Drugs for the treatment of diabetes mellitus
Characteristics• Type 1 (10%)
Type 2
Onset (age)Usually 30
Usually >40
Type of onset
• Abrupt
• gradual
• Nutritional statusUsually thin
• Usually obese• Ketosis
Frequent
Usually absentendogenous insulin
Absent
Present but usually ineffective
Insulin therapy
Required
Required in only 20-30%
• Hypoglycemic drugs
Should not be used
Clinically indicatedInsulins
1- Ultra-Short acting insulin2- Short-acting (regular) insulin
3- Intermediate-acting insulin
4- Long-acting insulin
Insulins are administered SC
Ultra short and short insulin can be given IV in emergency cases
Insulins
1- Ultra-Short acting insulin(Lispro, aspart)
Onset within 5 minutes and duration 2-4 hours
2- Short acting insulin (regular)
(Humulin, Novolin )
Onset of action within 30-45 minutes and duration 6-8 hours
Insulins
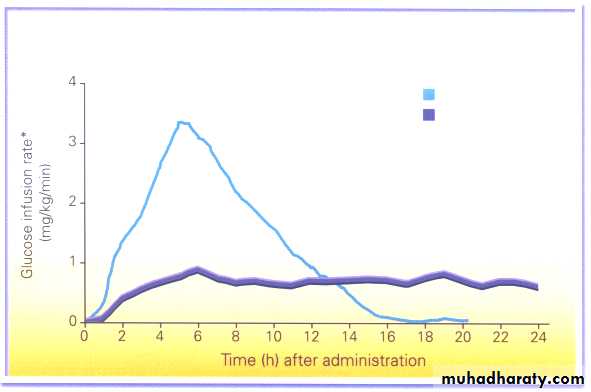
3- Intermediate-acting insulins(isophane (NPH), Lente insulin)
• Onset of action 1-2 hr and duration of action 13-20 h
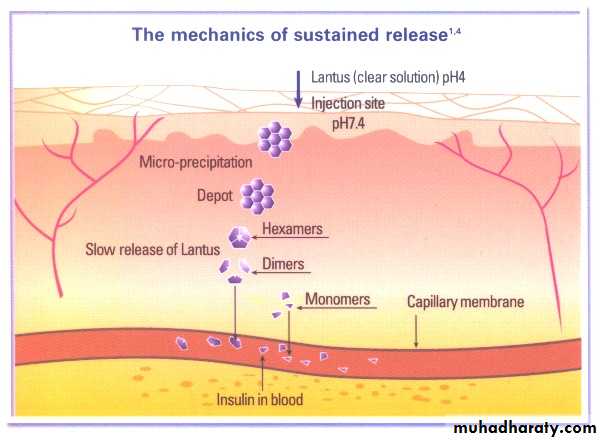
4- Long-acting insulins
(Insulin glargine, ultralente)
Onset of action 2 hr and duration of action up to 24 hr
8
KATP Channel Structure and Function
NBF
Nucleotide Binding Fold = site of ATP/ADP binding
Four copies of each subunit combine to form an active KATP channel
NBFNBF
Sulfonylurea Receptor Inwardly Rectifying
K+ Channel
K+
ATP-sensitive K+ Channel (KATP Channel)
ADPADP
glucose
Membrane
Depolarization
insulin secretion
ATP
ATP
ATP
Voltage-dependent
Ca2+ Channelglucose
metabolismCa2+
Influx9
IRS-1/2
Mechanism of Insulin ActionGlucose
GlucoseTransporter
Insulin
Receptor
P
P
P
P
P
IRS-1/2
PP
P
P
P
P
Translocation
of
Glucose
Transporters
Skeletal muscle
Adipose Tissue
Recruitment of Effectors
Protein:Protein InteractionsSignal Transduction Networks
Activation of Phosphorylation Cascades
Biologic Response
Glargine
Profile of Insulin Glargine vs NPHNPH
Glargine
complications of insulin therapy
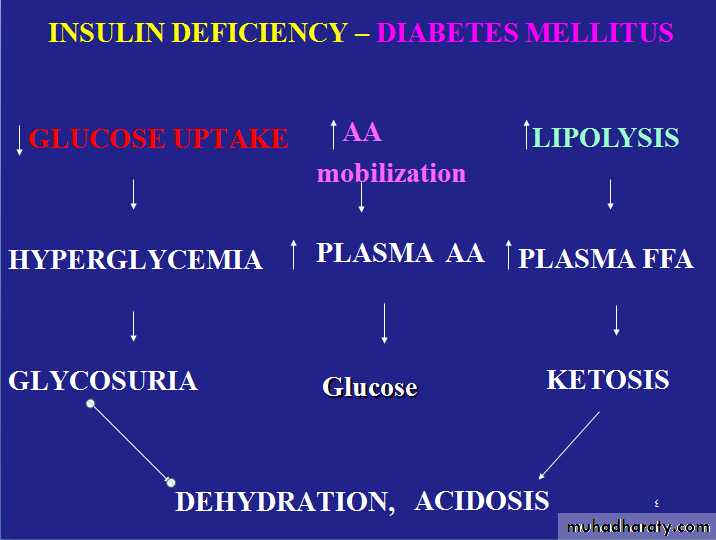
• 1. Severe Hypoglycemia (< 50 mg/dl )– Life threatening• Overdose of insulin
• Excessive (unusual) physical exercise
• A meal is missed
• 2. Weight gain
• 3. Local or systemic allergic reactions (rare)
• 4. Lipodystrophy at injection sites
• 5. Insulin resistance
• 6. Hypokalemia
Oral Hypoglycemics
1- SulphonylureasFirst generation- chloropropamide
Second generation-
Short acting- glipizide
Long acting- Glibenclamide, glimipride
2- Biguanides
Metformin
3- Meglitinides
Repaglinide, Nateglinide
4- Thiazolidinediones
Rosiglitazone, Pioglitazone
5- α-Glucosidase Inhibitors
Acarbose
1- Sulphonylureas
Mechanism of action of sulphonylureas• 1) Release of insulin from β-cells
• 2) Reduction of serum glucagon concentration• 3) Potentiation of insulin action on target tissues
17
17
Mechanism of Sulfonylurea Action
NBF
NBF
Sulfonylurea Receptor Inwardly Rectifying
K+ Channel
K+
ATP-sensitive K+ Channel (KATP Channel)
MembraneDepolarization
Ca2+
Influxinsulin secretion
Voltage-dependent
Ca2+ ChannelADP
ADP
ATP
ATP
Sulphonylureas
Side effects• 1) Nausea, vomiting, abdominal pain, diarrhea
• 2) Hypoglycaemia
• 3) Blood dyscrasias
• 5) Weight gain
2- BIGUANIDES (group)
Metformin
Mechanism of action
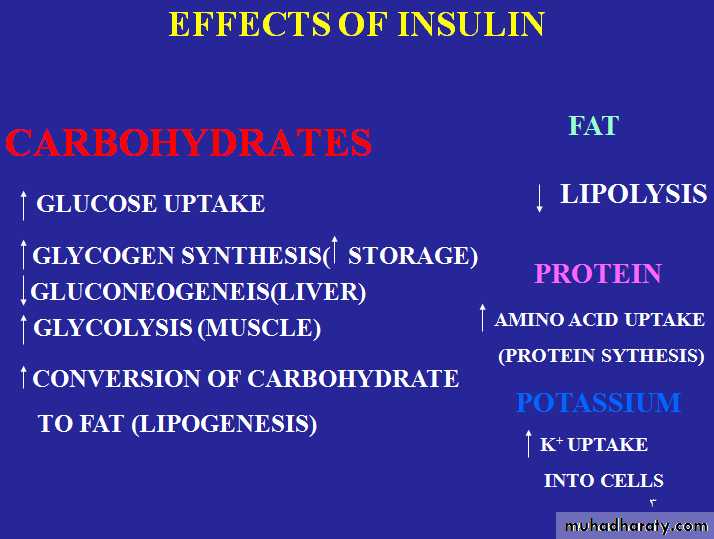
1- Increase peripheral glucose utilization
2. Inhibits gluconeogenesis
3. Impaired absorption of glucose from the gut
BIGUANIDES (group)Metformin
UsesIt is used in obese patients with type 2 diabetes
It does not cause hypoglycemia or weight gain (causes anoroxia)
It can be used in combination with sulphonylureas
It used in polycystic ovary disease.
2- BIGUANIDES (group)Metformin
Side effects• 1. Metallic taste in the mouth
• 2. Gastrointestinal (anorexia, nausea, vomiting, diarrhea, abdominal discomfort)
• 3. Vitamin B 12 deficiency (prolonged use)
4.Lactic acidosis in hepatic and renal failure.
3- Meglitinides (group) Repaglinide, Nateglinide
• Mechanism of action
• Bind to the same KATP Channel as do Sulfonylureas, to cause insulin release from β-cells
3- Meglitinides (group) Repaglinide, Nateglinide
Uses• Approved as monotherapy and in combination with metformin in type 2 diabetes
• Taken before each meal, 3 times / day
• It s main advantage by reducing postprandial blood glucose
• Side effects
• Hypoglycemia
• Wt gain ( less than Sufonylureas)
Thiazolidinedione
New class of oral antidiabetics• Rosiglitazone
• Pioglitazone
Mechanism of action
• Increase target tissue sensitivity to insulin by:• reducing hepatic glucose output & increase glucose uptake & oxidation in muscles & adipose tissues.
Uses
• Type II diabetes alone or in combination with
• metformin or sulfonylurea or insulin in patients
• resistant to insulin treatment.
Adverse effects
• Mild to moderate edema, wt gain, myalgia• hepatotoxicity ?
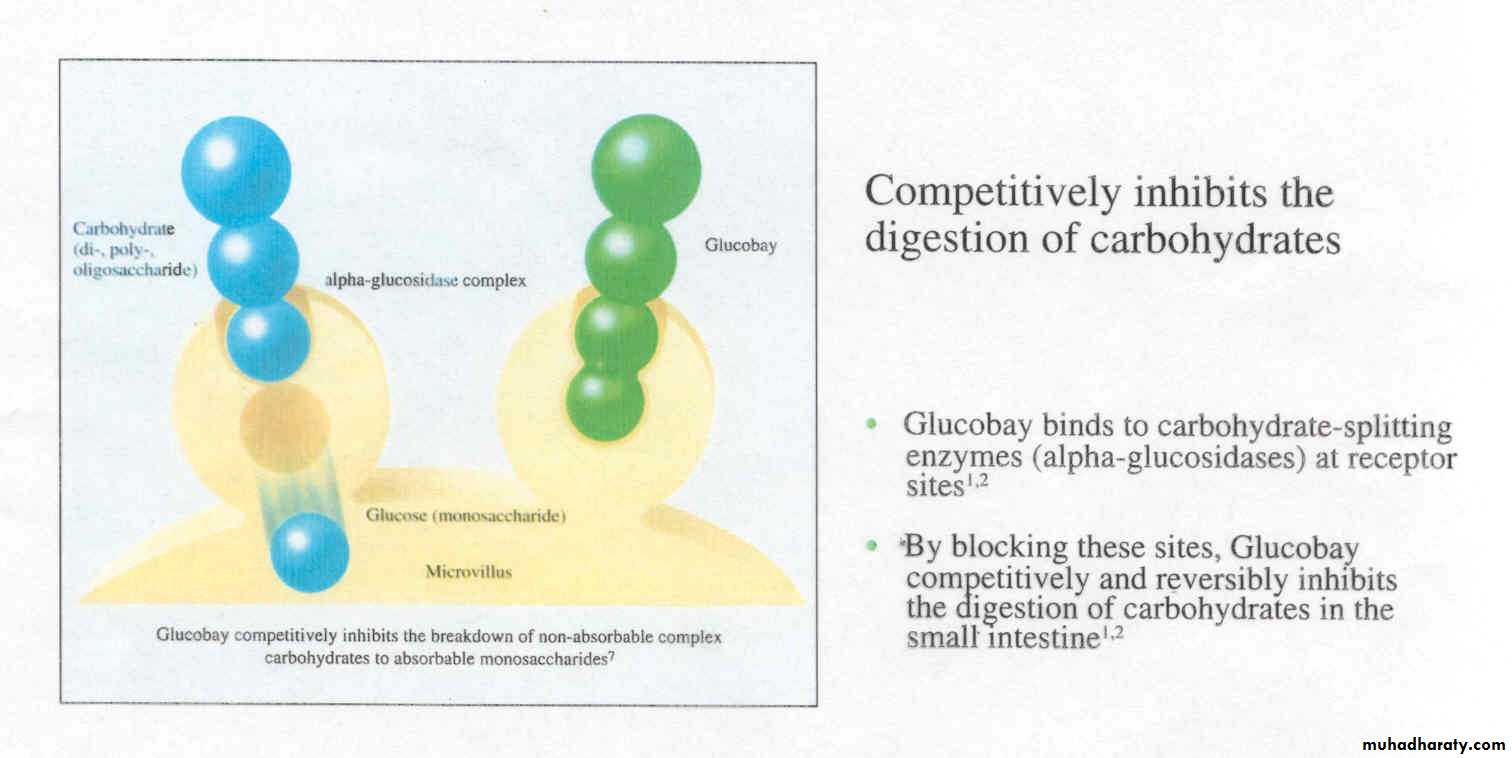
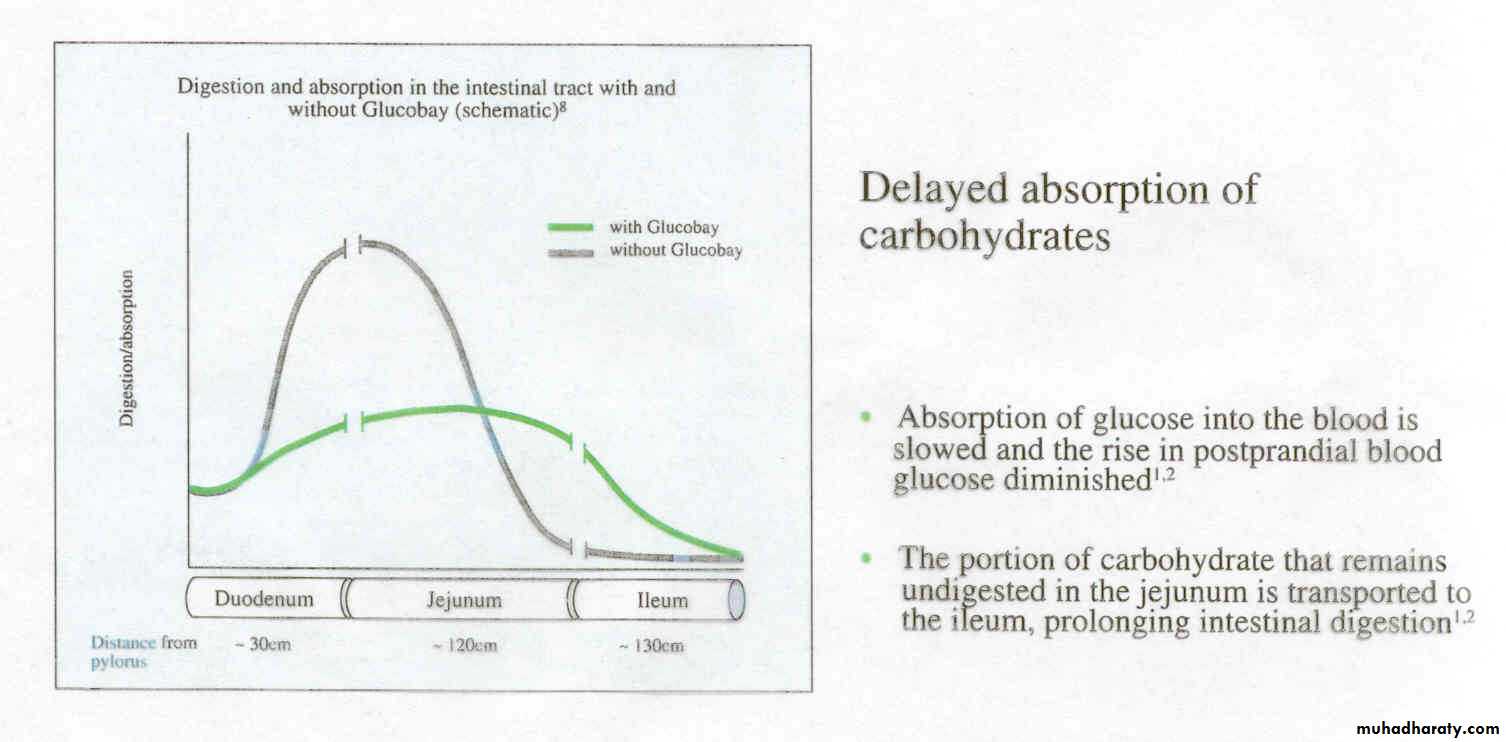
α-glucosidase inhibitors Acarbose
Mechanism of action• Inhibits intestinal alpha-glucosidases and
• delays carbohydrate absorption, reducing postprandial increase in blood glucose
α-GLUCOSIDASE INHIBITORSMECHANISM OF ACTION
Acarbose
AcarboseAcarbose
30
α-Glucosidase inhibitors
•α-glucosidase inhibitors Acarbose
Uses• Patients with Type II inadequately controlled by
• diet with or without other antidiabetic drugs
• may be helpful in obese Type II patients
• (similar to metformin)
α-glucosidase inhibitors Acarbose
• Side effects• Flatulence, loose stool or diarrhea, abdominal pain, alone does not cause hypoglycemia