
Paromomicin,Isepamicin,arbekacin
AMINOGLYCOSIDES
PHARMACOKINETICSStructurally related amino sugars
attached by glycosidic linkages
Polar compounds
Not absorbed orally
AMINOGLYCOSIDES
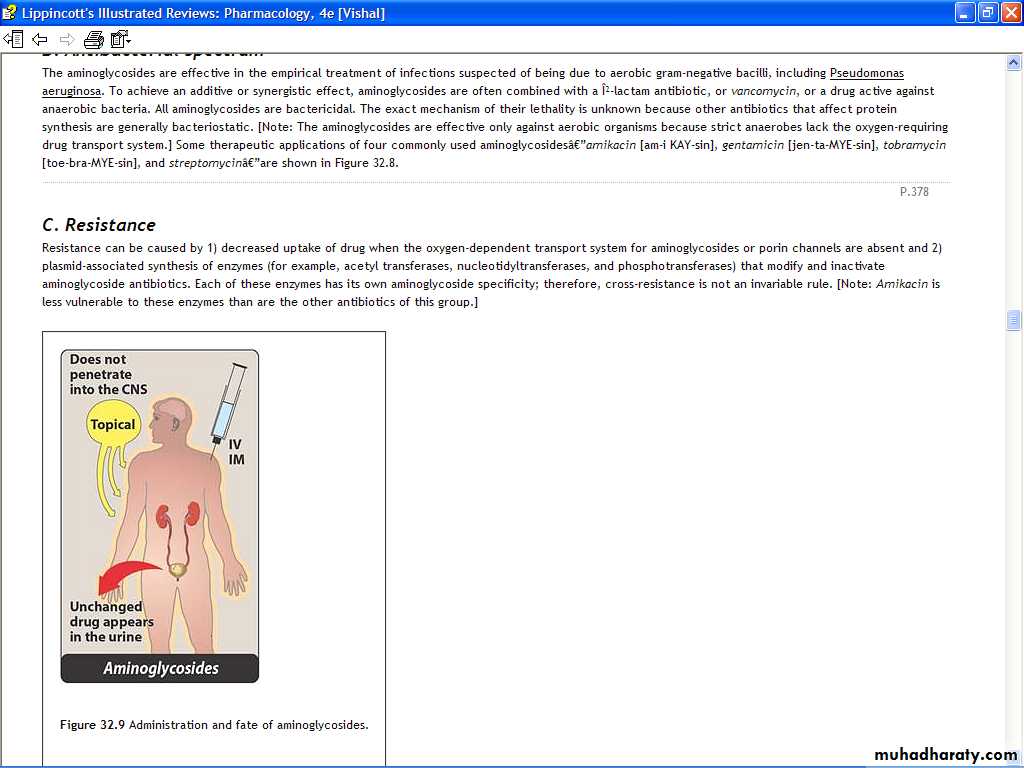
PHARMACOKINETICSGiven intramuscularly or intravenously
for systemic effects
Limited tissue penetration
Do not readily cross the blood-brain
barrier, what about usage in meningitis?!
AMINOGLYCOSIDES
PHARMACOKINETICSMajor mode of excretion
Glomerular filtration
Plasma levels are affected by changes
in renal function
AMINOGLYCOSIDES
PHARMACOKINETICSExcretion is directly proportional to
creatinine clearance
With normal renal function, elimination
half-life is 2-3 h
AMINOGLYCOSIDES
PHARMACOKINETICSDosage adjustment must be made in
renal insufficiency to avoid toxic accumulation
Monitoring plasma levels is needed for
safe and effective dosage selection and adjustment
AMINOGLYCOSIDES
PHARMACOKINETICS
For traditional dosing regimens
2 or 3 times daily
AMINOGLYCOSIDES
Buy AT 30 and CEL at 50
MECHANISM OF ACTION
Bactericidal (irreversible) inhibitors of
protein synthesis. Bind to 30S ribosomal unit
Interfere with protein synthesis
Clinical Uses of Aminoglycosides:
1. Gram negative bacillary infections particullarly , septicemia, pelvic and abdominal sepsis. Gentamicin remains the drug of choice but tobramycin should be preferred for infections caused by Pseudomonas aeroginosa.
2. Bacterial Endocarditis : Aminoglycosides are used in combination
( penicillinG + gentamicin IV)
with Penicillins for the treatment of Enterococcal, Streptococcal or Staphylococcal endocarditis.
3. Streptomycin is used for the treatment of brucellosis, tularemia, plague and tuberculosis.
4. Biliary tract infections.
5. Meningitis ( gentamicin intrathecally ).
6. UTIs.
7. Prophylaxis of surgical infections.
8. Paromomicin to treat intestinal amoebiasis
8. Topically: Gentamicin and framycetin as creams ,ointments and solutions for the treatment of infected burns, wounds or skin lesions.
Gentamicin-PMMA (Polymethyl methacrylate)
A new drug delivery system for Osteomyelitis.Small acrylic beads impregnated with gentamicin.
Threaded over surgical wire and implanted in bone cavity
Left for 10days.
Then removed along with wire.
Adverse Effects:
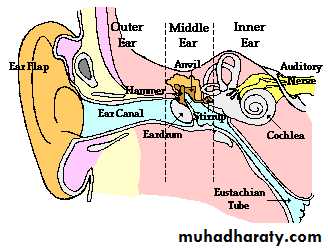
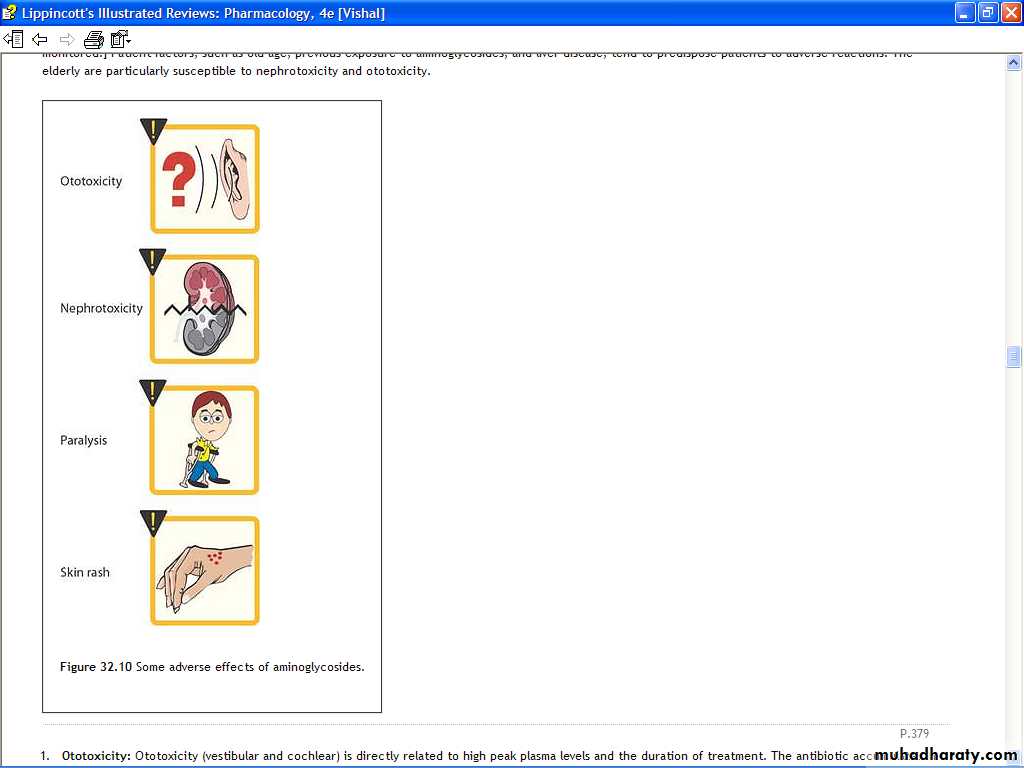
1. Ototoxicity: Both vestibular (streptomycin & gentamycin) and auditory damage (amikacin,kanamycin &neomycin) may occur causing hearing loss, vertigo, tinnitus, headache, dizziness or nausea,
2. Nephrotoxicity: All aminoglycosides are nephrotoxic . It is more likely to occur with large doses, high blood levels, long duration of therapy, in elderly patients, renal disease and in patients receiving furosemide diuretic.
Most nephrotoxic
Gentamicin and tobramycin
Side effects and Toxicity
Ototoxic-
Concentrated in labyrinthine fluid
Released from there when plasma concentration decreases.
Less seen in routine dose. (High dose, long time high chance)
Damage of sensory and hair cells
Vestibular- streptomycin & gentamycin
Presents with Vertigo, Ataxia, Nystagmus
(Headache, Nausea, Vomiting, Dizziness)
Recover slowly ( Least recovery in elderly)
Cochlear- amikacin,kanamycin &neomycin
High frequency affected first
Recovery is very poor.
Deafness may be permanent, more in elderly
Presents with tinnitus (reversible) followed by hearing loss (irreversible)
AMINOGLYCOSIDES
The NEPHROTOXICITY isMore common in elderly patients
Patients concurrently receiving
Amphotericin B
Cephalosporins
Vancomycin
3. Neuromuscular Blockade: Neomycin and Streptomycin
Aminoglycosides may impair neuromuscular transmission and aggravate myasthenia gravis or cause a transient myasthenia syndrome. Non significant in otherwise normal cases in routineDangerous in
Myasthenia gravis
Direct administration of Aminoglycosides into pleural and peritoneal cavities
If patient received curare like muscle relaxant during surgical procedure
4. Aminoglycosides may cause: Skin rashes (8% when neomycin is applied topically.
Note:Contraindicated introduction of aminoglycosides in the same syringe with penicillins, polymyxin B, cephalosporins - possible physical and chemical incompatibility!!!Q. Can you give B-lactum Antibiotic with aminoglycoside
Advantage of adding Beta lactamsBeta Lactam antibiotics weaken the bacterial cell wall
Facilitate passive diffusion of Aminoglycoside.(Synergism
Chloramphenicol
Presented by
Professor Dr. Imad A-J Thanoon
INTRODUCTION
An antibiotic produced by Streptomyces venezuelae, an organism first isolated in 1947 from a soil sample collected in Venezuela.Acts primarily by inhibits protein synthesis in bacteria by binding reversibly to the 50 S ribosomal subunit.
Pharmacokinetics:
Chloramphenicol is available for oral administration in two forms: the active drug itself and the inactive prodrug, chloramphenicol palmitate (which is used to prepare an oral suspension). Chloramphenicol then is absorbed from the gastrointestinal tractpeak concentrations occur within 2 to 3 hours after the administration of a 1-g dose.
The preparation of chloramphenicol for parenteral (IV) use is the water-soluble, inactive sodium succinate preparation.
Distribution
Chloramphenicol is well distributed in all body fluids and readily reaches therapeutic concentrations in CSF, where values are approximately 60% of those in plasma (in the presence or absence of meningitis).
Chloramphenicol is present in bile, is secreted into milk, and readily traverses the placental barrier. It also penetrates into the aqueous humor after subconjunctival injection.
Fate and Excretion cont.
The major route of elimination of chloramphenicol is hepatic metabolism to the inactive glucuronide. This metabolite, as well as chloramphenicol itself, is excreted in the urine by filtration and secretion.Fate and Excretion cont.
Patients with hepatic cirrhosis have decreased metabolic clearance, and dosage should be adjusted in these individuals.Therapeutic Uses
Chloramphenicol has a wide range activity that includes gram+, gram-, aerobic and anaerobic bacteriaTyphoid Fever
Bacterial Meningitis
Anaerobic Infections
Rickettsial Diseases
Brucellosis
Adverse effects cont. Hematologic Toxicity
The most important adverse effect of chloramphenicol is on the bone marrow.Chloramphenicol affects the hematopoietic system in two ways:
by an non-dose-related idiosyncratic response manifested by aplastic anemia, leading in many cases to fatal pancytopenia.
by a dose-related toxic effect that presents as anemia, leukopenia, or thrombocytopenia, and
Gray baby syndrome
Fatal chloramphenicol toxicity may develop in neonates, especially premature babies, when they are exposed to excessive doses of the drug.
The illness, the gray baby syndrome, usually begins 2 to 9 days after treatment is started.
The manifestations in the first 24 hours are vomiting, refusal to suck, irregular and rapid respiration, abdominal distention, periods of cyanosis, and passage of loose, green stools. Soon they become flaccid, turn an ashen-gray color, and become hypothermic
Gray baby syndrome cont
Two mechanisms are apparently responsible for chloramphenicol toxicity in neonates(1) failure of the drug to be conjugated with glucuronic acid, owing to inadequate activity of glucuronyl transferase in the liver, which is characteristic of the first 3 to 4 weeks of life; and (2) inadequate renal excretion of unconjugated drug in the newborn.
Hypersensitivity Reactions
Although relatively uncommon, macular or vesicular skin rashes occur as a result of hypersensitivity to chloramphenicol. Fever may appear simultaneously or be the sole manifestation.Angioedema is a rare complication.