
1
د. مصطفى
امراض
44
\
2
\
2142
( عدد االوراق
6
) م
\
3
\
موصل
lec: 1
Blood vessels
pathology
Mechanisms Of Diseases Due To
Vascular Pathology
• Narrowing or complete obstruction of the lumen
• Weakening of the wall leading to dilation or rupture
Constituents Of The Wall
• Endothelial cells
• Smooth muscle cells
• Extracellular matrix, (elastin, collagen, glycosoaminoglycans)
these constituents form 3 layers:
-Intima
-Media
-Adventitia
Vessels
• Arteries
• Veins
• Lymphatics
Types Of Arteries Based On Their Size And Structure
1. Large or elastic arteries
2. Medium-sized or muscular arteries
3. Small arteries (less than 2mm in diameter)
4. Arterioles
Functions
Elastic arteries: recoil of the wall during diastole, propel blood
through the peripheral vascular system
Muscular arteries and arterioles: regulate regional blood flow
and blood pressure by changes in lumen size, controlled by:
- Autonomic nervous system
- Local metabolic factors and cellular
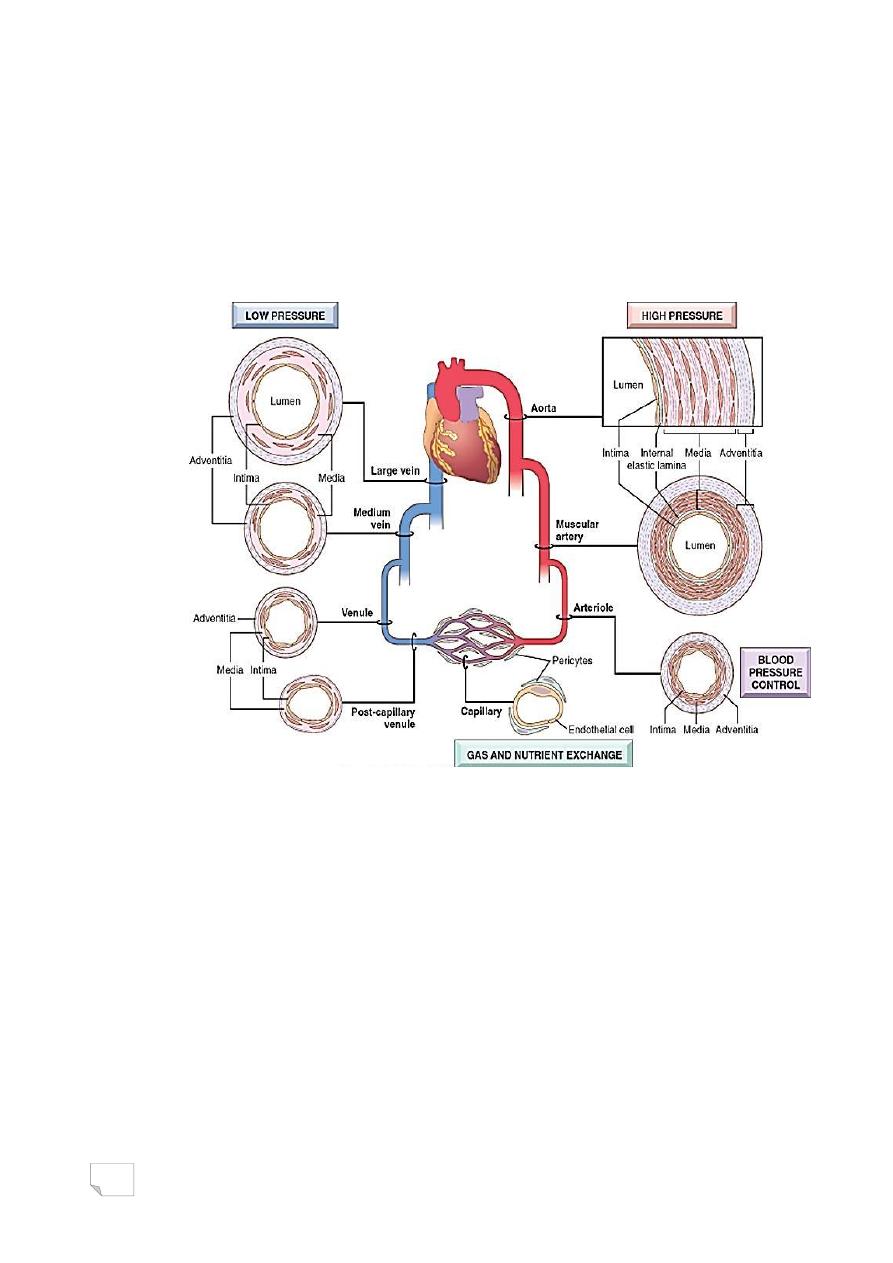
2
interactions
Capillaries: serve exchange of diffusible substances between
blood and tissue
• The venous system: collectively, has a large capacity,
approximately 2/3 of all blood is in veins.
• Lymphatics: serve as drainage system for returning
interstitial tissue fluid and inflammatory cells to the blood
Regional specializations of the vasculature
Congenital Anomalies
.Mostly are important in surgery during
which an unexpected vessel can be
injured.
.The anomalies are rarely symptomatic
except in the coronary tree.
Arterio-Venous Fistulae
Abnormal communications between arteries and veins
*Causes:
-Developmental defects
3
-Produced from
1. Rupture of an arterial aneurysm into adjacent vein
2. Penetrating injuries
3. Inflammatory necrosis of adjacent vessels
*Clinical significance:
-may short circuit blood
-may rupture
Berry Aneurysms
• Saccular congenital of unknown etiology
• Cigarette smoking and hypertension are predisposing factors
• Most frequent at the 5
th
decade
• Slightly more common in females
• They occur where the arterial media is
congenitally attenuated
Clinical features:
.Rupture> subarachnoid hemorrhage,
• Probability of rupture depends on:
• -size of the lesion
• -acute increase in intracranial pressure
acute feature
-generalized vasospasm of non- involved blood
vessels>ischemia
late sequelae
-meningeal fibrosis
Arteriosclerosis
Means: hardening of the arteries
1 - Atherosclerosis.
2 - Monckeberg medial calcific sclerosis.
3 - Arteiolosclerosis:
• Hyaline
• Hyperplastic
Atherosclerosis
• The most common arteries involved in
descending order:
4
-Aorta
-Coronary
-Popliteal
-Internal carotid
-Vessels of circle of willis
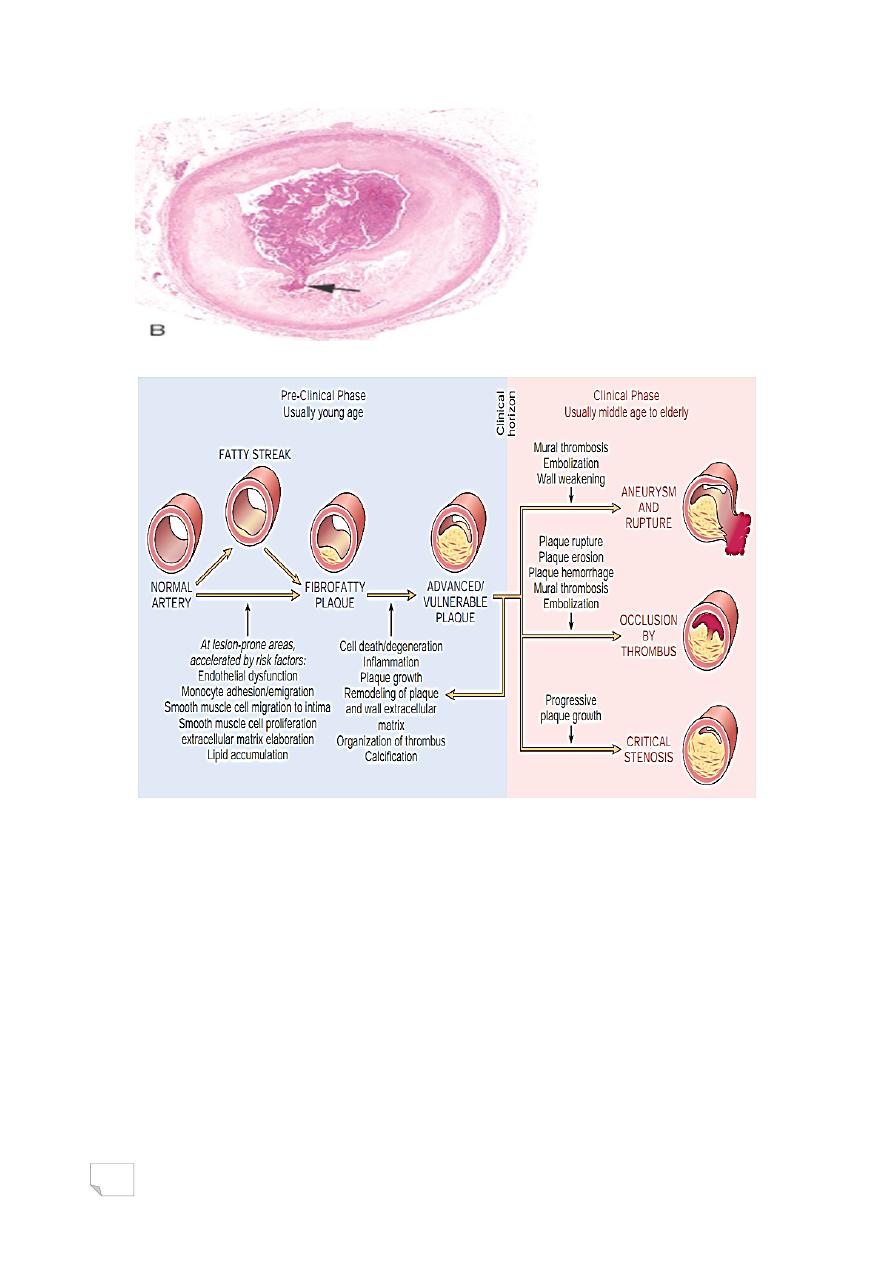
Natural history and main consequences
• The lesion is divided into 6 types:
1- fat dots
2- fatty streak
3- intermediate
4- atheroma
5- fibroatheroma
6- complicated atheroma
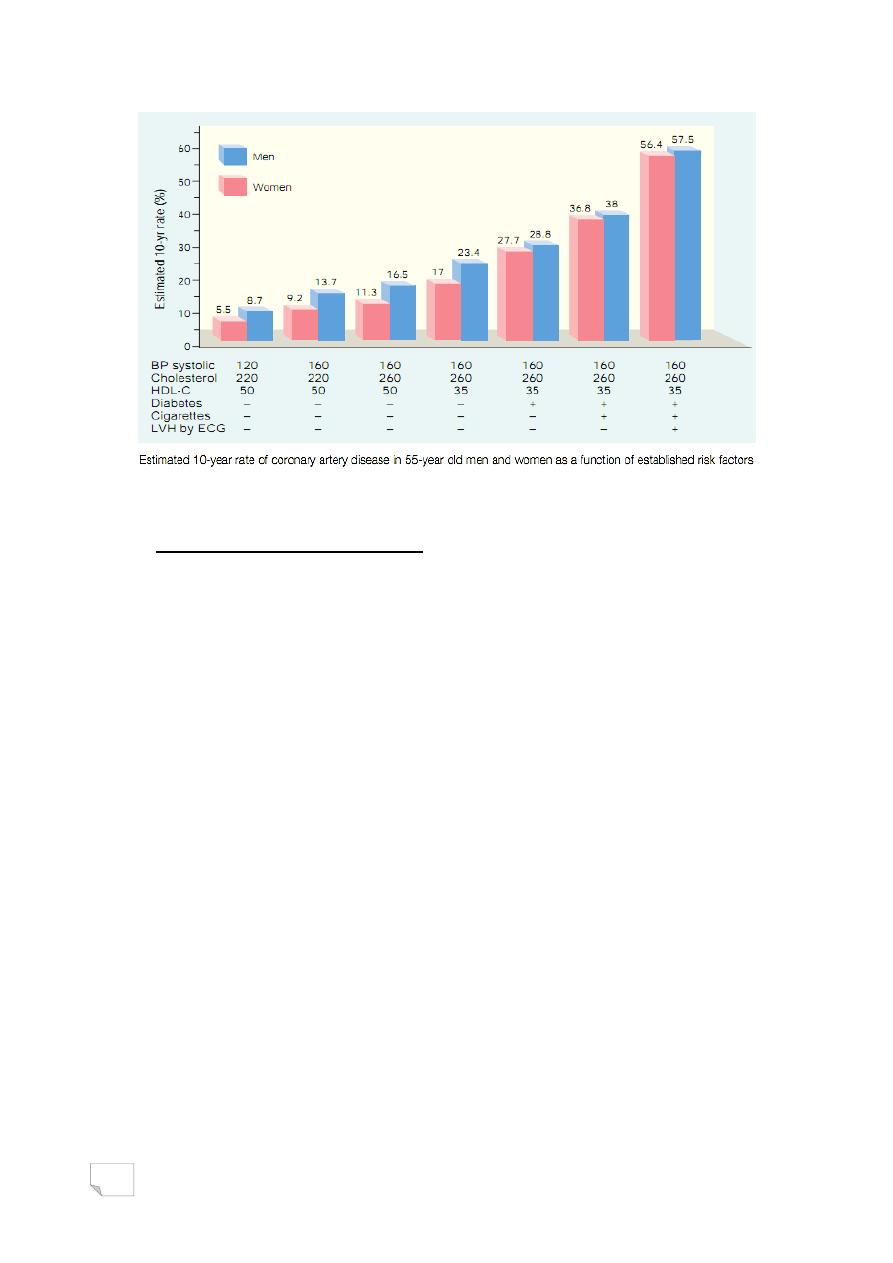
Risk factors including: age, gender( male), obesity smoking, DM, lack of
exercise, hypertension, hyperlipidaemia, type A personality (impatient,
workaholic)
Risk factors
I- Major factors
- Non modifiable
(Constitutional)
(age, gender, genetic)
- Modifiable
- Hyperlipidemia
- Hypertension
- Smoking
- Diabetes mellitus
- Inflammation

5
II- Other minor factors
.lack of exercise
.stressful life
.obesity
.hyperhomocystinemia
.lipoprotein a
Hyperlipidemia
• Specifically hypercholesterolemia; even in the absence of other
risk factors, it is sufficient to initiate lesion development.
• The major component of serum cholesterol associated with
increased risk is low-density lipoprotein (LDL) cholesterol
(―bad cholesterol‖).
• In contrast, high-density lipoprotein (HDL) is the complex that
mobilizes cholesterol from the periphery (including atheromas)
and transports it to the liver for excretion Consequently,
higher levels of HDL (―good cholesterol‖) correlate with
reduced risk.
Hypertension
Hypertension increase the risk of IHD by approximately 60% versus
normotensive populations.
• Cigarette smoking
.one or more packs per day for several
years increases the death rate from IHD by up to 200%
Diabetes mellitus
.Induces hypercholesterolemia
.Other factors being equal, DM cause:
- 2 folds increases incidence of MI
- increases incidence of stroke
- 100 fold increases the risk of gangrene
at the lower extremities
6
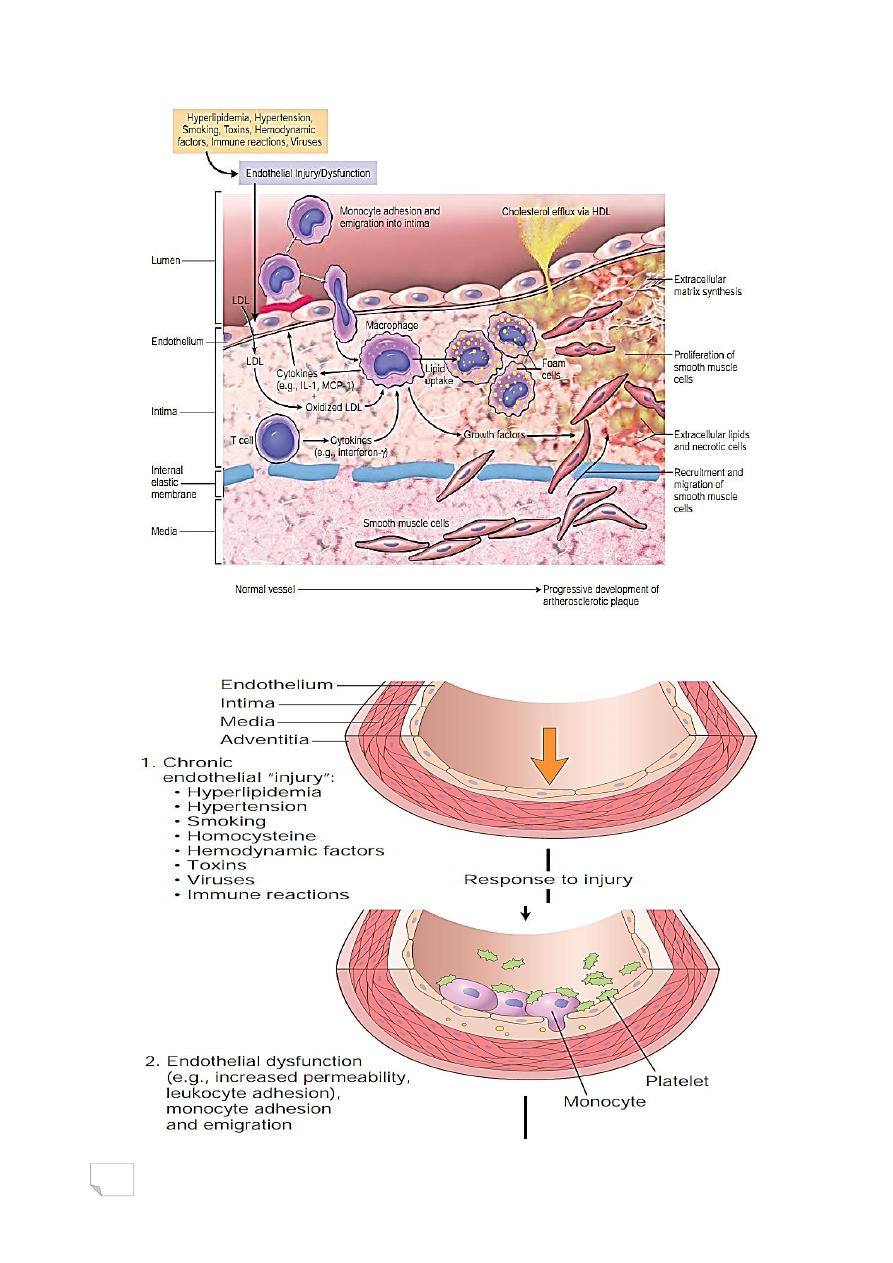
Pathogenesis
I- Response to injury hypothesis
• Endothelial injury and dysfunction: causing increased vascular
permeability, leukocyte adhesion, and thrombosis
• Accumulation of lipoproteins (mainly LDL and its oxidized forms) in
the vessel wall
• Monocyte adhesion to the endothelium, followed by migration into
the intima and transformation into macrophages and foam cells
• Platelet adhesion
• Factor release from activated platelets, macrophages, and vascular
wall cells, inducing smooth muscle cell recruitment, either from the
media or from circulating precursors
• Smooth muscle cell proliferation, extracellular matrix production,
and recruitment of T cells.
• Lipid accumulation both extracellularly and within cells
(macrophages and smooth muscle cell)
7
Sequence of cellular interactions in atherosclerosis
Evolution of arterial wall changes in response to injury hypothesis
8
II- Other hypotheses:
-Oligoclonality of lesion
-Infection
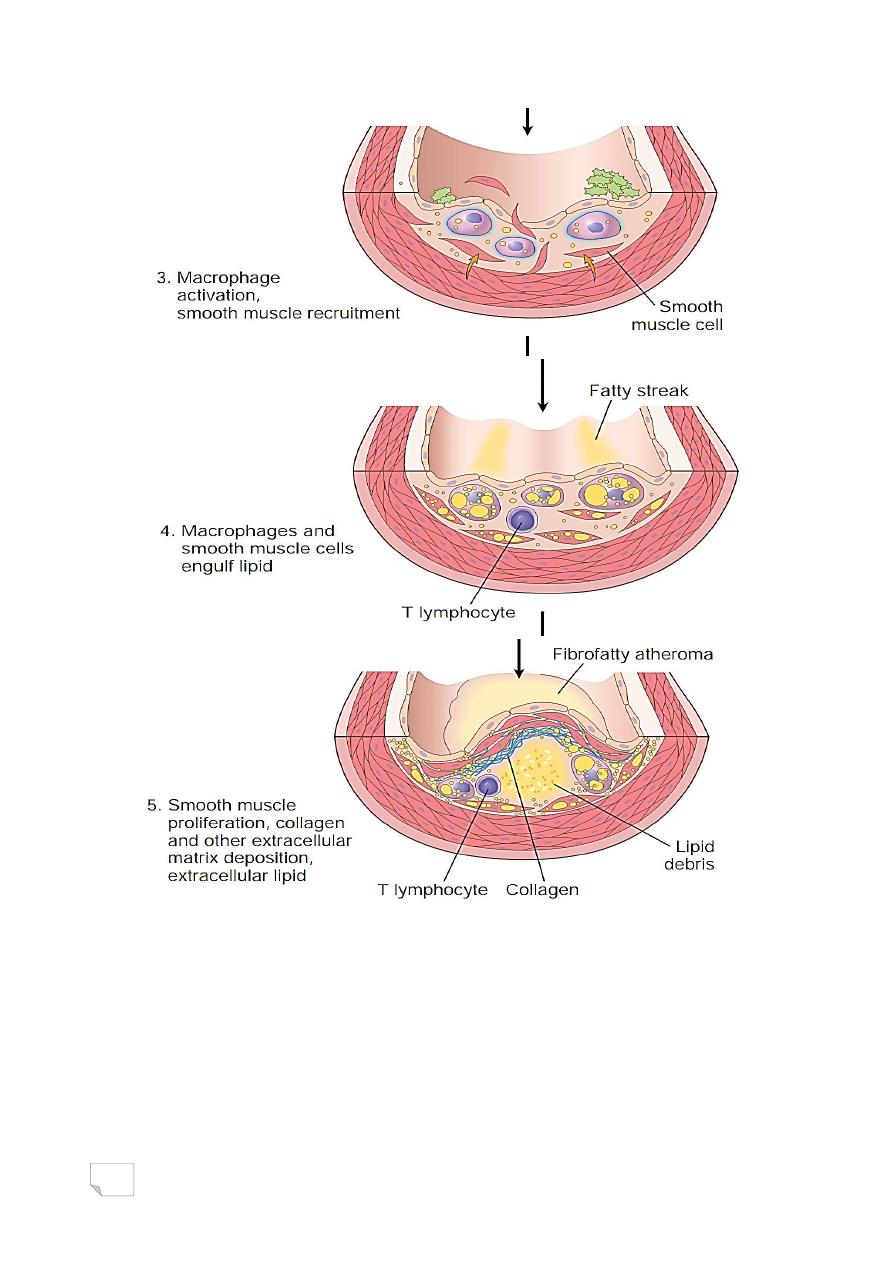
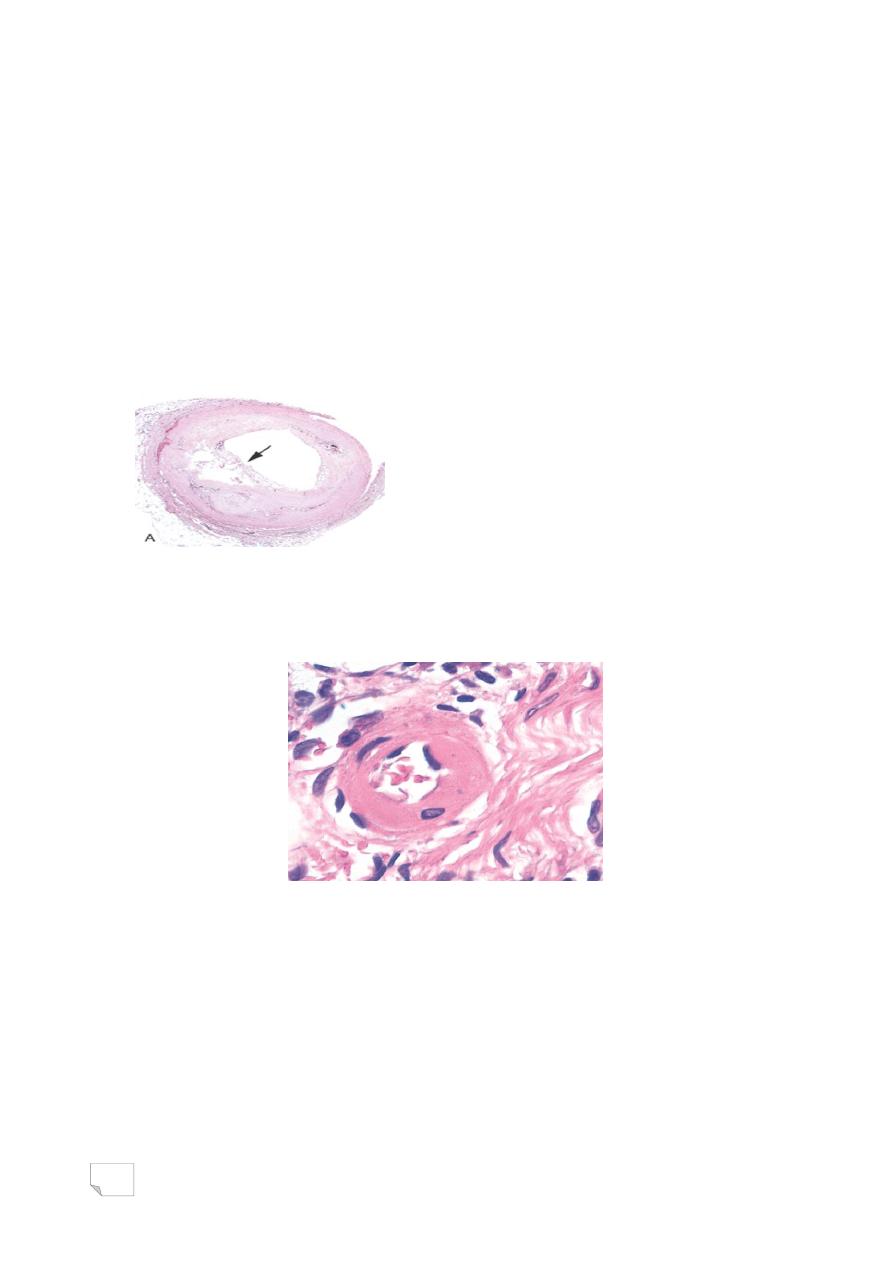
Morphology:
Raised focal lesion within the intima with soft yellow core of
lipid (mainly cholesterol and cholesterol esters), covered by firm
fibrous cap.
9
Size range is 0.3-several centimeters, at first patchy in which
later on becomes more numerous and diffuse
Components:
Cells: (smooth muscle, macrophages
and other leukocytes)
Extracellular matrix, (collagen, elastic fibers and proteoglycans)
Lipid
The key components of atheromatous plaque.
Aorta; Fat streaks
Aorta, mild atherosclerosis
10
Aorta ; severe atherosclerosis
Coronary artery, atheromatous plaque
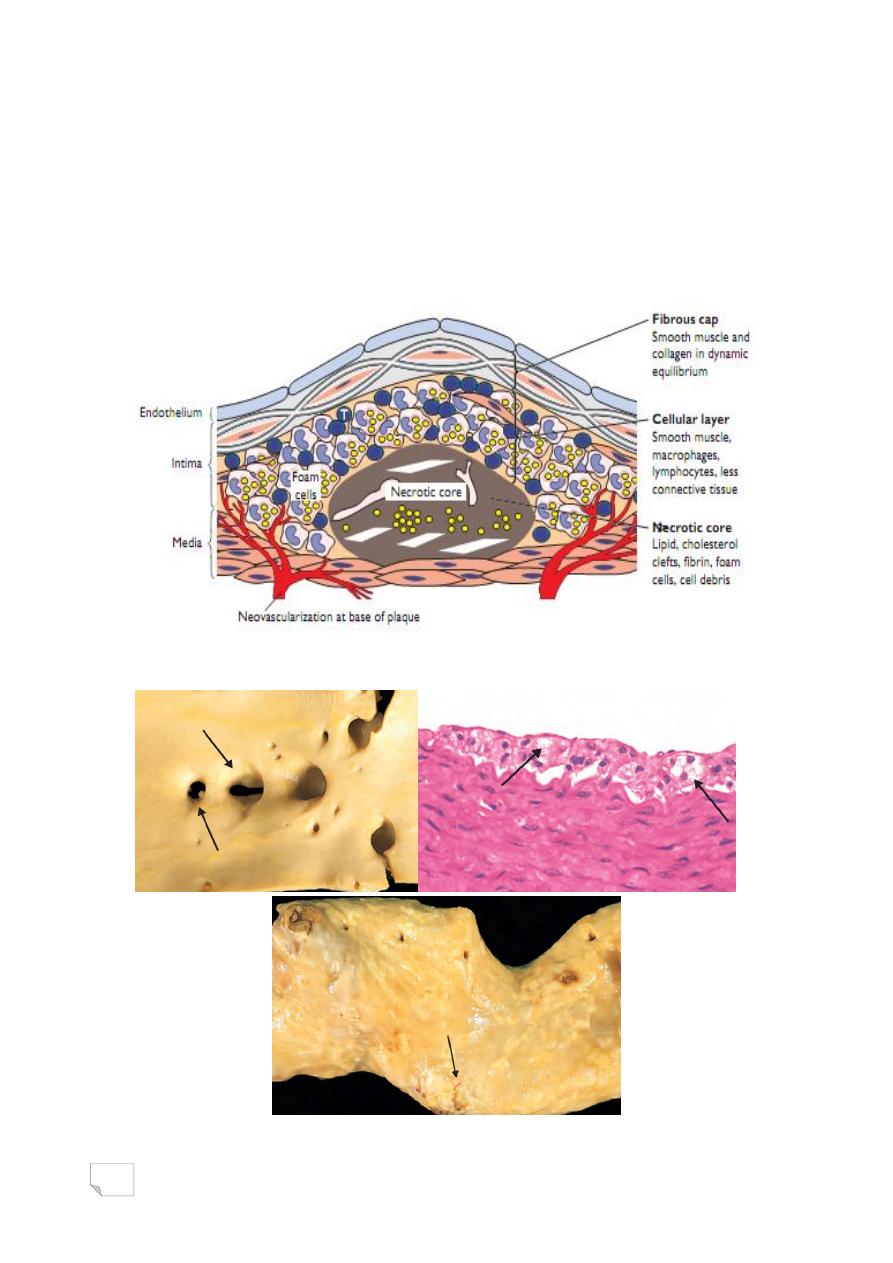
• Complications:
1. Rupture, ulceration, and erosion of the surface> thrombosis
2. Hemorrhage in to plaque.
3. Thrombosis
4. Atheroembolism
5. Aneurysm
Coronary artery, plaque rupture
11
Coronary artery, thrombus overlying complicated atheroma
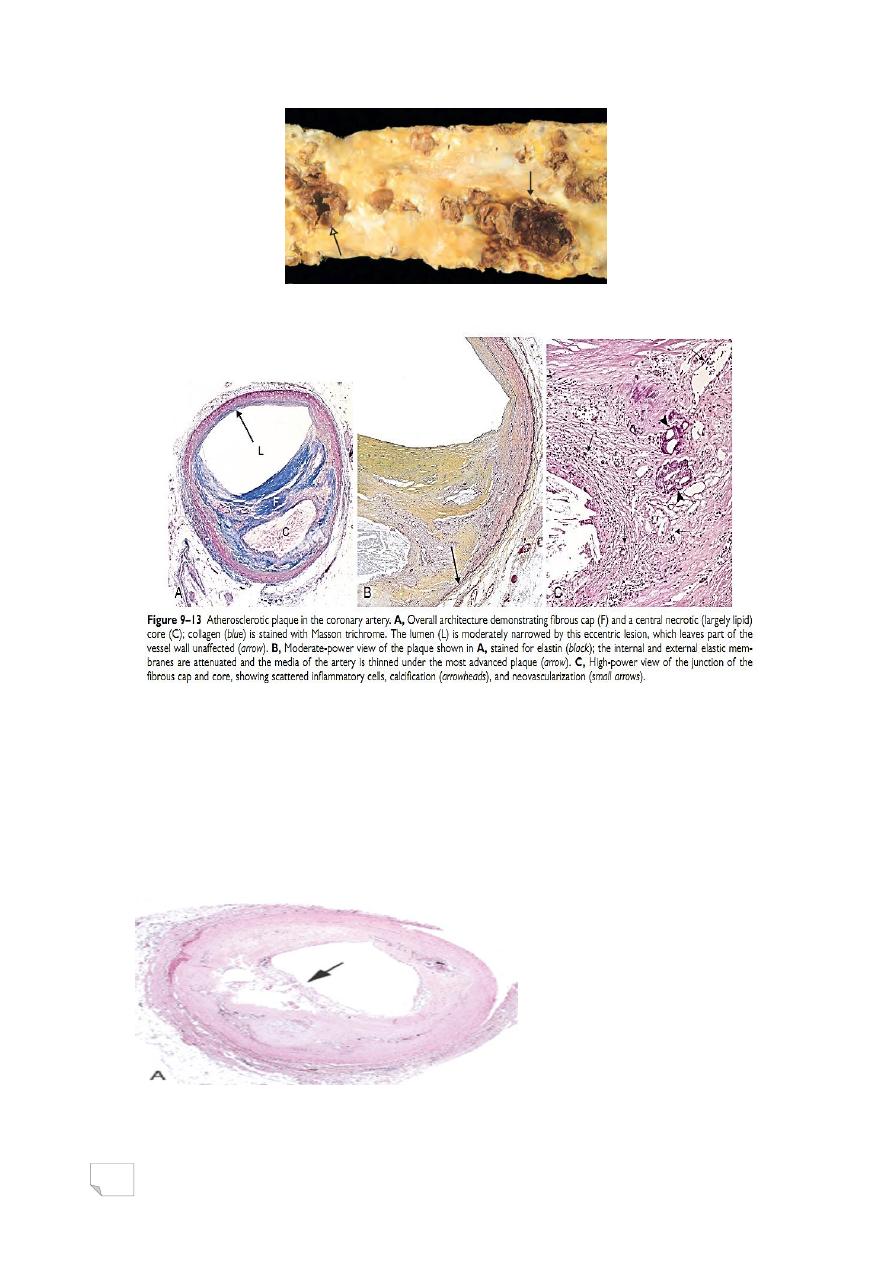
Atherosclerosis, natural history, morphology, pathogentic events,
complications
12
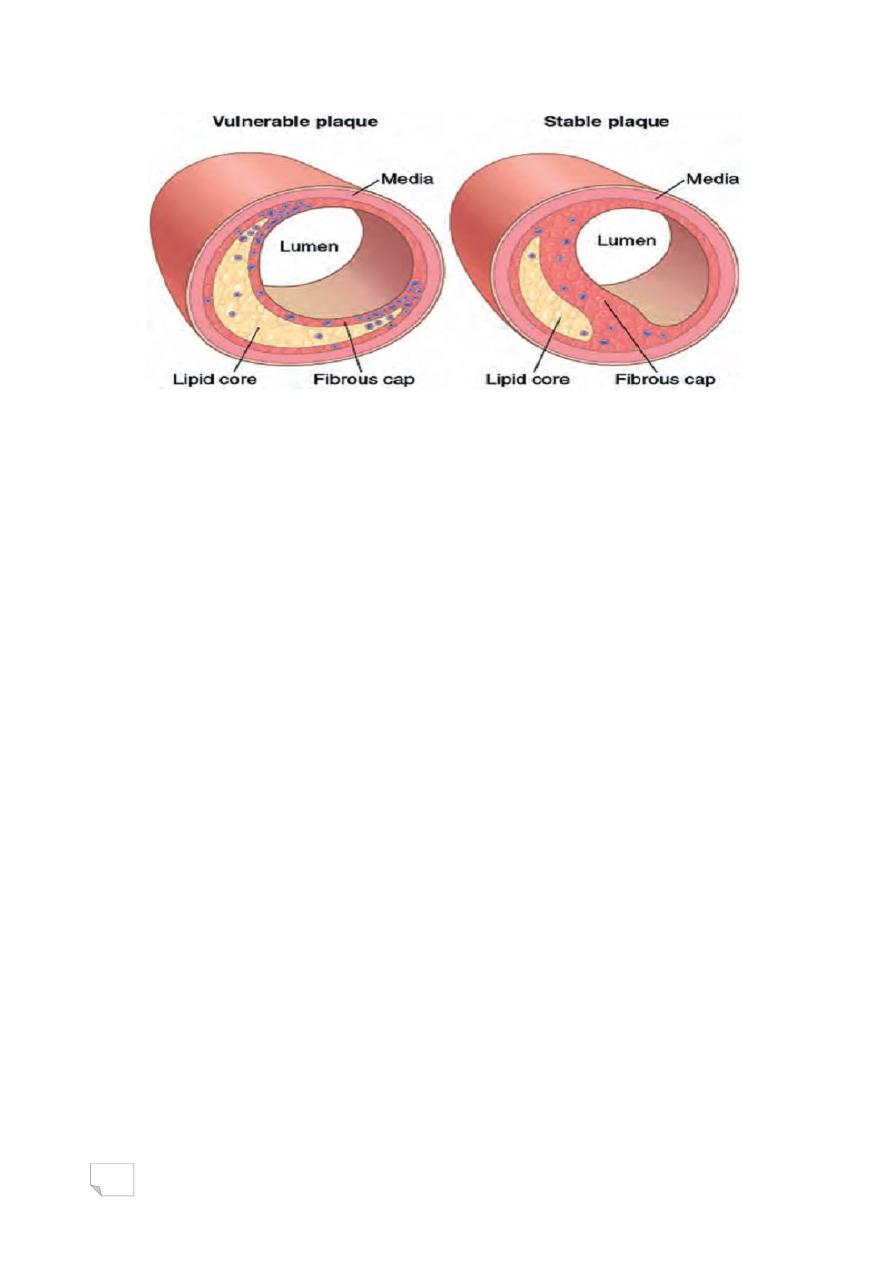
• Vulnerable plaques have thin fibrous caps, large lipid cores,
and greater inflammation.
• Stable plaques have thickened and densely collagenous fibrous
caps with minimal inflammation and underlying atheromatous
core.
Major consequences of atherosclerosis
• Myocardial infarction (heart attack)
• Cerebral infarction (stroke)
• Aortic aneurysms
• Peripheral vascular disease (gangrene of the legs)
• Bowel ischaemia

13
د. مصطفى
امراض
45
\
2
\
2142
( عدد االوراق
6
) م
\
3
\
موصل
lec:2
Blood vessels pathology
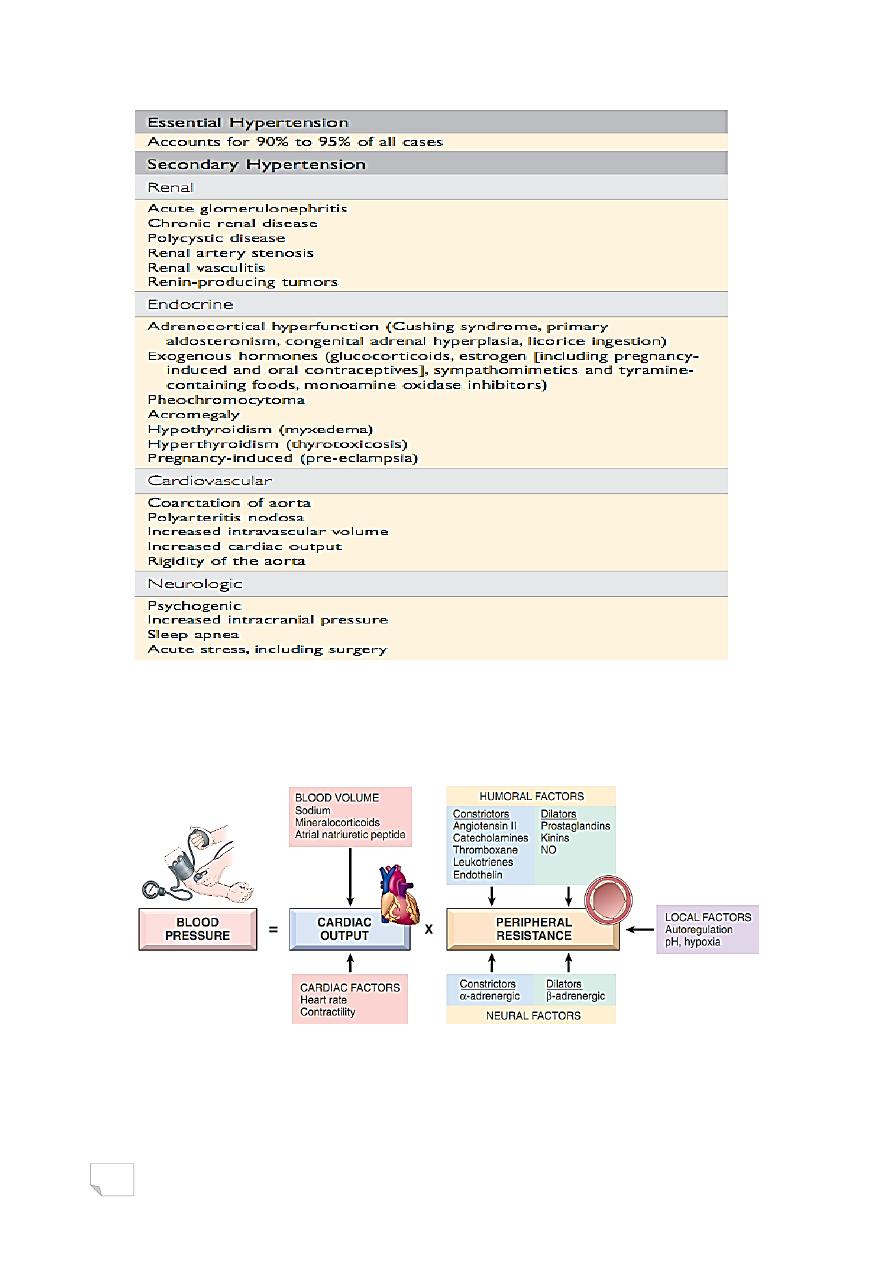
Hypertensive vascular disease
• Multifactorial disorder, (genetic &
environmental)
• Defined as: sustained elevation of blood pressure above 140/90
mmHg
.Types:
-Essential (idiopathic) 95%
-Secondary 5% to
.renal disease
.endocrine abnormality
.cardiovascular disorder
.neurogenic cause
Types & causes of hypertension
14
Regulation of normal blood pressure
Blood pressure is controlled by:
1. Cardiac output
2. Peripheral vascular resistance
BP regulation
1. Cardiac output is dependent on blood volume, itself is greatly
influenced by sodium homeostasis
2. Peripheral vascular resistance is
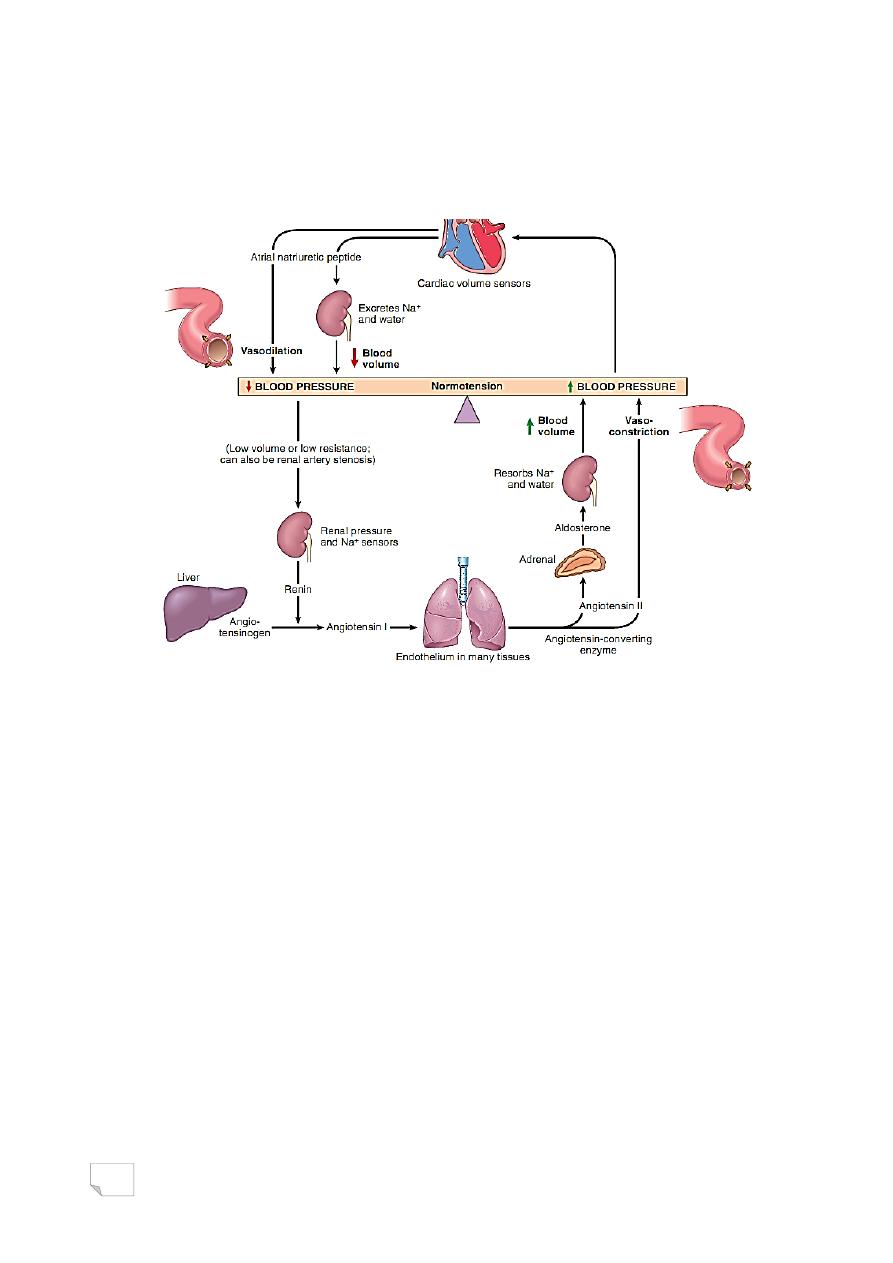
15
determined at the arteriolar level and is affected by neural and
humoral factors
-vasoconstricting agents
-vasodilating agents
Interplay of renin, angiotensin, aldosterone, and atrial natriuretic peptide
in blood pressure regulation
• Major factors determining blood
pressure variation
-age
-gender
-body mass index
-diet principally sodium intake
.other factors include
-auto-regulation
-local factors (pH, hypoxia)
-alpha and beta adrenergic systems
*Clinically
16
-Benign in 95% of cases
-Malignant affecting 5% of patients ( 200/120 mmHg)
(associated with renal failure and retinal hemorrhages, +/-
papilledema.)
*Morphology
-Atherosclerosis
-Hyaline arteriolosclerosis
-Hyperplastic arteriolosclerosis
• Hypertension accelerates atherogenesis
• Causes degenerative changes in the walls, can lead to aortic
dissection and cerebrovascular hemorrhage.
Associated with benign hypertension. It is marked by homogeneous,
pink hyaline thickening of the arteriolar walls, and luminal narrowing
caused by leakage of plasma components across injured endothelial cells
17
Typical of severe hypertension. “onionskin,” concentric, laminated
thickening of arteriolar walls and luminal narrowing . The laminations
consist of smooth muscle cells and thickened, reduplicated basement
membrane.
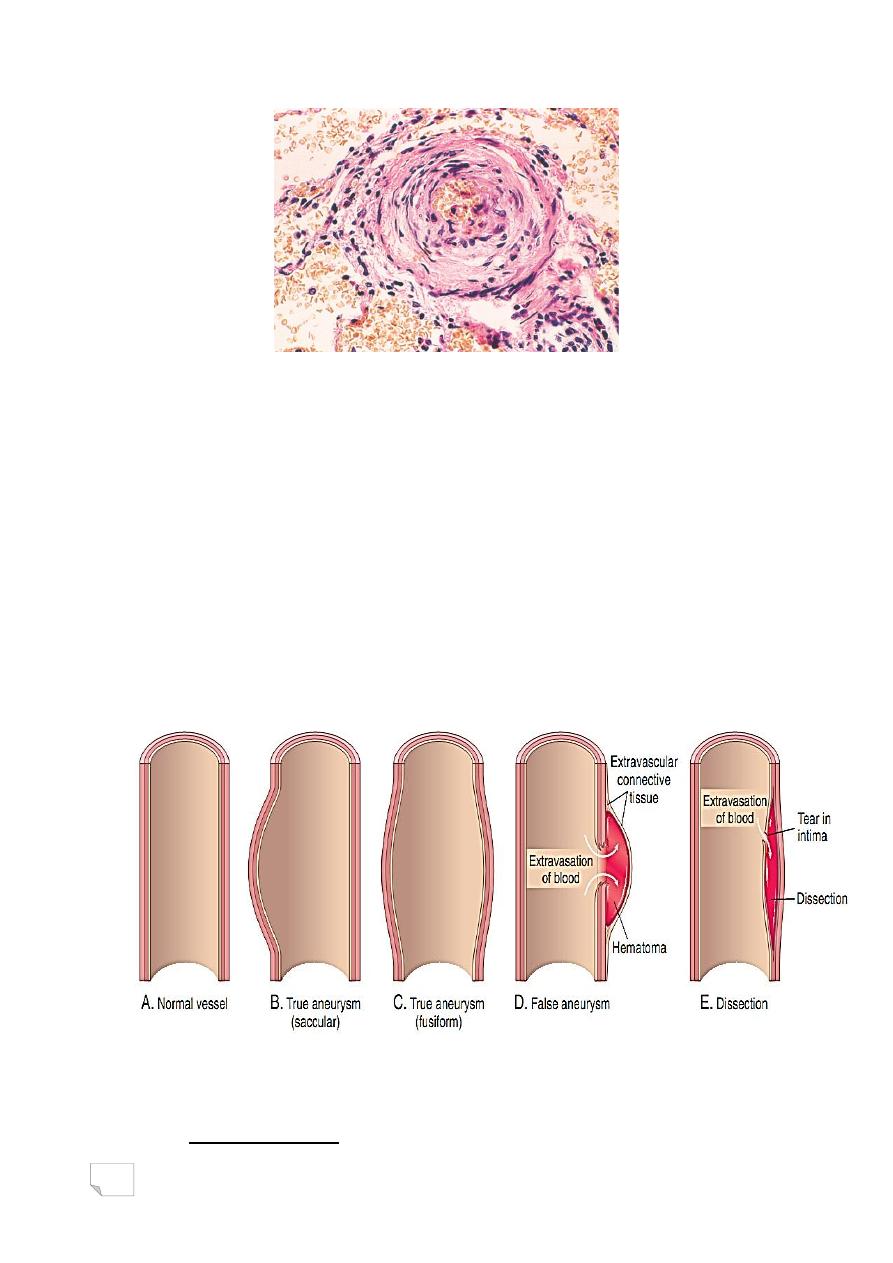
Aneurysm
• Localized abnormal dilation (saccular
or fusiform) of blood vessels or the wall
of the heart.
• Classified into:
-True
-False
Aneurysms
• Causes of aneurysm:
- Atherosclerosis

18
•
Most important
- Hypertension
- Congenital
- Trauma
- Infection …syphilis
- Inflammation
Pathogenesis of aneurysm:
• Inadequate or abnormal connective tissue synthesis:
– Marfan syndrome: defective synthesis of the scaffolding
protein Fibrillin
– Ehlers-Danlos syndrome: Defective type III collagen
synthesis
• Excessive connective tissue degradation: such as by
macrophages in atherosclerotic plaque.
• Loss of smooth muscle cells or change in the smooth muscle cell
synthetic phenotype: Atherosclerotic thickening of the intima
can cause ischemia of the inner media
Abdominal Aortic Aneurysm (AAA)
• Rare <50 yrs
• > in males
• Positioned between renal arteries
origin and bifurcation of aorta
• Either saccular or fusiform
• Up to 15cm in diameter and 25cm in length
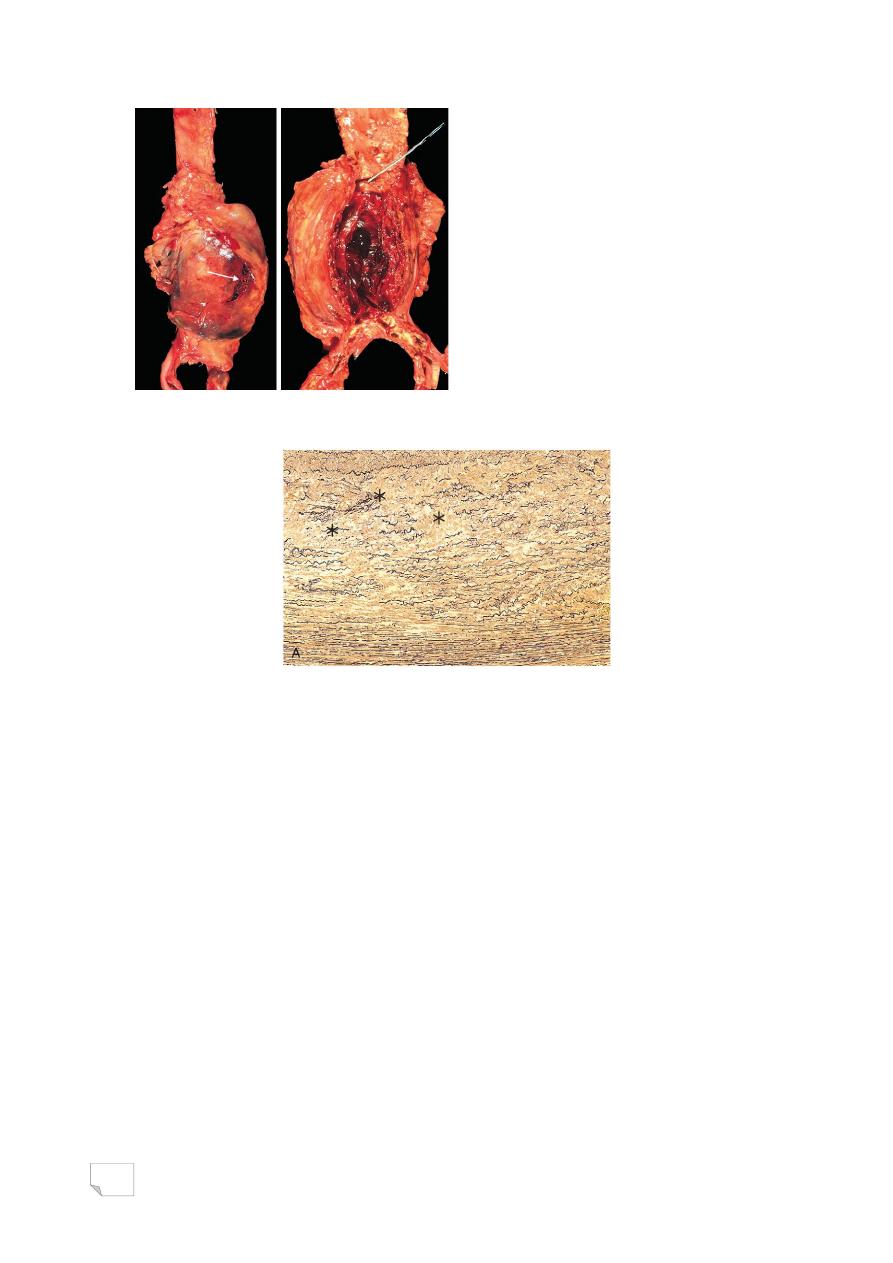
19
Abdominal aortic aneurysm
Aorta, cystic medial degeneration with loss of elastin
* Clinical course:
. Rupture (related to size)
. Obstruction of blood vessels
. Embolism
. Pressure on adjacent structures
. Abdominal mass
Syphilitic Aneurysm
Involvement of the aortic annulus> aortic valve incompetence and
subsequent left ventricular hypertrophy.
* Pathogenesis :
-obliterative endarteritis of vaso vasoreum >patchy loss of medial
elastic fibers and muscle cells>inflammation and scarring
>weakening of wall> aneurysm formation
* Symptoms are due to
-Pressure on mediastinal structures
-Heart failure
20
-Rupture
Aortic Dissection
.Catastrophic illness characterized by
- Dissection of blood between and along the laminar planes of the
media
- Formation of a blood filled channel within the aortic wall which
often ruptures either outward or into the lumen with second distal tear(
double barrel)
• Affects 2 groups of patients:
- Hypertensive men of 40-60yrs.
- Young people with systemic or localized abnormality of connective
tissue
* Morphology
. Transverse or oblique intimal tear within 10cm of aortic valve 1-5cm
in length
. Dissection extends proximally and distally
. The hematoma is between the middle and outer thirds of the wall
* Histology: cystic medial degeneration
• Aortic dissection
• Aortic dissection
21
Pathogenesis of aortic dissection
I.
Hypertension is the major risk factor for aortic dissection,
resulting in medial hypertrophy of the vasa vasorum
associated with degenerative changes in ECM and variable loss
of medial smooth muscle cells
II.
Connective tissue disorders: produce abnormal aortic ECM,
including Marfan syndrome, & Ehlers-Danlos syndrome type
IV
III.
The trigger for intimal tear and intramural aortic hemorrhage
is unknown in most cases
* Clinical course
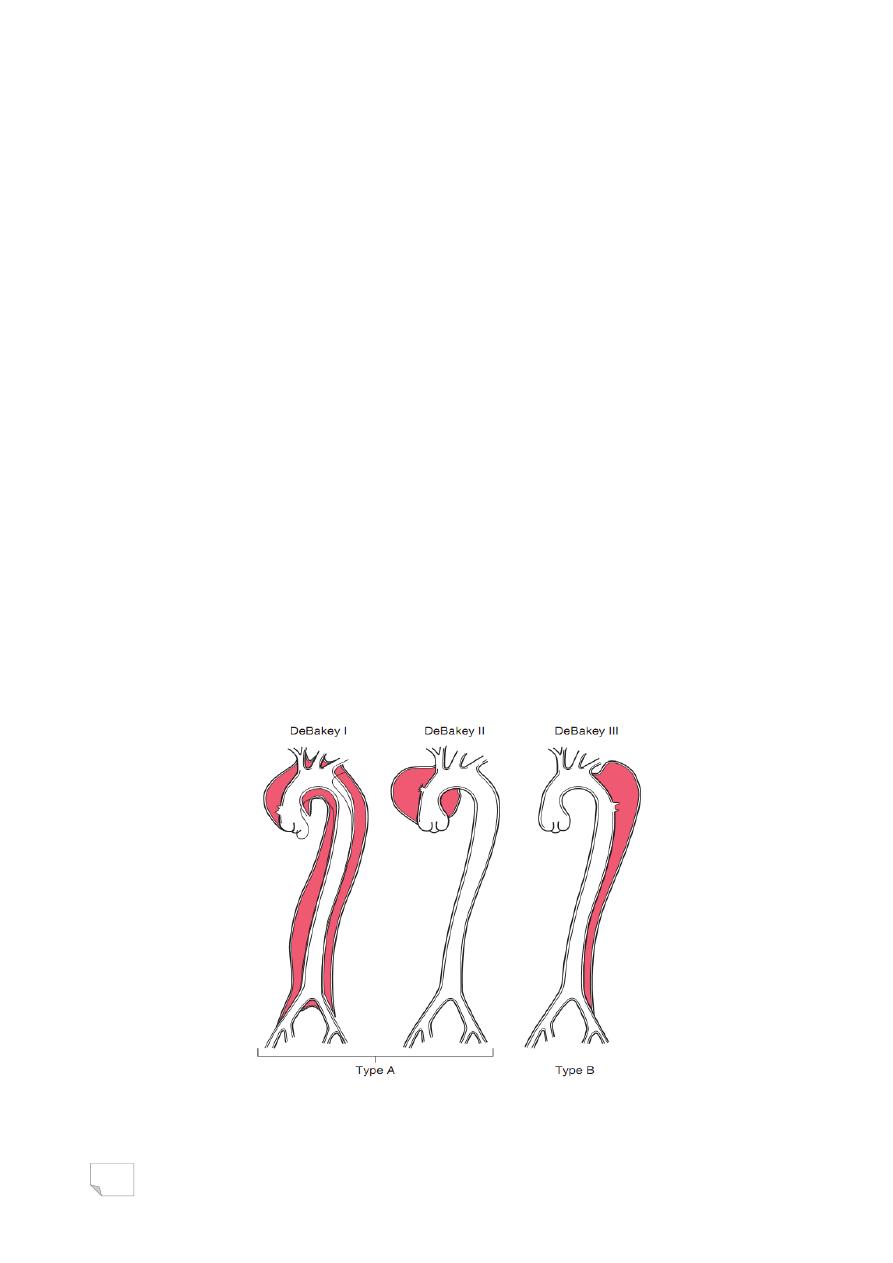
1. Type A (proximal), involving either the ascending portion only
or both the ascending and the descending aorta
2. Type B (distal), starts distal to the subclavian artery origin
- patient suffers from sudden chest pain
radiating to the back and downward
- common cause of death is rupture to:
(pericardium, pleura, peritoneum)
• Aortic dissection, classification

22
VASCULITIS
Vasculitis : vessel wall inflammation.
Pleural: VASCULITIDES
• Clincal features:
• Are protean & largely depend on the vascular bed affected
(e.g., CNS vs. heart vs. small bowel).
• Constitutional symptoms such as fever, myalgias &
arthralgias.
VASCULITIS
* Causes & pathogenesis
I- Direct microbiological infection:
eg. Pseudomonas , Aspergillus & Mucor
II - Immune-mediated:
1) Immune complex deposition
2) Antineutrophil cytoplasmic antibodies
3) Antiendothelial cell antibodies
4) Autoreactive T cells
III-Others (Physical and chemical injury, including radiation,
mechanical trauma, and toxins)
Immune Complex-Associated Vasculitis
Autoantibody production and formation of immune complexes that
deposit in vessels, eg.
1. SLE
2. Drug hypersensitivity vasculitis ( penicillin)
3. Vasculitis secondary to infections ( hepatitis B).
Anti-Neutrophil Cytoplasmic Antibodies
• Circulating autoantibodies that react with neutrophil
cytoplasmic antigens ( mainly enzymes), also called pauci
immune.
• ANCAs are very useful diagnostic markers; their titers
generally mirror clinical severity, and a rise in titers after
periods of quiescence is predictive of disease recurrence.
• Types:
23
1. Antiproteinase-3 (PR3-ANCA), previously called c-ANCA. Eg.
Wegener granulomatosis
2. Anti-myeloperoxidase (MPO-ANCA), previously called p-
ANCA. Eg. microscopic polyangiitis and Churg-Strauss
syndrome.
Anti-Endothelial Cell Antibodies.
Antibodies to endothelial cells, eg. Kawasaki disease
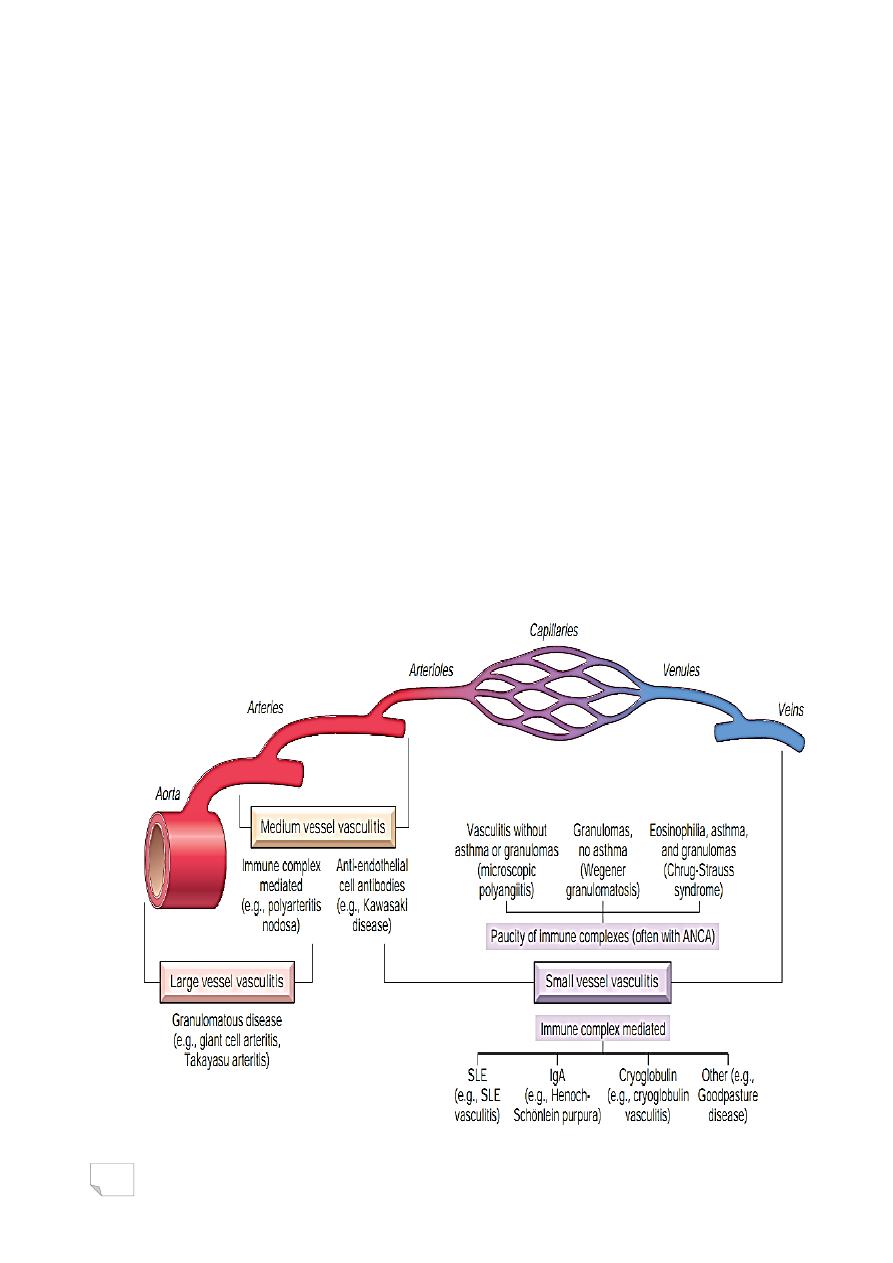
Classification
• Some 20 primary forms of vasculitides are recognized
• The classification schemes attempt to group them according to:
1. Vessel diameter ( size),
2. Role of immune complexes,
3. Presence of specific autoantibodies,
4. Histology & Granuloma formation,
5. Organ specificity,
6. Even population demographics
Vasculitis, types-sites relation

24
د. مصطفى امراض
42
\
2
\
2142
( عدد االوراق
5
) م
\
3
\
موصل
lec: 3
Blood vessels
pathology
Giant Cell Arteritis
.The most common form of vasculitis in elderly ( > 50yrs).
. Chronic, typically granulomatous inflammation of large to small
size arteries
.Most common arteries involved are:
(temporal, vertebral, ophthalmic, aorta ”giant cell aortitis”)
• Pathogenesis:
- T cell mediated immune response to an as-yet uncharacterized
vessel wall antigen that drive subsequent Pro-inflammatory cytokines
release (especially TNF)
- Anti-endothelial cell antibodies & anti-smooth muscle ab found
in 2/3 of cases.
* Clinical features
• Temporal artery: headache & pain in artery course
• Ophthalmic artery: diplopia , loss of vision
Temporal artery, giant cell arteritis
• Morphology:
segemental involvement of vessel
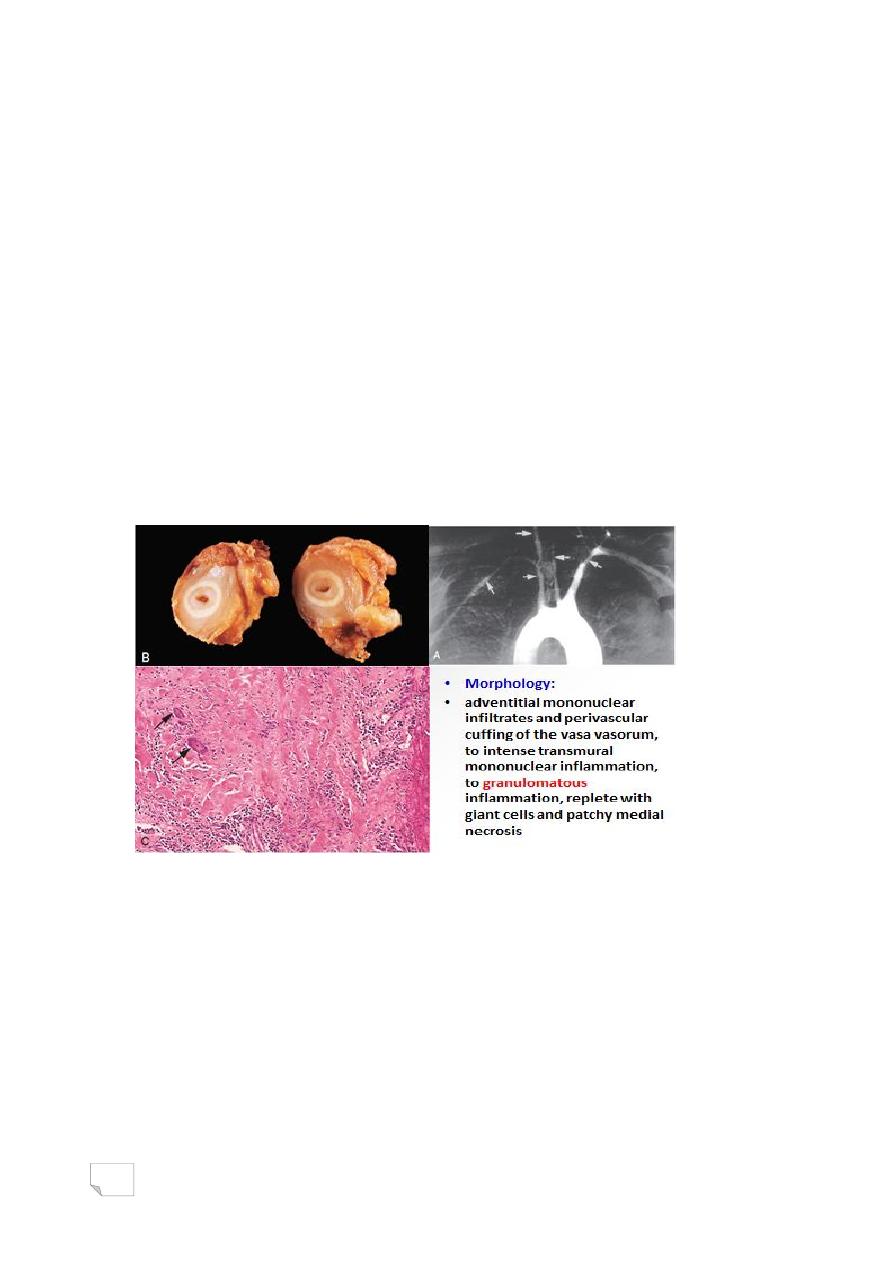
25
• Giant cells arteritis:
• Granulomatous inflammation within the inner media with
multinucleate giant cells
• Fragmentation of the internal elastic laminas
Takayasu arteritis
• Granulomatous vasculitis of medium-sized and larger arteries
• Classically affects the aortic arch and arch vessels & pulmonary
arteries are involved in 50% of patients
• Age < 50 yrs
• Characterized by:
- Ocular disturbances
- Marked weakening of the pulses in the upper
extremities (pulseless disease)
• Takayasu aortitis shares many attributes with giant cell
aortitis, including clinical features and histology.
• Indeed, the distinction is typically made based on the age of the
patient:
- Older than 50, it is giant cell aortitis
- Younger than 50, it is Takayasu aortitis
26
Polyarteritis nodosa
• Systemic vasculitis of small or medium-sized muscular arteries
• Typically involves the renal and visceral vessels
• A ―classic‖ presentation:
• Hypertension due to renal artery involvement
• Abdominal pain and bloody stools caused by vascular
gastrointestinal lesions
• Spares the pulmonary circulation.
• There is no association with ANCAs
• 1/3 of cases have chronic hepatitis B infection
• PAN: segmental transmural fibrinoid necrosis of small artery
Kawasaki disease
• Acute, febrile, usually self-limited illness of infancy and
childhood (80% < 4 years)
• Mainly involve large to medium-sized vessels.
• Coronary arteritis cause aneurysms that rupture or
thrombose, resulting in myocardial infarction ( MI ! in
children).
• Also called mucocutaneous lymph node syndrome
• Muco: conjunctival and oral erythema and blistering
• Cutaneous: desquamative rash
• LN: cervical lymph node enlargement
27
Granulomatosis with Polyangiitis (Wegener Granulomatosis)
• Systemic disease characterized by:
-Acute necrotizing granulomas of upper and/or lower respiratory
tract
-Necrotizing granulomatous vasculitis of small and medium-sized
vessels
-Glomerulonephritis
• > males , Peak at 5th decade
• Due to:
• T-cell–mediated hypersensitivity response to inhaled microbial
or other environmental agents
• PR3-ANCAs : 95% of cases
• Clinically:
- Pneumonitis
- Chronic sinusitis
- Renal disease
• Morphology:
• Granulomas with geographic patterns of central necrosis and
accompanying vasculitis
• Multiple granulomas can coalesce to produce radiographically
visible nodules that can also cavitate
• Focal and segmental glomerulonephritis & crescentic
glomerulonephritis
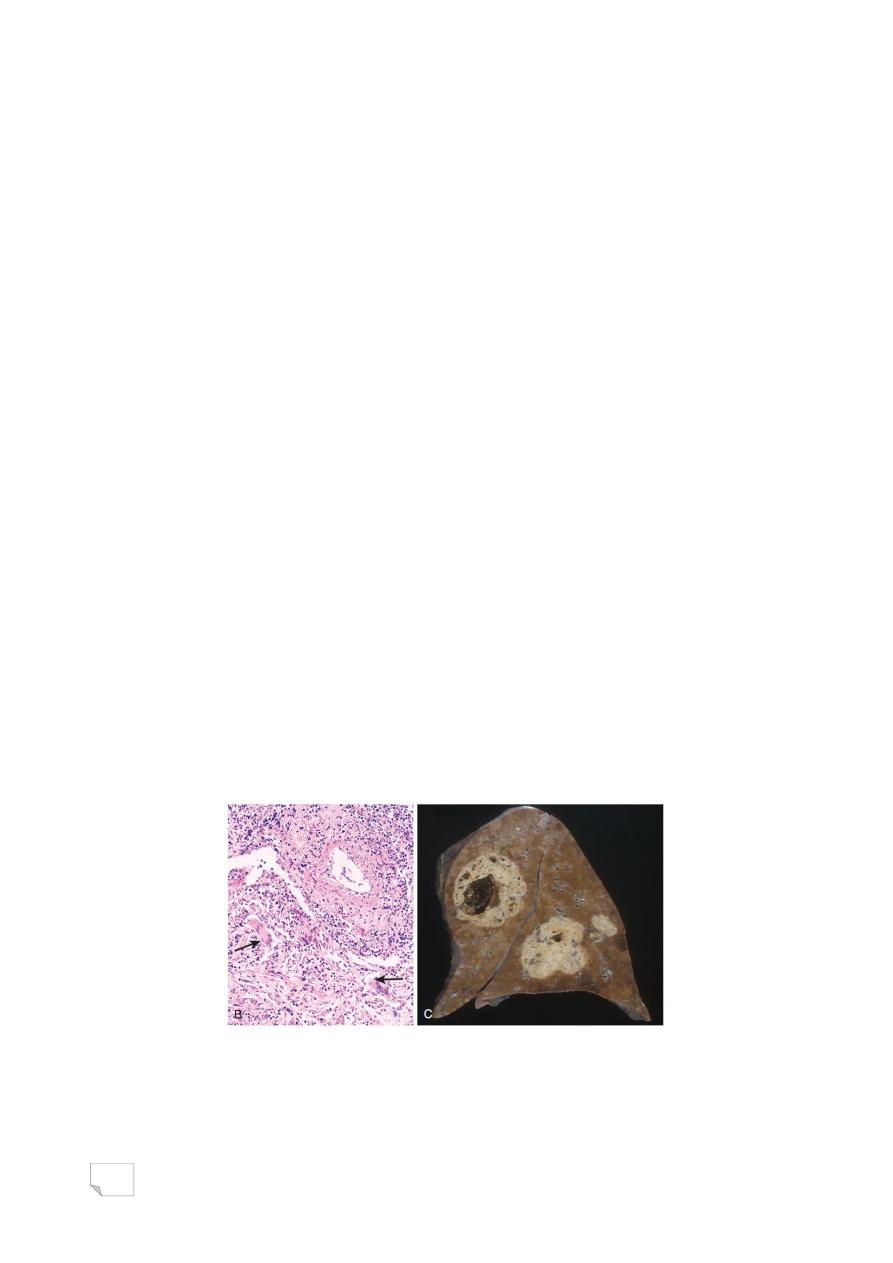
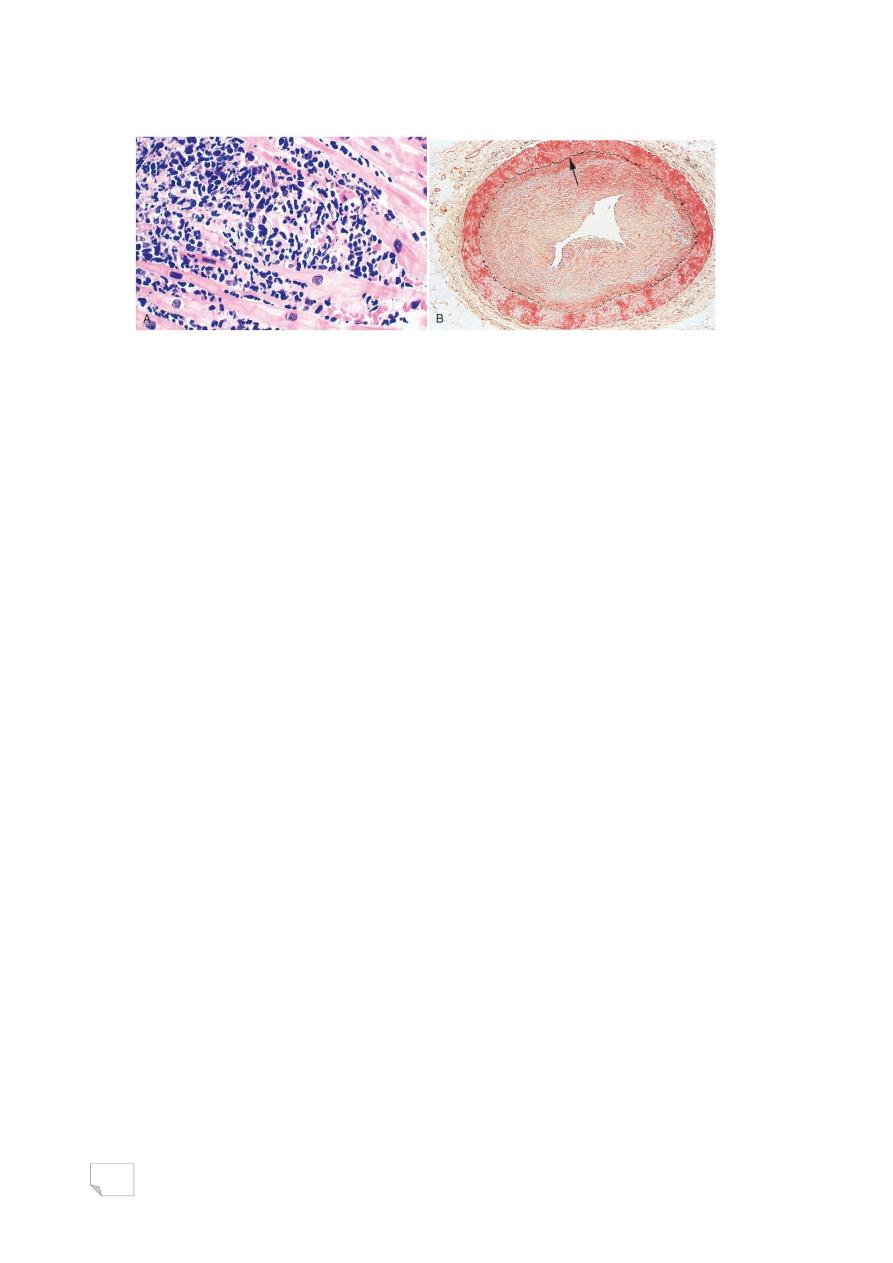
• Wegener granulomatosis. Vasculitis of a small artery with
adjacent granulomatous inflammation including giant cells
(arrows).
• Lung demonstrating large nodular cavitating lesions.
28
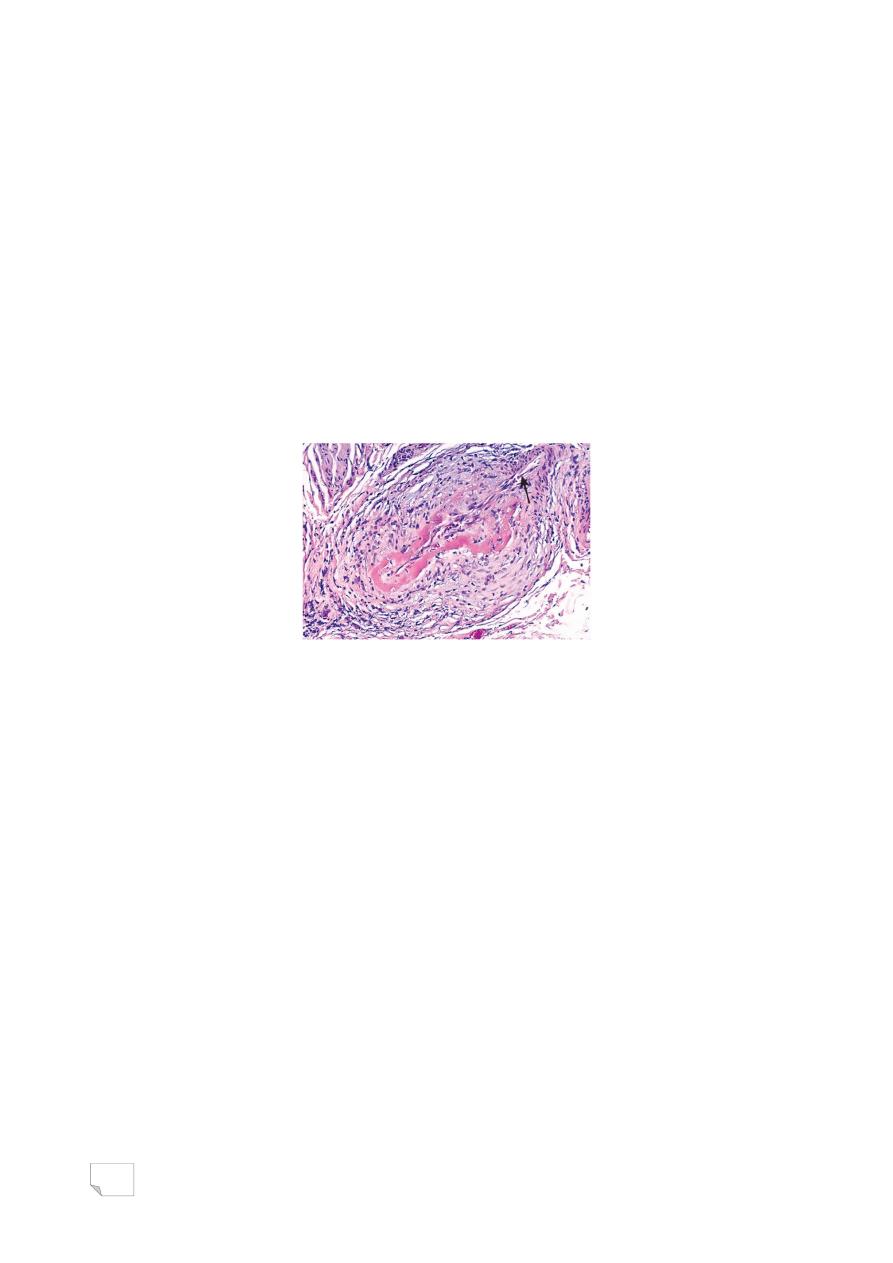
Thrombo Angiitis Obliterans
(Buerger Disease)
• Focal acute and chronic inflammation of medium-sized and
small arteries ( especially tibial and radial arteries)
• Associated with thrombosis & frequently results in severe
vascular insufficiency and gangrene of the extremities
• Occasionally, secondary extension into adjacent veins and
nerves
• usually < 35 yrs.
• Occurs almost exclusively in heavy tobacco smokers :
- direct toxicity
- hypersensitivity
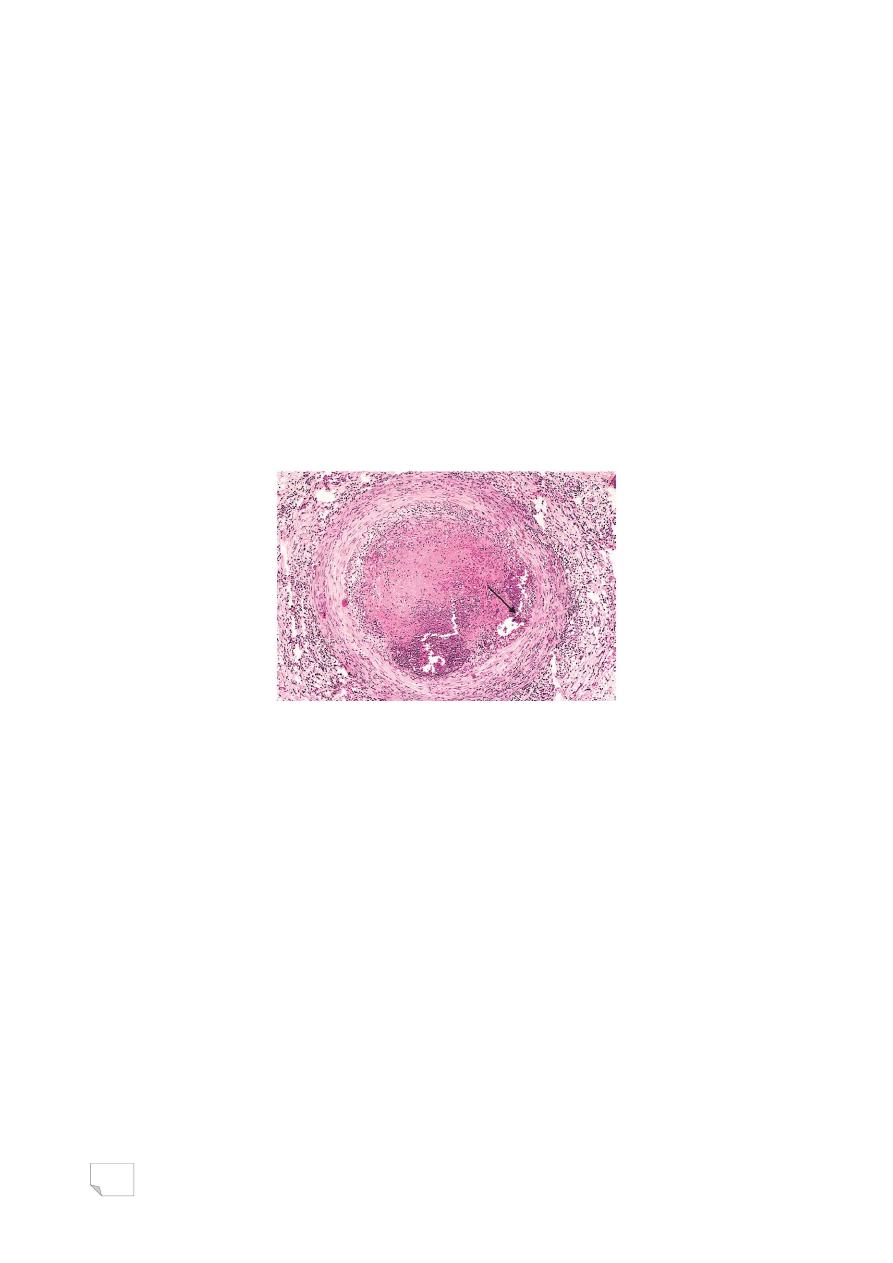
• Thromboangiitis obliterans (Buerger disease). The lumen is
occluded by thrombus containing abscesses (arrow) and the vessel
wall is infiltrated with leukocytes.
Behçet Disease
• Small- to medium-vessel neutrophilic vasculitis
• Classically presents as a clinical triad:
- Recurrent oral aphthous ulcers
- Genital ulcers
- Uveitis.
Raynaud Phenomenon
• Exaggerated vasoconstriction of arteries and arterioles in the
extremities, particularly: fingers and toes, also nose, earlobes,
or lips.
• Digits show ―red - white - blue‖

29
• Raynaud phenomenon
1. Primary Raynaud Phenomenon
• Caused by exaggerated central and local vasomotor responses to
cold or emotion
• Affects 3% to 5% of population
• Symmetrically affect the extremities
• The severity and extent of involvement typically remains static
over time.
2 . Secondary Raynaud Phenomenon
. Arterial insufficiency of the extremities caused by:
-SLE
-Systemic sclerosis
-Atherosclerosis
-Buerger disease
• Asymmetric involvement of the extremities
• Progressively worsens in extent and severity over time.
Varicose Veins
• Abnormally dilated, tortous veins, often
scarred with thrombosis, secondary to:
- prolonged high intraluminal pressure
- loss of vessel wall support
• Mostly involve superficial veins of legs,
causing leg edema>stasis dermatitis
• People at risk:
- period of standing
-older than 50 years
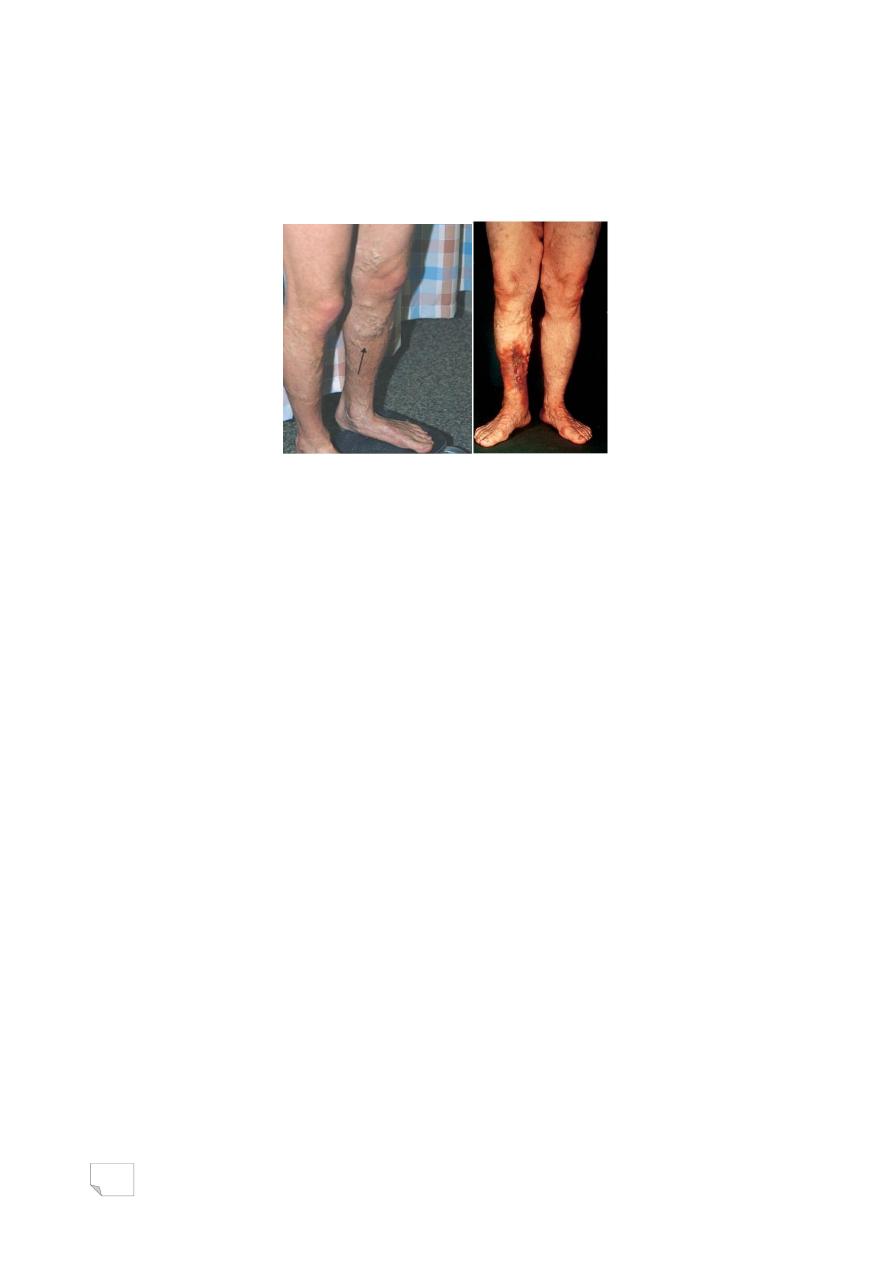
30
-obese
-women with multiple pregnancies
-familial tendency (weakness of wall)
• Varicose vein of legs
• Apart from legs, varices occur also at :
-The lower end of esophagus ( esopahgeal varices)
-Ano-rectum (hemorrhoids)
-Scrotum (varicocele)
Thrombophlebitis & phlebothombosis
• In 90% of cases deep veins of the legs are involved
• Predisposing factors:
-cardiac failure
-neoplasia
-pregnancy
-obesity
-postoperative state
-prolonged bed rest
-hypercoagulability syndromes
• Clinically, pain is elicited
-by pressure over affected veins
-on dorsiflexion (Homan sign)
• Pulmonary embolism is a common and serious sequelae
31
• Migratory thrombophlebitis (Trousseau sign):
• In patients with cancer, hypercoagulability occurs due to
elaboration of procoagulant factors by tumor cells resulting in
venous thromboses, classically appear in one location,
disappear, and then occur in another site
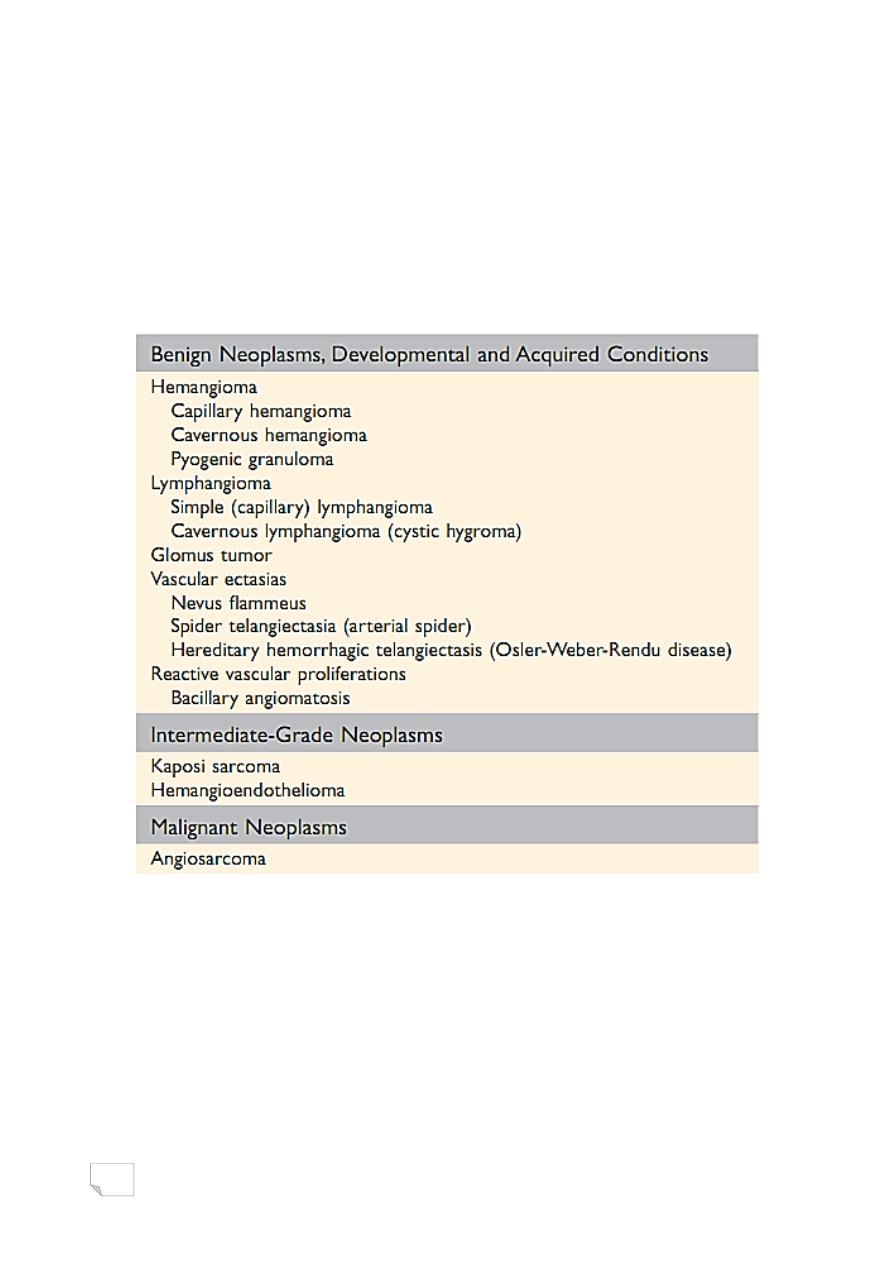
Classification of Vascular Tumors and Tumor-like Conditions
Hemangiomas
• Very common tumors composed of blood-filled vessels.
• Constitute 7% of all benign tumors of infancy and childhood;
• Capillary hemangiomas
• Most common type
• Occur in the skin, subcutaneous tissues, and mucous membranes of
the oral cavities and lips, as well as in the liver, spleen, and kidneys
• Histologically: thin-walled capillaries with scant stroma
• Cavernous hemangiomas
32
• Composed of large, dilated vascular channels.
• Frequently involve deep structures
• Not spontaneously regress.
Lymphangiomas
• Benign lymphatic counterpart of hemangiomas.
• Simple (capillary) lymphangiomas
• Occur predominantly in the head, neck, and axillary subcutaneous
tissues.
• Histologically: networks of endothelium-lined spaces
• Cavernous lymphangiomas (cystic hygromas)
• Typically neck or axilla of children
• Common in Turner syndrome.
• Massively dilated lymphatic spaces lined by endothelial cells +
lymphoid aggregates.
Kaposi Sarcoma
• Vascular neoplasm caused by Kaposi sarcoma herpes virus
(KSHV, also known as human herpes-virus-8, or HHV-8).
• Four forms of KS:
• Classic KS; Endemic African KS; Transplant-associated KS;
AIDS-associated (epidemic) KS
• Three stages: patch, plaque, nodule.
• Histologically: proliferating spindle cells, slit like vessels,
extravasated RBC
33
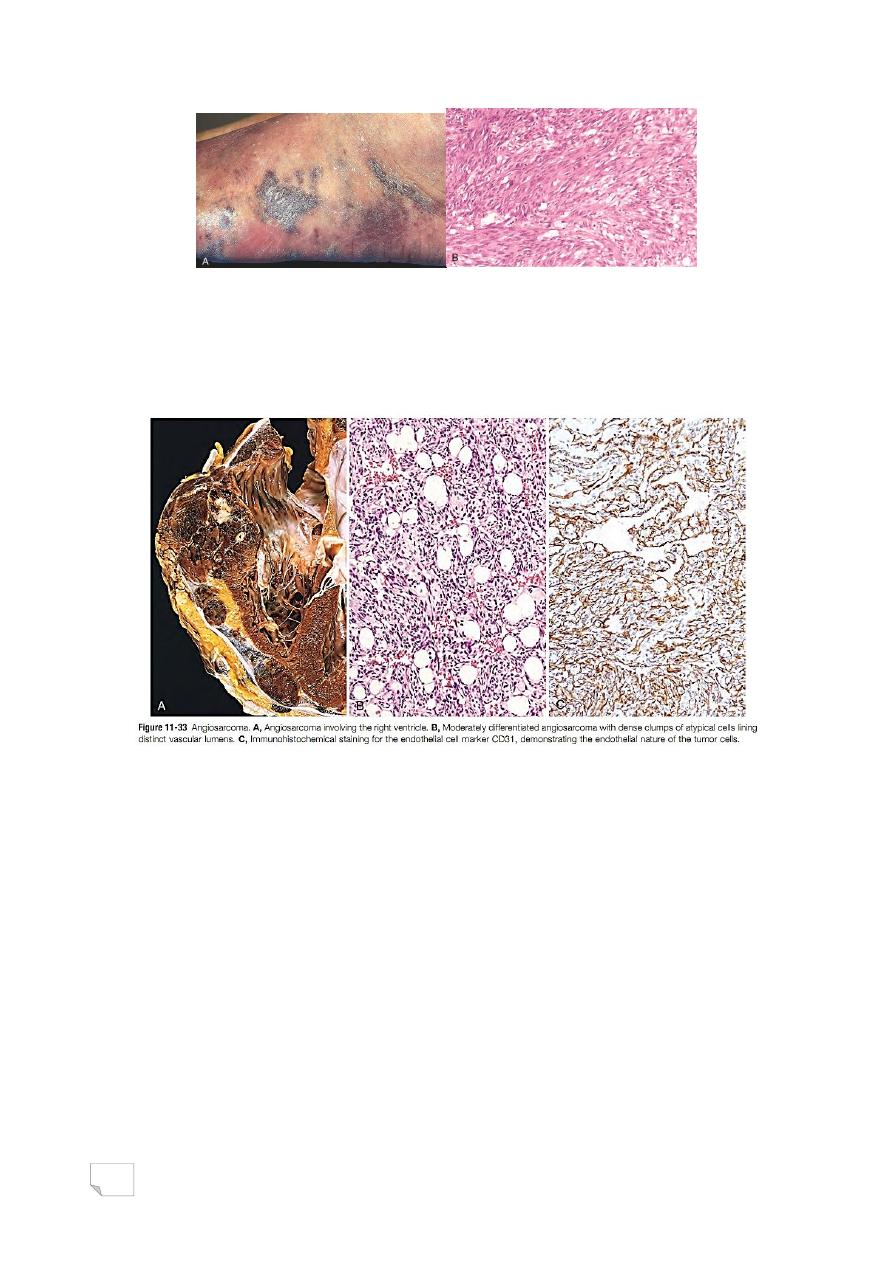
Angiosarcoma
Malignant endothelial neoplasm that primarily affects older adults.
• Most often involves skin, soft tissue, breast, and liver.
• Heart, angiosarcoma, moderately differentiated, endothelial cell
marker (CD31)

34
د. مصطفى امراض
02
\
0
\
0202
( عدد االوراق
5
) م
\
3
\
موصل
lec: 4
The Heart
—
Heart weight varies with body weight and height, (250-300gm in
females, 300-350g in males)
—
Thickness of right ventricle is 0.3-0.5cm and of left ventricle is 1.3-
1.5cm
—
Myocytes form 25% of the total number of cells in the heart
—
Epicardial coronary arteries, (left anterior descending, left
circumflex, right)
—
Intramural are vessels that penetrate the myocardium
Mechanisms of cardiac dysfunction
Pump failure
Outflow obstruction
Flow regurgitation
Conductive failure
Disruption of the continuity of the circulatory system
HEART FAILURE
Definition:
Inability of the heart to pump blood at a rate needed by tissues for
normal metabolism or does it only at an elevated filling
pressure.

35
Causes of heart failure
Failure of myocardial contractility : (systolic dysfunction)
.ischemic injury
.pressure overload
.volume overload
.dilated cardiomyopathy
Inability of the heart to relax or expand: (diastolic
dysfunction)
.myocardial abnormality (hypertrophy, fibrosis, amyloidosis)
.pericardial abnormality (constrictive pericarditis )
Types of heart failure
-Forward (diminished cardiac output)
-Backward (damming back of blood in the venous system)
Pathophysiology of cardiac hypertrophy
- Increase in protein synthesis
- Hyperplasia of sarcomeres and mitochondria
- Increase in dimension and mass of myocytes> increase in heart size
- Prolonged overload>production of fetal type of protein
- Structural alteration (decrease in capillary to myocyte ratio, interstitial
fibrosis)
- Sustained cardiac hypertrophy>cardiac failure
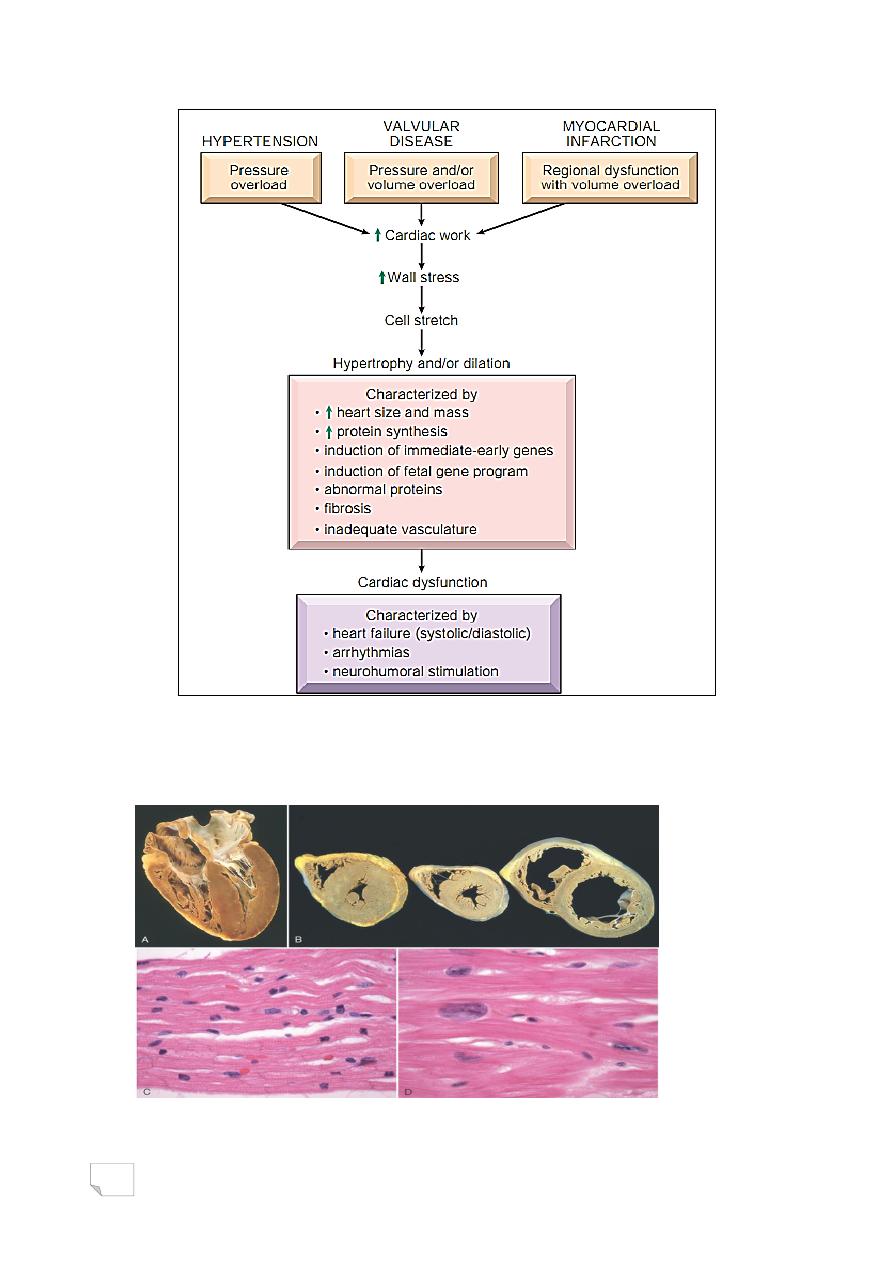
36
Causes and consequences of cardiac hypertrophy
—
Left ventricular hypertrophy

37
Left-Sided Heart Failure
Causes:
-Ischemic heart disease
-Systemic hypertension
-Aortic and mitral valvular diseases
-Non-ischemic myocardial diseases
Organ changes in Lt side HF
Heart, changes are variable
Lungs, congestion, edema>dyspnea, orthopnea, paroxysmal
nocturnaldyspnea
Kidneys, activation of renin-angiotensin- aldosterone systemic
retention of fluid and salt
Brain, hypoxic encephalopathy, irritability, restlessness, coma
RIGHT-SIDED HEART FAILURE
Causes:
-Secondary to left-sided failure
-Chronic pulmonary hypertension
Organ changes in Rt side HF
liver, congestive hepatomegaly > cardiac cirrhosis
spleen, congestive splenomegaly and ascites (portal hypertension)
kidneys, congestion

38
bowels, congestion
pleural cavity, effusion
pericardial sac, effusion
systemic, edema > anasarca
CONGENITAL HEART DISEASES
Most common types of heart diseases among children
Occur in about 1% of live births, higher incidence in prematures
and stillborns
Etiology and pathogenesis
I.
Most are developmental anomalies during gestational 3-8 weeks
II.
Multiple factors account for most cases:
1. Genes involved have been identified in only a minority of
conditions, trisomy 21 is the most common
2. In utero rubella and syphilitic infections of the fetus
Clinical Features
-Right to left shunt
-Left to right shunt
-Flow obstruction
Shunt : is an abnormal communication between chambers or blood
vessels.
39
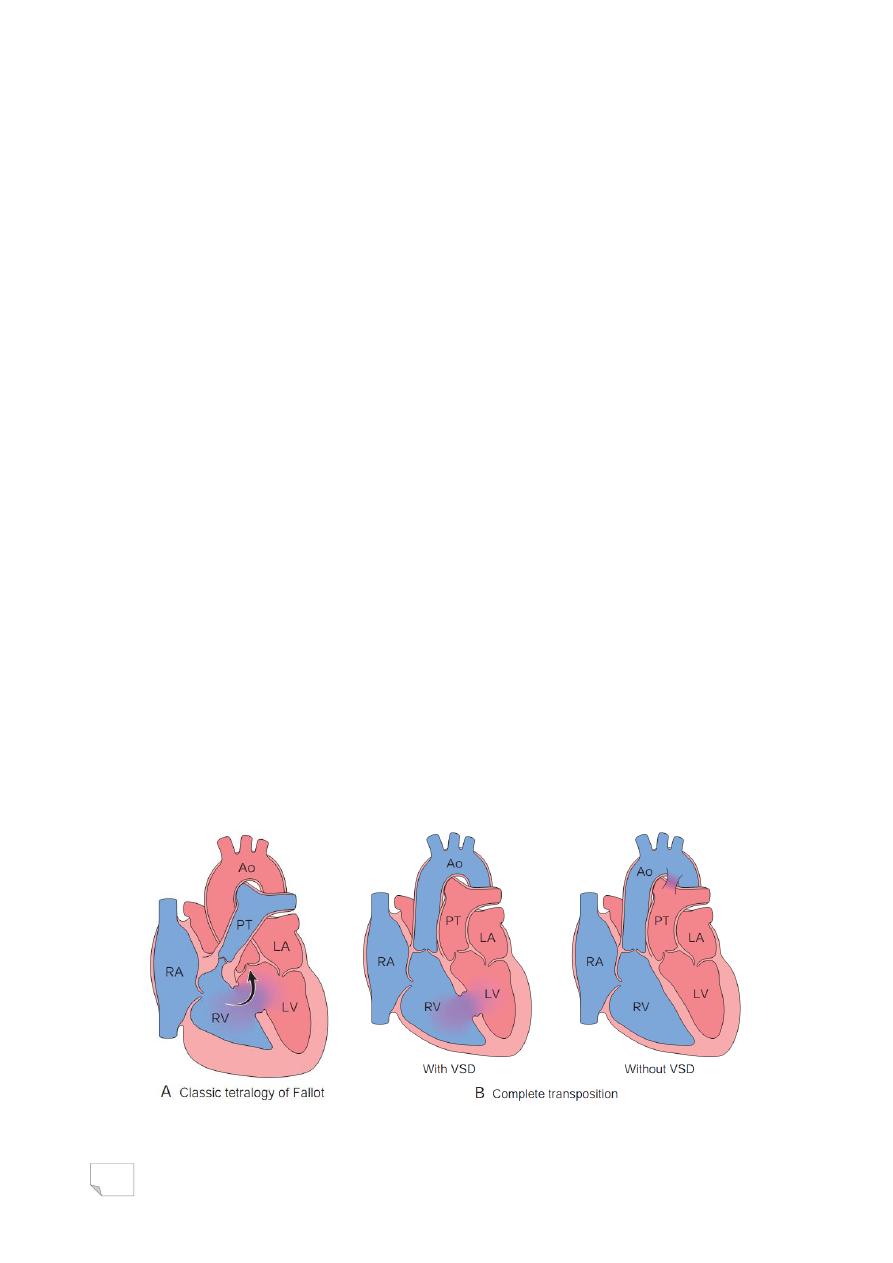
Right to left shunt
-Cyanosis is early,
examples:
.Tetralogy of Fallot
.Transposition of the great arteries
.Persistent truncus arteriosus
.Tricuspid atresia
.Total anomalous pulmonary venous
connection
Tetralogy of Fallot
TETRA:
1) VSD
2) Subpulmonary stenosis
3) Aorta overrides the VSD
4) Right ventricular hypertrophy
—
The heart is typically enlarged and is classically “boot-shaped” due
to marked right ventricular Hypertrophy.
—
10% of untreated patients are alive at 20 years
—
Congenital heart disease, right-to-left shunt

40
—
Congenital heart disease, transposition of the great arteries
Left to right shunt
- Cyanosis is no an early feature - examples
.Atrial septal defect (ASD)
.Ventricular septal defect (VSD)
.Patent ductus arteriosus (PDA)
.Atrioventricular septal defect
ASD
—
Abnormal, fixed openings in the atrial septum
—
Usually asymptomatic until adulthood
—
Classified according to their location:
1. Secundum ASD (90%), in center of the atrial septum.
2. Primum anomalies (5%), adjacent to the AV valves
3. Sinus venosus defects (5%), located near the entrance of the
superior vena cava.
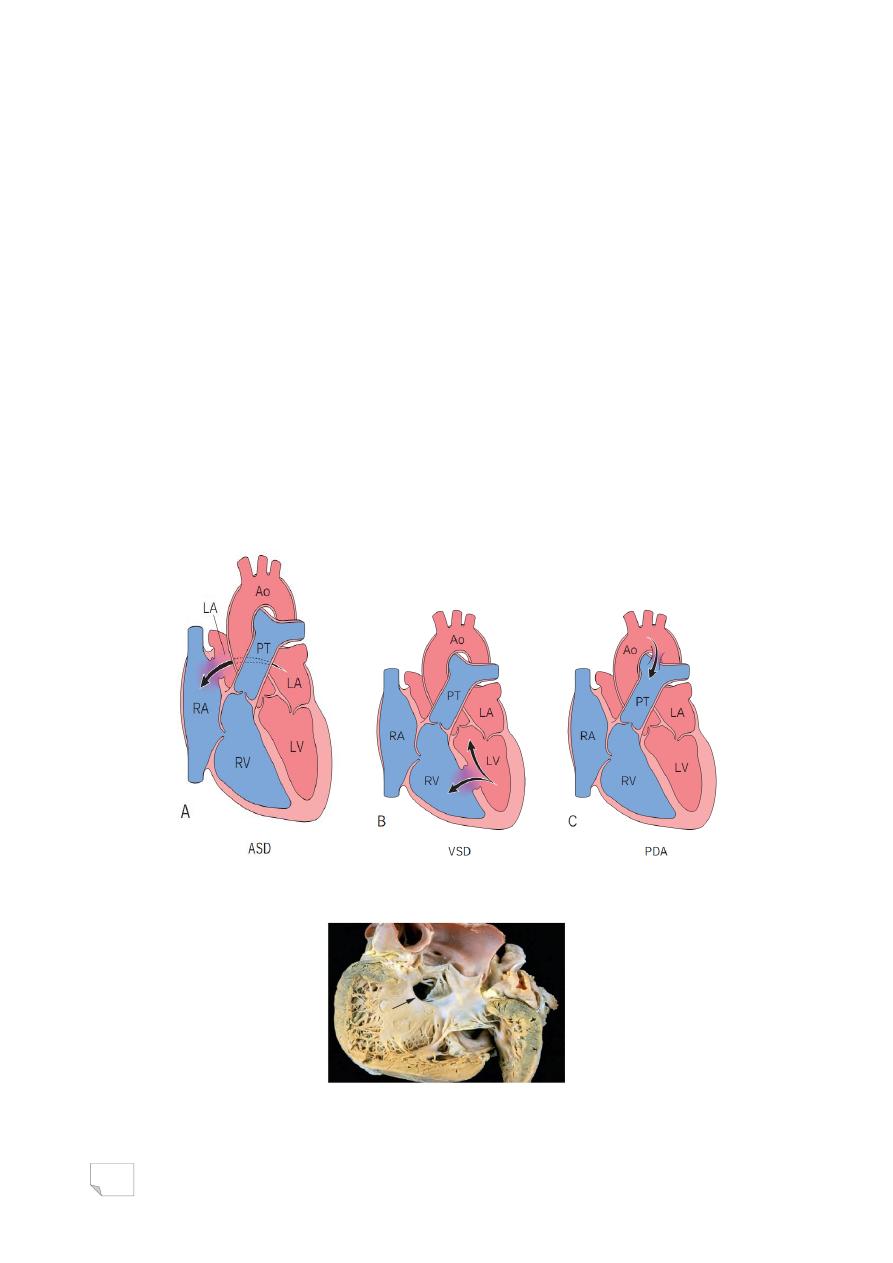
41
VSD
—
Incomplete closures of the ventricular septum
—
Only 20% to 30% are isolated.
—
90% occur in the region of the membranous interventricular
septum
—
10% occur below the pulmonary valve (infundibular VSD) or within
the muscular septum.
—
Most VSDs are single, but those in the muscular septum may be
multiple.
—
Approximately 50% of small muscular VSDs close spontaneously.
—
Congenital heart disease, left-to-right shunt
—
VSD; membraneous

42
Eisenmenger syndrome
—
In left to right shunt: prolonged shunting causes volume and
pressure overload in pulmonary circulation & eventually
pulmonary hypertension.
—
Secondarily right-sided pressure increases & exceeds that on the
left
—
At that point, reversal of blood flow occurs, with resultant right-
to-left shunting of unoxygenated blood into the systemic
circulation and the development of cyanosis.
Obstructive congenital heart diseases
-examples
.Coarctation of the aorta
.Aortic valvular stenosis
.Pulmonary valvular stenosis
Coarctation of the Aorta
—
Coarctation: (narrowing, constriction)
—
Males are twice affected.
—
Females with Turner syndrome are frequently affected
—
Two classic forms:
(1) “Infantile” form: symptomatic in early childhood with tubular
hypoplasia of the aortic arch proximal to PDA
(2) “Adult” form: discrete ridge-like infolding of the aorta just
opposite the closed ductus arteriosus (ligamentum arteriosum) distal to
the arch vessels
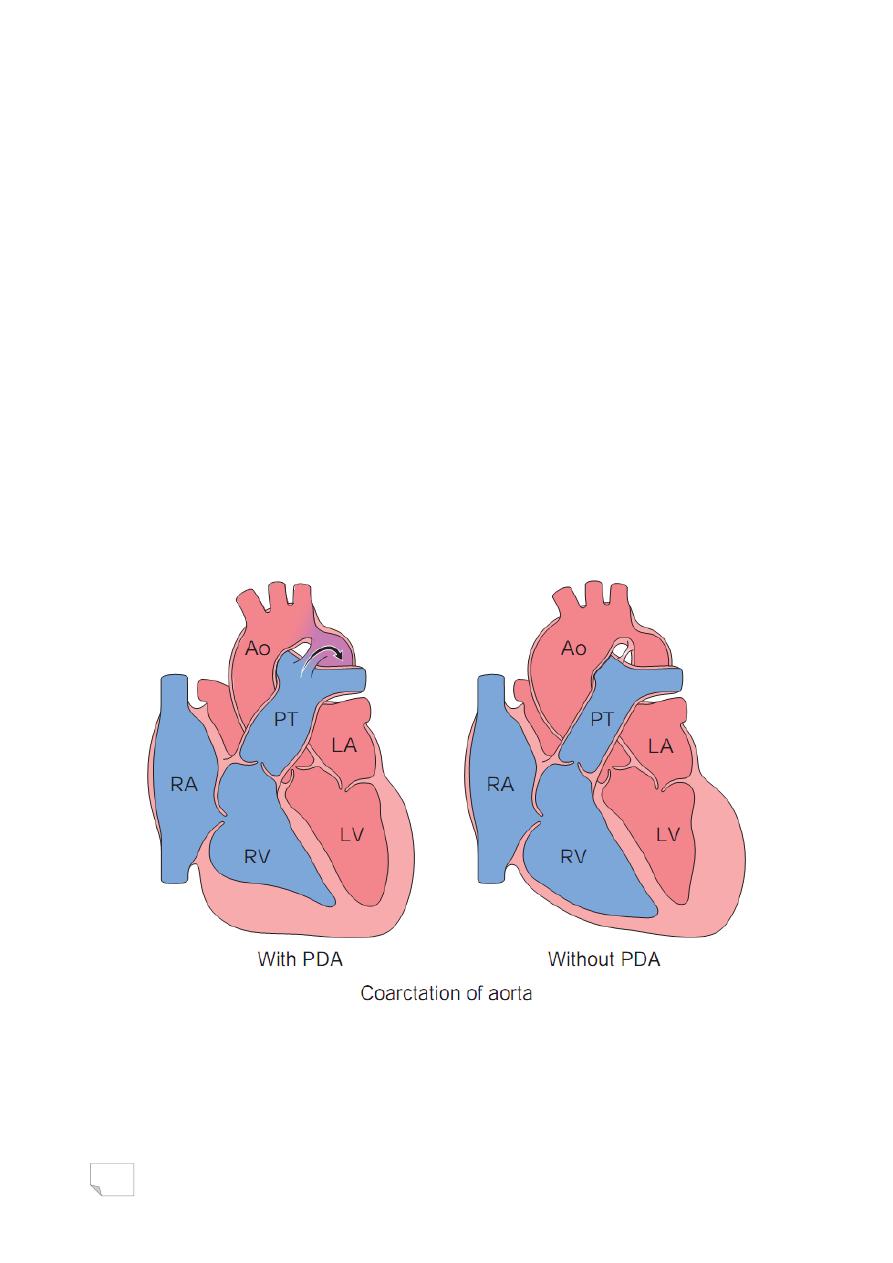
43
Coarctation of the Aorta
—
Clinically;
—
Depend on severity of the narrowing and patency of ductus
arteriosus.
1. CA with PDA: manifests early in life, passage of unsaturated blood
through PDA produces cyanosis localized to the lower half of the body
2. CA without PDA: asymptomatic, and may unrecognized until adult
life. Typically; hypertension in the upper extremities with weak pulses &
hypotension in the lower extremities, + arterial insufficiency (i.e.,
claudication and coldness).
—
Congenital heart disease, coarctation of the aorta

44
د. مصطفى امراض
24
\
2
\
2142
( عدد االوراق
6
) م
\
3
\
موصل
lec: 5
The Heart
ISCHEMIC HEART DISEASE (IHD)
. A group of closely related syndromes due to imbalance between
(perfusion) and demand of the heart for oxygenated blood.
. Ischemia comprises:
-insufficiency of oxygen
-reduced availability of nutrients
-inadequate removal of metabolites
. IHD is the leading cause of death in most parts of the world
ISCHEMIC HEART DISEASE (IHD)
- > 90% of cases, IHD is a consequence of reduced coronary
blood flow secondary to obstructive atherosclerotic vascular
disease
- Less frequently, IHD can result from:
- Increased demand ( increased heart rate or HT)
- Diminished blood volume (hypotension or shock)
- Diminished oxygenation (pneumonia or CHF)
- Diminished oxygen-carrying capacity (anemia or CO poisoning).
Syndromes
1 -Myocardial infarction ( MI)
2 -Angina pectoris
3 -Chronic ischemic heart disease
4 -Sudden cardiac death
The term acute coronary syndrome is applied to any of the three
catastrophic manifestations of IHD— unstable angina, acute MI, and
SCD.
45

46
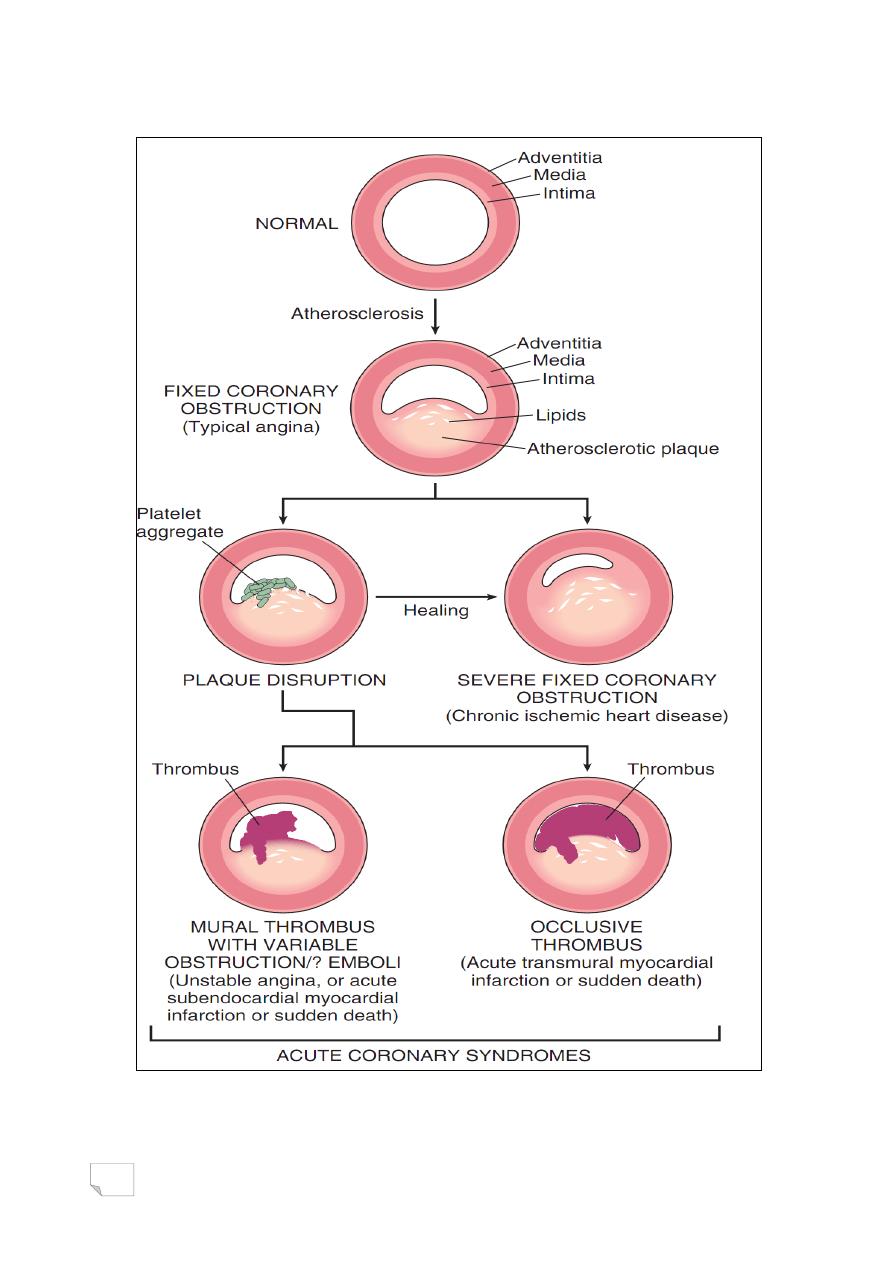
Sequential progression of coronary artery lesions to acute coronary
syndromes
Pathogenesis of ischemic heart disease
- Diminished coronary perfusion relative to myocardial demand
- Combination of preexisting ―fixed‖ atherosclerotic occlusion of
coronary arteries and new, superimposed thrombosis and/or
vasospasm.
- Fixed stenotic lesion of 70% or greater is symptomatic after
exercise
- 90% stenosis can lead to inadequate coronary blood flow even at
rest
- Common sites of stenosis are:
. at first centimeters of LAD and LCX
. along the entire length of the RCA
— Role of acute plaque changes
- In most patients there is abrupt plaque
changes followed by thrombosis
.rupture/fissuring
.erosion/ulceration
.hemorrhage into the atheroma
. Role of inflammation
- Plays an essential role at all stages of atherosclerosis, from
inception to plaque rupture
- Destabilization and rupture of plaque may be the result of metallo-
proteinase secretion by macrophages
— Role of coronary thrombus
-Partial or total thrombosis is associated with disrupted plaque
-Embolization of mural thrombus
-Thrombus is a potent activator of multiple growth-related signals in
smooth muscle cells which contribute to growth of atherosclerotic
lesions

47
. Role of vasoconstriction
-At sites of atheroma is stimulated by
- Circulating adrenergic agonists
- Locally released platelets contents
- Endothelial dysfunction causing imbalance between relaxing factors
( nitric oxide) & contracting factors (endothelin)
- Mediators released from perivascular
inflammatory cells
ANGINA PECTORIS
. Paroxysmal and recurrent attacks of substernal or precordial chest
discomfort (as constricting, squeezing, choking or knife- like), caused
by transient (15seconds- 15minutes) myocardial ischemia that is
insufficient to induce myocyte necrosis.
. 3 over-lapping patterns:
1- Stable (typical)
2- Prinzmetal variant
3 - Unstable or crescendo
Stable Angina (typical)
. Most common form of angina
. Caused by an imbalance in coronary perfusion (due to chronic
stenosing coronary atherosclerosis) relative to myocardial demand ,
such as that produced by physical activity, emotional excitement or
psychological stress.
. Relieved by rest or vasodilators (nitroglycerin)
Prinzmetal Angina or variant angina
. Uncommon
. Is due to coronary artery spasm.
. The attacks are unrelated to physical activity ( occur at rest)
. Responds to vasodilators

48
Unstable Angina ( Crescendo)
. Frequent, prolonged (>20 min), or severe angina or chest discomfort
, precipitated by progressively lower levels of physical activity or even
occurring at rest
. Associated with plaque disruption with superimposed partial
thrombosis, distal embolization &/or vasospasm
. It is often the harbinger of MI, caused by complete vascular
occlusion
MYOCARDIAL INFARCTION
―Heart Attack,‖ is the necrosis of cardiac muscle due to prolonged
severe ischemia.
. Acute plaque change>total thrombotic
occlusion>death of cardiac muscle
— Incidence and risk factors of MI
-Occurs at any age, frequency rises progressively with
increasing age
-Nearly 10% occur in people under 40 years and 45% occur in
people under 65 years
-Males > females
Transmural versus subendocardial infarction
-Tansmural infarct involves full or nearly full wall thickness of
ventricular wall in the distribution of a single coronary artery
- It is associated with:
.atherosclerosis
.acute plaque change
.superimposed thrombosis
- Subendocardial infarct is limited to inner 1/3-1/2 of ventricular
wall,
- Occurs:
. As a result of plaque disruption followed
by coronary thrombus that lyses before

49
necrosis extends across full or near full
wall thickness
. Following prolonged or severe hypotension,
(shock), often super-imposed on chronic
non-critical coronary stenosis.
Pathogenesis of MI
- Coronary arterial occlusion (90%)
. Sudden change in the morphology of
an atheromatous plaque( hemorrhage, ulceration,…)
. Platelets adhesion, aggregation, activation
. Vasospasm
. Activation of extrinsic pathway of coagulation
. Thrombosis
- In 10% of cases there is no atherosclerotic plaque thrombosis.
- Other mechanisms may be involved:
. Vasospasm eg. Cocaine, adrenalin..
. Emboli from left side of heart or paradoxical
. Others (vasculitis, hemoglobinopathies,
amyloid deposition in vessel wall, vascular
dissection)
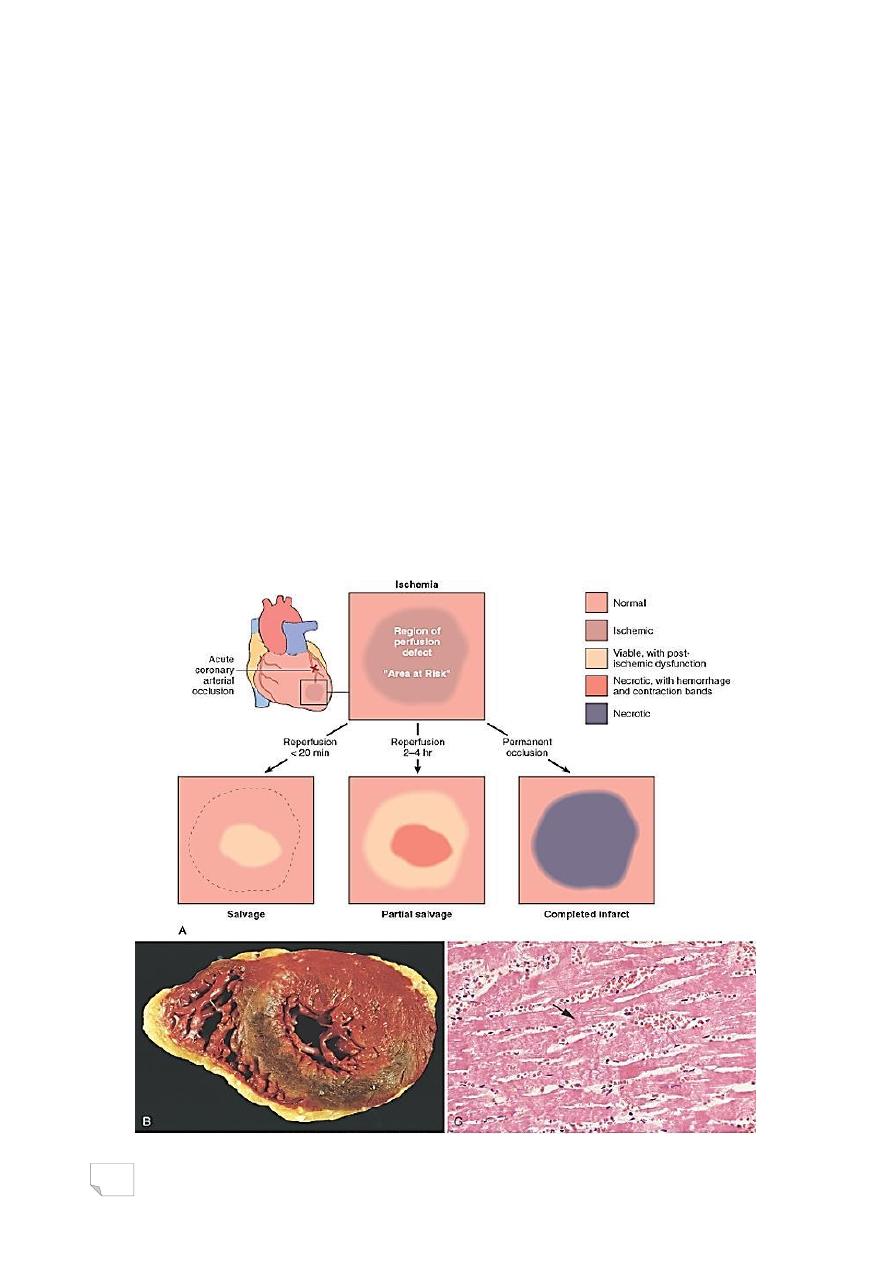
Myocardial response in MI :
. Biochemical: within seconds >Cessation of aerobic glycolysis >
accumulation of lactic acid
. Functional: within 60 seconds of ischemic onset Loss of contractility
> acute heart failure
. Morphological: After 20-40 minutes ischaemia > necrosis
.Irreversible injury first subendocardial>
transmural
50
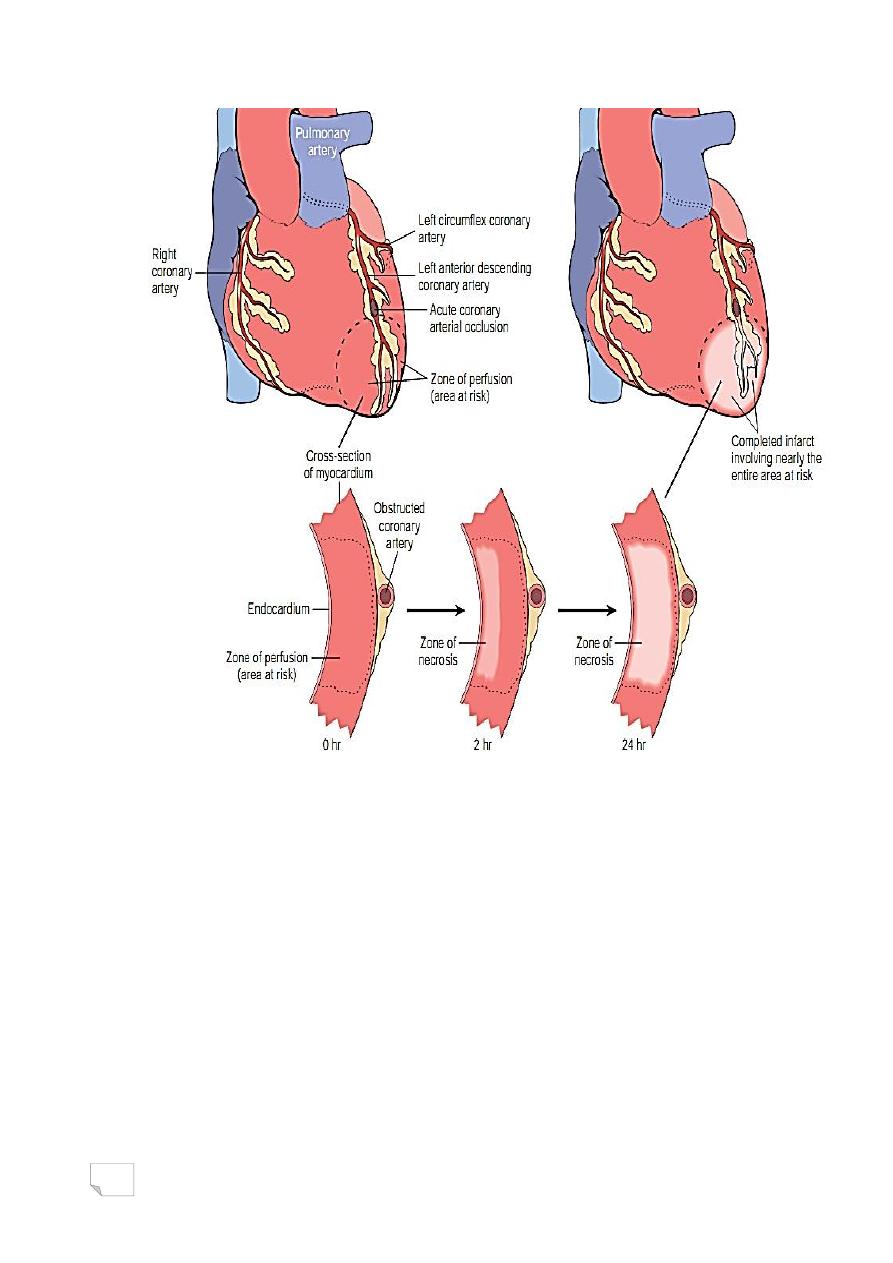
Progression of myocardial necrosis following coronary artery
occlusion
.Morphology of MI
- Nearly all transmural infarcts involve at least a portion of the left
ventricle
- Isolated infarction of right ventricle occurs in up to 3% of cases
- Presence of multiple severe stenoses or thromboses in absence of
infarction suggests protection by collaterals
- Narrowing and thrombosis of:
.LAD, infarction of anterior wall of left ventricle
near apex, anterior portion of ventricular
septum and apex circumferentially
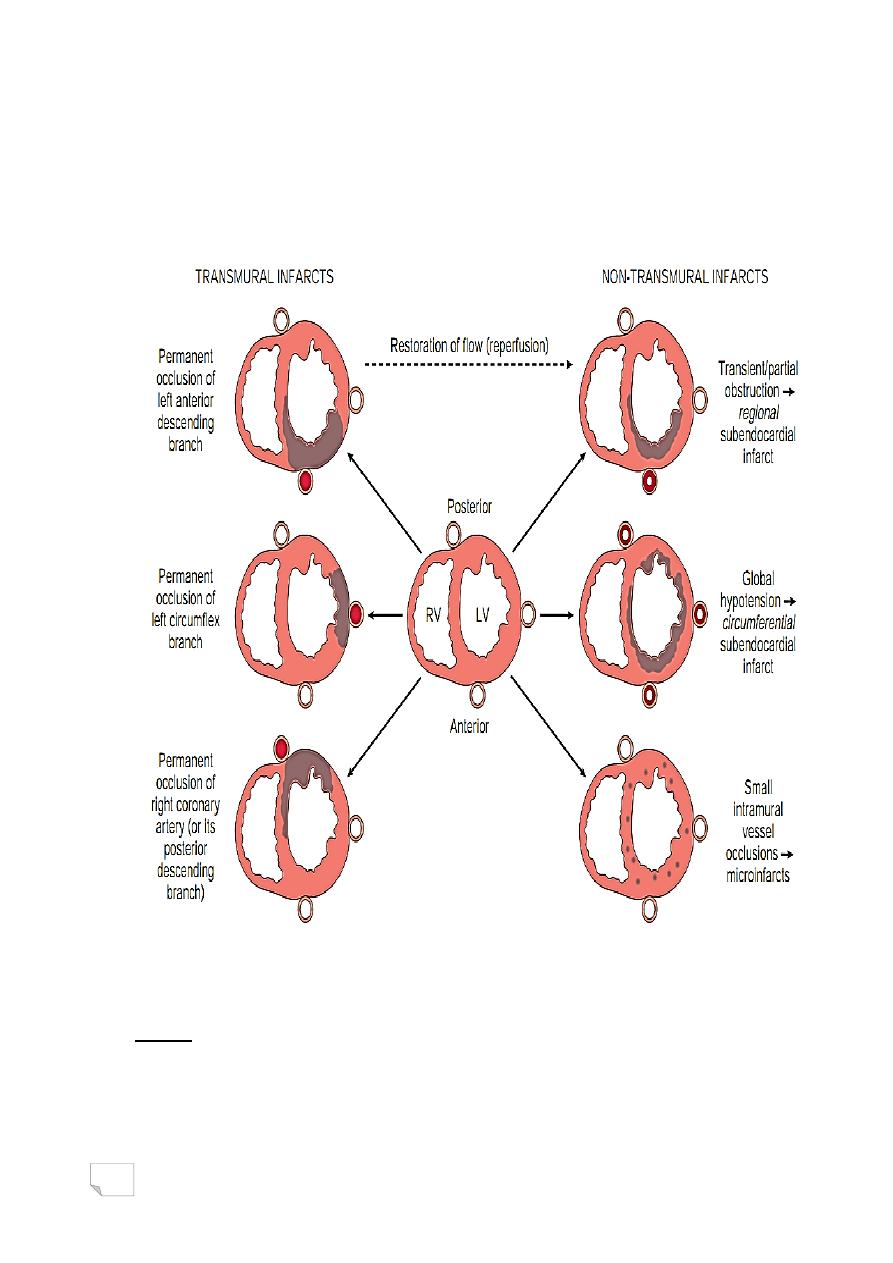
51
.RC, infarction of posterior wall of Lt ventricle, posterior portion of
ventricular septum and posterior wall of right ventricle
.LXC, infarction of lateral wall of left ventricle except the apex
— Distribution of myocardial infarction in relation to coronary
artery occlusion
Morphology
Gross:
. Infarcts <12 hrs are usually not apparent grossly, can be
demonstrated by solution (triphenyltetrazolium chloride)
.Infarct older than 12-24 hrs appears red/ blue ( stagnant blood),
progressively becomes yellow/tan
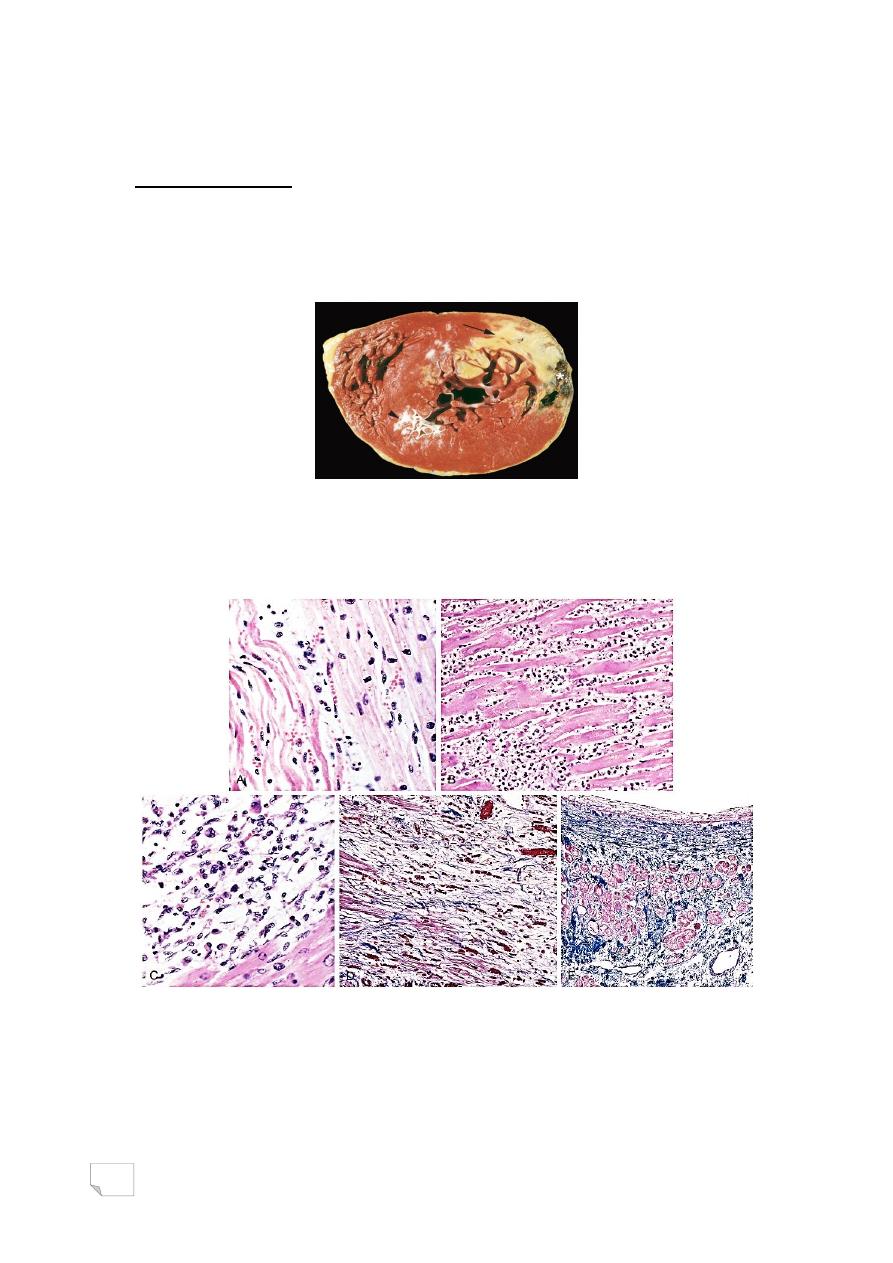
52
.By 3-7 days is rimmed by hyperemia / central yellow tan
.Over weeks scar will develop
Light microscopy:
. 4-24 hrs beginning & ongoing coagulative necrosis
. 1-3 days Coagulative necrosis & acute inflammation
. 1-2 weeks granulation tissue peaking
. > 2 months dense colgenous scar
— Transmural myocardial infarction, staining by
tripheniletetrazolium chloride: pale zone due to loss of
dehydrogenases
Myocardial infarction, 1 day, 3-4 days, 7-10 days, granulation tissue,
scar
53
Infarct modification by reperfusion
- Reperfusion is achieved by:
. Thrombolysis
. Balloon angioplasty
. Coronary arterial bypass graft
Factors contributing to reperfusion injury
1) Mitochondrial dysfunction: ischemia alters the mitochondrial
membrane permeability, releasing mitochondrial contents that
promote apoptosis
2) Myocyte hypercontracture: in ischemia the intracellular levels of
calcium are increased as a result of impaired calcium cycling and
sarcolemmal damage. After reperfusion the contraction of myofibrils
is augmented and uncontrolled, causing cytoskeletal damage and cell
death
3) Free radicals from leukocytes

54
Reperfusion injury
.Clinical features of MI
- Patient has chest pain, rapid weak pulse, dyspnea, profuse
sweating, nausea
- Painless MI: diabetic neuropathy / elderly
- Diagnosis depends on:
. Typical symptoms
. Biochemical evidence
. ECG changes
Laboratory diagnosis
— Depends on measuring leaky cellular substances
1- Myoglobin
2- Cardiac troponins T and I
3 - Creatine kinase (MB fraction)
4- Dehydrogenase enzyme
The best are troponins T and I, both rise
at 2-4 hrs and peak at 48 hrs, and remain
elevated for 7-10 days
-C-reactive protein serves as a marker to predict the risk of MI in
patients with angina and the risk of new infarcts in patients who
recover from infarcts
.Factors associated with poor prognosis
- Advanced age
- Female gender
- Diabetes mellitus
- Previous MI
Complications after Acute MI
- Contractile dysfunctions & pump failure
- Papillary muscle dysfunction
- Arrhythmias
- Pericarditis & Dressler syndrome
- Infarction of right ventricle
- Mural thrombus
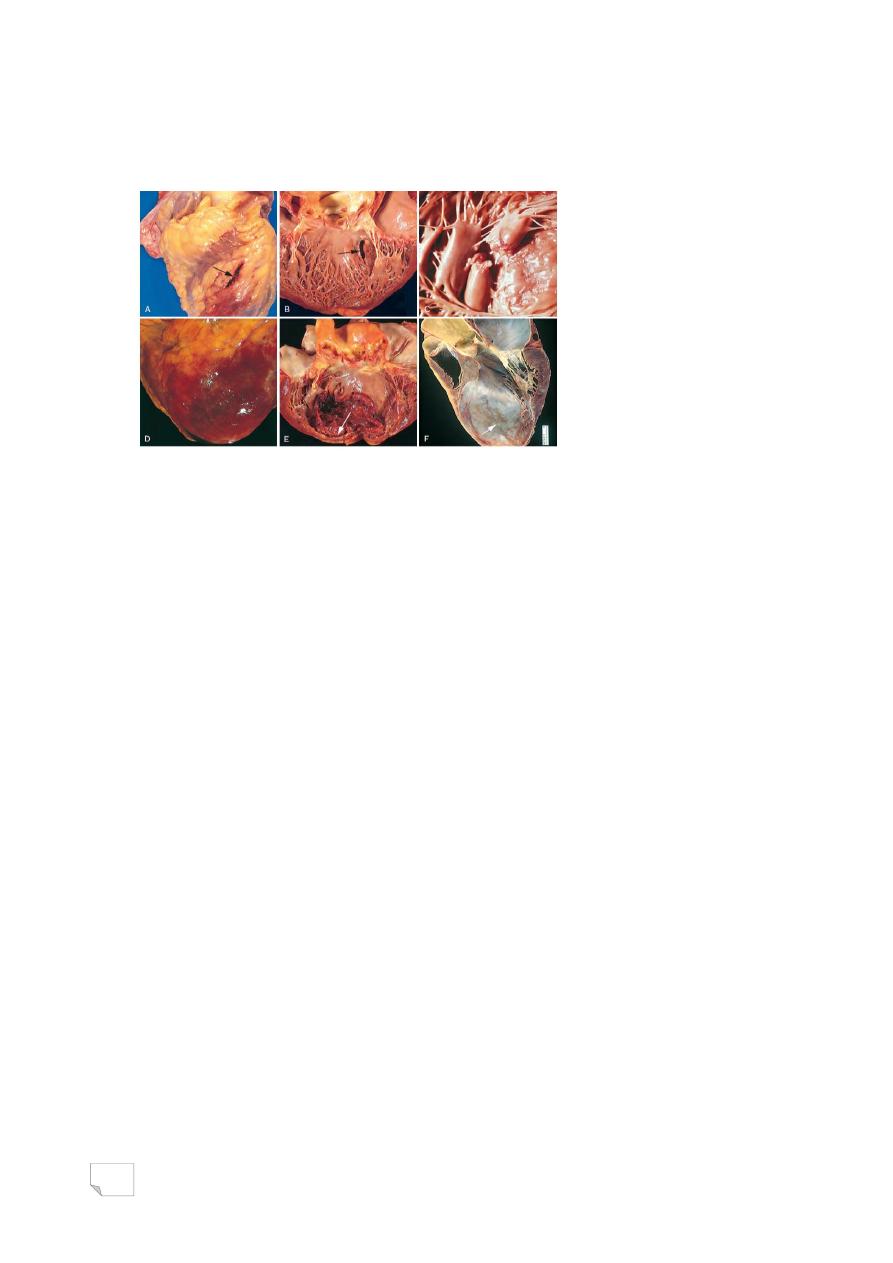
55
- Myocardial rupture (Lt vent. Or septal)
- Ventricular aneurysm
- Progressive late heart failure
Complications of myocardial infarction, rupture, pericarditis,
expansion, aneurysm
CHRONIC ISCHEMIC HEART DISEASE
. Elderly patients with progressive heart failure due to ischemic
damage, in most cases they have
- Prior MI
- Sometimes coronary intervention or bypass
. Morphology
-Heart is enlarged and heavy due to left ventricular hypertrophy and
dilation
-Coronary arteries, (moderate to severe stenosis, total occlusion)
-Myocardium, (discrete gray/white scars of healed infarcts)
SUDDEN CARDIAC DEATH
. Unexpected death from cardiac causes early after symptom onset or
without symptoms
. Mechanism: lethal arrhythmia
. Causes
- Complication and often the first clinical manifestation of IHD
- Congenital cardiac anomalies
- Aortic valve stenosis
- Myocarditis
- Dilated/Hypertrophic cardiomyopathy
- Pulmonary hypertension

56
د. مصطفى امراض
22
\
2
\
2142
( عدد االوراق
4
) م
\
3
\
موصل
lec: 6
The Heart
HYPERTENSIVE HEART DISEASE
LEFT-SIDED HYPERTENSIVE HEART DISEASE
.Minimal criteria for diagnosis
- Left ventricular hypertrophy in the absence
of other causes
- History or pathologic evidence of hypertension
. Left ventricle weighs more than 500gm
. May be asymptomatic or patient has atrial fibrillation, CHF or both
— RIGHT-SIDED HYPERTENSIVE HEART DISEASE
(CORPULMONALE)
. Causes:
- diseases of lungs
- diseases of pulmonary vasculature
- disorders affecting chest movement
- massive pulmonary embolism
- prolonged pressure overload
. In acute state>marked dilation of right ventricle without
hypertrophy
. In chronic state>right ventricular hypertrophy
Hypertensive heart disease,
A: systemic B: pulmonary

57
VALVULAR HEART DISEASE
. Types:
- Stenosis (failure of a valve to open completely)
- Regurgitation (failure of a valve to close
completely)
. Valvular abnormalities may be congenital
or acquired, are either pure or combined
. Functional regurgitation results from:
- dilation of the ventricle
- dilation of aortic or pulmonary artery
Aortic Stenosis
. Causes
- calcification of normal valve
- calcification of congenitally bicuspid valve
- rheumatic fever
. Clinical presentation
- angina
- CHF
- syncope
— Aortic Insufficiency
. Due to dilation of ascending aorta related to hypertension and
aging
Mitral Valve Stenosis
. Due to rheumatic heart disease and degenerative calcification
Mitral Valve Insufficiency
. A result of, degenerative calcification, and myxomatous
degeneration
58
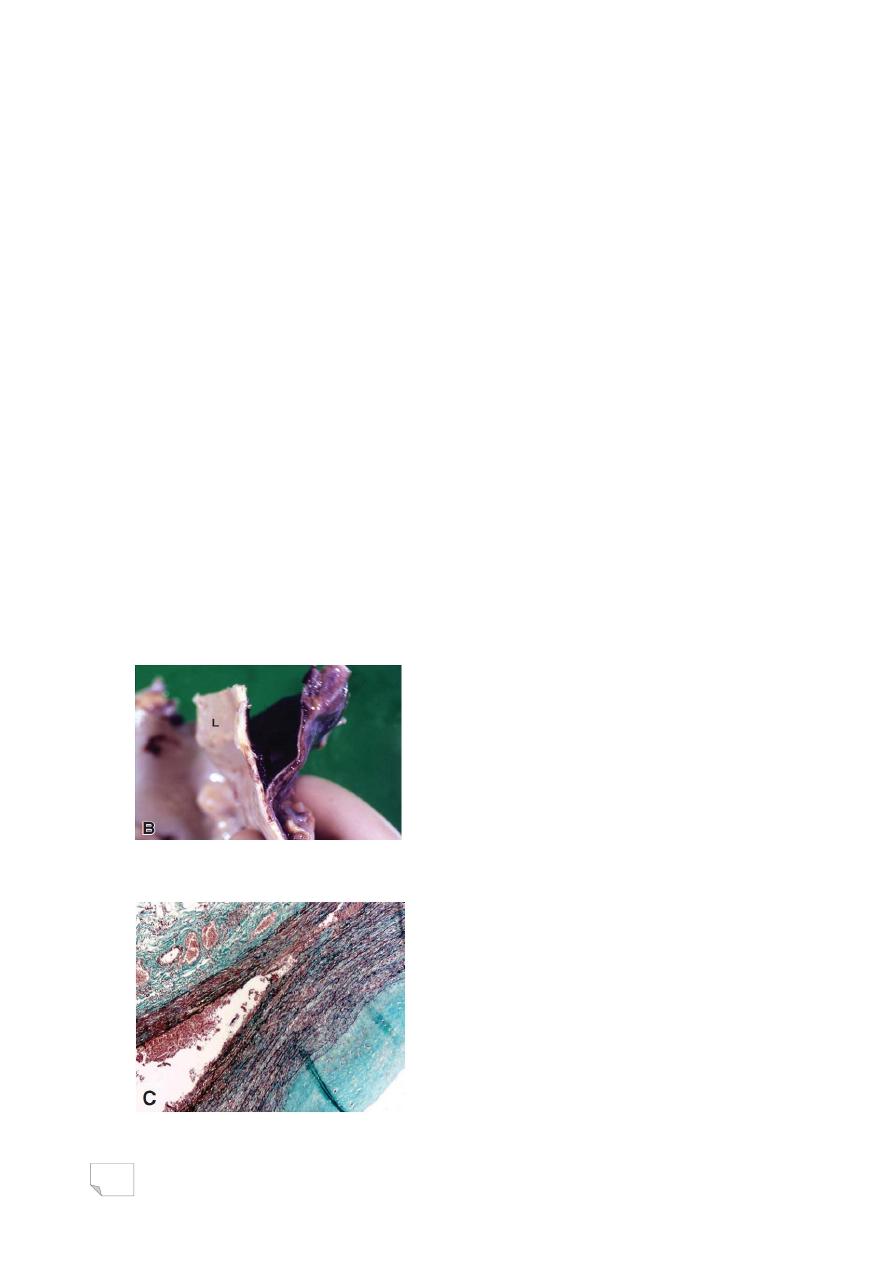
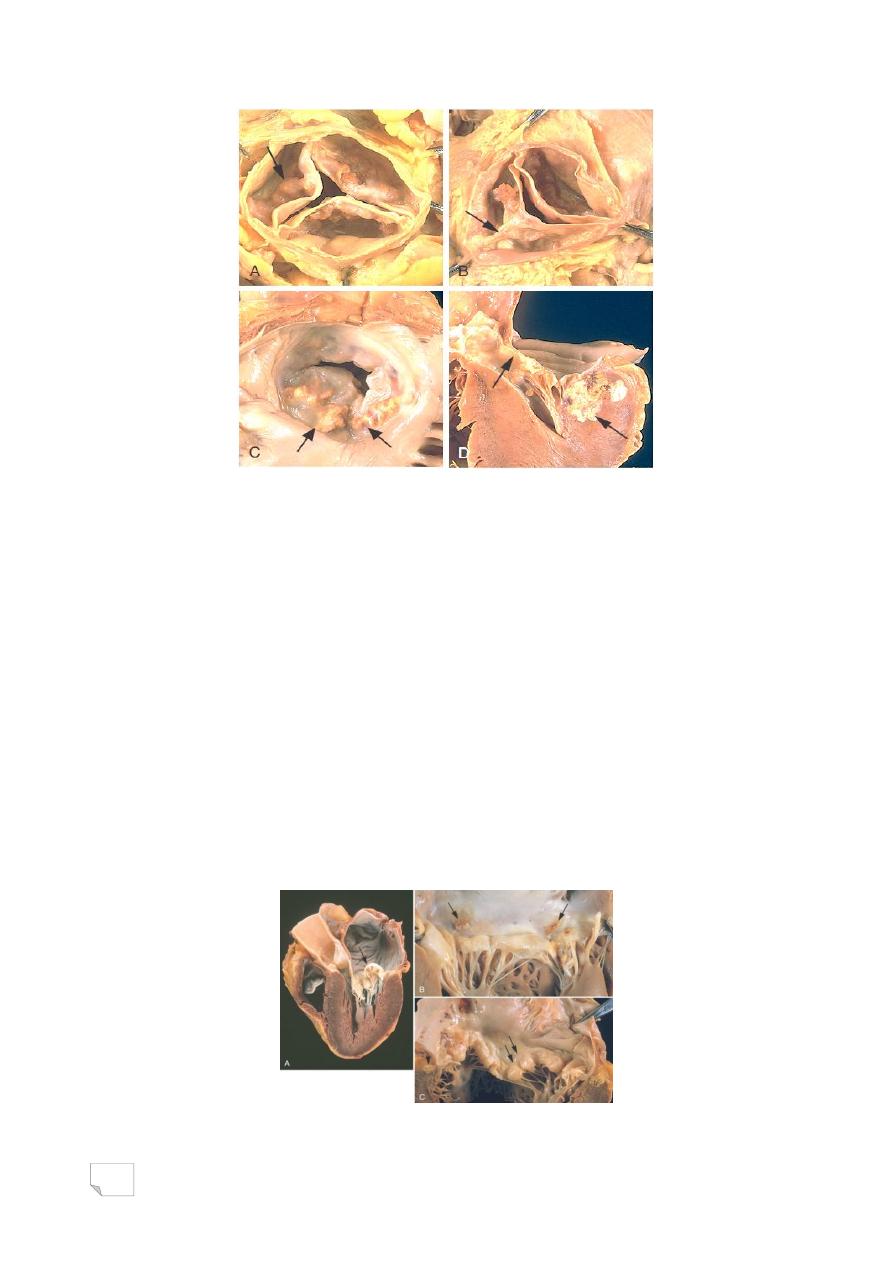
Calcific valvular degeneration,
A, B: aortic valve. C, D: mitral valve
Mitral Valve Prolapse
. Affects 3% of mostly young women
. Myxomatous change in the valve leaflets probably due to underlying
genetic defect of connective tissue
. Clinically
- Most asymptomatic
- Minority have mitral valve insufficiency
- Few patients have chest pain, dyspnea
and fatigue
. About 3% develop complications,
(infective endocarditis, stroke or other
systemic infarcts, arrhythmias)
Mitral valve prolapse
59
Mitral valve prolapse, myxomatous degeneration (Movat pentachrome
stain), collagen (yellow), elastin (black), proteoglycans (blue)
RHEUMATIC FEVER
. Acute immunologically mediated multi-system
inflammatory disease occur few weeks after
pharyngitis caused by group A beta hemolytic streptococci.
. Acute rheumatic fever most often affects children of 5-15 years of
age
. Chronic rheumatic carditis occurs years or even decades after acute
RF
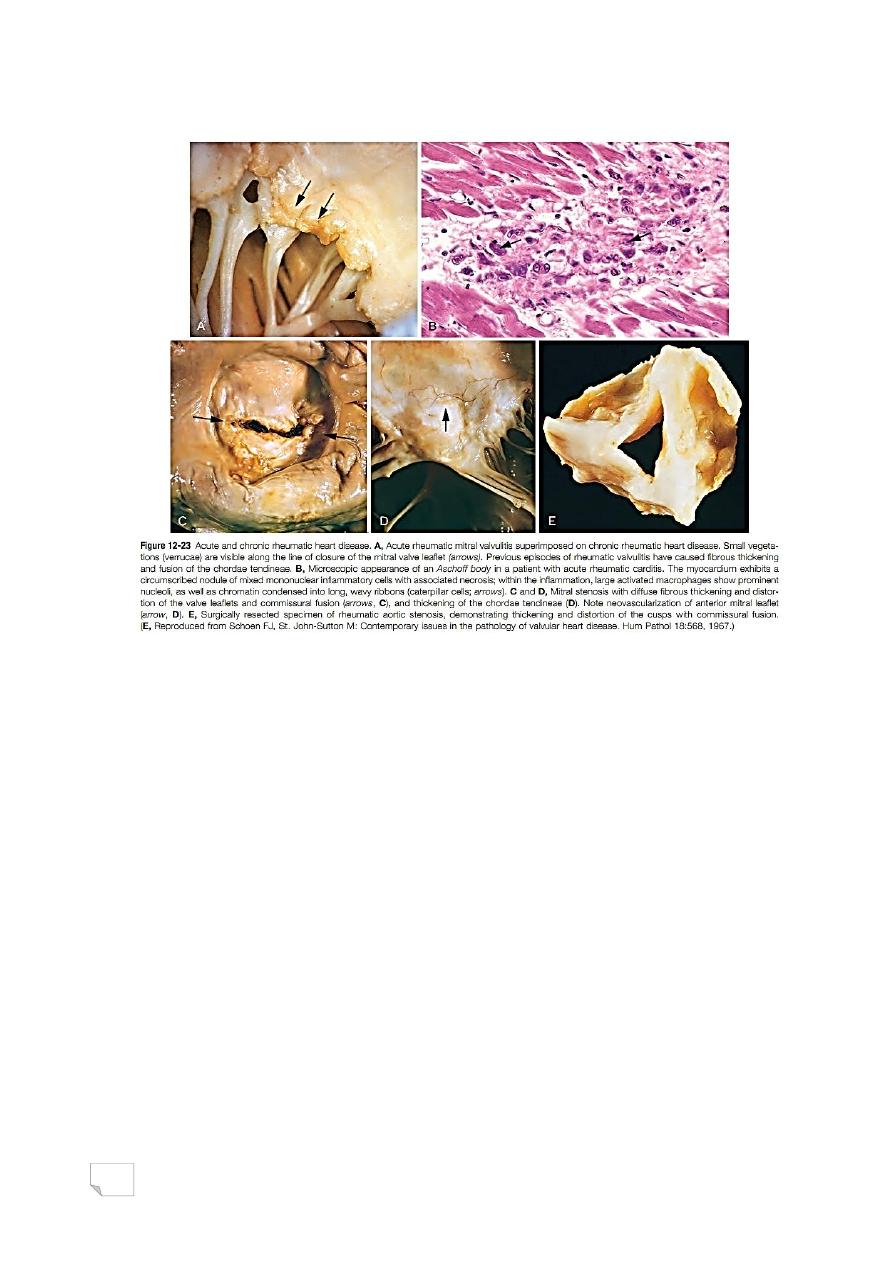
Morphology
- Acute RF is characterized by multi-system inflammatory lesions:
(Aschoff bodies, consist of foci of swollen collagen surrounded by
lymphocytes, occasional plasma cells, and plump macrophages -
Anitschkow cells-which may form giant cells)
- Chronic RHD is characterized by, organization of the acute
inflammation, fibrosis, and deformity of involved valves
- Mitral valve: leaflet thickening, commissural fusion
and shortening of chordae tendineae; creating ―fish-
mouth‖ or ―buttonhole‖ stenosis
60
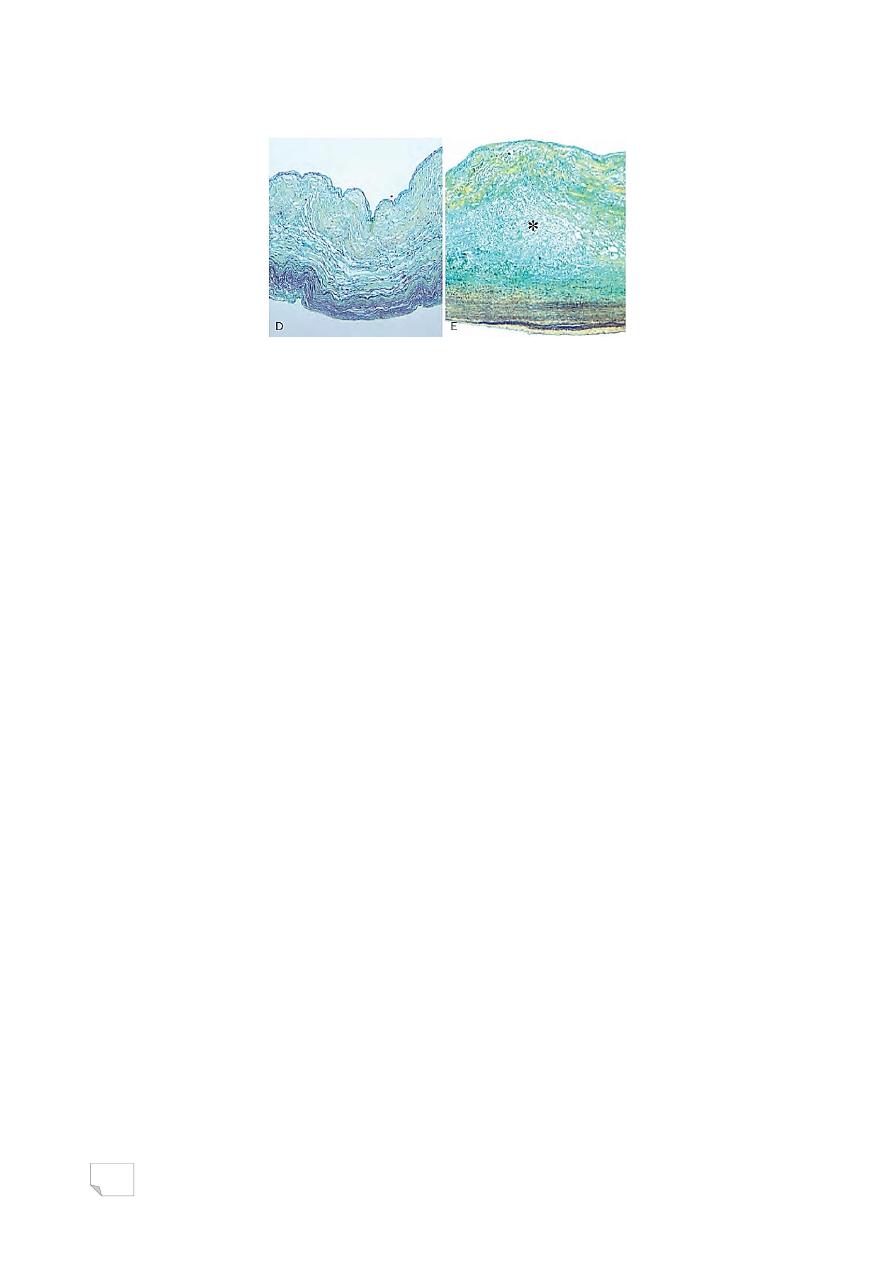
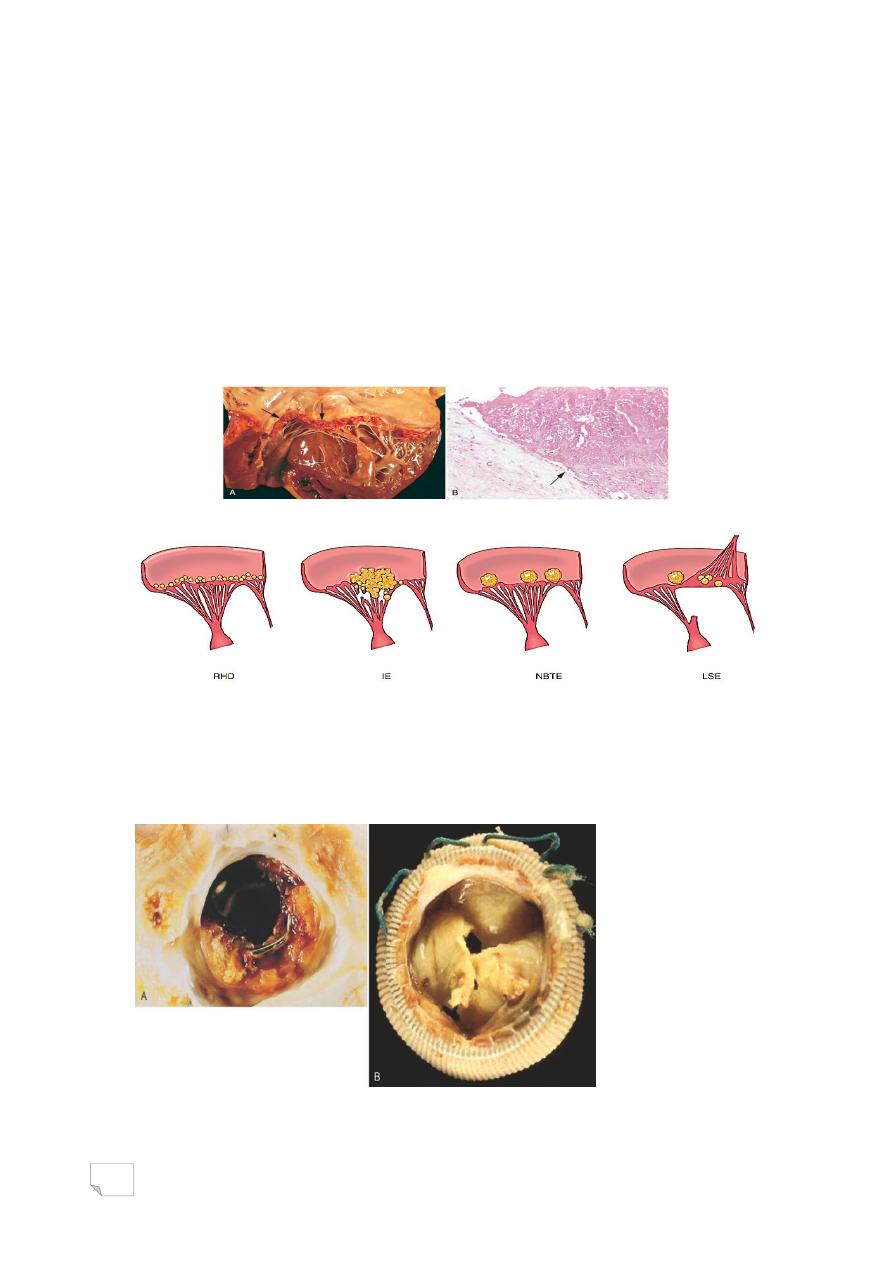
Rheumatic heart disease, acute, chronic
Pathogenesis
- Hypersensitivity reaction induced by streptococci in genetically
susceptible individual (3%)
- 2 Mechanisms are involved:
1 . Antibodies directed against M proteins of
certain strains of streptococci cross-react with glycoprotein antigens
in various tissues
2 . CD4+ T cells cross-react with host antigens and elicit cytokine-
mediated inflammatory responses.
Clinical features:
- Major manifestations
1. Migratory polyarthritis of large joints
2. Carditis
3. Subcutaneous nodules
4. Erythema marginatum
5. Sydenham chorea
61
- Minor manifestations
. Fever
. Arthralgia
. Elevated blood levels of acute phase reactants
— Diagnosis:
- Established by Jones criteria
. Evidence of streptococcal infection, plus
. Presence of 2 major manifestations OR
. one major and 2 minor manifestations
INFECTIVE ENDOCARDITIS
. Characterized by:
- Microbial infection of the heart valves or the mural endocardium
- Formation of friable vegetations (thrombotic debris & organism)
- Destruction of the underlying cardiac tissues
. Causes:
- Bacteria (most cases) inclduing: S. viridans, S. aureus, enterococci,
HACEK group, S epidermidis
- Fungi
- Rickettsia
- Chlamydia
Classification
- Acute, occurs in previously normal heart valve, caused by highly
virulent microbe (eg. S aureus)
- Subacute, occurs in a previously abnormal valve, caused by low
virulent microbe ( eg. S viridans)
* Both types are points along a spectrum and a clear delineation
between them does not always exist
Etiology and pathogenesis
- Predisposing cardiac conditions
. Rheumatic heart disease
. Myxomatous mitral valve
. Degenerative calcific valve
. Bicuspid aortic valve

62
. Artificial valves
- Host factors
. Neutropenia
. Immunodeficiency
. Malignancy
. Diabetes mellitus
. Intravenous drug and alcohol abuse
. Morphology:
- Single or multiple friable, bulky and destructive vegetations
containing inflammatory cells, fibrin, and microbes on the heart valves
- Aortic and mitral valves are most commonly involved
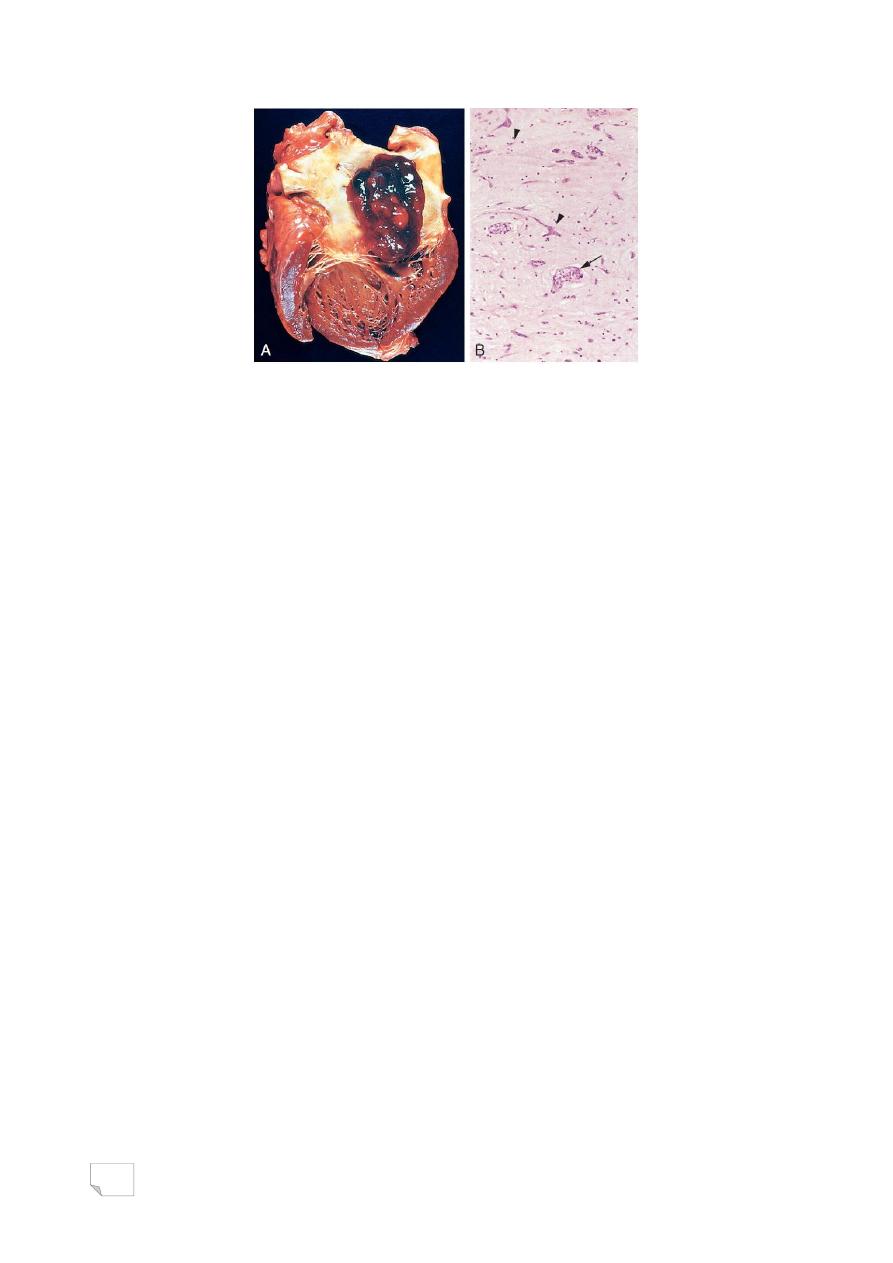
Infective bacterial endomcarditis
A. large friable vegetations.
B. congenitally bicuspid aortic valve with extensive cuspal destruction
and ring abscess
. Clinical features
- fever
- fatigue
- loss of weight
- Murmur
- Petechia in nail bed (splinter) hemorrhages, retinal hemorrhages
(Roth spots), painless palm or sole erythematous lesions (Janeway
lesions), or painful fingertip nodules (Osler nodes)
. Complications
- Ring abscess
- Systemic emboli causing septic infarcts and
mycotic aneurysms
63
NON INFECTIVE THROMBOTIC
ENDOCARDITIS
. Deposition of small vegetations on cardiac valves surfaces
. Usually is found on previously normal valves.
. Hypercoagulable states are the usual precursor to NBTE
. Encountered in debilitated patients who are suffering from:
- Cancer
- Sepsis
- DIC
- Malnourishment
Nonbacterial thrombotic endocarditis (NBTE)
Vegetations
ARTIFICIAL VALVES
. Types
- Mechanical prostheses
- Bioprostheses
Artificial heart valves
A. mechanical B. bioprosthetic
64
د. مصطفى
امراض
22
\
2
\
2142
( عدد االوراق
5
) م
\
3
\
موصل
Lec: 7
The Heart
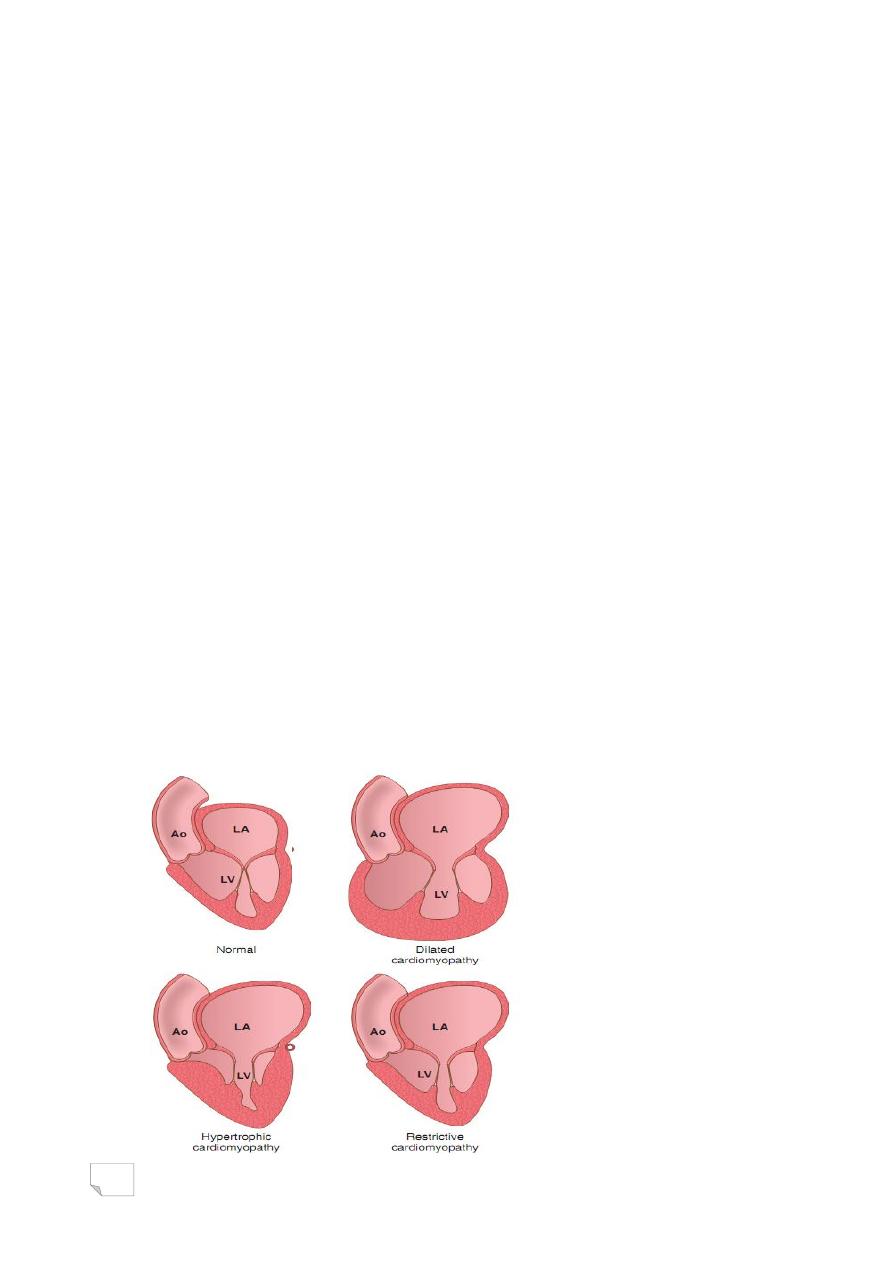
CARDIOMYOPATHIES
Definition: literally ―heart muscle diseases”
Etiology:
- Primary cardiomyopathies: are intrinsic diseases of the heart
muscle( genetic or acquired diseases of myocardium)
- Secondary cardiomyopathies : myocardial involvement as
component of systemic or multiorgan disorder.
. Types:
- Dilated( congestive) …… 90%
- Hypertrophic
- Restrictive ……. Least common
. Endomyocardial biopsy for:
- Diagnosis
- Management for
. patients with myocardial disease
. in cardiac transplant recipients
65
Cardiomyopathies
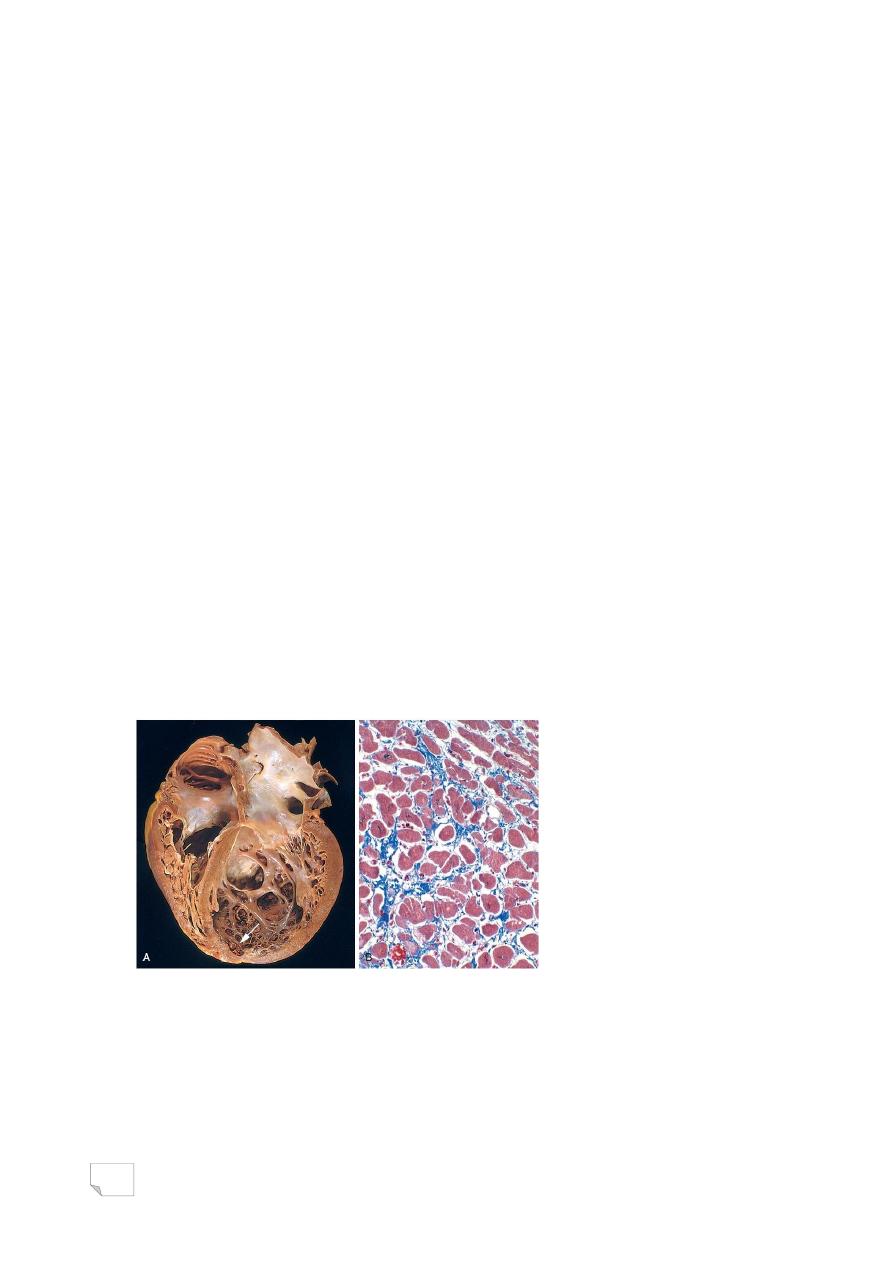
Dilated Cardiomyopathy
. Characterized by
- Progressive dilation
- Contractile (systolic) dysfunction (poor contraction) usually with
concomitant hypertrophy
. Causes
- genetic influence 30%-50% of cases (with TTN [titin protein]
mutation in 20%)
- chronic alcoholism
- myocarditis
- pregnancy-associated
- iron overload , hemochromatosis
- idiopathic
. Morphology:
- Gross, (heart is 2-3 times heavier than normal, is flabby and dilated,
with mural thrombi)
- Microscopy, (myocytes hypertrophy,
interstitial and endocardial fibrosis)
Dilated cardiomyopathy, Masson trichrome stain
. Clinical features
- Age incidence is 20-50 years,
- Patient has slowly progressive congestive cardiac failure
- 50% of patients die within 2 years
- only 25% survive more than 5 years
66
. Treatment
- Cardiac transplantation
Arrhythmogenic right ventricular hypertrophy:
- Inherited disease of myocardium causing right ventricular failure and
rhythm disturbances with sudden death.
- Morphologically,: thin right ventricular wall due to loss of myocytes, +
extensive fatty infiltration and fibrosis
Hypertrophic Cardiomyopathy
. Characterized by
- Myocardial hypertrophy
- Impaired diastolic filling > reduced stroke volume
- In about 1/3 of cases intermittent (dynamic) ventricular outflow
obstruction
. Pathogenesis
- Mutation in genes encoding sarcomere proteins
- Most cases are autosomal dominant with variable penetrance
— Morphology:
- Gross, (massive asymmetrical myocardial
hypertrophy without ventricular dilation,
ventricular cavity is banana-like)
- Microscopy:
-Marked myocyte hypertrophy
-Haphazard disarray of bundles of myocytes
-Fibrosis
67
Hypertrophic cardiomyopathy
. Clinical presentation:
- Atrial fibrillation>mural thrombus> embolism
- Infective endocarditis
- Cardiac failure
- Ventricular arrhythmias
- Sudden death
68
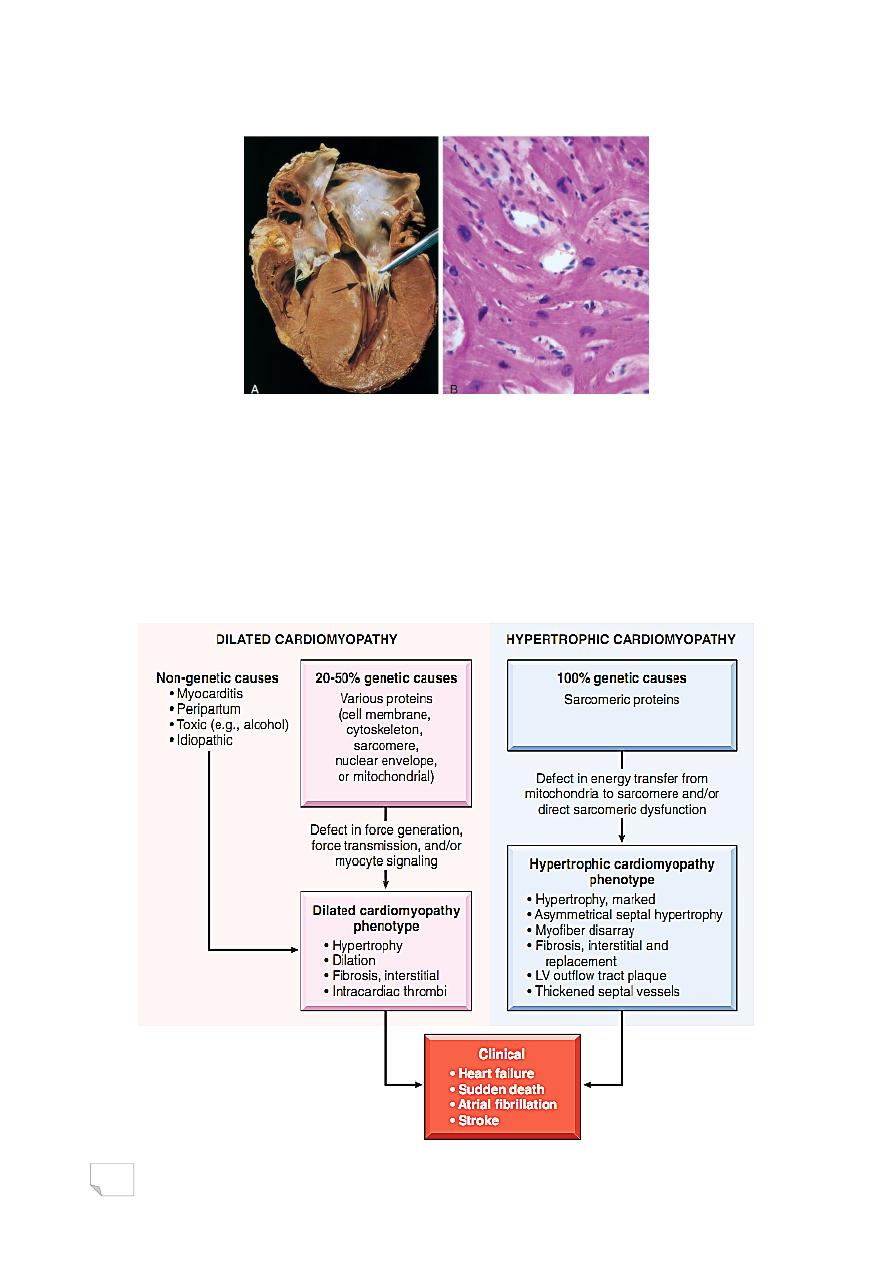
Causes and consequences of dilated and hypertrophic
cardiomyopathies
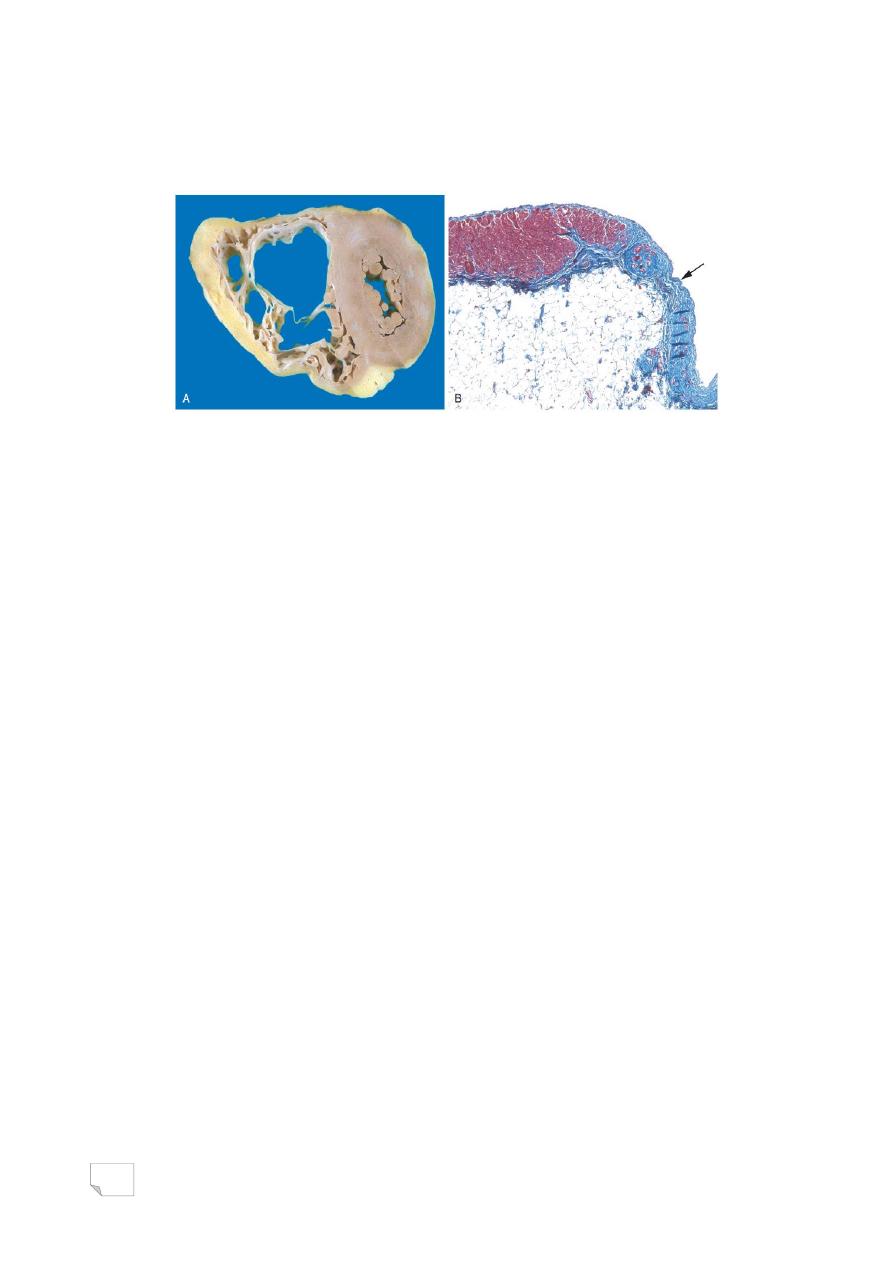
Restrictive Cardiomyopathy
. Primary decrease in ventricular compliance (stiff wall) > impaired
diastolic ventricular filling
. Idiopathic or associated with diseases that affect the myocardium,
(radiation fibrosis, amyloidosis, sarcoidosis, metastatic tumor, inborn
error of metabolism)
. Morphology:
- Gross, (normal size ventricles with normal cavities, myocardium is
firm)
- Microscopy, (interstitial fibrosis)
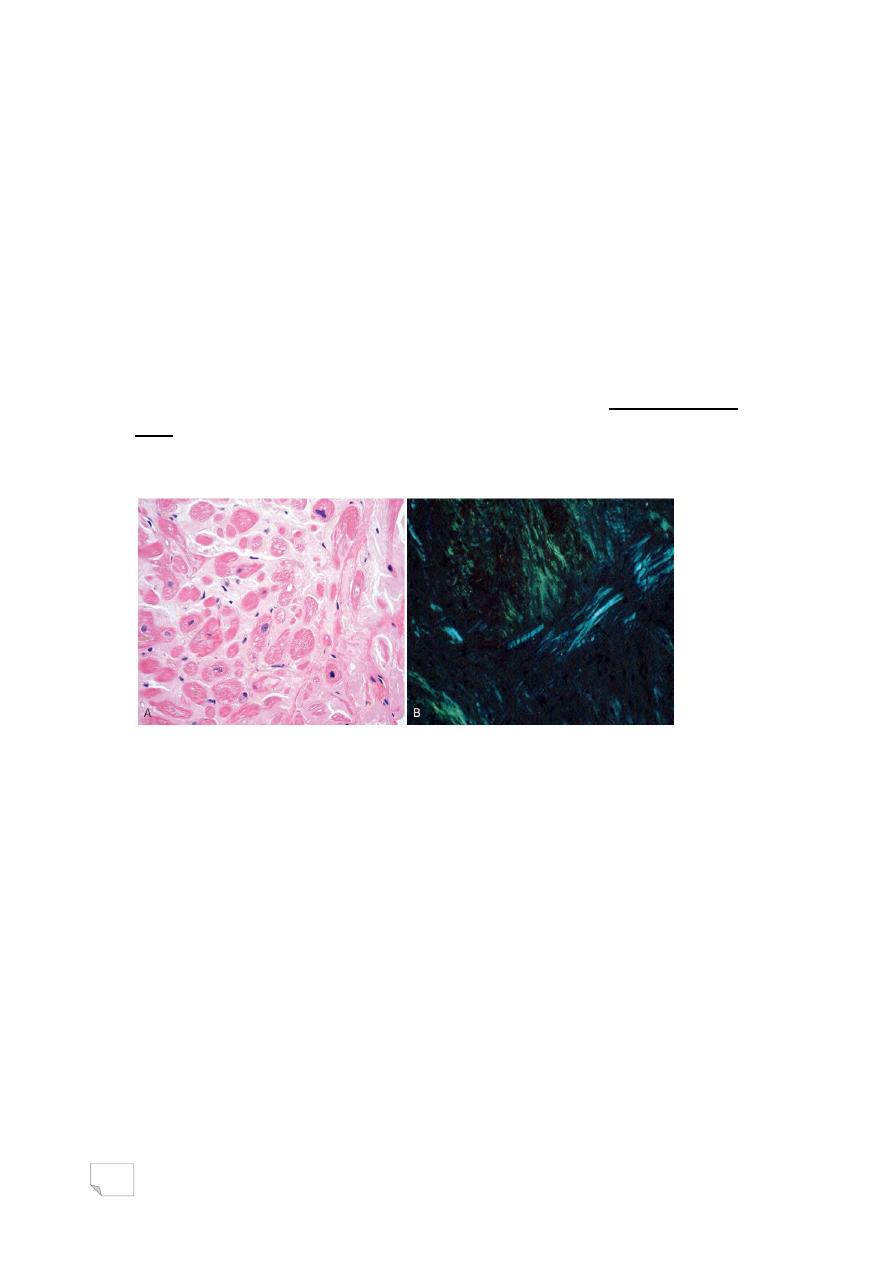
Cardiac amyloidosis, H & E stain, Congo red stain under polarized
light
Other restrictive Conditions of the heart:
. Endomyocardial fibrosis
. Loeffler endomyocarditis
. Endocardial fibroelastosis
MYOCARDITIS
. Inflammatory processes primarily target the myocardium (rather
than a response to myocardial injury as in IHD)
. Etiology
- Viruses (coxsackie viruses A and B)
- Protozoa (Trypanosoma cruzi) Chagas disease
- Helminthic (Trichinosis)
69
- Parasites (Toxoplasma)
- Bacteria (Diphtheria)
- Non-infectious causes including:
-hypersensitivity myocarditis
-giant cell myocarditis
. Morphology
- Gross, (ventricles are flabby with foci of hemorrhage, mural thrombi
may be present)
- Microscopy, (interstitial inflammation and fibrosis, focal necrosis of
myocytes)
. Clinical features
- asymptomatic
- heart failure
- sudden death
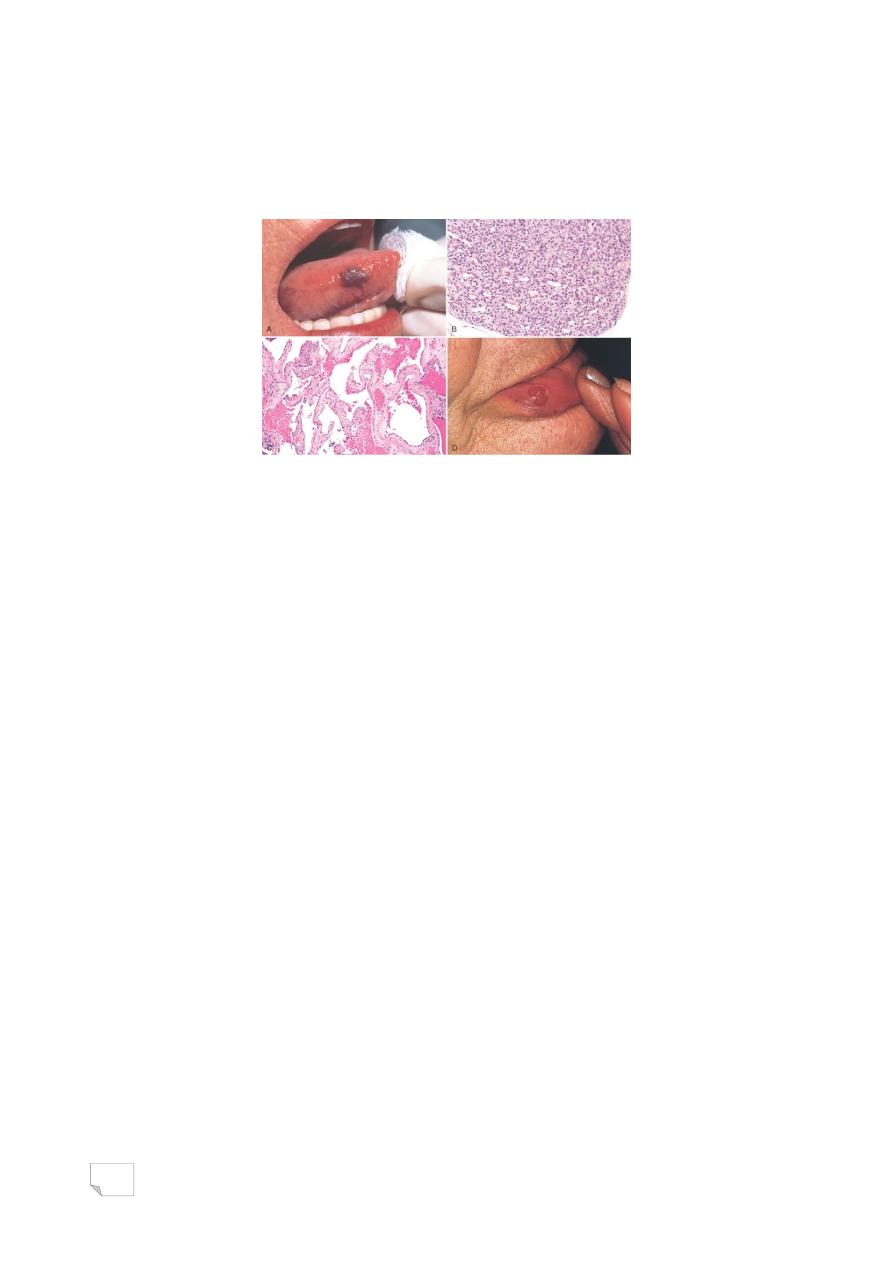
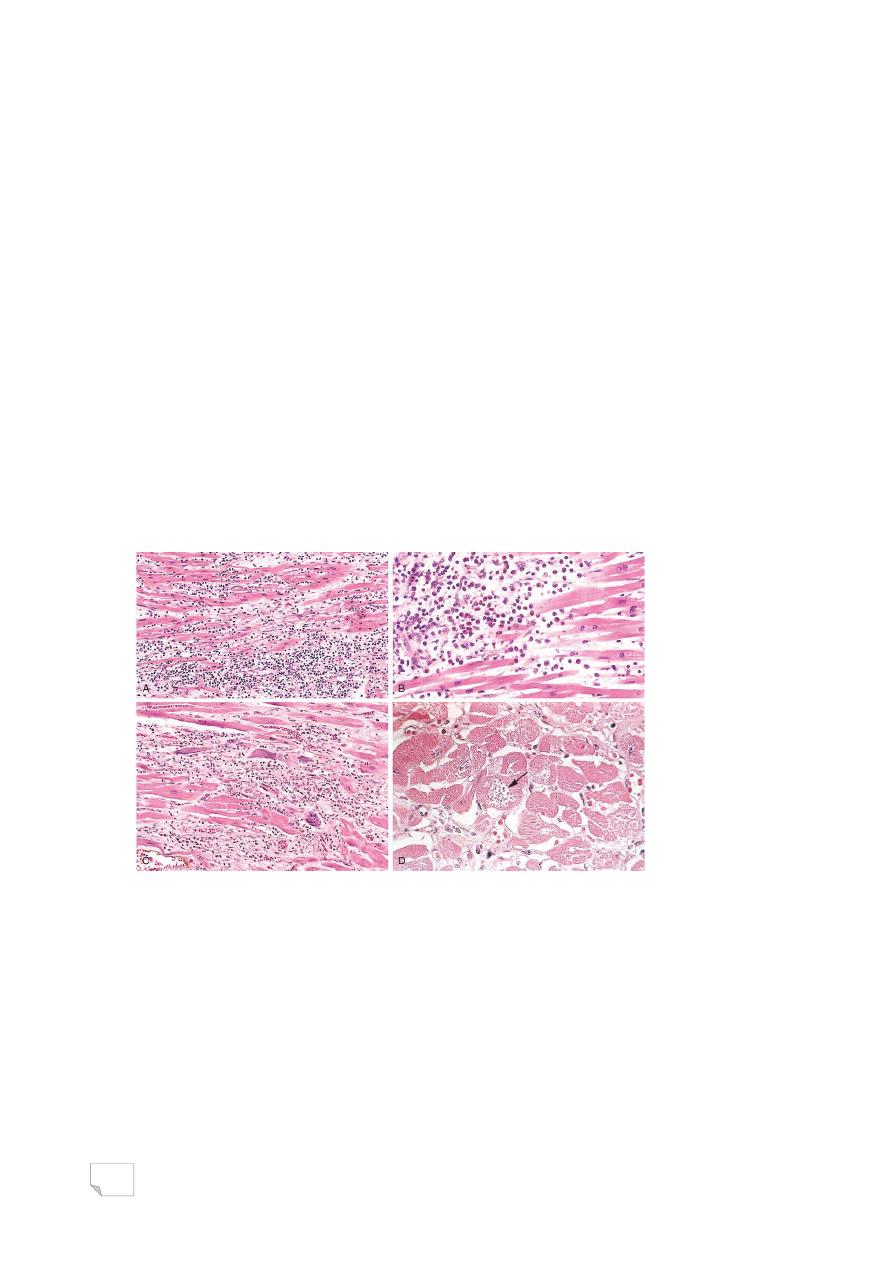
Myocarditis: A, Lymphocytic myocarditis. B, Hypersensitivity
myocarditis. C, Giant cell myocarditis. D, Chagas myocarditis
PERICARDIAL DISEASES
- Inflammation
- Effusion
70
Pericardial Effusion
. Abnormal accumulation of fluid in pericardial spaces ( normally:
30-50ml).
. Slowly accumulating effusion of less than 500 ml has little clinical
effect
. Rapidly accumulating fluid of as little as 200-300 ml> compression
of atria & vena cava> may produce potentially lethal cardiac
tamponade
— Serous fluid (pericardial effusion)
— Blood (hemopericardium)
— Pus (purulent pericarditis)
Pericarditis
— Acute:
- Serous pericarditis
- Fibrinous and serofibrinous pericarditis
- Purulent or suppurative pericarditis
- Hemorrhagic pericarditis
- Caseous pericarditis
— Chronic (healed):
- adhesive pericarditis: no effect on cardiac function
- constrictive pericarditis: limit diastolic expansion
— Primary pericarditis is uncommon, most often is due to viral
infection
— In most cases, pericarditis is secondary to cardiac, thoracic, or
systemic disorders, metastases from remote neoplasms, or cardiac
surgical procedures
— Pericarditis can:
(1) Cause large effusion > immediate hemodynamic complications
(cardiac tamponade)
(2) Resolve without significant sequelae
(3) Progress to a chronic fibrosing process.
71
Suppurative pericarditis
TUMORS OF THE HEART
. Primary tumors are rare
. Metastatic tumors occur in about 5% of
patients dying of cancer
Myxoma
. Most common primary tumor
. Benign
. Mostly (90%) located in the atria as solitary
sessile or pedunculated mass of 1-10cm
. Histology: stellate, frequently multinucleated myxoma cells
embedded in an abundant acid mucopolysaccharide ground
substance
. Clinical presentation
- Valvular “ball Valve”obstruction
- Embolization
- Constitutional symptoms, (fever, malaise)
72
Left atrial myxoma, A large pedunculated in fossa ovalis and extends
into the mitral valve orifice. B, Abundant amorphous extracellular matrix
contains scattered multinucleate myxoma cells (arrowheads) in various
groupings, including abnormal vascular formations (arrow).
— Other cardiac tumors:
- Lipoma
- Papillary fibroelastoma
- Angiosarcoma
CAERDIAC TRANSPLANTATION
. Indicated for severe intractable heart failure
. Factors contributing to the success of cardiac transplantation:
- Careful selection of candidates
- Improved immunotherapy
- Early histopathologic diagnosis of acute rejection by sequential
endomyocardial biopsy
. Complications:
-Rejection
-Infection
-Malignancy
-Progressive, diffuse stenosing intimal proliferation of the
coronaries, (graft
arteriopathy)
. silent MI
. congestive heart failure
. sudden death due to chronic immune
73
response
Complications of heart transplantation,
allograft rejection graft coronary atherosclerosis

74
