
1
د. ندوى
امراض
8
\
3
\
8108
( عدد االوراق
8
) م
\
3
\
موصل
6
lec:5 +
Gastrointestinal System
The gastrointestinal (GI) tract is a hollow tube extending from the oral
cavity to the anus that consists of anatomically distinct segments,
including the esophagus, stomach, small intestine, colon, rectum, and
anus
Oral Cavity
The mouth is subject to the same types of lesions as other
sites in the body, but these often show distinct features
peculiar to the mouth. In addition, there are a number of
specific lesions related to the teeth and their supporting tissues.
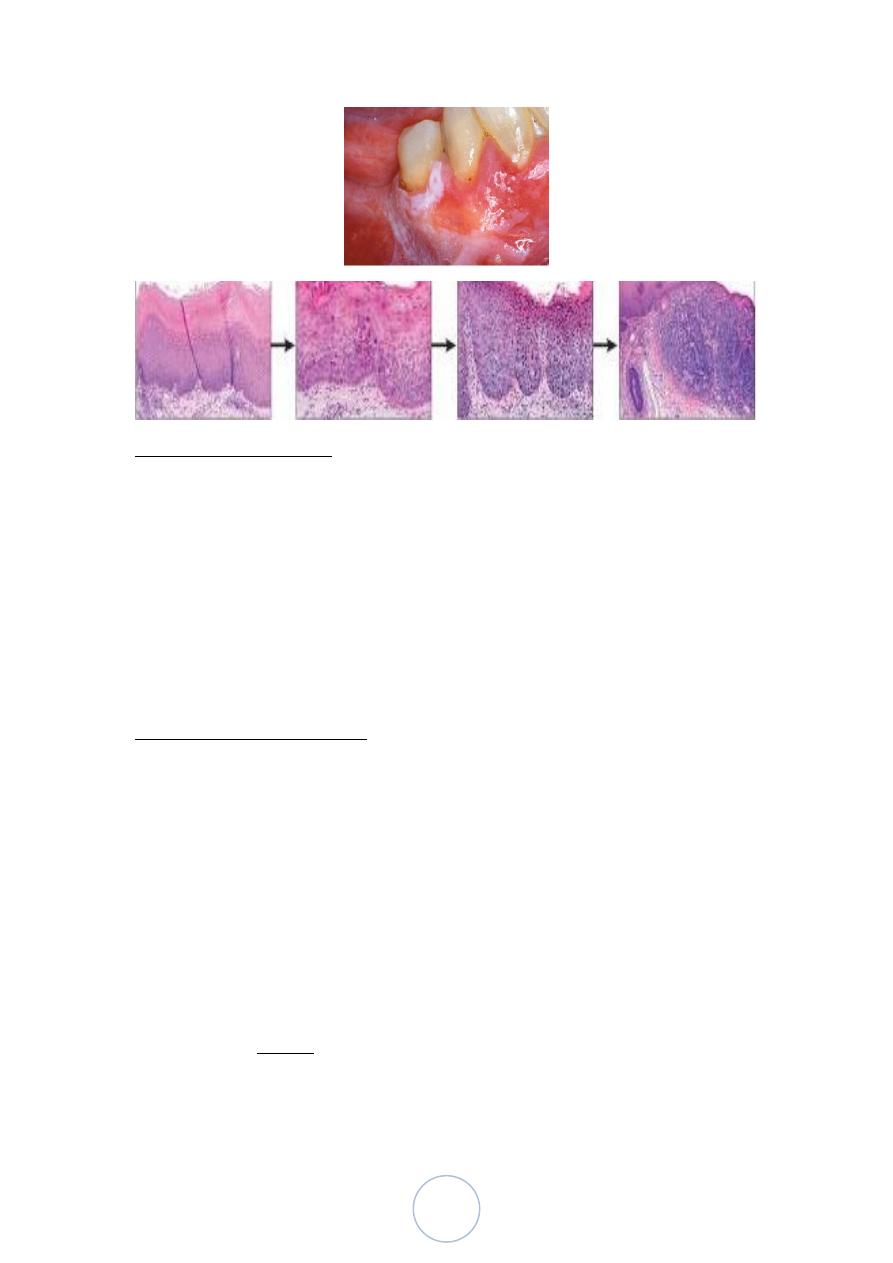
LEUCOPLAKIA
Leucoplakia and erythroplakia are potentially malignant lesions.
Leucoplakia is a white patch which cannot be attributed to any specific
disease
erythroplakia is the analogous term for the less frequent red patches.
Smoking and frictional irritation are common aetiological factors,
but many cases are of unknown aetiology.
Microscopically.
hyperkeratosis of the linning epithelium, and a variable inflammatory
infiltrate is present. A small proportion show dysplasia.
The more severe the dysplasia microscopically, the greater risk of
malignancy.
• High-risk sites for malignant change are floor of mouth, ventral and
lateral of the tongue.
2
SALIVARY GLANDS
• There are three major salivary glands
parotid, submandibular, and sublingual
• as well as numerous minor salivary glands distributed throughout
the mucosa of the oral cavity.
All these glands are subject to inflammation or to the development of
neoplasms.
Inflammation (Sialadenitis)
Causes :
Trumatic
Viral (Mumps)
Bacterial
Autoimmune (Sjögren syndrome)
Tumors of Salivary glands
Epithelial salivary gland neoplasms are a complex
group, mostly benign.
• 80% of salivary gland tumors involve the parotid
gland.
3
• Pleomorphic adenomas account for over 70% of
tumors.
• There is a higher relative incidence of carcinomas in minor salivary
glands.
PLEOMORPHIC ADENOMA
60% of tumors in the parotid, are less common in the
submandibular glands, and rarely in minor
benign tumors that consist of a mixture of ductal (epithelial) and
myoepithelial cells, and therefore they show both epithelial and
mesenchymal differentiation.
epithelial elements dispersed throughout the matrix along with
varying degrees of myxoid, hyaline, chondroid (cartilaginous), and
even osseous tissue
WARTHIN TUMOR (papillary cystadenoma lymphomatosum)
almost exclusively in the parotid
more commonly in males than in females, usually in the fifth to
seventh decades of life.
On microscopic examination cystic spaces are lined by a double
layer of neoplastic epithelial cells resting on a dense lymphoid
stroma
4
Adenoid cystic carcinoma
uncommon tumor, which in approximately 50% of cases is found
in the minor salivary glands , the major salivary glands affected are
parotid & submandibular
Microscopically: solid growth of small hyperchromatic neoplastic
cells surrounding small (microcystic) spaces filled with mucinous
secretions giving rise to cribriform appearance
THE OESOPHAGUS
25 cm in length, the oesophagus is a muscular
tube with a well-defined origin
Its function is a simple one, namely the conduction of food from the
pharynx to the stomach.
The mucosal lining is of stratified squamous epithelium, while the
underlying submucosa includes numbers of mucinous glands The muscle
coat is an inner circular and outer longitudinal coats.
5
MOTOR DISORDERS
Achalasia
Hiatal Hernia (sliding [95%], paraesophageal)
“ZENKER” diverticulum
Esophagophrenic diverticulum
Mallory-Weiss tear
Achalasia
Achalasia is a Greek term meaning „failure to relax‟ is
characterized by poor relaxation of the functional lower
oesophageal sphincter.
Causes: most of the cases is unknown ,but could be due to systemic
sclerosis and South American trypanosomiasis (Chagas‟ disease)
may present at any stage in life, usually with dysphagia and
regurgitation of undigested food material. Aspiration pneumonia is
a significant problem
Microscopically, the disease is characterized by a reduction in the
numbers of neurones in the muscular (myenteric) plexus of the lower
oesophagus, dilatation of proximal esophagus ,Inflammation &ulceration
of mucosa .
6
Esophagitis:
Inflammation of esophageal mucosa
Causes:
o Reflux oesophagitis : refluxed gastroduodenal contents
o Infectious agents (Candida, herpes simplex
virus) rarely in immunocompromised patient.
o
The oesophagus may be involved in Crohn‟s disease and in
systemic sclerosis.
o Oesophageal obstruction (tumour, achalasia)
leads to a secondary proximal oesophagitis.
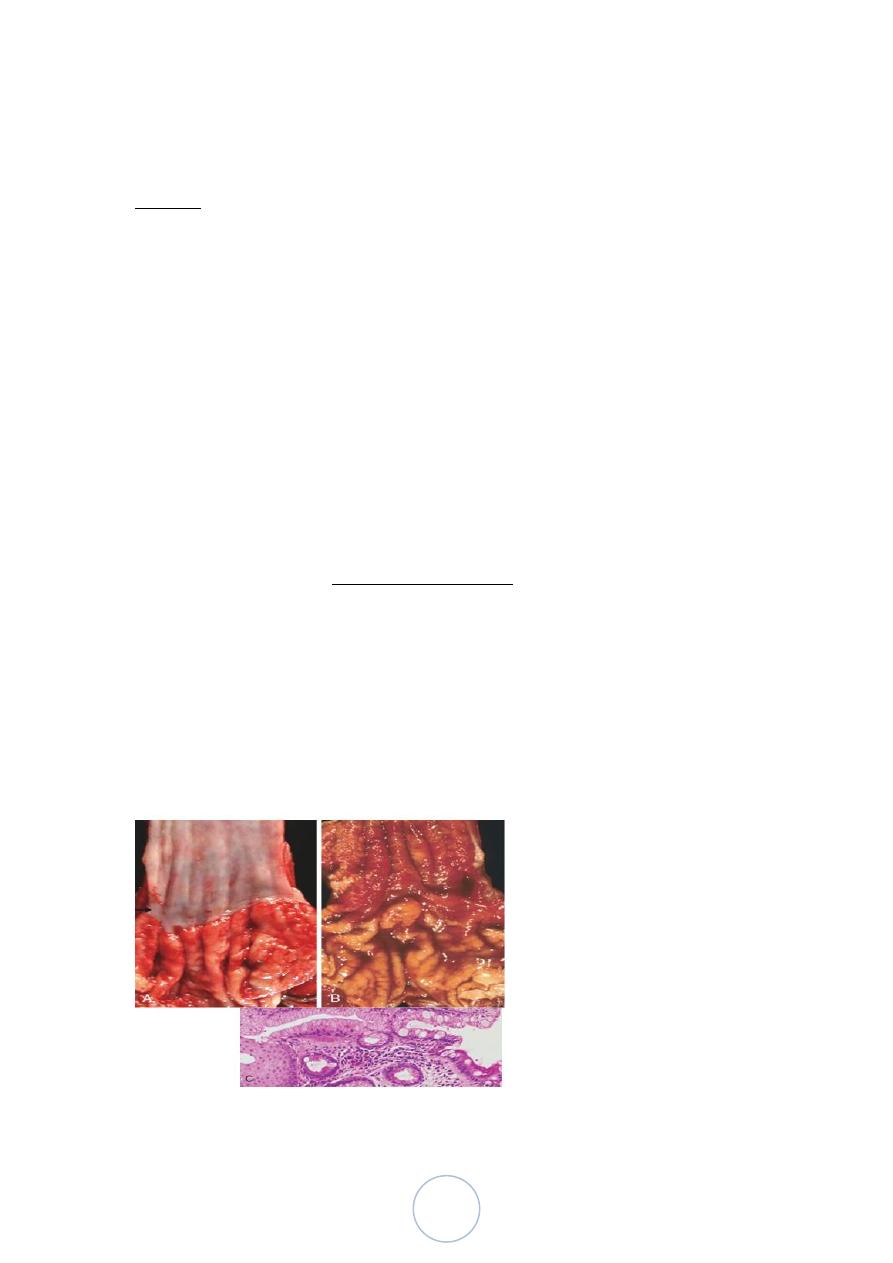
Barrett Esophagus:
characterized by intestinal metaplasia within the esophageal
squamous mucosa
10% of individuals with symptomatic Gastroesophageal reflux
diseases
most common in white males and it typically presents between 40
and 60 years of age.
The signifigance of it: an increased risk of esophageal
adenocarcinoma.
7
ESOPHAGEAL VARICES
development of a congested subepithelial and submucosal venous
plexus within the distal esophagus. These vessels, termed varices,
develop in 90% of cirrhotic patients, most commonly in association
with alcoholic liver disease. Hepatic schistosomiasis is the second
most common cause of varices.
they may rupture, causing massive hematemesis half of the patients
die from the first bleeding episode either as a direct consequence of
hemorrhage or following hepatic coma triggered by hypovolemic
shock.
8
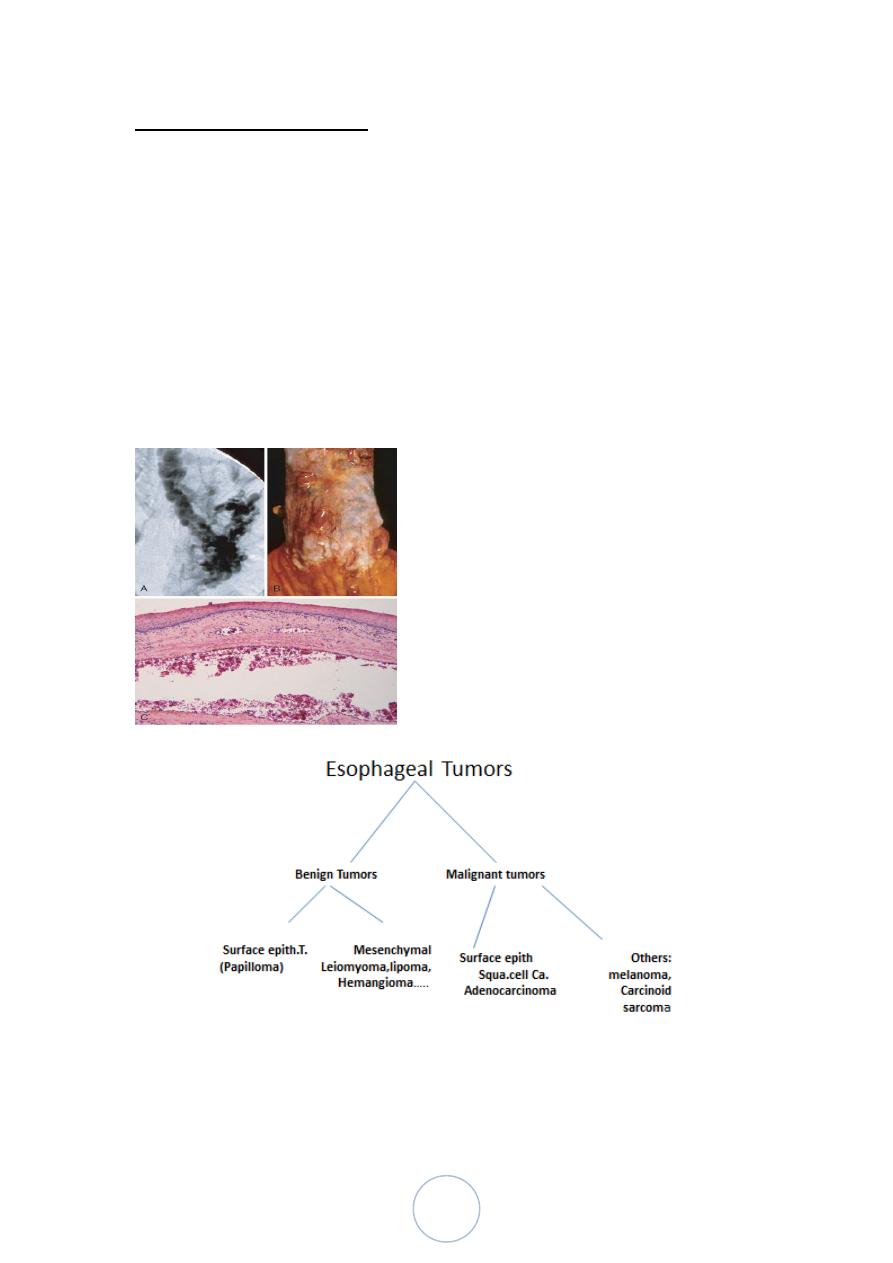
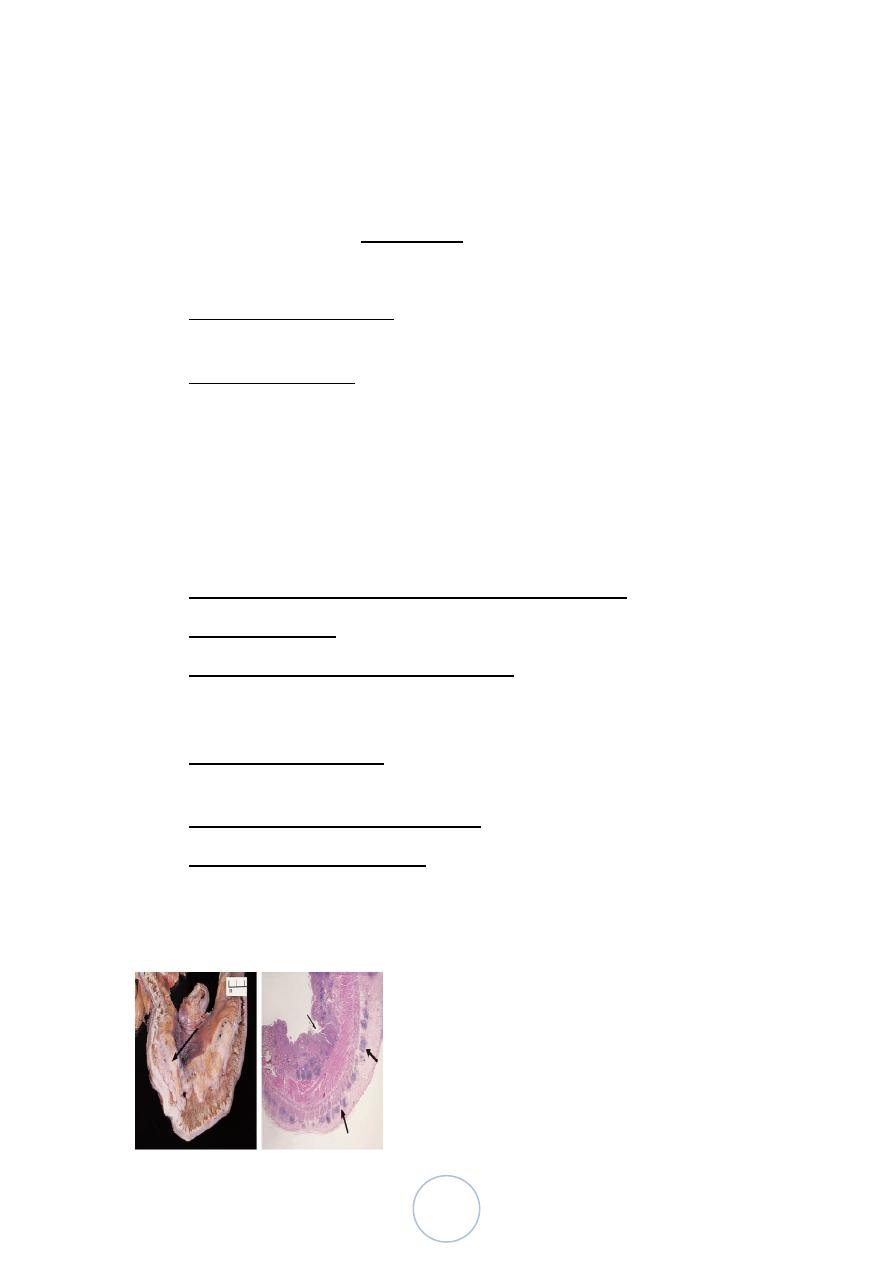
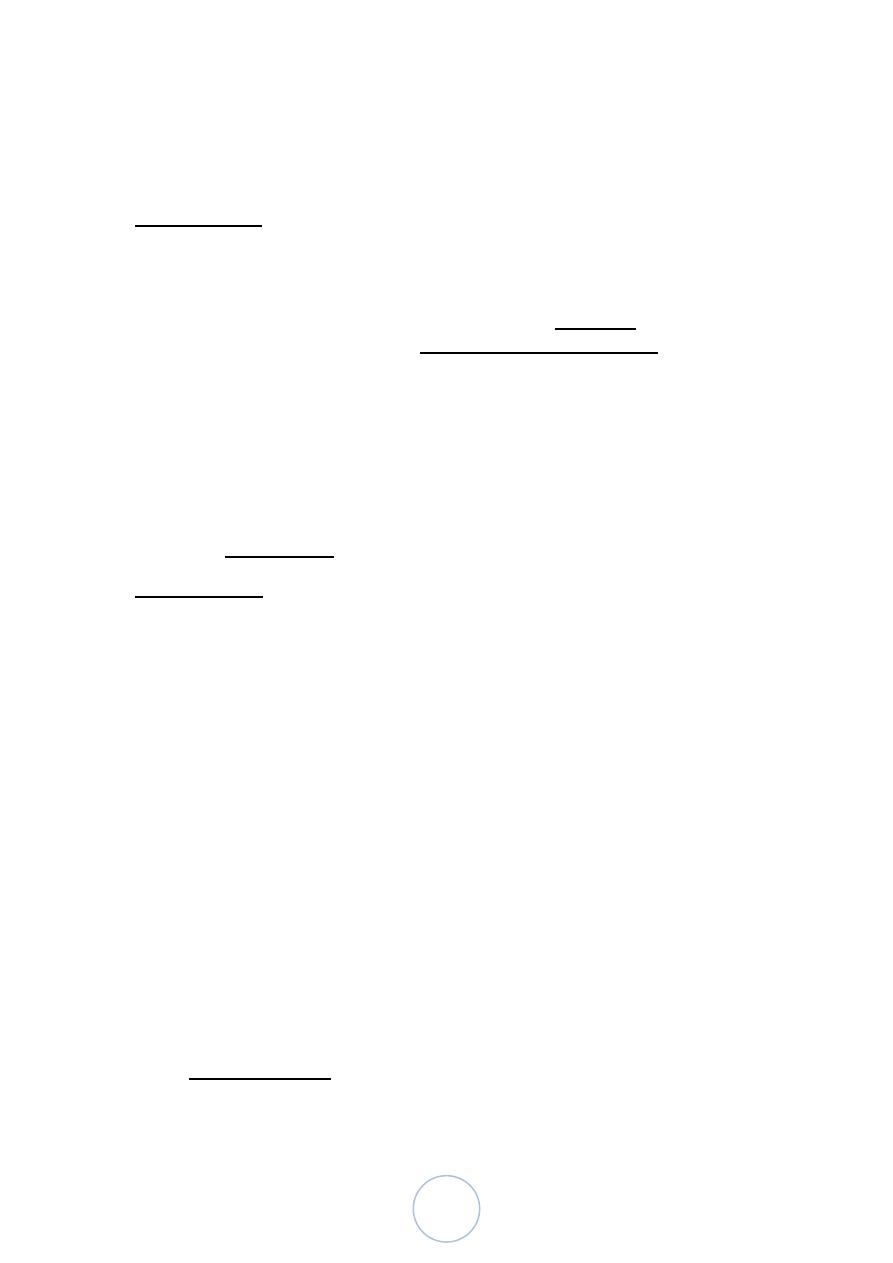
Squamous Cell Carcinoma
Arise from Sq.epithelium as exophytic, ulcerative
masses that partly or almost totally occlude the lumen.
Adenocarcinomas
generally arise in Barrett‟s oesophagus, this is a disease of Western
society
Lec:
9
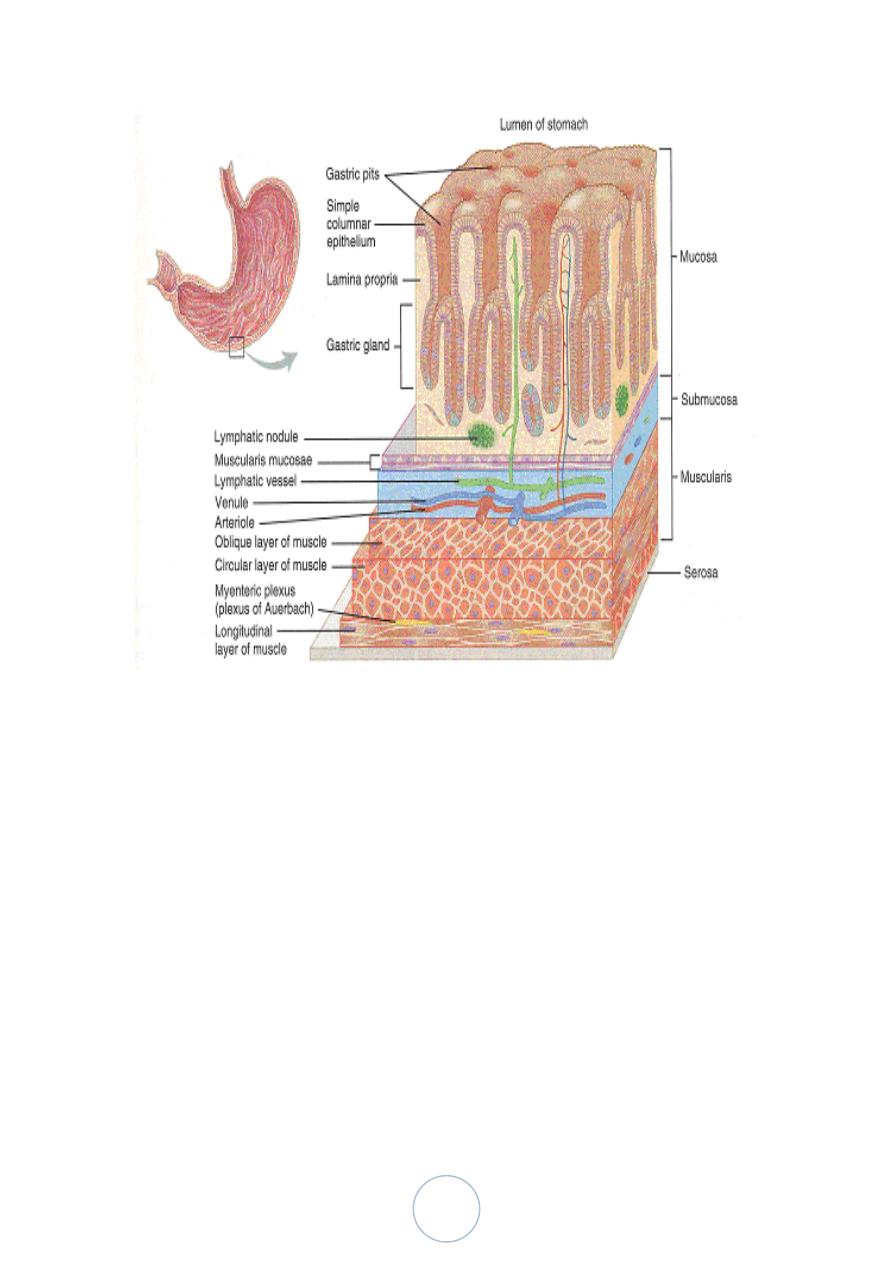
If you think of the acid production in the stomach to be ONLY in the
mid-BODY, and the proximal and distal ends as chiefly mucous to
protect the esophagus and duodenum from the harsh acid, then you will
understand the histology.
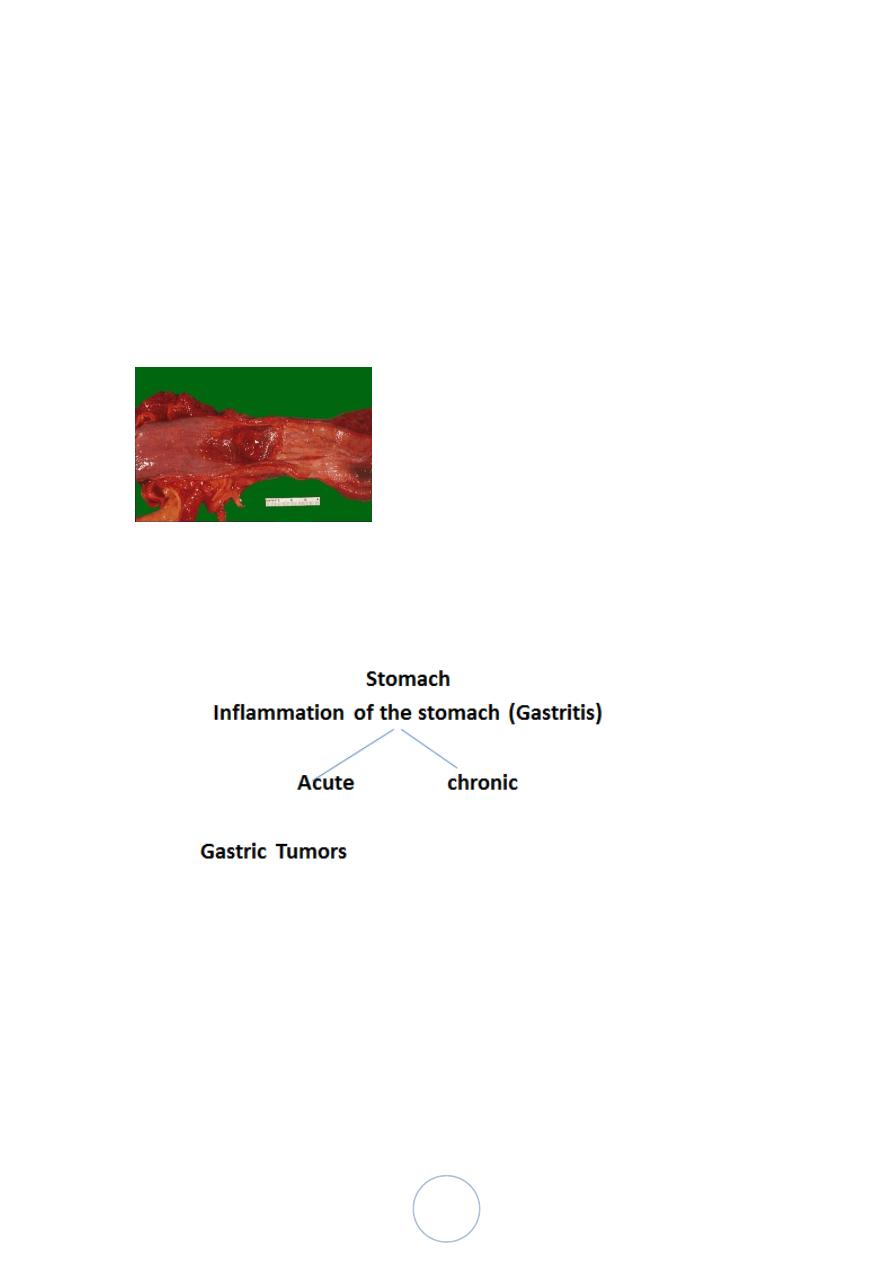
Acute Gastritis
is a transient mucosal inflammatory process
Pathogenesis:
Acute or chronic gastritis can occur following disruption of any of these
protective mechanisms
Mucin secreted by surface foveolar cells forms a thin layer of
mucus (defect occur as in elderly,
bicarbonate ion secretion ( NSAI drugs reduce producti on),
chemotherapy
rich vascular supply

10
Clinically:
Mild cases the pt. presented with nausea, vomiting in severe cases causes
bleeding
Microscopically :
Mild condition show neutrophils infiltrated the surface epithelium &
glands in lamina propria with lymphocytes and plasma chronic
inflammatory cells
In severe cases there are erosion of surface epithelium , ulceration ,
bleeding and hemorrhage.
ACUTE GASTRIC ULCERATION
Pathogenesis.
Stress ulcers are most common in individuals with shock, sepsis, or
severe trauma
Ulcers occurring in the proximal duodenum and associated with
severe burns or trauma are called Curling ulcers.
Gastric, duodenal, and esophageal ulcers arising in persons with
intracranial disease are termed Cushing ulcers and carry a high
incidence of perforation.
Acute gastritis: hyperemic erythmatous edematous gastric mucosa with
foci of superficial erosions. There are many causes for acute gastritis:
alcoholism, drugs, infections, etc
11
Chronic Gastritis
Causes :
The most common cause of chronic gastritis is infection with the
bacillus Helicobacter pylori.
Others : psychological stress, caffeine, alcohol, and tobacco .
Autoimmune gastritis ( cause atrophic gastritis, 10%of chronic
gastritis in the absence of H.pylori)
Less common causes : radiation injury, chronic bile reflux,
mechanical injury, and involvement by systemic disease such as
Crohn disease, amyloidosis, or graft-versus-host disease.
HELICOBACTER PYLORI GASTRITIS
o spiral-shaped or curved bacilli
o Presented in almost all patients with duodenal ulcers and the
majority of individuals with gastric ulcers or chronic gastritis.
o H. pylori has important roles in gastric and duodenal diseases.(
peptic ulcer disease, increased risk of gastric cancer)
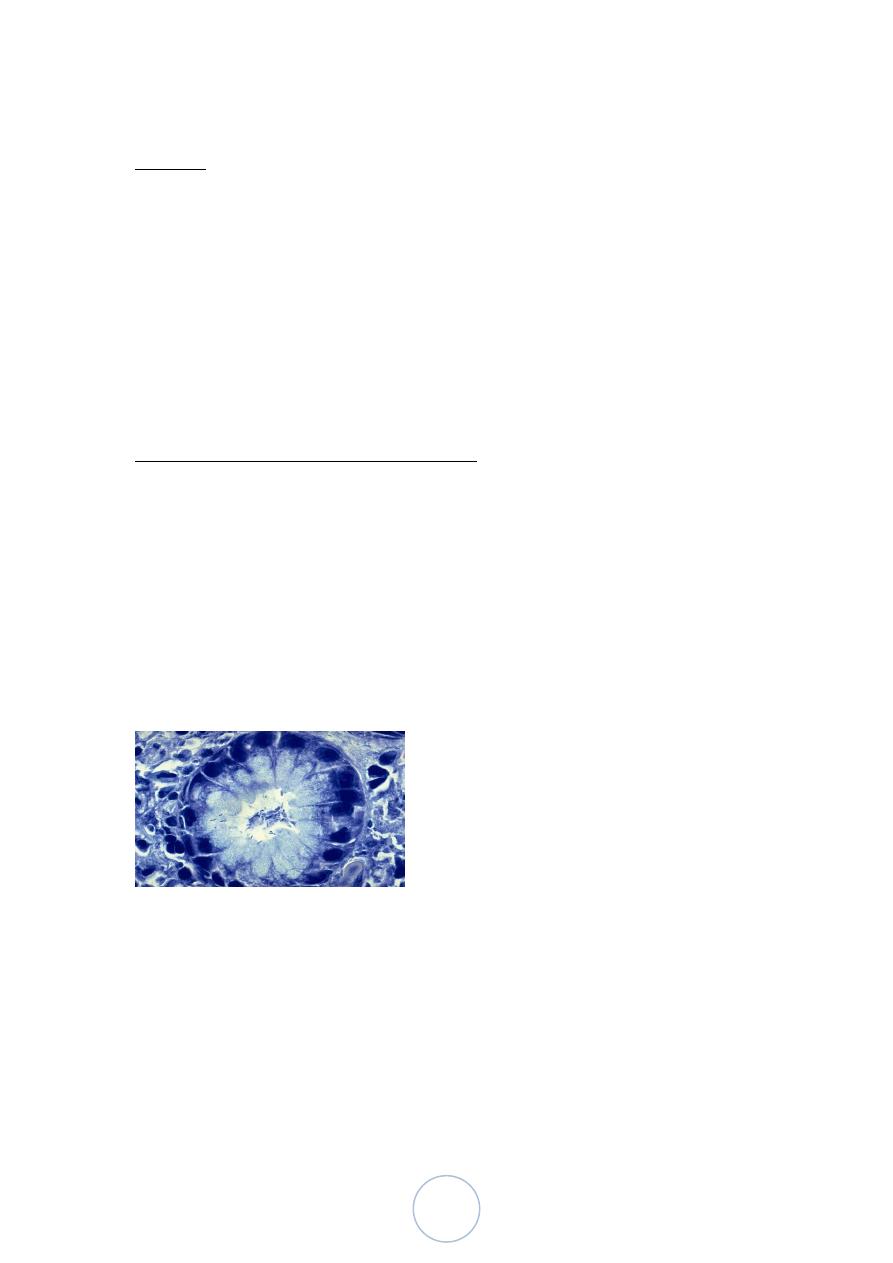
H-pylori This small curved to spiral rod-shaped bacterium is found in the
surface epithelium of most patients with active gastritis. The rods are seen
here with a methylene blue stain.
Pathogenesis.
H.Pylori causes Antral gastritis with high acid secretion , progress to
involve the fundic and body mucosa , in advanced untreated conditions
lead to pangatritis associated with multifocal mucosal atrophy, reduced
acid secretion, intestinal metaplasia, and increased risk of gastric
adenocarcinoma.
Morphological Features of H.pylori asssociated chronic gastritis:
12
H.Pylori is concentrated within the superficial mucus overlying
epithelial cells in the surface and neck regions.
H. pylori are typically found in the antrum ,
neutrophilic cells infiltration within the lamina propria
In addition, the superficial lamina propria includes large numbers
of plasma cells, often in clusters or sheets, and increased numbers
of lymphocytes and macrophages.
PEPTIC ULCER DISEASE
85% -100% are duodenal ulcers
65% gastric ulcer
Epidemiology.
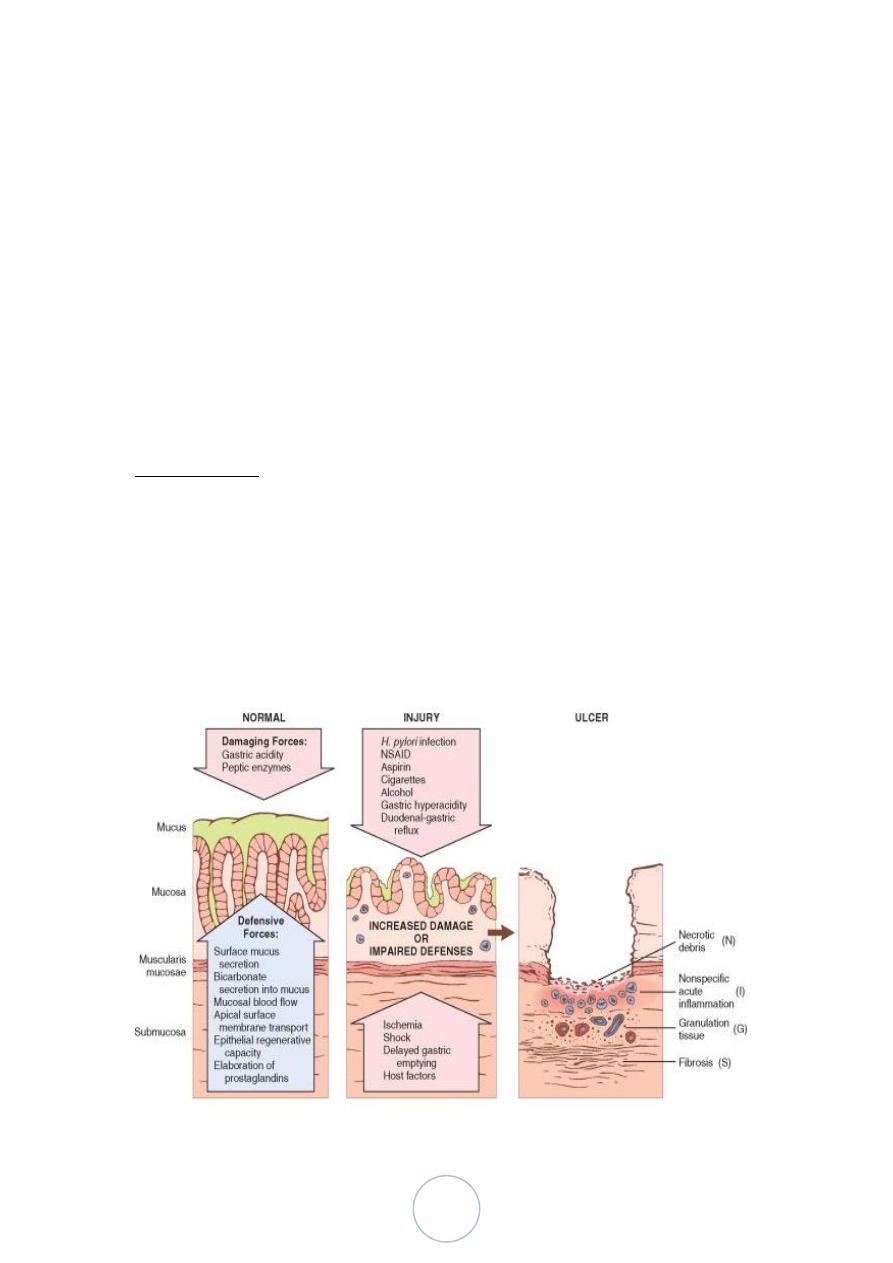
The imbalances of mucosal defenses and damaging forces that
cause chronic gastritis are also responsible for PUD
the main causes for hyperacidity: H.pylori, parietal cell
hyperplasia, hypergastrinemia, ….
Co-factors NSAIDrugs direct injury to the mucosa
Smoking , alcohol consumption affect the blood supply of mucosa

13
Morphology:
Duodenal ulcers involve the anterior duodenal wall.
Gastric peptic ulcers are predominantly located along the lesser
curvature near the interface of the body and antrum.
80% solitary ,round to oval, sharply punched-out defect, hang out
the surrounding mucosa
The base show fibrinoid material, Beneath this, active granulation
tissue infiltrated with mononuclear leukocytes and a fibrous or
collagenous scar
• Complications of Peptic Ulcers:
• Bleeding
– Occurs in 15% to 20% of patients
– Most frequent complication
– May be life-threatening
– Accounts for 25% of ulcer deaths
– May be the first indication of an ulcer
• Perforation
– Occurs in about 5% of patients
– Accounts for two thirds of ulcer deaths
– Rarely, is the first indication of an ulcer

14
• Obstruction from edema or scarring
– Occurs in about 2% of patients
– Most often due to pyloric channel ulcers
– May also occur with duodenal ulcers
– Causes incapacitating, crampy abdominal pain
– Rarely, may lead to total obstruction with intractable
vomiting
– Malignant transformation of peptic ulcers is very rare
Would this slide be seen in a REAL classroom to those sitting in the back
row?
GASTRIC TUMORS
• BENIGN:
– “POLYPS*” (HYPERPLASTIC vs. ADENOMATOUS)
– LEIOMYOMAS
– LIPOMAS
• MALIGNANT
– (ADENO)-Carcinoma
– LYMPHOMA
Others
– Gastro-Intestinal “Stromal” Tumor (GIST)
– CARCINOID (NEUROENDOCRINE)
In general. A “polyp*” can be thought of as ANYTHING which projects
as a bump or nodule from a mucosal surface.
HYPERPLASTIC POLYPS are considered to be NON-neoplastic, and
therefore NEVER turn into cancers. ADENOMATOUS polyps are true
benign neoplasms and MAY turn into carcinomas, particularly if the
exhibit DYSPLASIA on biopsy.
15
This SAME general principle, is even MORE true of the colon!
But in general, you know the drill: 1) Benign, 2) Malignant, and 1)
epithelial, 2) stromal, and 3) lymphoid
RISK FACTORS
o H. Pylori
o Type of food : Nitrites, smoked meats, pickled, salted, chili
peppers,
o Low Socioeconomic
o tobacco
o
Chronic gastritis, Barrett‟s, adenomas
o Family history
Morhophology: Adenocrcinoma
Intestinal Type :
Grossly : Exophytic , Nodular, ulcerative Excavaeted.
Microscopically: glandular component of malignant cells.
Diffuse type:
Infitrative to gastric wall , malignant cells had intracellular mucin push
the nucleus to the periphery (Linitis Plastica)
16
د.ندوى امراض
00
\
3
\
8108
( عدد االوراق
7
) م
\
3
\
موصل
lec:7+8
SMALL INTESTINE AND COLON
• The small intestine and colon account for the majority of GI
tract length and are the sites of a broad array of diseases
SI = 6 meters (100% intraP, except for duodenum), LI = 1.5 meters
(50% retroP)
Mucosa, submucosa, muscularis, serosa
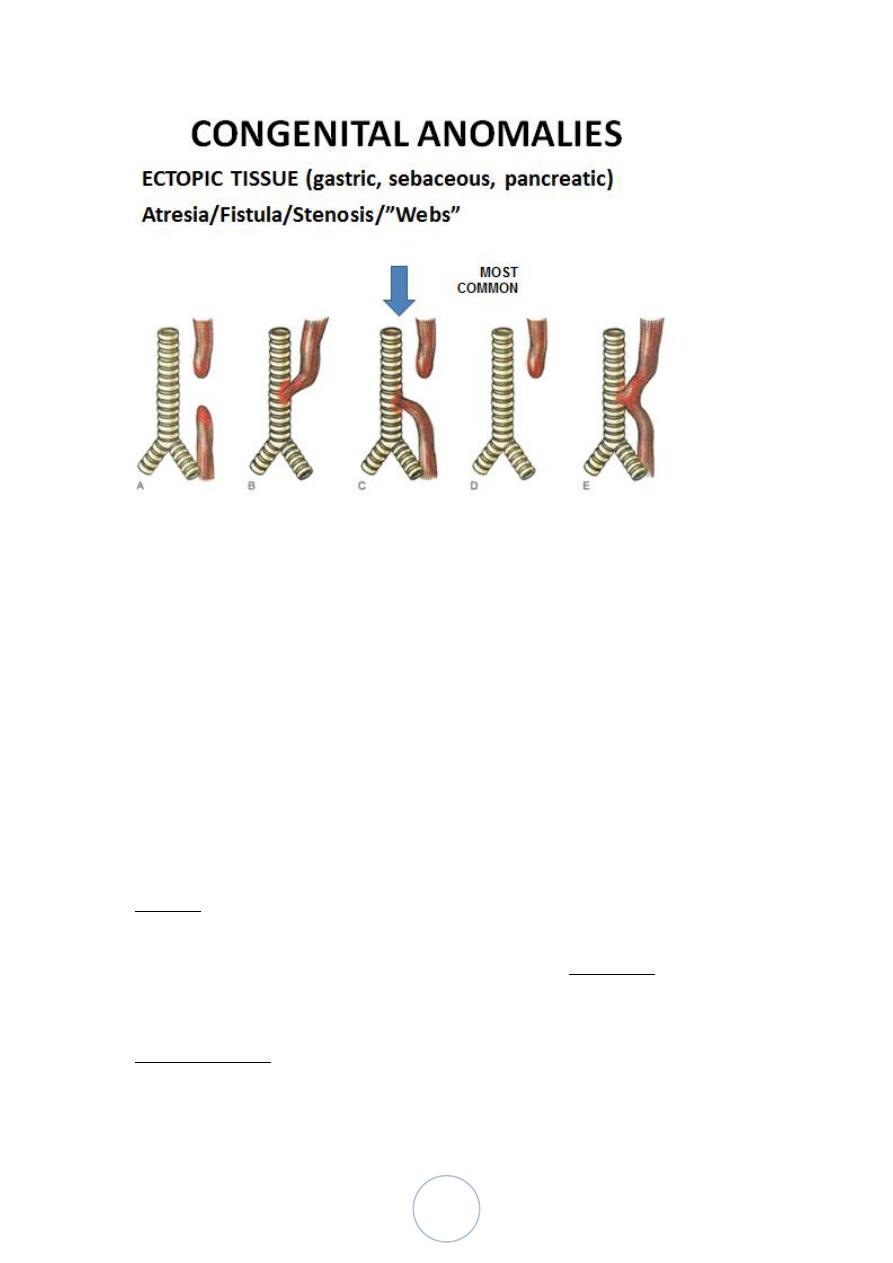
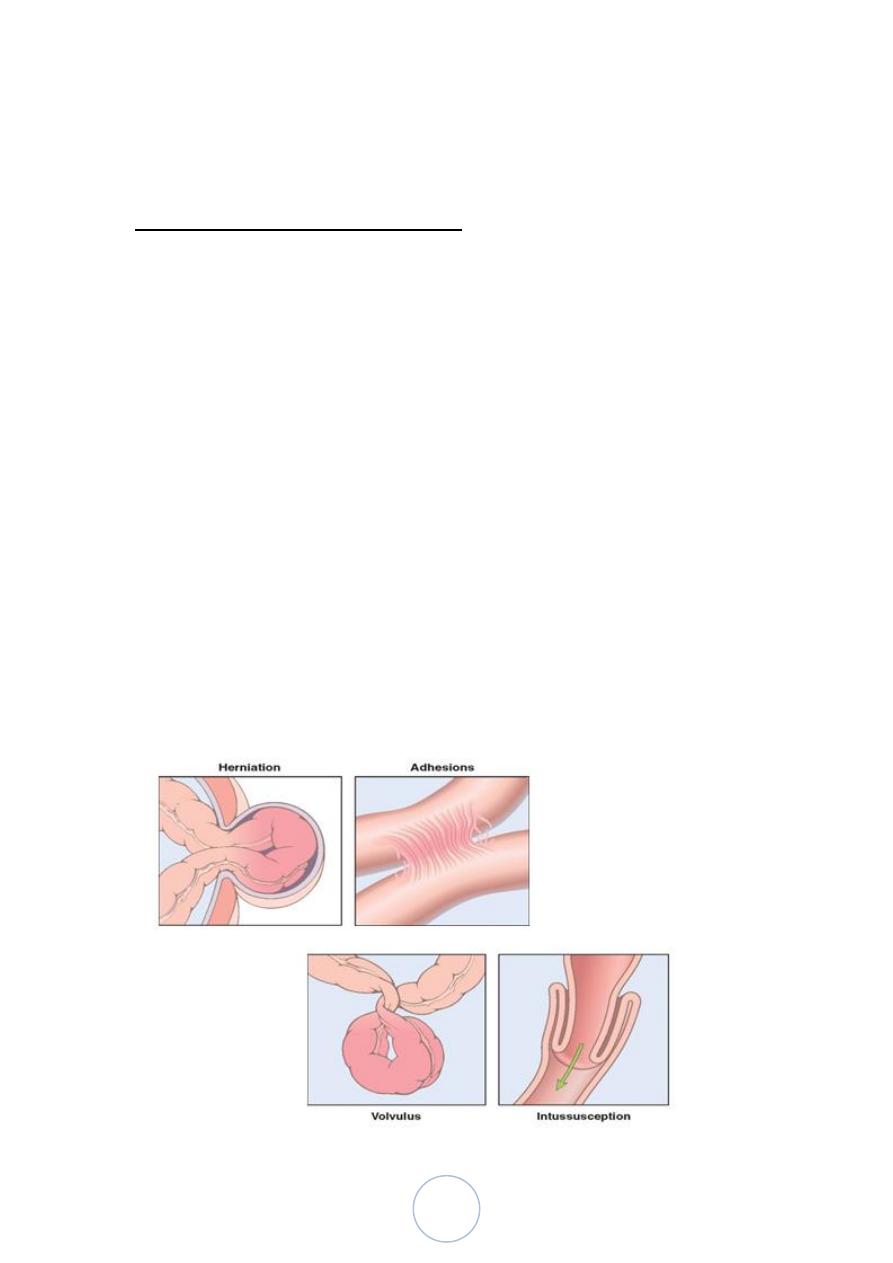
Intestinal Obstruction
small intestine is most often involved because of its relatively narrow
lumen.
Hernias,
Intestinal adhesions,
Intussusception
Volvulus account for 80% of mechanical obstructions
17
HERNIAS
Any weakness or defect in the wall of the peritoneal cavity may
permit protrusion of a serosa-lined pouch of peritoneum (hernial sac)
The inguinal and femoral canals or umbilicus, or at sites of surgical
scars
Pressure at the neck of the pouch may impair venous drainage of the
entrapped viscus , in severe cases both arterial & venous blood
supply lead to strangulation &infarction
ADHESIONS
Surgical procedures, infection, or other causes of peritoneal
inflammation, such as endometriosis, may result in development of
adhesion,
These fibrous bridges can create closed loops through which other
viscera may slide and become entrapped
VOLVULUS
Complete twisting of a loop of bowel about its mesenteric base of
attachment
occurs most often in large redundant loops of sigmoid colon, followed
in frequency by the cecum, small bowel, stomach, or, rarely,
transverse colon.
INTUSSUSCEPTION
when a segment of the intestine, constricted by a wave of peristalsis,
telescopes into the immediately distal segment
In infant & young children when a segment of the intestine,
constricted by a wave of peristalsis, telescopes into the immediately
distal segment
In older children and adults an intraluminal mass or tumor generally
serves as the point of traction that causes intussusception
18
Malabsorption:
defective absorption of fats, fat- and water-soluble vitamins, proteins,
carbohydrates, electrolytes and minerals, and water.
Clinically :
Chronic malabsorption can be accompanied by weight loss, anorexia,
abdominal distention, borborygmi, and muscle wasting. A hallmark
of malabsorption is steatorrhea
• Diseases that cause Malabsorbtion:
Celiac Disase
Cystic Fibrosis
Chronic pancreatitis
Primary bile acid malabsorption
Carcinoid syndrome
Autoimmune enteropathy
Disaccharidase deficiency
Whipple disease
Inflammatory bowel disease
Mechanisms of Malabsorbtion
Malabsorption results from disturbance in at least one of the four
phases of nutrient absorption:
(1) intraluminal digestion( proteins, carbohydrates, and fats)
(2) terminal digestion, which involves the hydrolysis of carbohydrates
and peptides by disaccharidases and peptidases, respectively, in the brush
border of the small intestinal mucosa
(3) transepithelial transport, in which nutrients, fluid, and electrolytes are
transported across and processed within the small intestinal epithelium
(4) lymphatic transport of absorbed lipids.
19
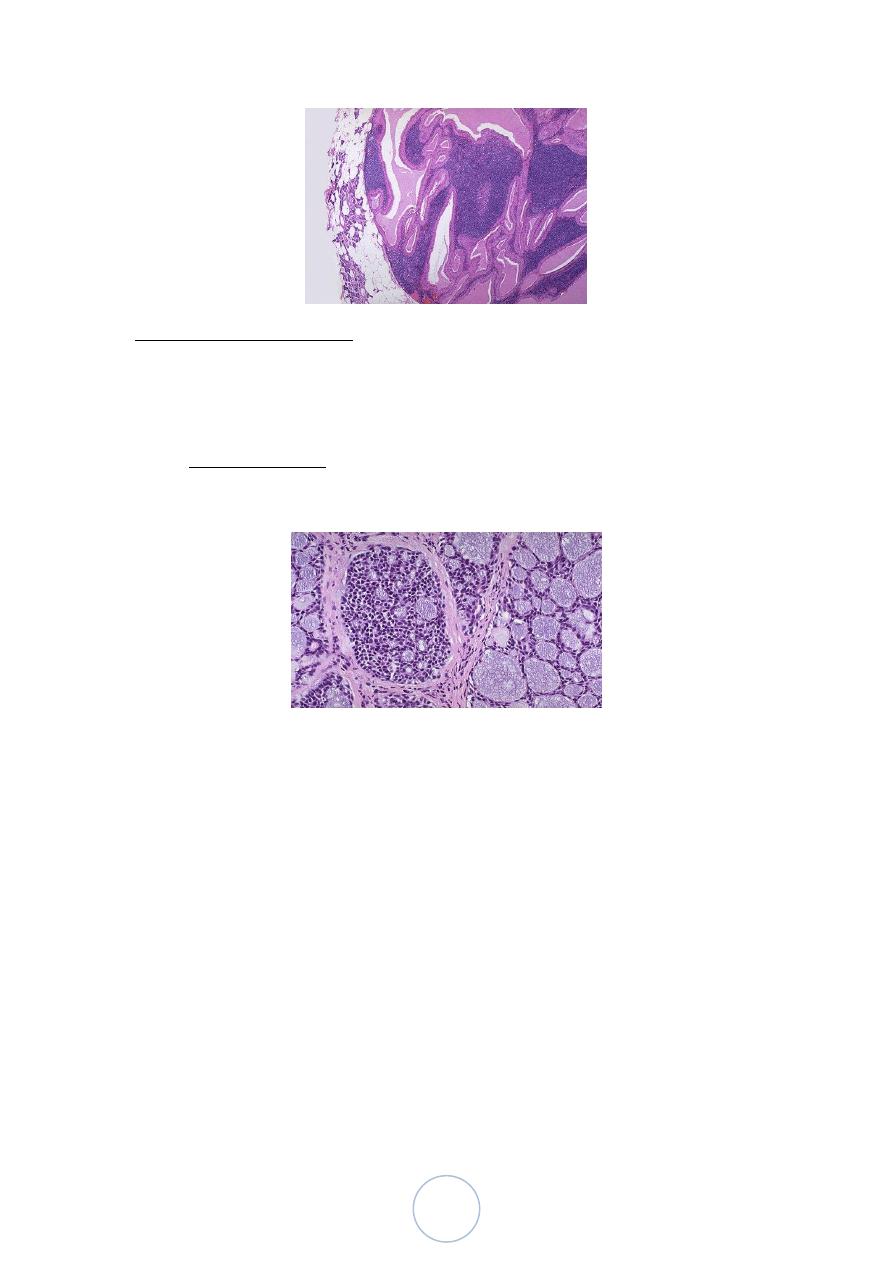
CELIAC DISEASE
celiac sprue or gluten-sensitive enteropathy
It is an immune-mediated enteropathy triggered by the
ingestion of gluten-containing cereals, such as wheat, rye, or
barley
genetically predisposed individuals
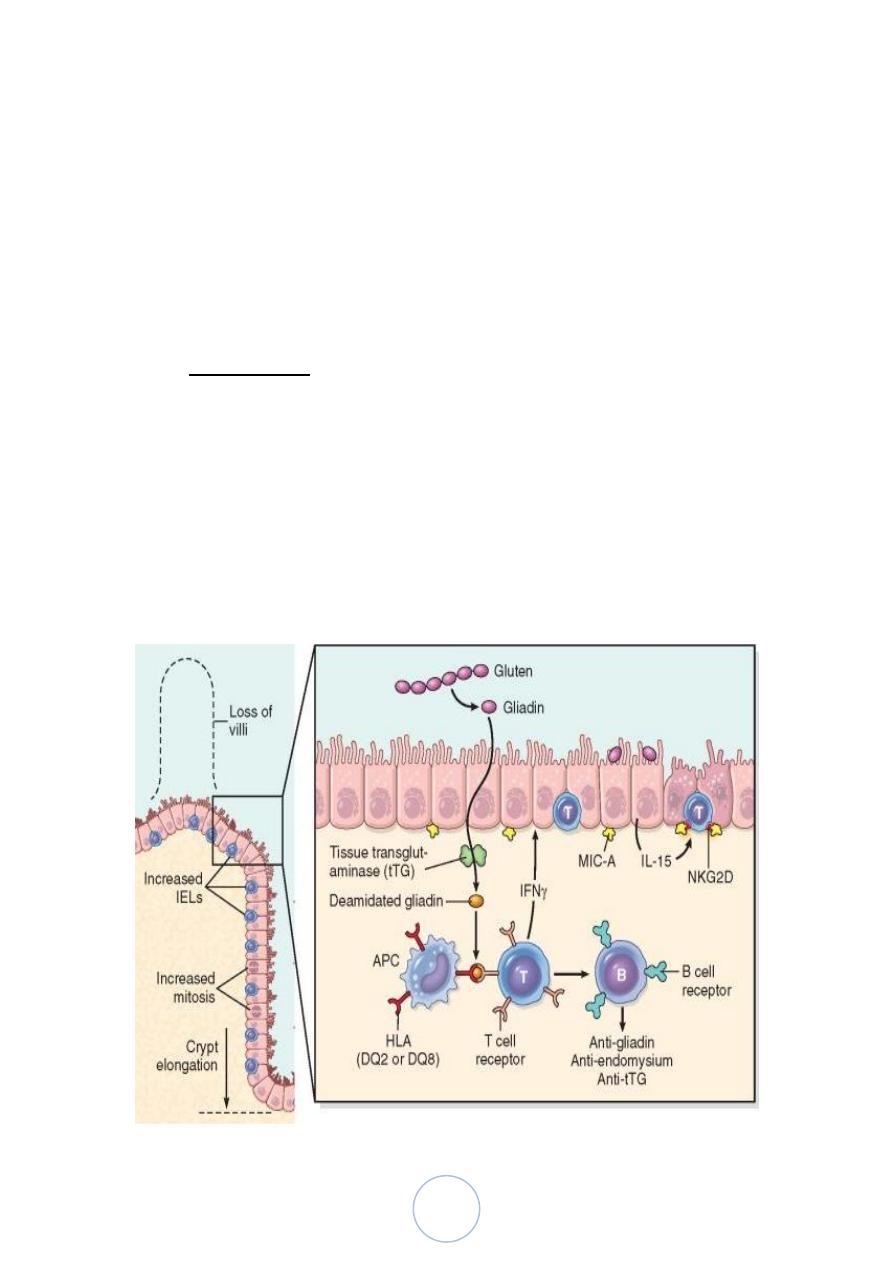
• Pathogenesis.
Gluten is the major storage protein of wheat and similar grains, and
the alcohol-soluble fraction of gluten
is digested by luminal and brush-border enzymes into amino acids
and peptides
Some gliadin peptides induce epithelial cells to express IL-15,
which in turn triggers activation and proliferation of CD8+
intraepithelial lymphocytes
induced to express NKG2D, a natural killer cell marker
20
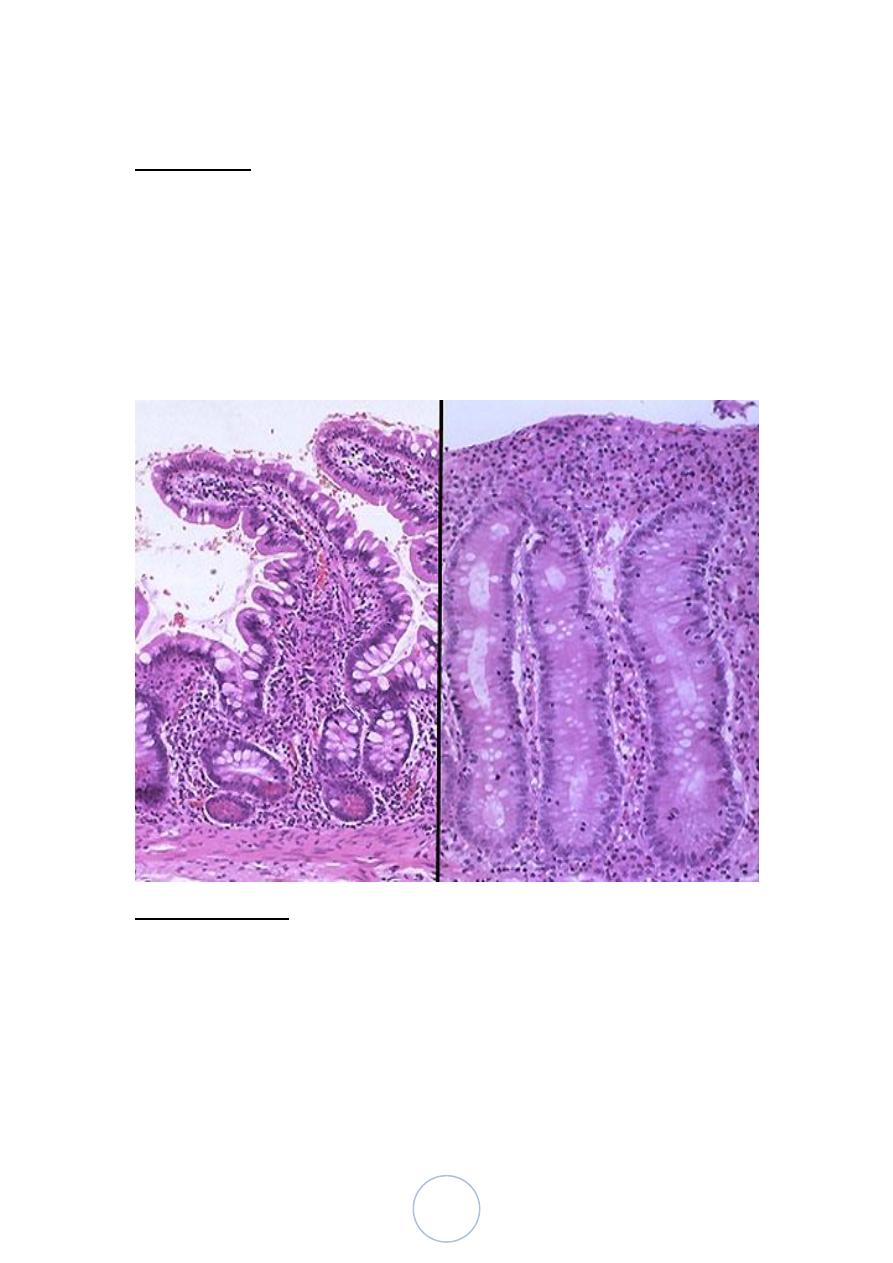
Morphology.
Biopsy specimens from the second portion of the duodenum or
proximal jejunum
increased numbers of intraepithelial CD8+ T lymphocytes
(intraepithelial lymphocytosis), crypt hyperplasia, and villous
atrophy
Other features of fully developed celiac disease include increased
numbers of plasma cells, mast cells, and eosinophils,
Clinical Features:
Pediatric celiac disease, which affects males and females equally,
may present with malabsorption, disease typically begins between
ages of 6 and 24 months,
In adults, celiac disease presents most commonly between the ages
of 30 and 60.
Symptomatic adult celiac disease is often associated with anemia,
chronic diarrhea, bloating, or chronic fatigue.
21
Common extra-intestinal complaints include arthritis or joint pain,
seizure disorders, aphthous stomatitis, iron deficiency anemia,
pubertal delay, and short stature.
itchy, blistering skin lesion, dermatitis herpetiformis
The most common celiac disease–associated cancer is enteropathy-
associated T-cell lymphoma, to lesser extent adenocarcinoma of
small intestine
PSEUDOMEMBRANOUS COLITIS
known as antibiotic-associated colitis or antibiotic-associated
diarrhea
caused by Clostridium difficile
apply to diarrhea developing during or after a course of antibiotic
therapy
Pathogenesis:
It is likely that disruption of the normal colonic flora by antibiotics
allows C. difficile overgrowth
Immunosuppression is also a predisposing factor for C. difficile
colitis.
Toxins released by C. difficile lead to disruption of the epithelial
cytoskeleton, tight junction barrier loss, cytokine release, and
apoptosis
Morphology.
• Fully developed C. difficile–associated colitis is accompanied by
formation of pseudomembranes
• layer of inflammatory cells and debris at sites of colonic mucosal
injury
• The surface epithelium is denuded, and the superficial lamina
propria contains a dense infiltrate of neutrophils and occasional
fibrin thrombi within capillaries
22
WHIPPLE DISEASE
is a rare, multivisceral chronic disease
Clinical symptoms occur because organism-laden macrophages
accumulate within the small intestinal lamina propria and
mesenteric lymph nodes, causing lymphatic obstruction.
Morphology.
• The morphologic hallmark of Whipple disease is a dense
accumulation of distended, foamy macrophages in the small
intestinal lamina propria
• The villous expansion caused by the dense macrophage infiltrate
imparts a shaggy gross appearance to the mucosal surface.
Lymphatic dilatation and mucosal lipid deposition account for the
common endoscopic detection of white to yellow mucosal plaques
• bacteria-laden macrophages can accumulate within mesenteric
lymph nodes, synovial membranes of affected joints, cardiac
valves, the brain,
23
Lec:8
Inflammatory Bowel Disease
is a chronic condition resulting from inappropriate mucosal immune
activation
IBD includes Crohn disease and ulcerative colitis
24
Pathogenesis:
IBD is an idiopathic disorder
Genetics. Genetic factors contribute to IBD
Mucosal immune responses. Although the mechanisms by
which mucosal immunity contributes to ulcerative colitis and
Crohn disease
Epithelial defects
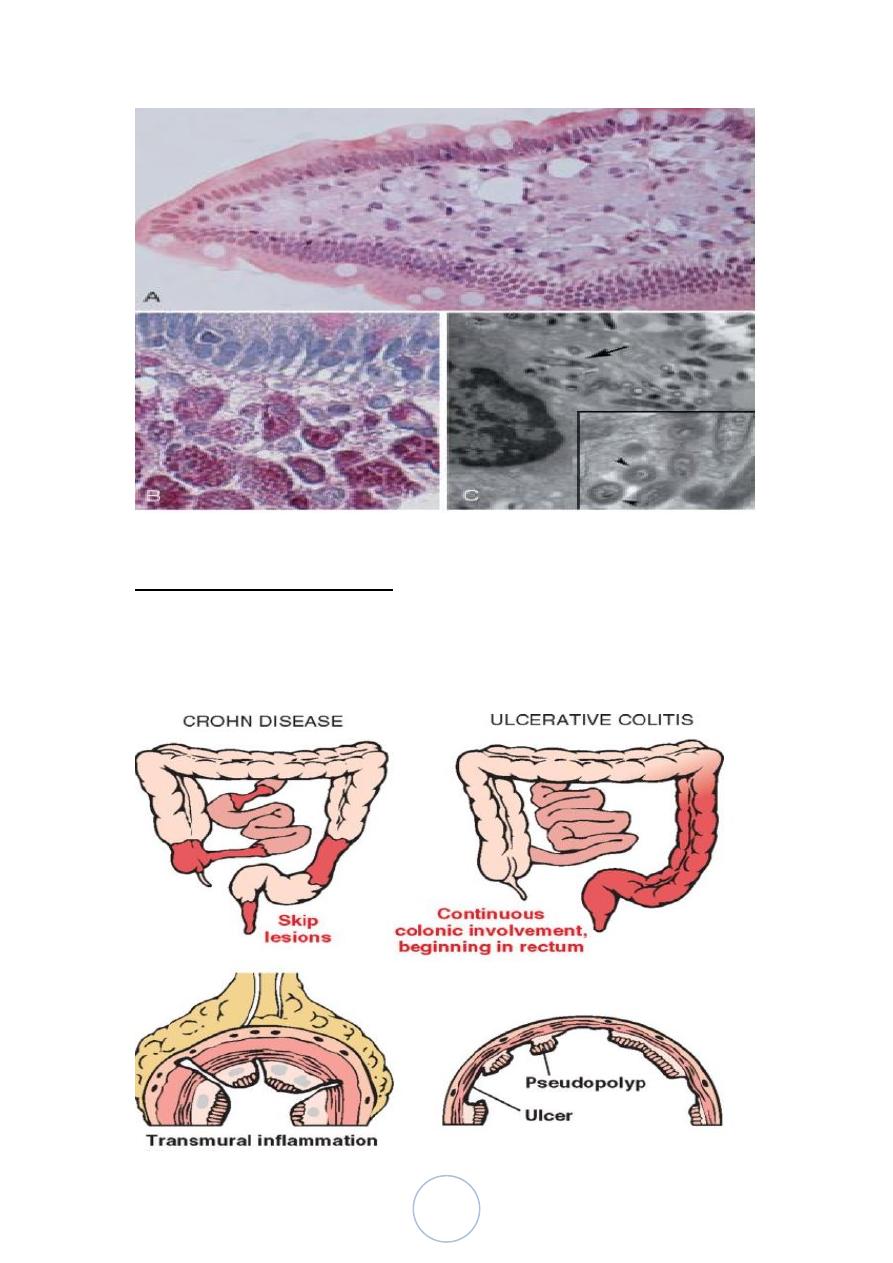
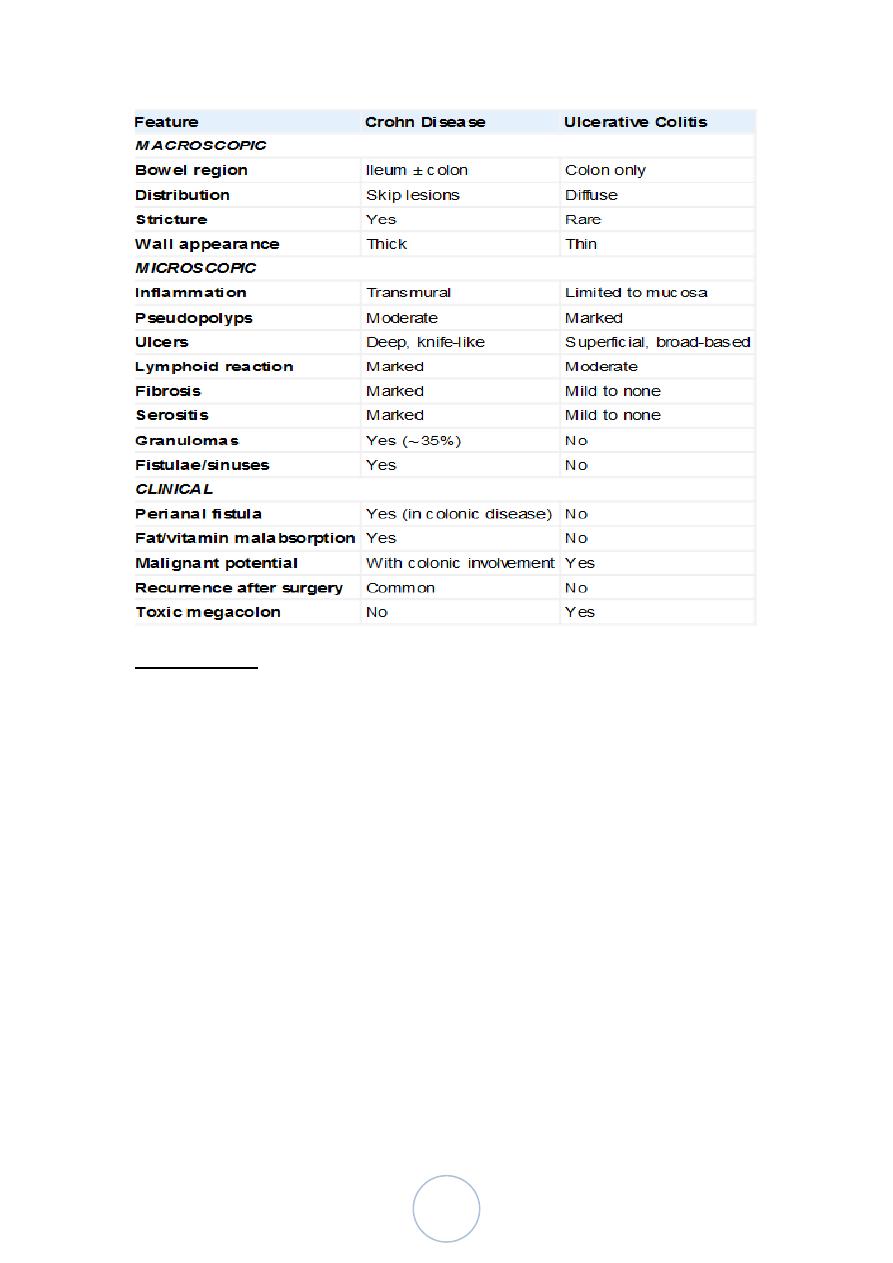
CROHN DISEASE
Morphology.
Crohn disease may occur in any area of the GI tract, but the most
common sites involved at presentation are the terminal ileum,
ileocecal valve, and cecum.
25
is limited to the small intestine alone in about 40% of cases; the
small intestine and colon are both involved in 30% of patients; and
the remainder have only colonic involvement.
The presence of multiple, separate, sharply delineated areas of
disease, resulting in skip lesions,
cobblestone appearance in which diseased tissue is depressed
below the level of normal mucosa
Fissures frequently develop between mucosal folds and may extend
deeply to become fistula tracts or sites of perforation
The intestinal wall is thickened and rubbery as a consequence of
transmural edema, inflammation, submucosal fibrosis, and
hypertrophy of the muscularis propria, all of which contribute to
stricture formation
• The microscopic features of active Crohn disease
1. Crypt abscesses : Clusters of neutrophils within a crypt .
2. Distortion of mucosal architecture : the normally straight and
parallel crypts take on bizarre branching shapes and unusual
orientations to one another
3. Epithelial metaplasia gastric antral-appearing glands , panth
cell metaplasia
4. Ulceration of the linning mucosa
5. Noncaseating granulomas a hallmark of Crohn disease, are
found in approximately 35% of cases, The absence of
granulomas does not preclude a diagnosis of Crohn disease
26
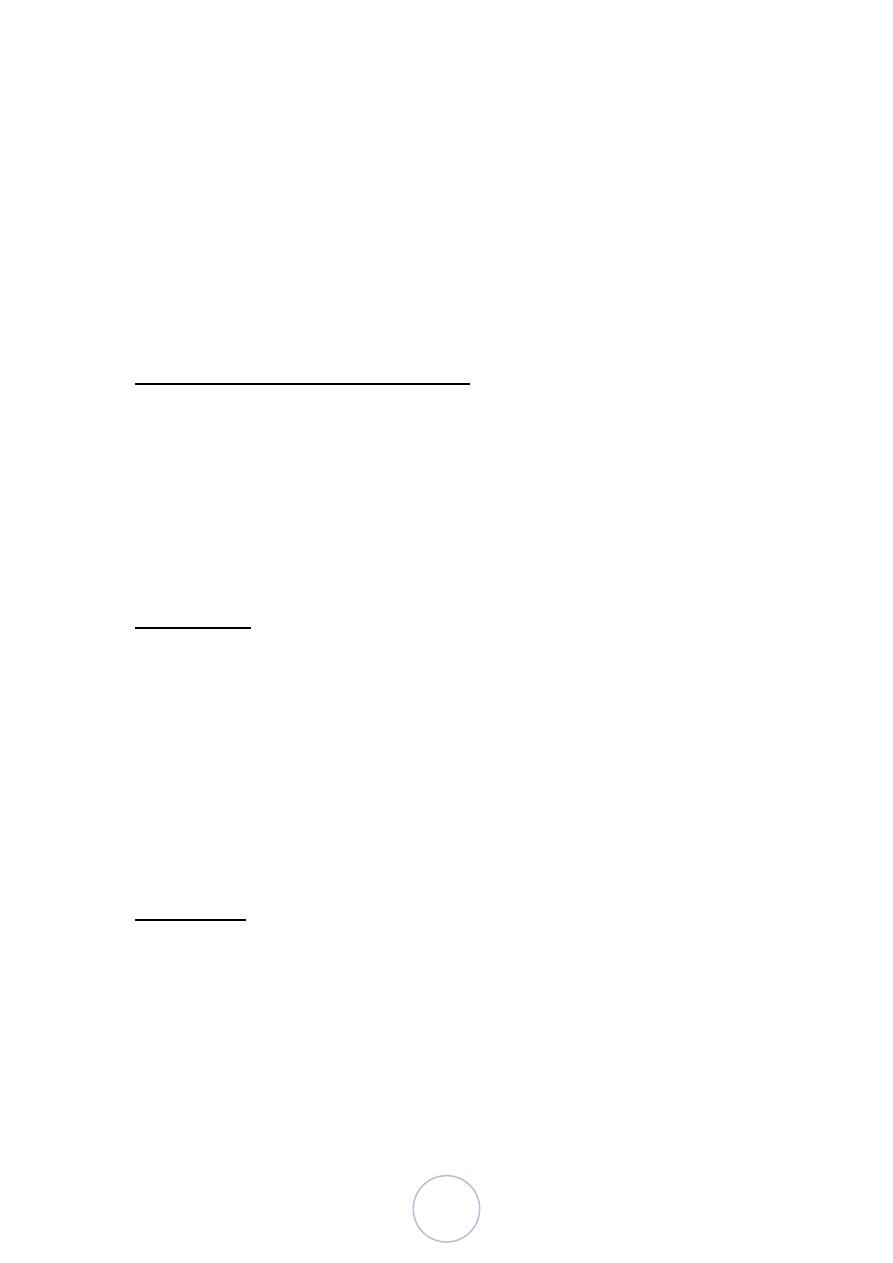
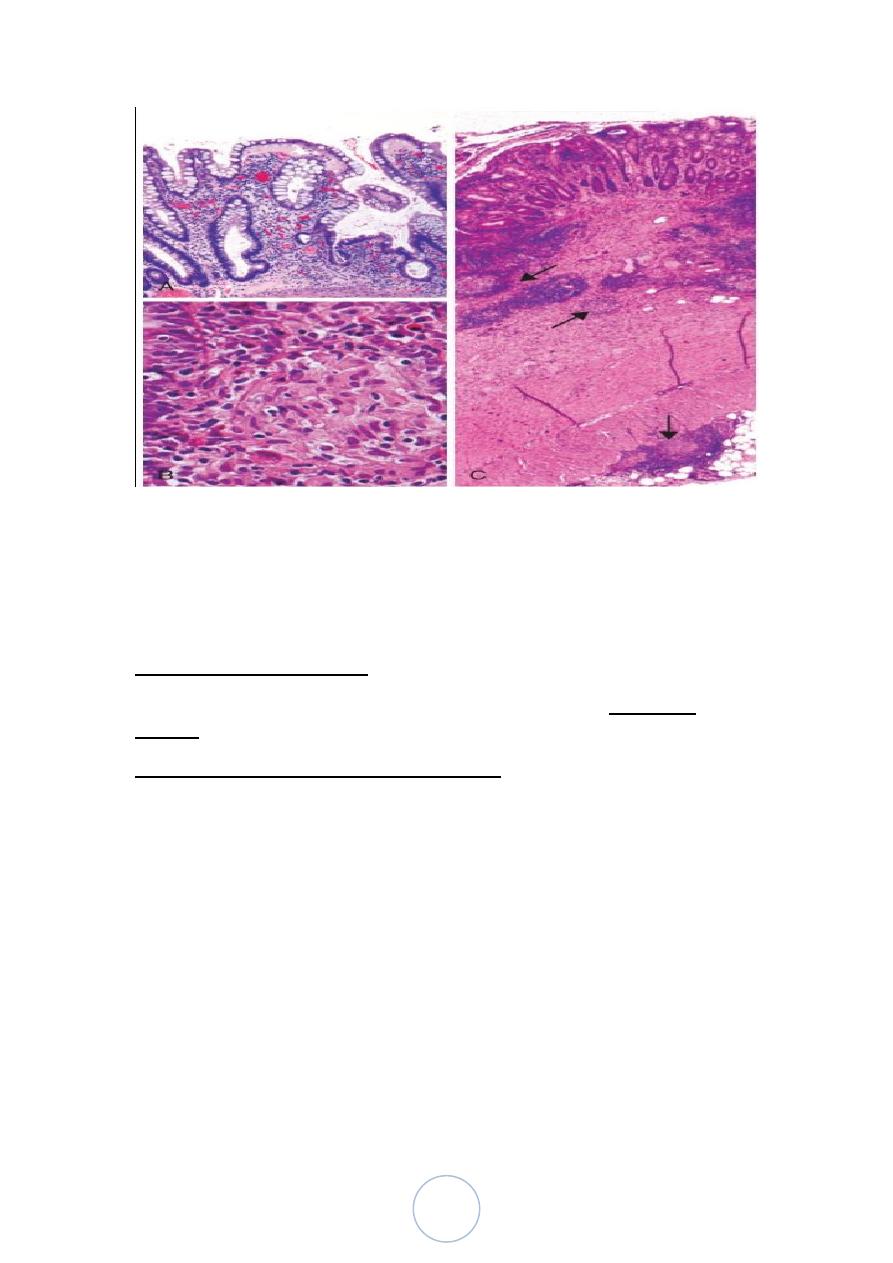
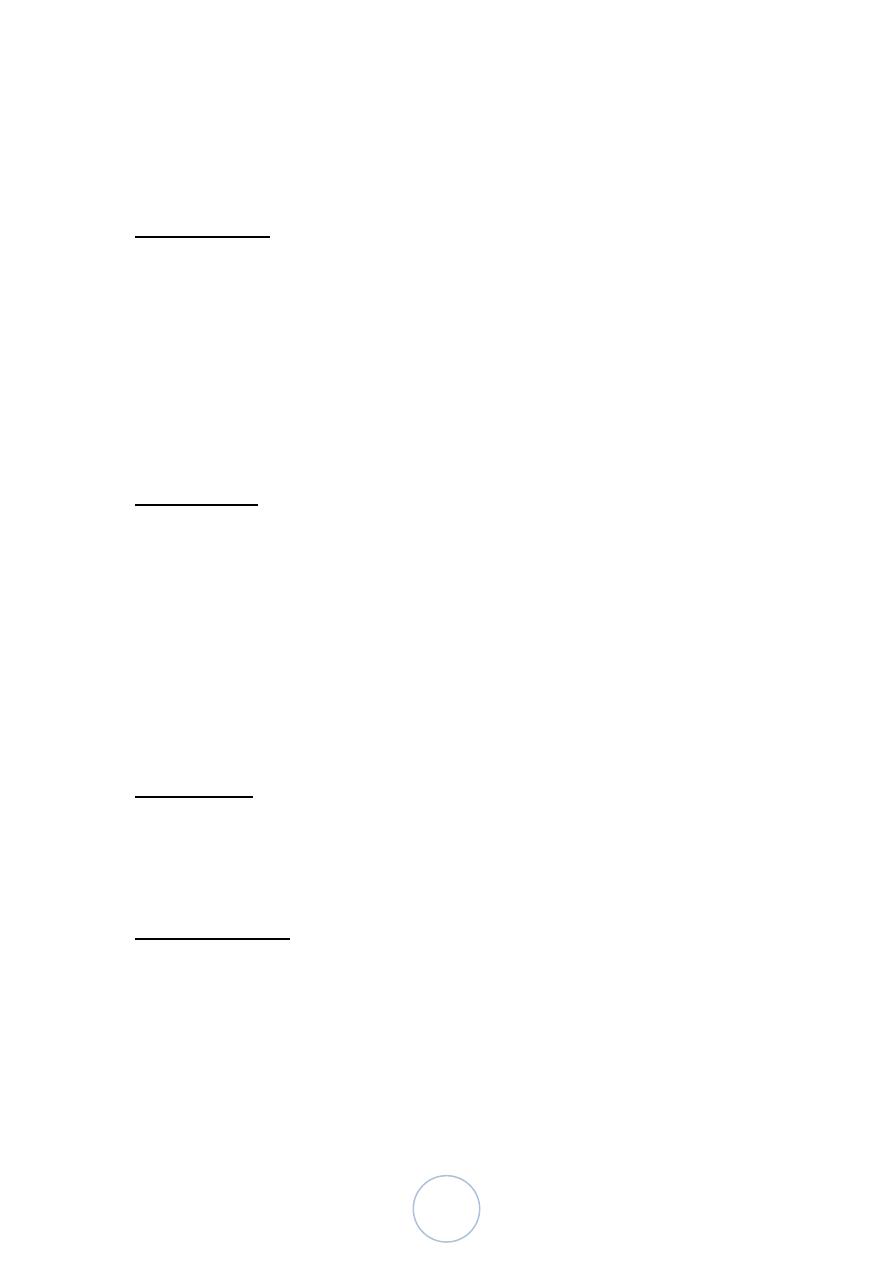
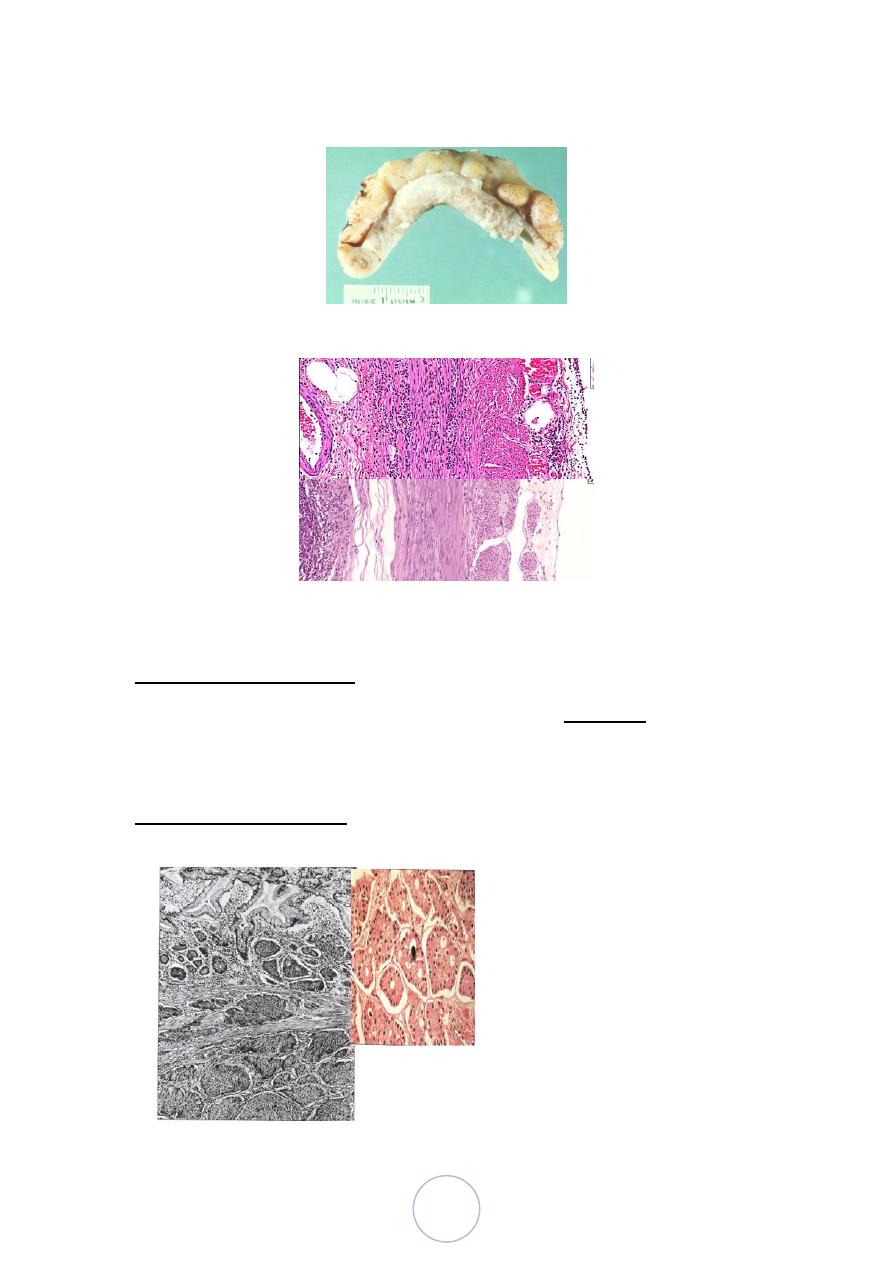
Microscopic pathology of Crohn disease. A, Haphazard crypt
organization results from repeated injury and regeneration. B,
Noncaseating granuloma. C, Transmural Crohn disease with
submucosal and serosal granulomas (arrows).
ULCERATIVE COLITIS
intestinal disease in ulcerative colitis is limited to the colon and
rectum
Common extra-intestinal manifestations of ulcerative colitis overlap
with those of Crohn disease and include
migratory polyarthritis, sacroiliitis, ankylosing spondylitis, uveitis,
skin lesions, pericholangitis, and primary sclerosing cholangitis
Morphology:
Grossly :
ulcerative colitis always involves the rectum and extends proximally
in a continuous fashion to involve part or all of the colon.
Most of the cases pancolitis , Limited distal disease may be referred
to descriptively as ulcerative proctitis or ulcerative proctosigmoiditis.
27
Grossly:
involved colonic mucosa may be slightly red and granular or
have extensive, broad-based ulcers
Isolated islands of regenerating mucosa often bulge into the
lumen to create pseudopolyps
mural thickening is not present, the serosal surface is normal,
and strictures do not occur
• Histologic features :
the inflammatory process is diffuse and generally limited to the
mucosa and superficial submucosa
Granulomas are not present in ulcerative colitis.
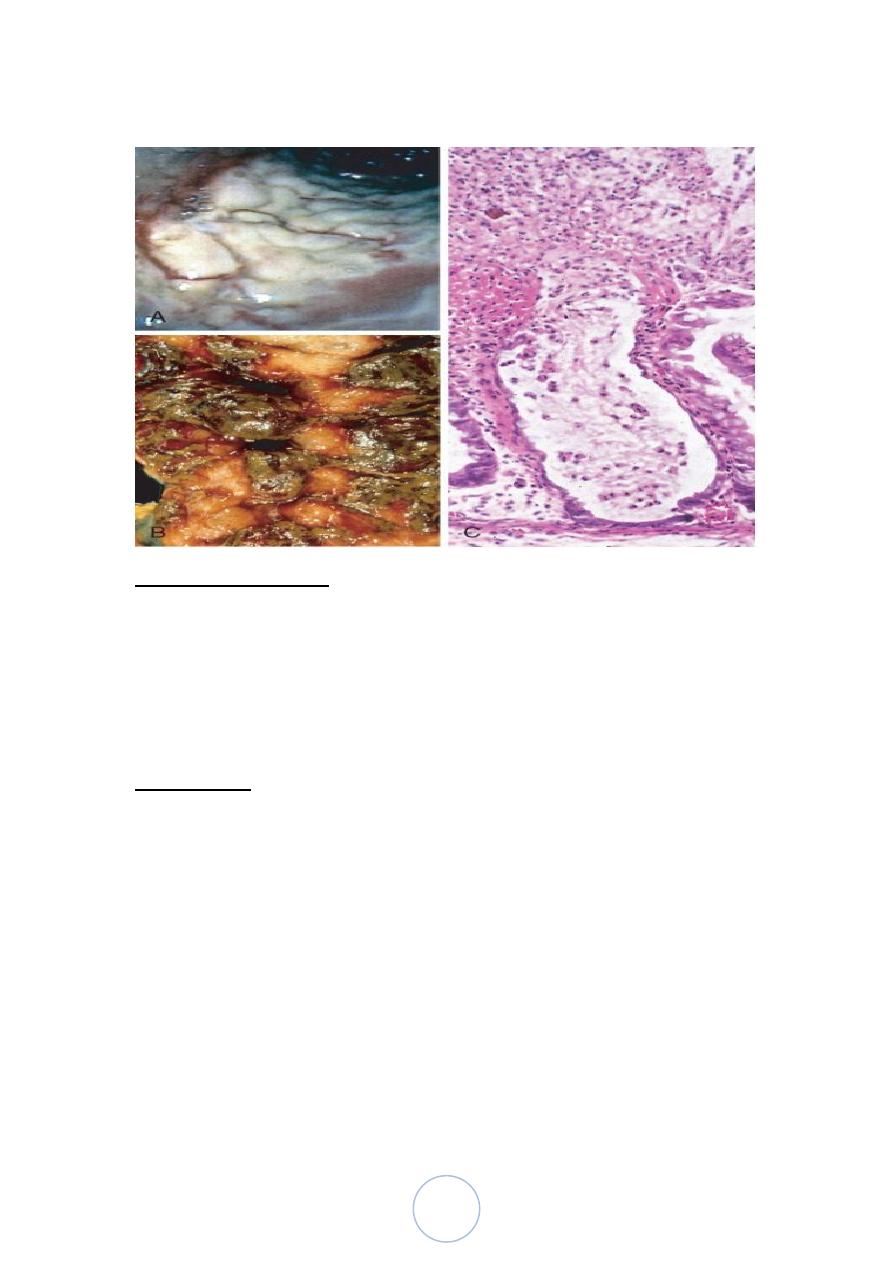
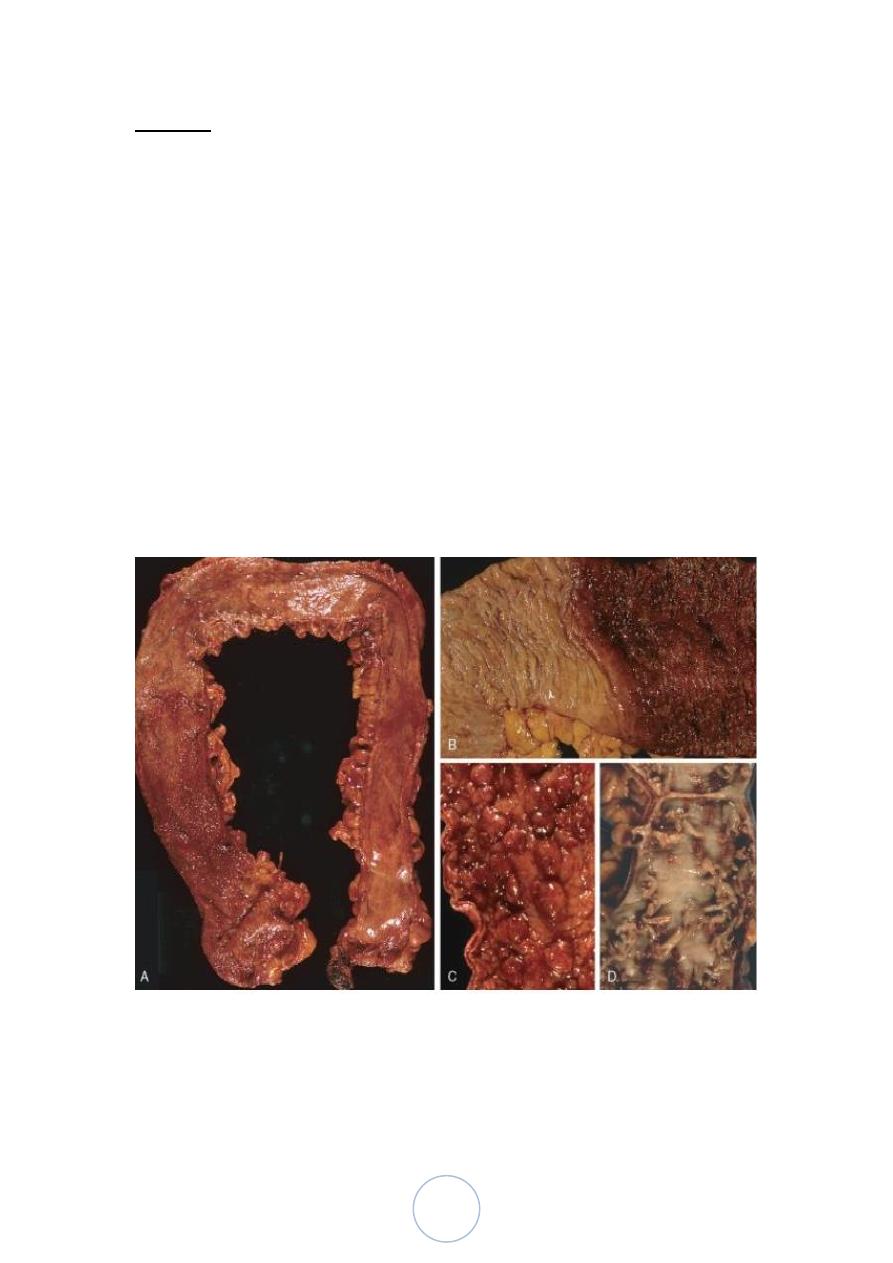
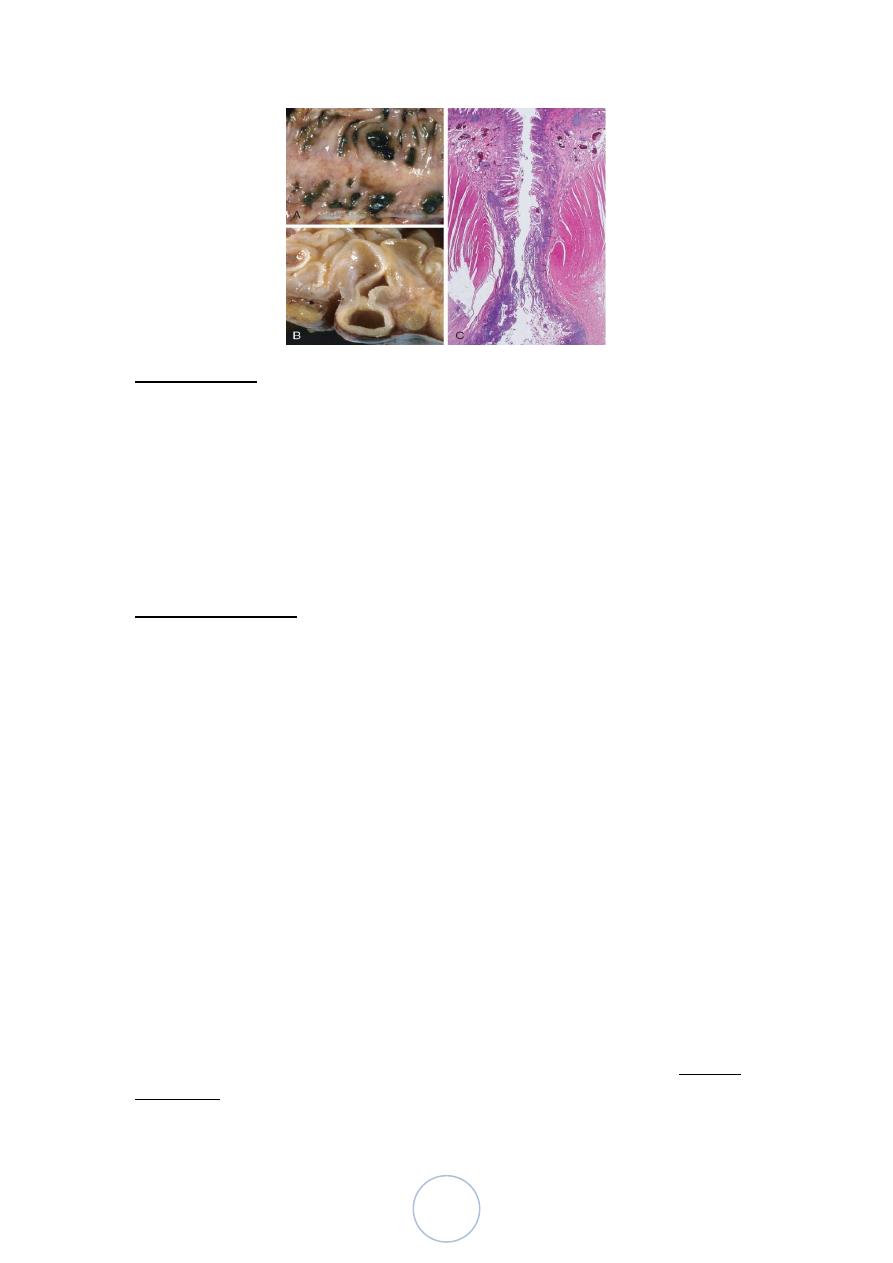
Gross pathology of ulcerative colitis. A, Total colectomy with
pancolitis showing active disease, with red, granular mucosa in the
cecum (left) and smooth, atrophic mucosa distally (right). B, Sharp
demarcation between active ulcerative colitis (right) and normal
(left). C, Inflammatory polyps. D, Mucosal bridges.
28
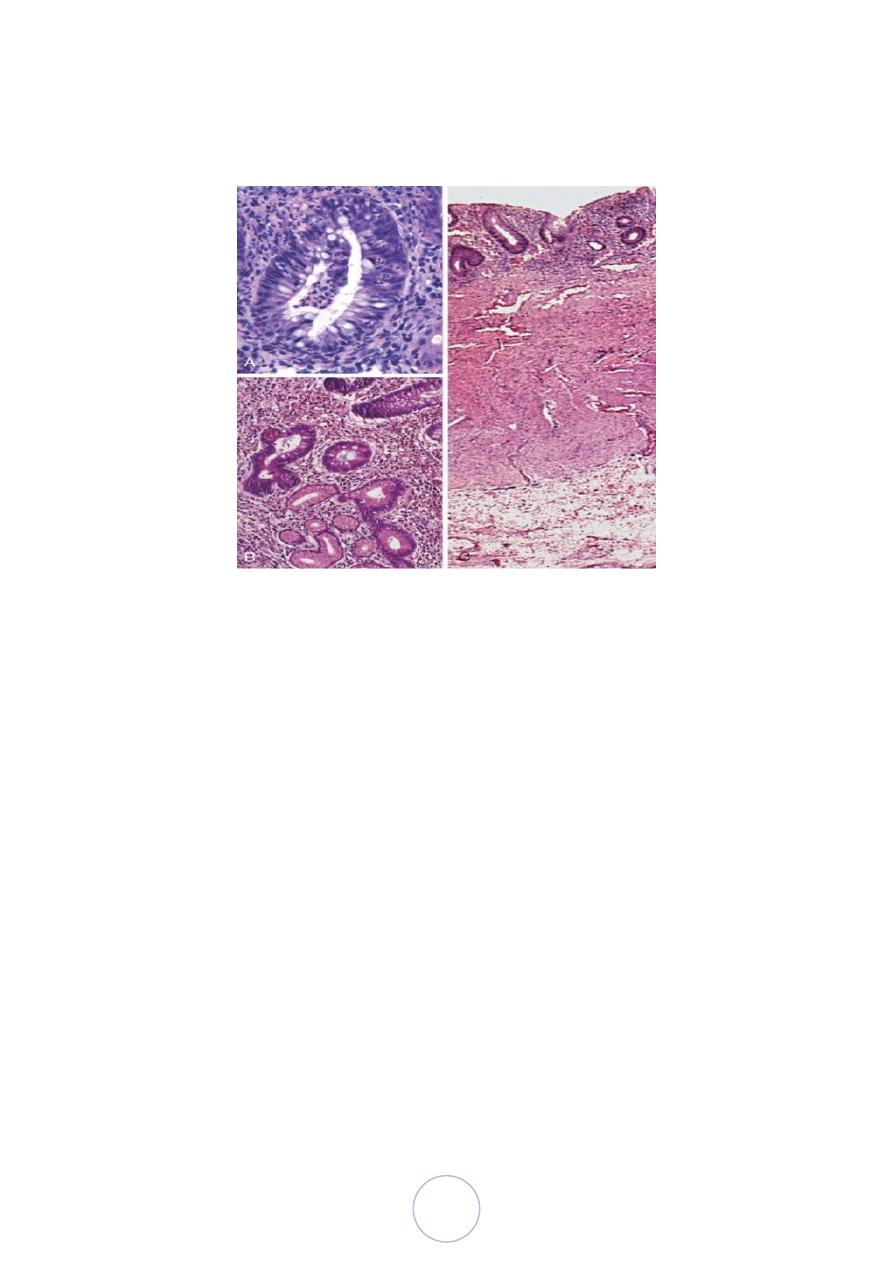
Microscopic pathology of ulcerative colitis. A, Crypt abscess. B,
Pseudopyloric metaplasia (bottom). C, Disease is limited to the
mucosa
Colitis-Associated Neoplasia
Risk increases sharply 8 to 10 years after disease initiation
Patients with pancolitis are at greater risk than those with only left-
sided disease
Greater frequency and severity of active inflammation (characterized
by the presence of neutrophils) may increase risk
29
د. ندوى امراض
01
\
3
\
8108
( عدد االوراق
1
) م
\
3
\
موصل
lec: 8
Diverticulosis :
Acquired pseudo-diverticular outpouchings of the colonic
mucosa and submucosa.
Rare in persons under age 30, but the prevalence approaches
50% in Western adult populations over age 60.
Occurs due to increased intraluminal pressure in the sigmoid ,
due to constipation (low fiber diet)
Pathogenesis:
Increased intraluminal pressure is probably due to exaggerated
peristaltic contractions.
may be enhanced by diets low in fiber, which reduce stool bulk,
particularly in the sigmoid colon.
nerves, arterial vasa recta, and their connective tissue sheaths
penetrate the inner circular muscle coat, focal discontinuities in
the muscle wall are created.
Morphology:
colonic diverticula are small, flask-like outpouchings, usually 0.5 to 1
cm in diameter
regular distribution alongside the taeniae coli
Microscopically :
Colonic diverticula have a thin wall composed of a flattened or
atrophic mucosa, compressed submucosa, and attenuated or,
most often, totally absent muscularis propria
Obstruction of diverticulae leads to inflammatory changes,
producing diverticulitis and peri-diverticulitis
30
Complication
Ulceration
Bacterial infection & abscess formation
Perforation & peritonitis
Fistula formation (with bladder , vagina)
Intestinal Polyps :
Non-neoplastic polyp
• Inflammatory polyp : form as a result of chronic cycles of
injury and healing. ( seen in large bowel in Inflammatory
disases as crohn’s disease or ulcerative colitis)
• Hamartomatous polyp tumor-like growths composed of mature
tissues that are normally present at the site in which they
develop e.g/ autosomal dominant inherited condition of Peutz–
Jeghers syndrome,
Neoplastic polyp:
more common in the large than small bowel , about one-third of
individuals at 60-70 years of age.
the most common and clinically important neoplastic polyps are colonic
adenomas, benign polyps that are precursors to the majority of colorectal
adenocarcinomas.
31
Adenomas are intraepithelial neoplasms that range from small,
often pedunculated polyps to large sessile lesions
Most adenomas are clinically silent, with the exception of large
polyps that produce occult bleeding and anemia and rare
villous adenomas that cause hypoproteinemic hypokalemia by
secreting large amounts of protein and potassium
Morphology
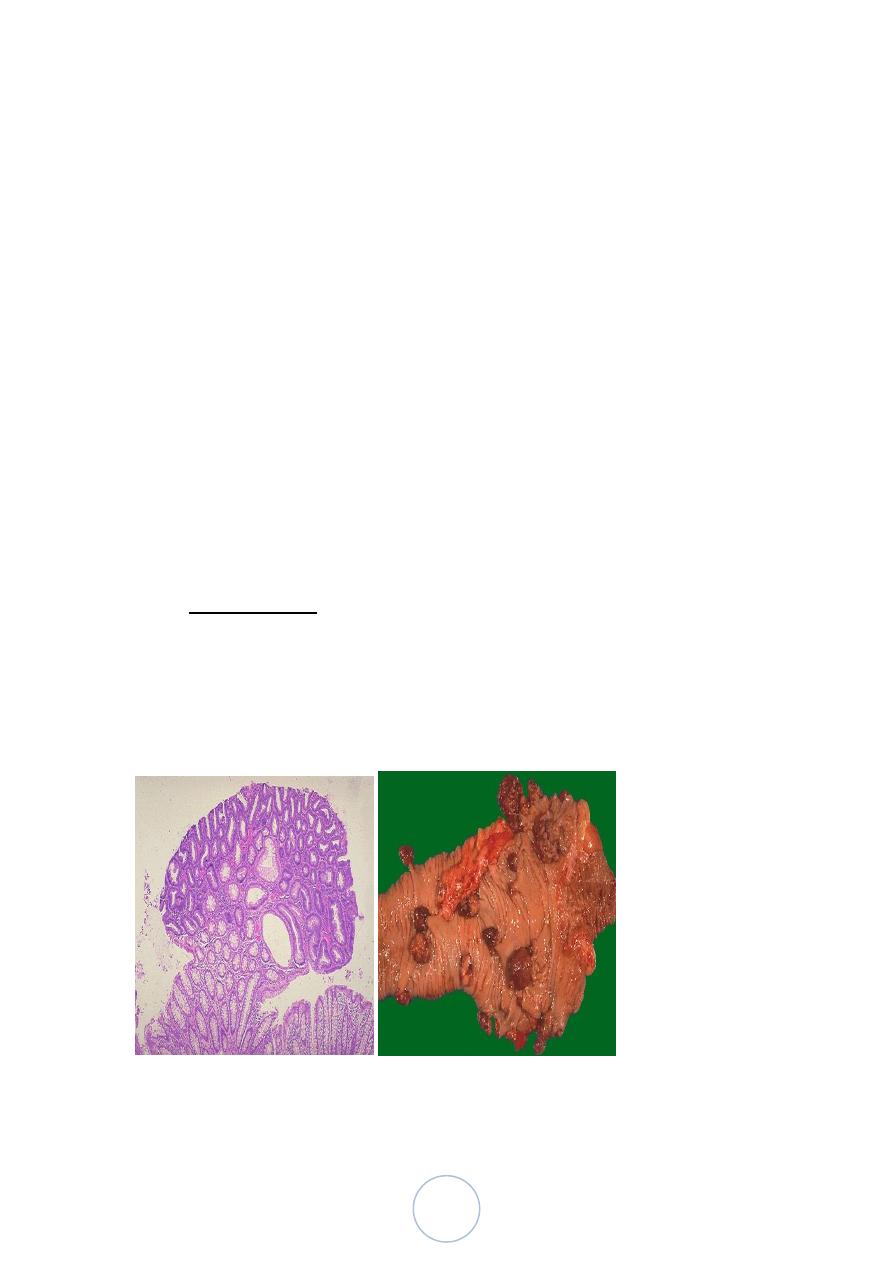
• Adenomas can be classified as tubular, tubulovillous, or villous
based on their architecture
• Tubular adenomas tend to be small, pedunculated polyps composed
of small rounded, or tubular, glands
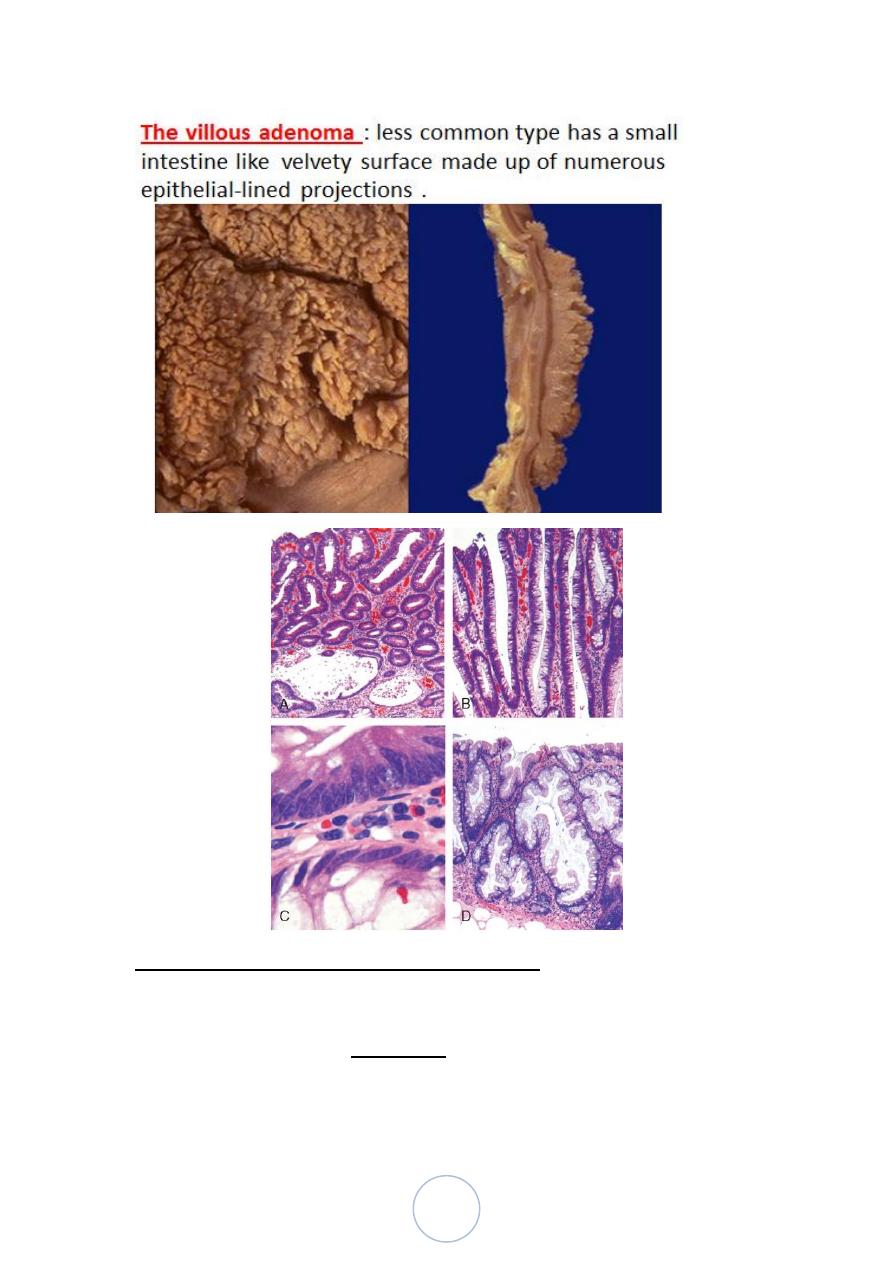
• villous adenomas, which are often larger and sessile, are covered
by slender villi
• Tubulovillous adenomas have a mixture of tubular and villous
• Histologically, the cytologic hallmark of epithelial dysplasia is
nuclear hyperchromasia, elongation, and stratification.
The tubular adenoma:
32
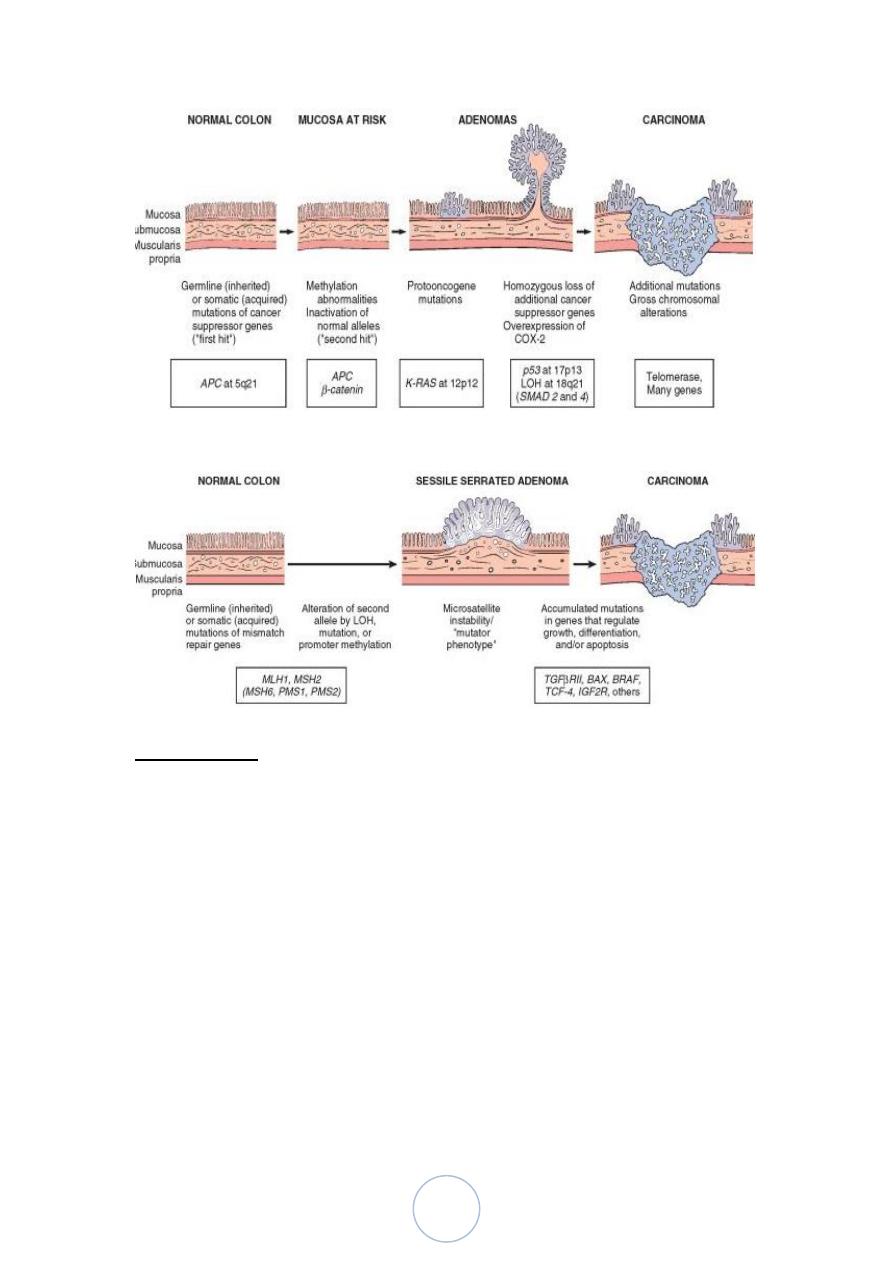
FAMILIAL ADENOMATOUS POLYPOSIS
Familial adenomatous polyposis (FAP) is an autosomal dominant
disorder in which patients develop numerous colorectal adenomas as
teenagers. It is caused by mutations of the adenomatous polyposis coli,
or APC, gene.
At least 100 polyps are necessary for a diagnosis of classic FAP
33
Colorectal adenocarcinoma develops in 100% of untreated FAP
patients, often before age 30.
As a result, prophylactic colectomy is the standard therapy for
individuals carrying APC mutations.
Adenocarcinoma
Adenocarcinoma of the colon is the most common malignancy of the
GI tract and is a major cause of morbidity and mortality worldwide
Low fiber diet , high intake of refind carbohydrate &Fat.
Low antioxidant Vit A,C,E
(all had a role in developing adenocarcinoma of large bowel).
34
Morphology :
About one-half are found in the rectum, a further
one-third in the sigmoid, and the rest are spread equally
across the remainder of the colon
Tumors of proximal colon appear as exophytic or ulcerative mass
rarely cause obstruction
In distal part presented as annular lesion cause narrowing of lumen
and obstruction .
Tumors composed of glandular structures lined by malignant cells
at different differentiation
Some times signet ring ca. as in gastric Ca.
35
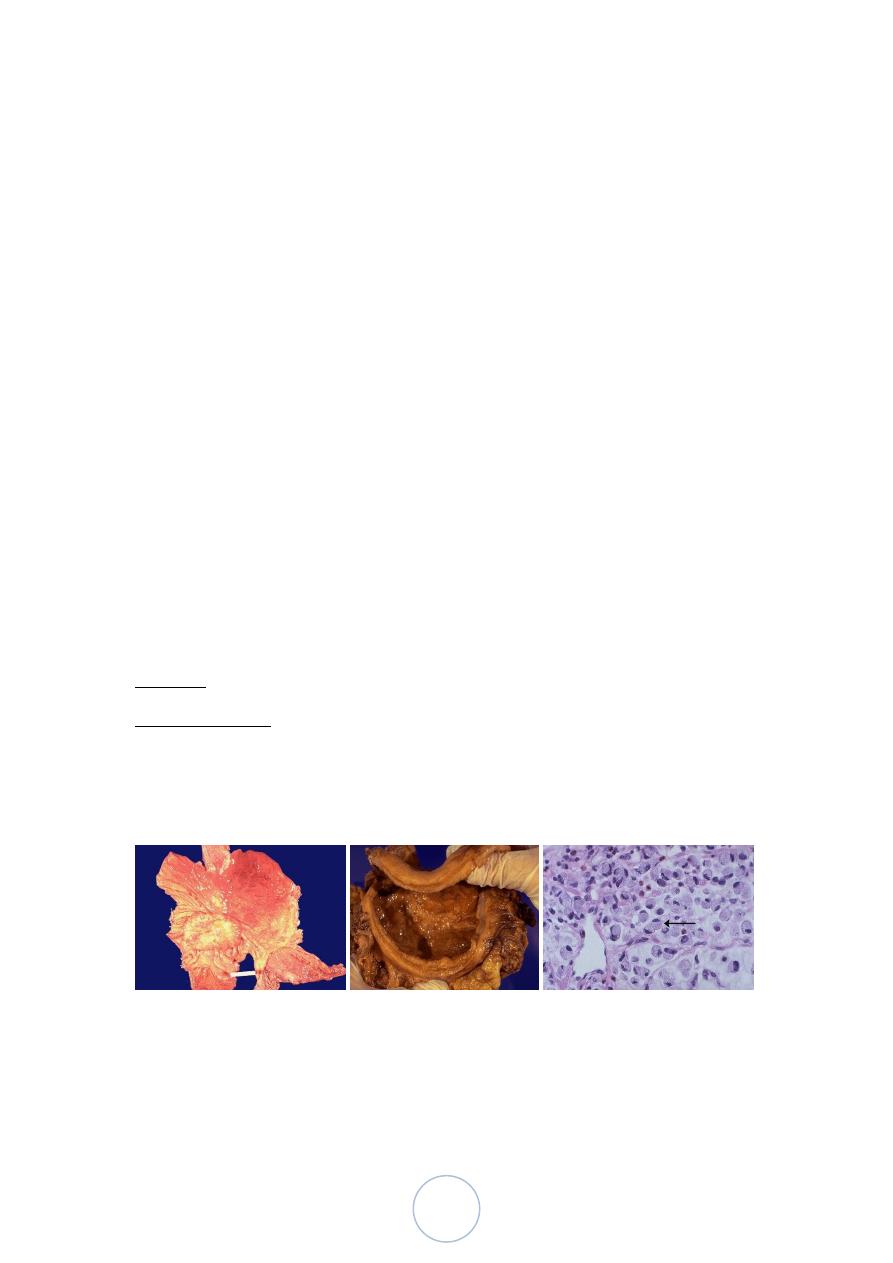
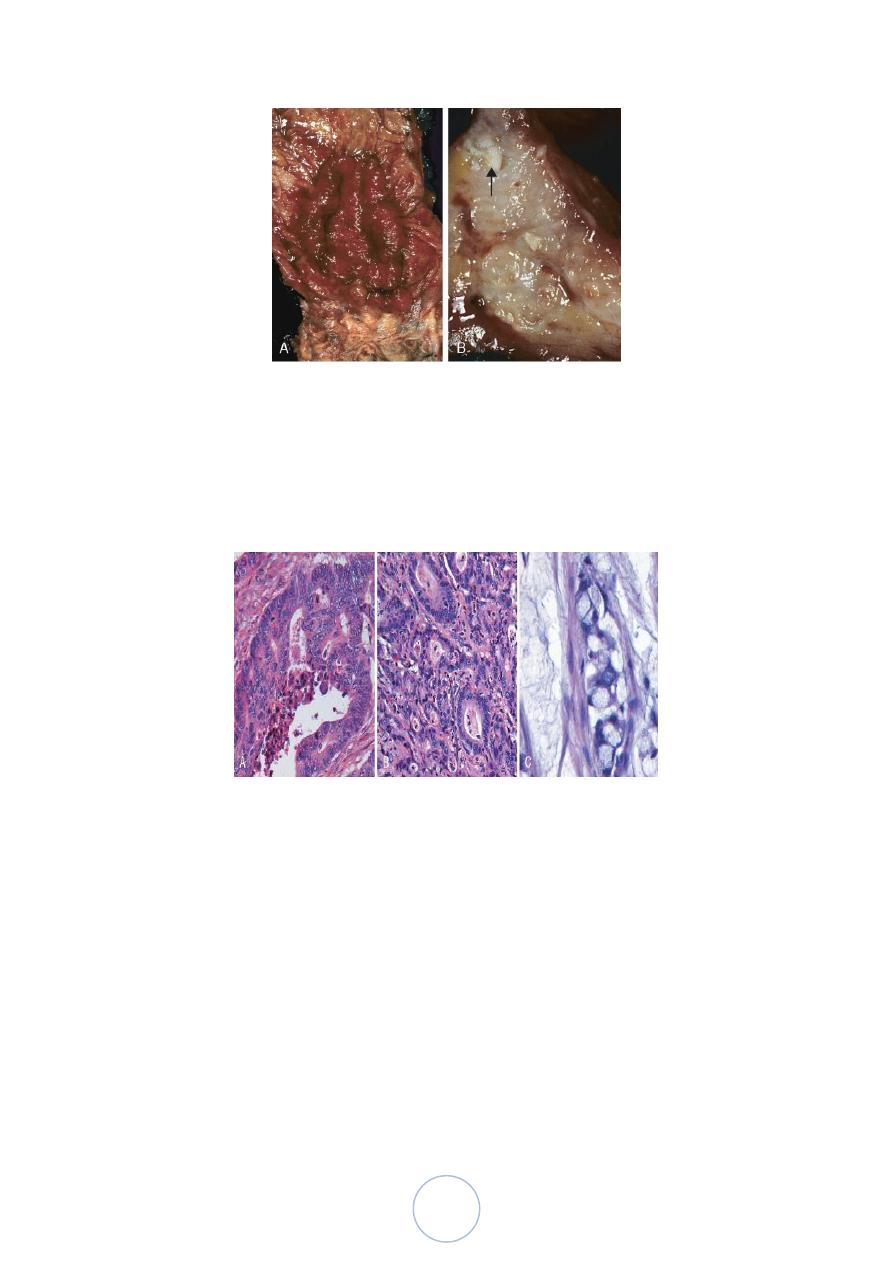
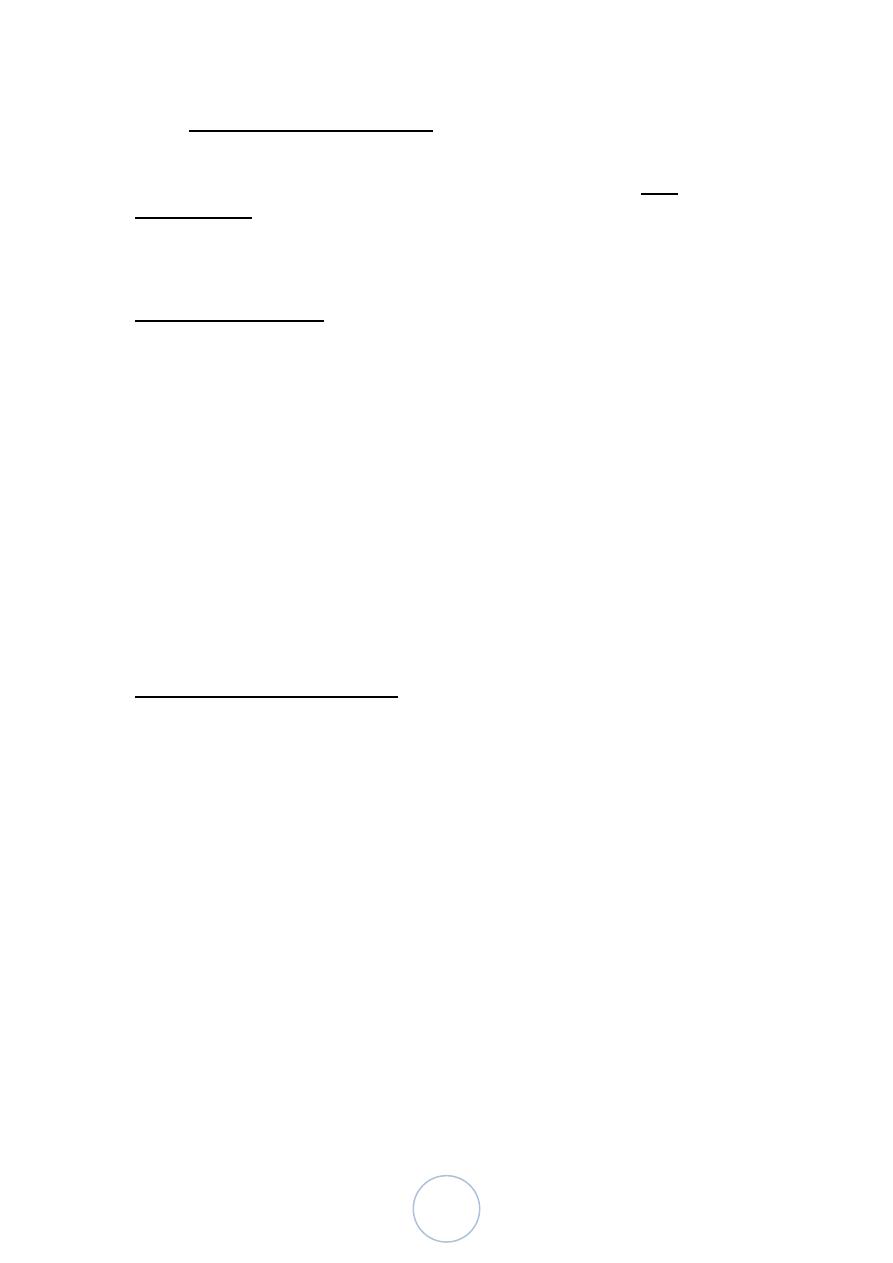
Colorectal carcinoma. A, Circumferential, ulcerated rectal cancer.
Note the anal mucosa at the bottom of the image. B, Cancer of the
sigmoid colon that has invaded through the muscularis propria and
is present within subserosal adipose tissue (left). Areas of chalky
necrosis are present within the colon wall (arrow).
Histologic appearance of colorectal carcinoma. A, Well-differentiated
adenocarcinoma. Note the elongated, hyperchromatic nuclei.
Necrotic debris, present in the gland lumen, is typical. B, Poorly
differentiated adenocarcinoma forms a few glands but is largely
composed of infiltrating nests of tumor cells. C, Mucinous
adenocarcinoma with signet-ring cells and extracellular mucin pools.
The two most important prognostic factors are depth of invasion
and the presence or absence of lymph node metastases.
Invasion into the muscularis propria confers significantly
reduced survival that is decreased further by the presence of
lymph node metastases
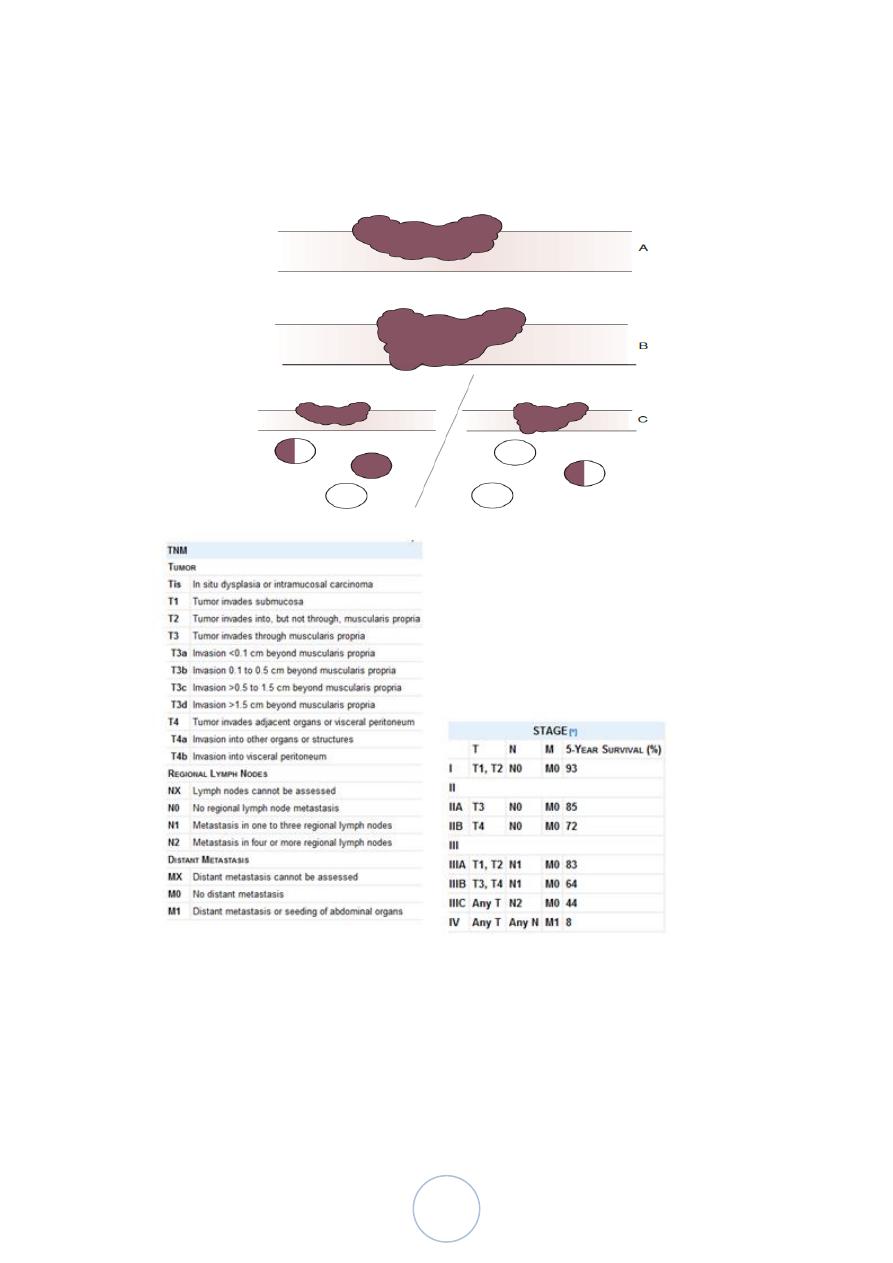
36
• Many systems for staging of colorectal ca. one of them Dukes
Staging System
ANAL CANAL CARCINOMAS
MORE LIKELY TO BE SQUAMOUS, or “basaloid”
WORSE IN PROGNOSIS
HPV RELATED
37
د. ندوى امراض
01
\
3
\
8108
( عدد االوراق
8
) م
\
3
\
موصل
lec: 9
Hemorrhoids:
affect about 5% of the general population and develop secondary to
persistently elevated venous pressure within the hemorrhoidal plexus
The most frequent predisposing influences are straining at stool
because of constipation and the venous stasis of pregnancy.
Morphology.
Collateral vessels within the inferior hemorrhoidal plexus are located
below the anorectal line and are termed external hemorrhoids
while those that result from dilation of the superior hemorrhoidal plexus
within the distal rectum are referred to as internal hemorrhoids
Histologically,
thin-walled, dilated, submucosal vessels that protrude beneath the anal or
rectal mucosa.
In their exposed position, they are subject to trauma and tend to
become inflamed, thrombosed, and, in the course of time,
recanalized. Superficial ulceration may occur.
THE APPENDIX
is a normal true diverticulum of the cecum that is prone to
acute and chronic inflammation
Acute Appendicitis
o initiated by progressive increases in intraluminal pressure that
compromise venous outflow. In 50% to 80% of cases, acute
appendicitis is associated with overt luminal obstruction caused
by stool (fecolith, oxyuriasis vermicularis (worm), tumor…)
o Microscopically: transmural infiltration of neutrophils with
ulceration of linning mucosa
38
ACUTE APPENDICITIS
What is the white junk coating the surface? Answer: FIBRIN
The presence of neutrophils invading the muscularis is the diagnostic
criteria needed to diagnosis or confirm, acute appendicitis!
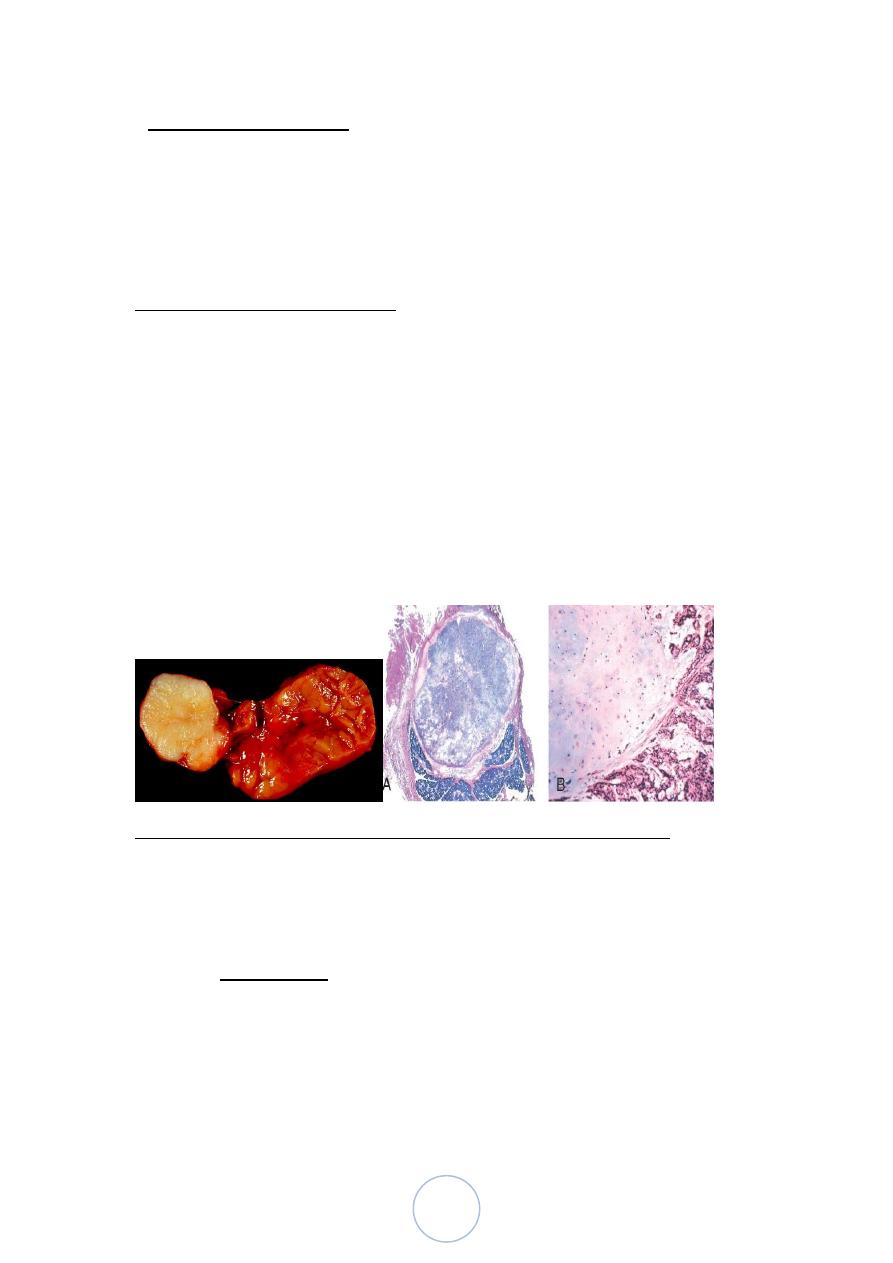
Tumors of the Appendix
The most common tumor of the appendix is the carcinoid
discovered incidentally at the time of surgery or examination of a
resected appendix
At the tip of appendix , a solid bulbous swelling up to 2 to 3 cm in
diameter
39
• Other tumors of Appendix :
Mucocele, a dilated appendix filled with mucin, may simply represent
an obstructed appendix containing inspissated mucin or be a
consequence of mucinous cystadenoma or mucinous
cystadenocarcinoma.
THE PERITONIUM
Inflammatory Disease: could be bacterial infection or chemical irritants
Leakage of bile or pancreatic enzymes
Perforation or rupture of the biliary system
Acute hemorrhagic pancreatitis
Foreign material, including that introduced surgically (e.g., talc
and sutures)
Endometriosis
Perforation of abdominal viscera
PERITONEAL INFECTION
Bacterial peritonitis occurs when bacteria from the gastrointestinal lumen
are released into the abdominal cavity, typically following perforation
acute appendicitis, peptic ulcer, cholecystitis, diverticulitis, and
intestinal ischemia. Acute salpingitis, abdominal trauma, and
peritoneal dialysis are other potential sources of contaminating
bacteria.
Morphology.
• loss of glistening serosal and peritoneal surfaces
• serous or slightly turbid fluid begins to accumulate within 2 to 4
hours of infection.
• As the infection progresses, creamy suppurative material that may
be extremely viscous accumulates.
40
• The cellular inflammatory response is composed primarily of
dense collections of neutrophils and fibrinopurulent debris that
coat the viscera and abdominal wall.
Tumors
Most tumors of the peritoneum are malignant and can be divided
into primary and secondary forms
Primary tumors arising from peritoneal lining are mesotheliomas (are
almost always associated with significant asbestos exposure.)
Secondary tumors of the peritoneum are, in contrast, quite common.
In any form of advanced cancer, direct spread to the serosal surface
or metastatic seeding (peritoneal carcinomatosis) may occur.(ovarian
and pancreatic adenocarcinoma, Appendiceal mucinous carcinomas
are the most common malignant tumor)
